Abstract
Acupuncture has been widely used in China for three millennia as an art of healing. Yet, its physiology is not yet understood. The current interest in acupuncture started in 1971. Soon afterward, extensive research led to the concept of neural signaling with possible involvement of opioid peptides, glutamate, adenosine and identifying responsive parts in the central nervous system. In the last decade scientists began investigating the subject with anatomical and molecular imaging. It was found that mechanical movements of the needle, ignored in the past, appear to be central to the method and intracellular calcium ions may play a pivotal role. In this review, we trace the technique of clinical treatment from the first written record about 2,200 years ago to the modern time. The ancient texts have been used to introduce the concepts of yin, yang, qi, de qi, and meridians, the traditional foundation of acupuncture. We explore the sequence of the physiological process, from the turning of the needle, the mechanical wave activation of calcium ion channel to beta-endorphin secretion. By using modern terminology to re-interpret the ancient texts, we have found that the 2nd century b.c. physiologists were meticulous investigators and their explanation fits well with the mechanistic model derived from magnetic resonance imaging (MRI) and confocal microscopy. In conclusion, the ancient model appears to have withstood the test of time surprisingly well confirming the popular axiom that the old wine is better than the new.
Keywords: Acupuncture, Acoustic wave, Ca2+ ion channels, Calcium waves, Meridians, Chinese traditional medicine
Introduction
Acupuncture has been used in China from its very beginning some 2,500 years ago [26]. But it has been a puzzle for the West since it was brought back by the Jesuits in the 17th century. In its recent form, acupuncture became popular only after an unexpected treatment of a New York Times reporter in 1971. Since then, it has been widely deployed with clinical success for migraine, knee and back pain, chemo-induced nausea, vomiting and hot-flash among other aches and pains. Yet the typical Westerner, particularly the American doctor, is still looking at it with a suspicious eye. The main reason is the lack of a satisfactory scientific theory of its basic mechanism. Why can the little needle perform such a miracle without any help from drugs? How do the needle and the muscle interact? What is the driving force? Do tissues and cells know the needle is working in the neighborhood? What is its sphere of influence? How is it possible to produce the biochemical reaction that gives rise to pain suppression? Why are there no side effects? Why do the so-called sham, Korean, and Japanese acupuncture also work? Is it just a placebo effect? These are some pertinent questions people would like to have answered.
In the last four decades, a great deal of research in acupuncture has been performed [38]. This review plans to take a look at the basic mechanisms from its long history to find out how far we have come and what is still missing. A number of theoretical models have been proposed. The crucial questions to ask are whether the model is science based and reproducible, whether it covers the complete healing process, not just a part, and whether it conforms to the clinical and experimental data. These are exacting demands in order to arrive at a self-consistent explanation.
From ancient history to modern times
Since its first report in Yellow Emperor’s Manual of Corporeal Medicine (Huang Di Nei Jing, also known as Inner Canon) in the 2nd century b.c., acupuncture has been widely implemented but not understood. While its method in the Nei Jing is simple, its language is archaic and principle veiled, making it a real challenge even for the initiated [29].
The ancient Chinese tradition and history appears to be an attempt of telling the truth about acupuncture. Although empirical, the old data, including the maps of meridians and acupoints, indicate they were carefully collected, examined, analyzed and reported. But the lack of scientific knowledge and technical terms at the time restricted its description so that most of the ancient texts were interpreted based on the interpreter’s experience, more subjective than objective. The challenge is therefore to clarify the model and true meaning presented 2,200 years earlier. We have to understand the traditional acupuncture and present it in the light of the 21st century scientific thoughts and experimental evidence. In the old Chinese vernacular, our attempt is to harmonize the seemingly conflicting evidence so as to fill the gaps of misunderstanding. This would have been an impossible job but for the latest results of research and development. In the last 10 years, it is beyond doubt that acupuncture is effective from both small and large scale randomized controlled clinical trials. Yet, we are far from plumbing the depth in finding out how our body is capable, with a little help of pricking, of healing itself without a large dosage of chemicals.
The ancient Chinese have a profound conviction of the organic unity of the universe and of the human body as a whole. They believed there are two fundamental forces, the yang and the yin, the former represents the light, masculine, external, sunny and dry side and the latter the dark, feminine, internal, shadowy and moist. These are not prejudices if one takes it as sun and moon, positive and negative charge, or matter and anti-matter. (However, we must focus on the science alone as there were quite a bit of superstitions, mystics, voodoo, and philosophical musing in the ancient world that should have no place in our scientific thoughts.) The two forces are working together and in balance. In the body, this duality is expressed in the qi (yang) and the blood (yin) as two separate circulation systems. The concept of qi is analogous to the pneuma of Stoic and Greek medicine [29]. The great biochemist-turned-historian Joseph Needham said both qi and pneuma are untranslatable but could be called life-breath, subtle influence or ethereal—a rarefied form of energy. While the blood is pumped by the heart and circulates through the arteries, veins and capillaries, the qi is generated by the lungs and flows through invisible tracts called jin-luo (meridian) in the body [39].
The meridian is an occidental translation attempting to describe jin-luo as having multi-functions in analogy with astronomical hour-circles or terrestrial longitude. Thus, meridians are the conductive pathways or arrays of network supporting the circulation of qi. The blood and qi are interrelated, mutually supportive or counter balancing as yin and yang. These two forces along with the meridians and five elements are fundamental to the basic physiology and pathology in ancient Chinese medicine. The function of the tract-channel system of the human body is to promote a normal circulation of the blood and qi so that the vital essentials derived from man’s food can nourish the yin and yang, sustain the muscle, sinews and bones, and lubricate the joints [39]. As for the meridians, Needham described it intuitively as a system for transporting energy and fundamentally circulatory in nature to all tissues round the body [29]. Jin may be translated as channel with luo as the multiple branches so that the body surface is all under the jin-luo influence [39]. Along the meridians are a large number of “points” on the surface of the body, 365 were numbered (probably corresponding to the calendar days) in the 1st century b.c. and over 400 in late 20th century. But for practical purpose, fewer than 50 are normally employed [26].
“Lost my appendix in an operation by acupuncture”
Acupuncture made its grand entrance to the modern world by means of James Reston, arguably the most powerful reporter of the world in 1971. As if we needed more confusion, Reston [32] coined this subtitle, a typical misleading statement about acupuncture. In a critical moment of China–America rapprochement, Reston, after being shaken up in a detour set off by Kissinger, had an appendectomy and was in considerable discomfort in Beijing. Acupuncturist Li, presumably sent by Zhou En-Lai to save the day, inserted three long thin needles into the outside of Reston’s right elbow and below his knee. There was a noticeable relaxation of the pressure and distension within an hour and no recurrence of the problem thereafter [31]. This report on the front page of the New York Times transformed the humble needle into the new sensational instrument of healing. The publicity brought about new interest and rigor leading to deeper and more diverse explorations by serious scientists employing the latest scientific methods and technology. We are indebted to Reston for giving up his appendix. Acupuncture was re-born in travail and adversity.
Neural mechanisms of acupuncture analgesia
Acupuncture in the early 1970s immediately ran into two major obstacles. The first was high expectation from the public. The second was the lack of a theory to explain what went on physiologically and pathologically in the body after the insertion of the needles. As pointed out earlier, one of the biggest challenges is to learn whether the traditional Chinese theory of acupuncture is close to the truth or not. We have to first translate the ancient archaic language into the ordinary tongue or the 21st century scientific terms. But meridian is invisible in our anatomy and cannot be explained by present-day physiology. We do not know what qi is. The concept of de qi is not well defined. To handle this lack of precision, a standard description of feeling “soreness, numbness, heaviness and distension” by the patient is employed. For a large number of researchers, the meridians may be conceived as a functional but not anatomical concept. They may summarize multiple physiological functions including the circulatory, endocrine, nervous, and immune systems. Since meridian and qi are not observable, most of the research since 1970 has focused on the neural based mechanisms. The references are listed in book and review articles [12, 38, 42], and they include the most quoted references [13, 27, 28, 30].
Let us summarize this field based on a recent review [42]: (1) Traditional Chinese (verum) acupuncture analgesia is manifest only when de-qi concurs. (2) Afferent nerve fibers are activated in manual or electrical acupuncture. (3) It is an integrated process at different levels of the central nervous system (CNS) between impulses from acupoints and afferent signaling from painful regions. (4) Spinal pathways of acupuncture impulses from acupoints ascend mainly through the ventrolateral funiculus. Most of sensory nuclei such as the nucleus raphe magnus (NRM) and the nucleus reticularis gigantocellularis (Rgc) are constitutive parts of the endogenous descending inhibitory system in CNS. (5) Opioid peptides and glutamate are implicated. (6) Effectiveness of acupuncture, without adjunct drugs for surgery is not satisfactory. (7) Acupuncture is effective in treating chronic pain. (8) Conflicting results of acupuncture are caused by activation of different afferent nerve fibers. Central to these models is the participation of the afferent nerve fibers and CNS. Recent research has moved to pain control and brain imaging [13].
There is a significant concern for the neural mechanism. In replacing the meridians by nerves and CNS, the modern researchers have effectively changed the basic model of the ancient texts. Ancient Chinese medicine was much more advanced and sophisticated than its Western counterpart. Circulation of blood was recognized in 6th century b.c., and both circadian rhythms and endocrinology were known in 2nd century b.c., around the time acupuncture was practiced [29]. Jin-luo was not the nerves. But the decision in Inner Canon of using jin-luo as the basis for their model should not be dismissed off hand. It is possible the neural pathway is part of the connecting networks unrelated to the traditional Chinese model. We need to take meridian and qi seriously to find out what they are and how they can be fit into the current experiments and clinical data.
The underlying neural mechanism of acupuncture was investigated by using functional magnetic resonance imaging (fMRI) starting from the mid 1990. The activation of visual cortices of the brain by stimulation of vision-related acupoints was found and confirmed [4, 22] implying the existence of a vision-related meridian or jin-luo. It was noted that sham acupuncture may produce similar analgesic effect as verum with verum having a greater area of activation [16]. Compared to control, stroke patients with sensory and language deficits seemed to be more sensitive to acupuncture treatment showing direct links between the acupoints and the cortices [21].
Small- and large-scale randomized clinical trials
As acupuncture has enjoyed a phenomenal growth in the world, a large number of randomized controlled clinical trials have been performed in Europe and North America with focus on analgesia. A half-dozen of these have sample size from 300 to more than a thousand. Almost all of them were successful when sham acupuncture was included, and these were published in the leading medical journals [5, 25, 41]. As an example, a program with chronic knee and back pain having 2,201 patients reported an extraordinary success rate of 92% for knee and 94% for lower back pain [7]. Migraine, osteoarthritis, chemo-induced nausea, vomiting and hot flash also were given good reports [8, 9, 11, 40]. The conclusion can be summarized in the following: First, the traditional Chinese (verum) acupuncture that requires de qi is found to accompany the best response. Second, in more than half of the trials, the sham acupuncture was also found to be effective even thought its efficacy is less than verum. This has become a point of contention since there is no physical model for sham acupuncture and placebo effect might have taken over. Third, in contrast with drug treatment, both verum and sham acupunctures are found to have no side effects. As it turns out, all of these observations are important to understand the physiological model and mechanism of acupuncture.
Mechanical modeling: tissue imaging and adenosine enhancement
Physically, acupoint can now be explained by the “needle grasp”, a measurable parameter. When acupuncture is performed properly, de qi is a characteristic needling sensation perceived by the patient while the acupuncturist feels a needle grasp. But the mechanics were overlooked until 10 years ago when it was studied under the microscope [17]. For fibroblasts and endothelial cells, focal adhesions form mechanical links between extracellular collagen matrix and intracellular cytoskeleton. Langevin observed that mechanical coupling between the needle and connective tissue with winding of tissue around the needle during needle rotation and needle manipulation transmits a mechanical signal to connective tissue cells via mechanotransduction. Making use of ultrasound elastography, Langevin et al. [18] showed that the patterns of tissue displacement by acupuncture can be mapped spatially and temporally and that increased rotation results in increased tissue displacement during upward and downward needle movement. It was evident that the needle movement was an effective mechanical stimulus leading to tissue displacement. A structural characterization of the muscle and connective tissues was presented demonstrating the acupuncture operation. However, the mechanistic model shows tissue displacements only on the order of 100 μm without long-range influence, and subsequent study of fibroblast network showed no functional relationship. There was no experimental support of the underlying molecular and cellular manifestation.
In a separate study, the mechanistic action of acupuncture was observed by focusing on adenosine [10]. It was found that insertion and manual rotation of acupuncture needles triggered a general increase in the extracellular concentration of purines, including the transmitter adenosine and ATP metabolites. Anti-nociceptive effect of acupuncture requires A1 receptors, and acupuncture failed to reduce pain in A1 knockout mice. Needle insertion without intermittent rotation stimulation failed to reduce pain sensitivity. While introducing biochemical insight, the mechanistic presentation remained qualitative; it was not clear how adenosine was produced at the molecular level and whether calcium signaling was involved.
Mechanistic acupuncture and cellular response
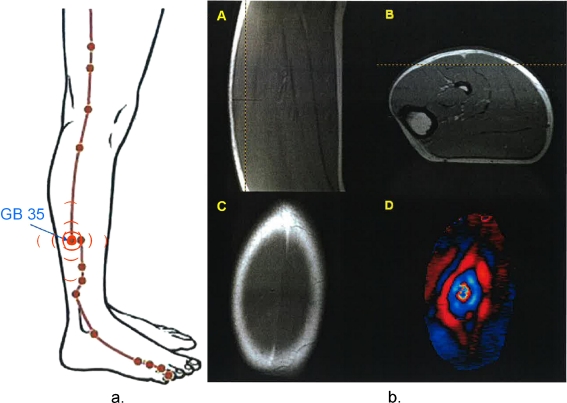
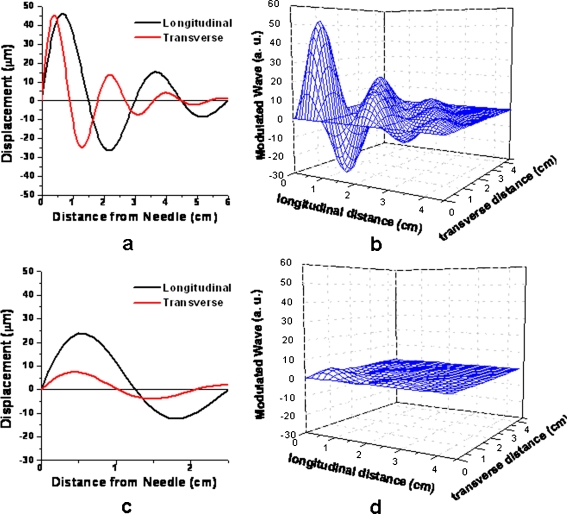
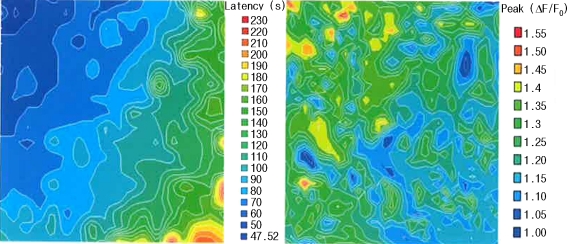
To unravel the complexity of acupuncture, a comprehensive study was initiated to start from the most elementary physical and biological principles [23]. Langevin has made a step in the right direction and her result is important to obtain the mechanical coupling between the needle and the tissues. But the movement of the needle has to be described mathematically to eliminate any ambiguity. Using a piezoelectric transducer to produce a controllable signal was the first step. The spatial and temporal response in the form of an acoustic shear wave could now be observed in the wave-guiding human muscle quantitatively by MRI. In Fig. 1b, A and B show the needle position and C a slice of the T1 images of soleus muscle. After the insertion of the needle and the acoustic shear wave applied, a movie is observed with the positive and negative half of the sinusoid shown in red and blue, respectively. The actual profiles along the vertical and horizontal lines are shown in Fig. 2a. The image shows that the shear wave has propagated more than twice the distance in the longitudinal direction than in the transverse direction. By combining the horizontal and vertical decay using the envelopes of Fig. 2a, an artist’s rendering of the 3D wave propagation is shown in Fig. 2b. A calculation was also made for a sham point that is one centimeter away from the acupoint GB35. The signal is now at significantly lower amplitude while its spreading is similar to that created by the acupoint (Fig. 2d). The contrast between Fig. 2b and d indicates that sham acupuncture has established an area of influence but with a much lower efficacy as projected earlier. The next step was to see if the same acoustic shear wave could activate cultured cells in both endothelial and fibroblast, cells that are known to have function as mechano-sensory cells. An almost trivial invention was needed to mimic the muscle elasticity with suitable gel having good acoustic energy coupling to the cells in a Petri dish. This turns out to be the critical step so that Ca2+ waves, oscillations, latency, and memory become observable under a confocal microscope. Taking a single set of images of the cells without averaging, the latency profile in Fig. 3a shows the calcium wave propagation from the upper left-hand corner to that of the lower right hand corner. The time of propagation is as long as 230 s. The corresponding signal amplitude decay distribution is shown in Fig. 3b. While the speed of the acoustic shear waves is between 1 and 5 m/s and the time scale in tens of milliseconds, the calcium response is in minutes, seemingly a snail’s pace or stationary if one rides on the acoustic driver signal. The actual response requires the superposition of Fig. 3 to that of Fig. 2b. Thus the calcium waves spread out after minutes from the 3D acoustic wave profile reaching out to a broader area of influence. In vivo studies of animals were then performed including the experiments of the two-photon fluorescence from acoustic wave activated calcium and beta-endorphin as the endogenous opioid. One important criterion in this multi-step process is that every step required in the experiments was taken with a one-to-one cause-to-effect response and was quantified.
Fig. 1.
a Acupuncture at GB35. b MRI and magnetic resonance elastography (MRE) imaging of mechanical waves in soleus muscle: (A and B) T1 images showing slice orientation; (C) T1 image of the soleus muscle; (D) MRE wave image in the soleus muscle
Fig. 2.
a Line profile of damped sinusoid in longitudinal and transverse directions at acupoint GB35. The driver frequency is at 100 Hz. b Artist’s rendering of the 3D acoustic shear wave along the jin-luo structure in the soleus muscle derived from the envelopes of the modulated waves. c, d Repeat of a and b for sham point 1 cm left of GB35
Fig. 3.
Intracellular calcium waves in fibroblast (NIH3T3) cells: latency and wave amplitude distributions in two dimensions. Initial spreading velocity is slightly more than 50 μm/s and quickly settled down to 5.5 μm/s within a few seconds. The diagonal spacing is 1.5 cm (with permission from Li et al. [24])
In addition to ancient texts and millennium tradition, we now have extensive clinical data as well as research papers on acupuncture. It is time to take stock of what we know. First, there is no question acupuncture is a mechanical operation. In fMRI, the needling sends a message indicating the muscle has been touched or punctured. Second, the mechanistic signaling can be represented by an acoustic shear wave mathematically. Such a model can represent both the verum and sham acupuncture in action with the tissues in the body forming the wave guiding networks. The propagation of the acoustic wave was observed using the magnetic resonance elastrography for both acupoint and non-acupoint (sham). The difference between the two was seen mainly through the acoustic energy coupling when the needle interacted with the muscle tissues at different positions. Third, both verum and sham acupuncture can be effective, but verum response is always better. Fourth, calcium ion channel appears to be the central cellular response presenting a complex picture of latency, oscillation, amplitude and frequency modulation and memory effects. Fifth, the secretion of endogenous opioid is demonstrated by in vivo beta-endorphin enhancement in blood plasma, which is blocked by Gd3+. Sixth, it is not addictive and there are no side effects.
In understanding of pain and analgesia, the peripheral mechanism is of special interest for their shared physiological effects with acupuncture [34–37]. Stein reported that beta-endorphin has produced strong analgesic effect in animals which was further demonstrated in the control of pain in peripheral tissues in humans. The generation and inhibition of pain is local and its focus is on events occurring in peripheral injured tissues. Evidence was shown that opioids acting outside of the central nervous system do not produce side effects in both animals and humans. The modulation of calcium channels seems to be the primary mechanism for the inhibitory effects of opioids on peripheral neurons [33]. The release of opioids from immunocytes is receptor-specific and calcium dependent. Direct consequence in relation to acupuncture is the necessity of increasing intracellular Ca2+ for opioid peptides secretion. Since acupuncture is capable of delivering the extra Ca2+, the release of opioid peptides through mechanical means appears to be consistent with the ion-channel studies reported. Stein’s model of peripheral has the added perspective that the endogenous opioid is not addictive and has no side effects. These are consistent with mechanical acupuncture model based on the acoustic shear wave activation and calcium signaling.
Qi and meridian are central to the acupuncture puzzle
In our search for the principle of acupuncture, we had first unknowingly dismissed qi and meridian as meaningless terms and the ancients have either through ignorance or deviousness purposely misled us. If accepted, we would have to throw away not only acupuncture but Chinese Medicine. By all accounts, the ancient Chinese were serious experimentalists. Otherwise, they could not have anticipated Western medicine in blood circulation and endocrinology in sex and pituitary hormones by 2 millennia [29, 39]. These ancient physiologists also recognized an inter-connecting system of distinctly neuromuscular character, the 12 jing jin in Huang Di Nei Jing Ling Shu in 1st century b.c., and this term is translated as nerve, muscle and tendon [29]. Let us get back to meridians and qi.
The circulation system is a key reference for the search of the meaning of yin and yang, yin being the blood pumped through the heart and yang the qi in breathing of the lungs, better characterized respectively as the fluid and gas in the form of a mechanical wave. Because yin and yang are an integrated system, we may take blood as the pulsating fluid that is visible and the gas invisible. Now, let us remove breathing for a moment. With the blood flow in earnest, a mechanical wave is emanating from the blood vessels as the invisible qi. This mechanical wave, being the same as acoustic shear wave will have to travel through its preferred paths by means of wave guiding principle. Thus, the meridians are just the physical waveguides that were worked out by the ancient Chinese experimentally. With this interpretation, the circulation system produces both yin and yang. And acupuncture, although externally applied, is based on these forces. In other words, the ancient Chinese model of acupuncture is mechanistic in nature. To complete the circulation, the qi represents not just the mechanical or acoustic wave but also the activation process of calcium and secretion of endorphin. It now appears that the ancient Chinese writer in Huang Di Nei Jing did not use nerves with a good reason. These were the physicians who knew blood circulation and endocrinology. After hundreds of years of experiments, they came to take meridians seriously. Putting it differently, it appears they might know the phenomenon precisely but lacked the scientific and technical terms to explain it. In this interpretation, it is clear that the acupuncture system is not the same as the nervous system. It may use the neurons in signaling. But by and large, acupuncture makes use of independent signaling paths of which our ancestors named jin-luo or meridians.
We may now take a highly speculative reconsideration of ancient Chinese medicine in the light of recent experimental evidence in molecular biology. The proposed acoustic signaling paths, jin-luo, while interacting with nerves, are distinctly and physically separated from the nervous system. This appears to be the missing “calcium” communication link proposed but not found in the frequency-encoded second messenger [2]. Ca2+ waves were observed by confocal microscopy in Xenopus laevis oocytes showing the possibility of encoded information in magnitude, frequency and spatial organization of changes in the cytosolic free Ca2+ [19, 20]. These complex molecular patterns were suggested as important for intracellular communication as the action potential in the central nervous system [14]. Spatial and temporal calcium sparks (pulse modulation) in heart muscle cells were observed [3] in microns and milliseconds. Based on the amplitude modulation of Ca2+ signaling in differential gene transcription in B lymphocytes [6], the AM and FM schemes of calcium signaling was proposed [1]. In the latest experiments, the time scale in latency, oscillation and memory is very slow, mostly in minutes [23] and could not have been related to the action potential [15]. Thus, the acoustic shear waves and calcium may be taken as the carrier of the biological modulation system, of which acupuncture has been implemented as the first application in clinical medicine. This newly proposed communication mechanism allows the peripheral nerve analgesia model to function locally without going through the CNS as observed by Stein and co-workers [34–37]. Returning to the interpretation of the ancient Chinese tradition, the two separate circulation systems of blood (yin) and waves (yang) have come full circle, interacting and mutually supportive as described in Huang Di Nei Jing. We are also returning to the Chinese concept of unity of the universe and the human body, symbolically, in making use of the de Broglie relationship—we are all particles and waves and we are all yin and yang.
Conclusion
A crucial difference between the present and past interpretations is to examine acupuncture as a mechanical activation and signaling process. With this change, it appears all the ancient Chinese concepts can be re-interpreted and harmonized with the latest finding in medical imaging, cell biology and physiology. In short, we do not have to throw away the 2,500 years clinical ideas while preserving modern judgment based on scientific method and technology. The initial action of acupuncture appears to be mechanical and not neural or electrical. In any case, the mechanistic function provides a model to explain acupuncture. It can be applied to traditional Chinese acupuncture, Korean or Japanese acupuncture, and sham acupuncture with its measured effectiveness consistent with the observation of the ancient medical establishment. Separated from the central nervous system, we speculate that the mechanism introduces a separate channel of cellular communications with calcium waves playing the role of the second messenger. The mechanical wave, the acoustic shear wave and the calcium wave turn out to have come from the same source, and these different forms of waves appear ideally suited to describe what the ancient Chinese called “qi”, the mysterious, invisible, untranslatable and unknowable ingredient of life.
Acknowledgements
We are indebted to Q.Y. Ma for his kind and unstinted support, Q.C.C. Chan and J.M. Liang for providing Figs. 2a and 3, respectively, and to D.K. Yang for editorial assistance.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Berridge MJ. The AM and FM of calcium signaling. Nature. 1997;386:759–760. doi: 10.1038/386759a0. [DOI] [PubMed] [Google Scholar]
- 2.Berridge MJ, Irvine RF. Inosital phosphates and cell signaling. Nature. 1989;341:197–205. doi: 10.1038/341197a0. [DOI] [PubMed] [Google Scholar]
- 3.Cheng H, Lederer WJ, Cannel MB. Calcium sparks: elementary events underlying excitation–contraction coupling in heart muscle. Science. 1993;262:740–744. doi: 10.1126/science.8235594. [DOI] [PubMed] [Google Scholar]
- 4.Cho ZH, et al. New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci U S A. 1998;95:2670–2673. doi: 10.1073/pnas.95.5.2670. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5.Diener HC, et al. Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomized controlled clinical trial. Lancet Neurol. 2006;5:310–316. doi: 10.1016/S1474-4422(06)70382-9. [DOI] [PubMed] [Google Scholar]
- 6.Dolmetsch RE, Lewis RS, Goodnow CC, Healy JI. Differential activation of transcription factors by calcium response amplitude and duration. Nature. 1997;386:855–858. doi: 10.1038/386855a0. [DOI] [PubMed] [Google Scholar]
- 7.Endres HG, et al. Acupuncture for the treatment of chronic knee and back pain. Dtsch Arztebl. 2007;104:A123–A130. [Google Scholar]
- 8.Endres HG, et al. Acupuncture for the treatment of chronic headaches. Dtsch Arztebl. 2007;104:A114–A122. [Google Scholar]
- 9.Ezzo J, et al. Acupuncture-point stimulation for chemotherapy-induced nausea and vomiting. J Clin Oncol. 2005;28:7188–7198. doi: 10.1200/JCO.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 10.Goldman N et al (2010) Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nat Neurosci. doi:10.1038/nn.2562 [DOI] [PMC free article] [PubMed]
- 11.Haake M, et al. German acupuncture trials (GERAC) for chronic low back pain. Arch Intern Med. 2007;167:1892–1898. doi: 10.1001/archinte.167.17.1892. [DOI] [PubMed] [Google Scholar]
- 12.Han JS, Ho YS. Global trends and performances of acupuncture research. Neruosci Biobehav Rev. 2011;35:680–687. doi: 10.1016/j.neubiorev.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Han JS, Terenius L. Neurochemical basis of acupuncture analgesia. Annu Rev Pharmacol Toxicol. 1982;22:91–104. doi: 10.1146/annurev.pa.22.040182.001205. [DOI] [PubMed] [Google Scholar]
- 14.Jaffe LF. Classes and mechanisms of calcium waves. Cell Calcium. 1993;14:736–745. doi: 10.1016/0143-4160(93)90099-R. [DOI] [PubMed] [Google Scholar]
- 15.Kandel ER, Schwartz J, Jessell T. Principles of neural science. 4. New York: Elsevier; 2000. [Google Scholar]
- 16.Kong J, et al. An fMRI study on the interaction and dissociation between expectation of pain relief and acupuncture treatment. NeuroImaging. 2009;47:1066–1076. doi: 10.1016/j.neuroimage.2009.05.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Langevin H, et al. Mechanical signaling through connective tissue: a mechanism for the therapeutic effect of acupuncture. FASEB J. 2001;15:2275–2282. doi: 10.1096/fj.01-0015hyp. [DOI] [PubMed] [Google Scholar]
- 18.Langevin H, et al. Tissue displacements during acupuncture using ultrasound elastography techniques. Ultrasound Med Biol. 2004;30:1173–1183. doi: 10.1016/j.ultrasmedbio.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 19.Lechleiter JD, Calpham DE. Molecular mechanisms of intracellular calcium excitability in X. laevis oocytes. Cell. 1992;69:283–294. doi: 10.1016/0092-8674(92)90409-6. [DOI] [PubMed] [Google Scholar]
- 20.Lechleiter J, et al. Spiral calcium wave propagation and annihilation in Xenopus laevis oocytes. Science. 1991;252:123–126. doi: 10.1126/science.2011747. [DOI] [PubMed] [Google Scholar]
- 21.Li G, Yang ES. An fMRI study of acupuncture-induced brain activation of aphasia stroke patients. Complement Ther Med. 2011;195:549–559. doi: 10.1016/j.ctim.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Li G, et al. visual cortical activations on fMRI upon stimulation of the vision-implicated acupoints. NeuroReport. 2003;14:669–673. doi: 10.1097/00001756-200304150-00002. [DOI] [PubMed] [Google Scholar]
- 23.Li G et al (2011) Physiology and cell biology of acupuncture observed in calcium signaling activated by acoustic shear wave. Pflugers Arch Euro J Physiol. doi:10.1007/s00424-011-0993-7 [DOI] [PMC free article] [PubMed]
- 24.Liang J (2010) Physiology of acupuncture—a study of mechanosensitive ion channels. PhD thesis, University of Hong Kong
- 25.Linde K, et al. Acupuncture for patients with migraine. JAMA. 2005;293:2118–2125. doi: 10.1001/jama.293.17.2118. [DOI] [PubMed] [Google Scholar]
- 26.Lu GD, Needham J. Celestial lancets: a history and rationale of acupuncture and moxibustion. Cambridge: Cambridge University Press; 1980. [Google Scholar]
- 27.Marx JL. Analgesia: how the body inhibits pain perception. Science. 1977;196:471. doi: 10.1126/science.195.4277.471. [DOI] [PubMed] [Google Scholar]
- 28.Mayer DJ, Price DD, Raffii A. Antagonism of acupuncture analgesia in man by the narcotic antagonist naloxine. Brain Res. 1977;121:368–372. doi: 10.1016/0006-8993(77)90161-5. [DOI] [PubMed] [Google Scholar]
- 29.Needham JL (1954–2000) Science and civilization in China, Vols. II, VI. Cambridge Univ. Press, Cambridge, UK
- 30.Pomeranz B, Chiu D. Naloxone blocks acupuncture analgesia and causes hyperalgesia: endorphin is implicated. Life Sci. 1976;19:1757–1762. doi: 10.1016/0024-3205(76)90084-9. [DOI] [PubMed] [Google Scholar]
- 31.Reston J (1971) Now, about my operation in Peking. The NY Times, July 26
- 32.Reston J. Deadline. New York: Random House; 1991. [Google Scholar]
- 33.Rittner HK, et al. Pain control by CXCR2 ligands through Ca2+-regulated release of opioid peptides from polymorphonuclear cells. FASEB J. 2006;20:2627–2629. doi: 10.1096/fj.06-6077fje. [DOI] [PubMed] [Google Scholar]
- 34.Stein C. The control of pain in peripheral tissue by opioids. N Engl J Med. 1995;332:1685–1690. doi: 10.1056/NEJM199506223322506. [DOI] [PubMed] [Google Scholar]
- 35.Stein C, Hassen AHS, Lehrberger K, Giefing J, Yassouridis A. Local analgesic effect of endogenous opioid peptides. Lancet. 1993;342:321–324. doi: 10.1016/0140-6736(93)91471-W. [DOI] [PubMed] [Google Scholar]
- 36.Stein C, Schafer M, Machelska H. Attacking pain at its source: new perspectives on opioids. Nat Med. 2003;9:1003–1008. doi: 10.1038/nm908. [DOI] [PubMed] [Google Scholar]
- 37.Stein C, et al. Peripheral mechanisms of pain and analgesia. Brain Res Rev. 2009;60:90–113. doi: 10.1016/j.brainresrev.2008.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stux G, Berman B, Pomeranz B. Basics of acupuncture. Berlin: Springer; 2003. [Google Scholar]
- 39.Temple R. The genius of China: 3,000 years of science, discovery and invention. New York: Simon and Schuster; 1986. [Google Scholar]
- 40.Walker EM, et al. Acupuncture versus Venlaaxine for the management of vasomotor symptoms in patients with hormone receptor-positive breast cancer: a randomized controlled trial. J Clin Oncol. 2010;28:634–640. doi: 10.1200/JCO.2009.23.5150. [DOI] [PubMed] [Google Scholar]
- 41.Witt C, et al. Acupuncture in patients with osteoarthristis of the knee: a randomized trial. Lancet. 2005;366:136–143. doi: 10.1016/S0140-6736(05)66871-7. [DOI] [PubMed] [Google Scholar]
- 42.Zhao ZQ. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol. 2008;85:355–375. doi: 10.1016/j.pneurobio.2008.05.004. [DOI] [PubMed] [Google Scholar]