Abstract
Platysma muscular bands are present during the aging period, generally starting in the second half of the fourth decade of life in both sexes. One or two bands along the anterior segment of the neck are the most frequent, with varied extensions and appearances. The literature records different techniques for solving the problem of platysma bands. All the methods involve submental incision, cutaneous dissection, and various tactics for eliminating the action of the platysma bands. This report aims to describe a procedure for deactivating these bands using a percutaneous approach that eliminates the need for submental, cutaneous incision and dissection. This technique involves the use of a steel wire loop that encircles the platysma band and is connected to a device known as the platysmotome through two puncture holes in the skin. Three to six sections along each band eliminate the platysma band, leaving no visible marks on the skin. This method is indicated as an isolated procedure for patients with visible platysma bands and no skin flaccidity, patients with recurring bands after face-lifting and no cervical skin flaccidity, patients who have bands with little cervical skin flaccidity but do not care to undergo face-lifting, and patients who undergo face-lifts for platysma bands that include closed platysmotomy and tightening of the platysma by lateral suture. The described technique is a method specifically designed for deactivation of the platysma bands that can be used both in isolation and in conjunction with face-lifting. Because this method avoids submental, cervical incision and dissection, it is a less invasive technique for “deleting” the bands, whether applied alone or in association with face-lifting. From May 2008 to November 2009 (19 months), 61 patients underwent surgery for the correction of platysma bands via percutaneous myotomy. Among them, the first 11 patients received postoperative follow-up evaluation ranging from 8 to 17 months.
Keywords: Closed platysma treatment, New platysma approach, Percutaneous platysma approach
The correction of platysma bands, whether isolated or in association with face-lifting, has received innumerable surgical refinements over recent decades. These include isolated or combined procedures to the skin, the platysma, the submucosal aponeurotic system (SMAS), and adipose deposits when present.
The literature reports a number of pioneers who have made excellent contributions to the improved appearance of the cervical region [1–10]. All these contributions involve submental incision and anterior, cutaneous, and cervical dissection to various degrees, with or without prior liposuction or liposuction performed at the time of surgery. Despite the many surgical refinements, frequent recurrence of platysma bands has been observed, within 1 year or even less postoperatively. Furthermore, problems of hematomas, seromas, and indurations have been described despite the use of suction drains.
This report describes a technique for platysma band sectioning with minimal trauma and no submental, cutaneous incisions, cervical skin dissection, or dead space. The technique uses a steel wire in the shape of a loop applied around the platysma band by way of two puncture holes made with a hypodermic needle. The ends of the steel wire are attached to a small instrument called the platysmotome. When the loop is pulled by way of a surgical maneuver, it cuts the platysma band before resurfacing. The myotomy is performed at three to six sites along each band depending on its length [11].
Anatomic Considerations
The skin of the neck is constantly submitted to stimuli throughout the day and even during sleep. It is virtually impossible to determine the number of times the skin and structures of the neck contract during a 24-h period. The appearance of the platysma bands in both sexes may be due to these factors as well as to genetics, age, neck length, thickness of skin and muscle, fat deposits, and lifestyle. In individuals with thin skin, the bands may become visible prematurely, which does not happen in cases of adipose necks, which hide the bands. Liposuction, in turn, may expose the bands, leaving them more apparent.
Currently, we do not have clear knowledge concerning the origins of platysma bands or their intensity, variations in shape and volume, asymmetries, or different lengths in the same person. The bands can extend from the lower border of the mandible to the hyoid or sternal furcula, whether symmetric or not.
Patients and Methods
From May 2008 to November 2009, 61 patients (2 men) ranging in age from 46 to 71 years (average, 58 years) underwent “closed correction” of platysma bands. Of these 61 patients, 20 received treatment only for platysma bands (isolated closed platysmotomy). Among these 20 patients, 8 presented with recurring platysma bands after conventional treatment. The remaining 41 patients underwent face-lifting in conjunction with closed platysmotomy, without submental incision or dissection, combined with lateral plication of the platysma. Among these 41 patients, 11 received follow-up evaluation for 8 to 17 months (average, 13 months).
The members of the first group that received treatment only for platysma bands (isolated closed platysmotomy) had one of the following indications: normal cervical skin without flaccidity, a prior face-lift with recurring platysma bands but no skin flaccidity, or visible platysma bands with minimal skin flaccidity and no desire to undergo face-lifting. The second group underwent face-lifting in conjunction with closed platysmotomy at the same time, with strong tightening and lateral plication of the platysma. In none of these cases was incision or dissection of the submental skin performed.
The cases that received the platysmotomy alone were treated as outpatients with local anesthesia. Those who underwent face-lifting (for flaccidity, flaccidity of the neck, submental fat, and platysma bands) in conjunction with a closed platysmotomy received general anesthesia with 24 h of hospitalization.
Platysmotome
The device we call the platysmotome is a tool we designed that allows us to execute a subcutaneous cut of an anatomic structure precisely without incisions or skin detachment. The tool consists of a solid shaft that passes through the interior of a metallic tube and turns inside it. A metal plate similar to a coin with a 1.5-mm hole in its center is attached to the metallic tube at one end by supports. The two ends of the wire that encircle the platysma band pass through this 1.5-mm tube. This “coin” rests on the skin.
Inside the metallic tube, the solid turning shaft has two holes at the end near the metal plate, to which the two free ends of the wire are tied. At the other end of the solid shaft, two butterfly-shaped wings are the support the surgeon uses to turn the shaft inside the tube with the strength of a lever.
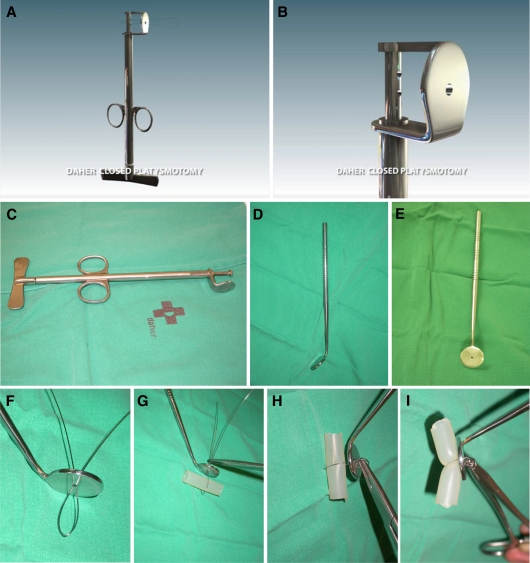
On the external body of the tube are two rings the surgeon uses to hold the platysmotome. While the shaft turns, the steel wire wraps around its tip, firmly and progressively tightening the loop that cuts the muscle (Figs. 1a–c, 2a–g).
Fig. 1.
(a–c) The platysmotome is a hollow metal cylinder with a solid cylinder inside that can be turned by a handle at the lower end. On the opposite end, a semicircular metal plate with a 1.5-mm hole in the center is attached to the cylinder, which envelops the turning rod. Two metal rings are attached to the external cylinder, by which the surgeon holds onto the device. Both ends of the wire, looped around the platysma band, are threaded through the central hole of the semicircular plate. They then are inserted separately through each hole in the solid cylinder and knotted. When the handle is turned, the wire loop is wrapped around the end of the movable rod, gradually pulling the loop, which cuts the muscle and then emerges from the skin. The simplified platysmotome (d, e) consists of a 2-cm-diameter metal plate with a central 1.5-mm hole soldered to a 12-cm rod at an angle of 140º (f, g). The two ends of the wire, after encircling the platysma band (represented in the figure by a tube of silicone), pass through the hole of the plate, which is resting against the patient’s skin. (h) The two ends of the wire are secured by a strong needleholder, which turns around itself. Its tail is a lever the surgeon uses to tighten it. The steel wire is wrapped around the end of the needleholder. (i) The loop is tightened around the muscular band, cutting it before surfacing through the point-like needle hole
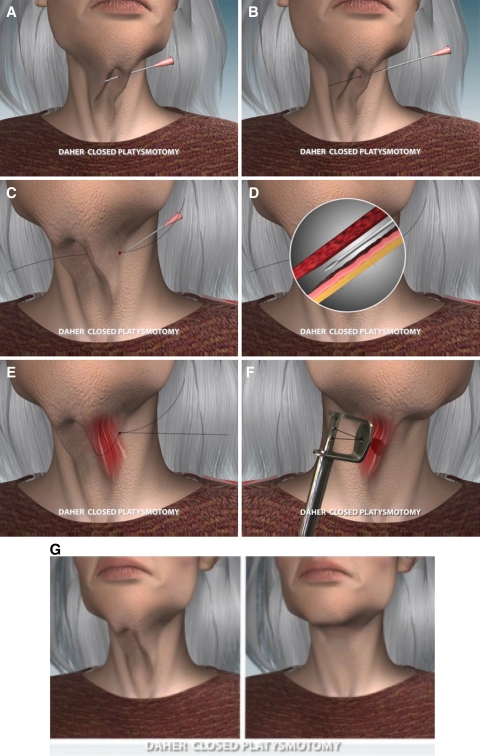
Fig. 2.
The platysma band myotomy proceeds through the following schematic steps: a The needle transfixes the skin and passes behind the platysma band before emerging from the skin on the opposite side. b, c The steel wire is threaded through the needle, emerging from the opposite end. The needle then is removed, leaving the wire in position. d The needle is reinserted through the first entrance point. By digital maneuvering, a space is created between the dermis and the space around the platysma band until the end of the needle exits from the opposite hole. e The steel wire is folded over itself to form a loop whose point is introduced at the end of the needle emerging from the opposite side. The wire encircles the band in a loop, with the two ends together and outside the first entrance hole of the skin. f The platysmotome plate, supported on the skin, receives the two steel wires, which pass through the central hole of the plate. The wires go through the respective smaller holes of the rod and are rolled around it, after which the excess wire is cut. The “butterfly” blades on the inferior end of the hollow cylinder are turned, which forces the loop to section the muscle and exit through the initial entrance hole. g Appearance of the neck before and after sectioning of the platysma band
The Simplified Platysmotome
We developed a second simpler and less expensive device that functions according to the same principle and, depending on the dexterity of the surgeon, allows the same objective to be reached: to pull on a subcutaneous loop that circles an anatomic structure, in this case the platysma band, to cut it without widening the access puncture holes or cutting the skin. This device consists of a 2-cm metallic circle with a central 1.5-mm hole soldered to a 12-cm shaft at a 140º angle.
After the two free ends of the loop are passed through the hole, the metallic plate is placed against the skin, and the wires are placed in a strong needleholder. We cut the excess wire and twist the needleholder, winding the steel wire around its tip. The tail of the needleholder serves as a lever that progressively tightens the loop. This cuts the underlying structure that it encircles, in this case the platysma band, before it surfaces (Fig. 1d–l).
Surgical Technique
The objective is to encircle the platysma band with the steel wire loop and tighten it until it cuts the band, maintaining the two access needle holes point-like after the surgery. The procedure is repeated three to six times on each band.
Demarcation is made with the patient awake, either seated or standing, for both isolated closed platysmotomy and platysmotomy in conjunction with a face-lifting procedure. With isolated platysmotomy, the surgery is performed using local anesthesia with or without sedation. Demarcation consists of three to six transverse lines 3 to 5 cm in length across each band. By way of a digital maneuver, the platysma band is secured with the muscle on its inside and transfixed by a hypodermic needle behind the muscle (40X × 12 (metric system), 18-G × 1.2 (inches) or even longer needle). A no. 5 steel wire is inserted through the needle at one end, which exits at the other end.
Next, the needle is removed, and the wire remains transfixed behind the band. The needle is reinserted through the same entrance hole and follows another path along a different plane, now between the platysma and the skin, exiting from the same skin hole on the opposite side. The end of the steel wire, together with the tip of the needle, is bent over itself, forming a loop that is reintroduced through the eye of the needle and exits through the opposite end. The needle then is removed, leaving the steel wire loop outside one of the holes and the two ends of the wire outside the other hole.
The steel wire loop is squeezed to reduce its diameter. When the two free ends of the steel wire on the opposite end are pulled, the loop submerges under the skin and encircles the muscular band. The two ends of the steel wire are threaded through the 1.5-mm hole of the circular metal plate on the platysmotome, which is resting on the skin of the neck. The same free ends of the wire are now threaded through the two holes of the metal turning shaft (inside the hollow cylinder) and tied together. The excess wire is cut with a pair of surgical wire-cutting pliers.
The surgeon holds the platysmotome in one of his or her hands by the rings on the external cylinder while the other hand twists the butterfly blades on the opposite end of the solid shaft. While the steel wire is turned around the solid shaft, the wire loop is tightened and cuts the band before it emerges from the entrance hole. The access routes through the skin (two needle holes for each muscular sectioning) remain point-like because the wires are kept together during the entire tightening process within the 1.5-mm hole of the metal plate. These point-like holes through the skin do not require sutures or bandages. The execution time for each cut is 1 to 3 min (Figs. 1a–i, 2a–g).
The cases depicted in Figs. 3a–r, 4a–b, 5a–h, 6a–d, 7a–f, 8a–f) illustrate the described technique and the results obtained from it. Patients who undergo face-lifting receive the same treatment for the platysma bands but under general anesthesia with 24 h of hospitalization.
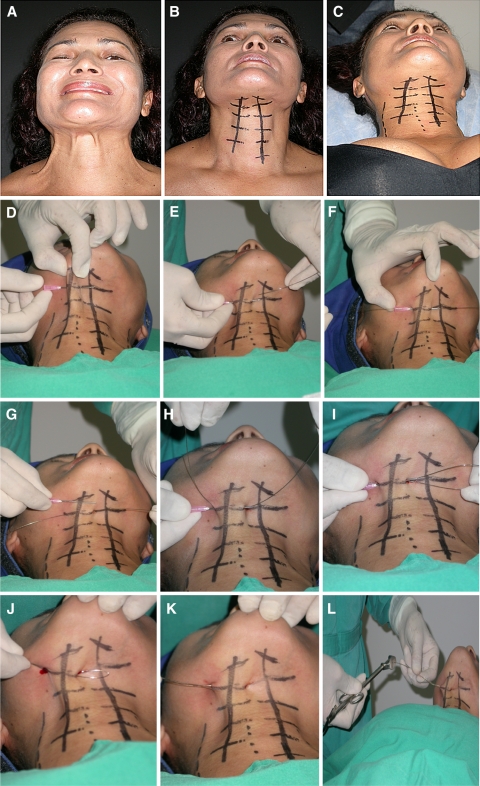
Fig. 3.
a Preoperative views of a 47-year-old Caucasian woman, with the platysma muscle contracted to provide a better view of the bands for skin demarcations. b, c Two longitudinal skin demarcations are made along the two bands. One side has five and the other side six transversal lines to indicate the number of myotomy sections to be performed. The outpatient surgery is performed with the patient under local anesthesia without preoperative medication. d–g The needle transfixes the skin behind the muscle band. The steel wire is threaded inside the needle tip and emerges from it, leaving the wire behind the muscular band and the two ends exposed. h–k The needle is removed and reinserted from the same skin entrance. It contours the muscular band and exits from the parallel skin puncture. The steel wire is again threaded through the needle to exit in the opposite direction, completing the loop around the muscular band. Light manual traction is applied to the wire to confirm that it has completed the loop around the band. l–n Both ends of the wire are inserted through the holes of the device and knotted. The excess is cut. o–q The device is placed gently against the skin with the wire ends protruding. When the handle of the platysmotome is turned, the metal loop cuts the muscle, and the wire emerges from the skin. It is important to realize that the circular plate, with the small center hole through which the two ends of the wire pass, is essential to keeping the wires held tightly together, preventing them from separating in the effort to cut the muscle, which could widen the puncture hole or cut the skin. Maintaining the puncture holes of the steel wire point-like is an indispensable condition of this technique because it guarantees rapid closure of the holes without scarring. r Final aspect of the neck. In this specific case, the central line of skin holes was used to treat both sides of the platysma bands. s, t An ice pack is applied for 15 min after surgery. u Final aspect of the neck skin after removal of the ice pack. v Another surgical option in which all the steel wires are previously transfixed to the specific sites on the platysma band
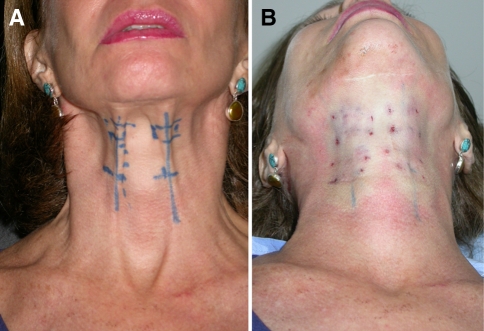
Fig. 4.
a Frontal, close-up, preoperative view of a neck with two long, separate platysma bands marked for the bands to be cut at four levels. b Immediately after the procedure performed to show the appearance of the skin, already described in the text. No face- or neck-lifts were performed for this patient
Fig. 5.
a, b Views before the operation and 1 week afterward showing a 57-year-old woman with a medial skin band based on possible platysma muscular fibers interlaced along the medial line. The two platysma bands were treated and eliminated through four myotomies on each side. Skin quality shows minimal trauma and rapid recovery. c–h Frontal and lateral views before the operation as well as 3 and 17 months afterward. No face- or neck-lift was performed. There is minimal evidence of the platysma bands, even in this case with excessively thin skin
Fig. 6.
a–d Left and right lateral views before the operation and 8 months afterward showing a 73-year-old woman who refused face-lifting in conjunction with a closed platysmotomy. Although the ideal indication for the case would have been face-lifting complemented by closed platysmotomy, we agreed to perform only the platysmotomy, considering the great hypertrophy of the bands, which the patient saw as a deformity. The patient underwent an isolated closed platysmotomy with five sections on the right and four on the left side. The outpatient surgery was performed with the patient under local anesthesia. No neck- or face-lift was performed
Fig. 7.
a–f Three-quarter and profile views before the operation as well as 3 and 16 months afterward showing a 45-year-old patient who underwent a face-lift and closed platysmotomy with three myotomies per side. There was no incision or detachment of the medial neck skin. The lateral detachment was moderate, and only lateral plication of the platysma was performed
Fig. 8.
a–f Lateral and profile views before the operation as well as 30 days and 15 months afterward showing a woman who underwent face-lift combined with closed platysmotomy. The two platysma bands were cut at four sites on each side. There was no submental skin incision or detachment
Postoperative Care
Cold compresses are used for approximately 15 min in the treatment of patients who undergo isolated closed platysmotomy. Occasional, minor hematomas, which recede within 1 or 2 weeks, may appear. In cases combined with face-lifting, routine care after this type of surgery is applied.
Discussion
The treatment of platysma bands is a constant challenge for surgeons performing rejuvenation surgeries in the cervical region. Many techniques for correction of platysma muscular bands have proved to be effective, with satisfactory long-term postoperative results [12–14]. After publications appeared regarding SMAS and the platysma [15], other invasive surgeries using lateral traction of the SMAS and platysma, with or without muscular sectioning and with or without muscular suturing along the cervical middle line, also were described. To date, all these techniques have included incision and dissection of the skin in the submental cervical region followed by different types of platysma sutures along the middle line, sometimes extending from the chin to the clavicular region.
We began the practice of performing the closed platysmotomy as an isolated outpatient procedure using local anesthesia without association with face-lifting. It was observed that after the platysma section lines had been marked on the skin and local infiltration (0.5–1 ml of lidocaine at 0.5% for each platysma section) had been performed, the bands disappeared completely, whether the patient was seated or standing, even when maneuvers to contract the bands were performed.
This observation was repeated for all the patients, allowing us to conclude that the bands do not originate from fibrosis or rigidity of the tissues or muscle, but rather from a strong muscular action of the platysma concentrated on the topography of the band. This, in turn, led us to deactivate the muscular action on the exact topography of the platysma bands by sectioning them in various points. Because the procedure is a noninvasive, closed, inexpensive process that can be performed on an outpatient basis, it was applied to a wide variety of patients.
It also was observed that deactivation of the platysma bands for patients with a great deal of skin flaccidity did not achieve the desired aesthetic objectives because the skin remained unchanged except in patients that had an excessively voluminous muscular band (Fig. 6a–d). It was concluded that isolated platysmotomy makes sense only when applied to patients with visible bands and no skin flaccidity, patients who had a previous face-lift and recurring bands but no skin flaccidity, and patients with evident bands and little skin flaccidity who do not want to undergo a face-lift. The results for cases with these criteria were very satisfactory, although less satisfactory the greater the skin flaccidity.
In 17 months, we did not have a single complete recurrence of any bands treated by surgery. In only one case did a small delineation of a previously treated band occur, although it was much less apparent than before surgery. On the other hand, poor results were verified for patients who received only one or two myotomies per band, which is why we began to perform three to six (3- to 5-cm-wide) sections on each band.
Some authors defend the idea that the aging process makes the anatomic structures on the various planes of the face go through a “descent” in a medial direction [13]. They recommend, therefore, that instead of suturing the platysma medially, it should be heavily pulled laterally and upward, going against the natural course the tissues follow during the aging process, bringing them back to their original position. Although this is not a widely divulged modern idea, it does exist and is followed by many. We believe this principle could have greater potential if in addition to strong lateral tightening of the platysma, the medial bands also were destroyed.
We began to use the closed platysmotomy in conjunction with face-lifting for patients with skin flaccidity and platysma bands associated with lateral traction of the platysma. The results were more effective in the medium- and long-term, with fewer risks, in addition to a shorter surgery time. This approach also is less invasive to the submental region, considerably diminishing the total area dissected during the face lift, which is consistent with current trends toward simpler rejuvenation procedures.
Even in the rare event of recurring platysma bands, which always appear much less evident than before sectioning, a second myotomy specific to the visible areas of the band is justified due to the rapid execution, low cost, and quick recovery of the procedure. The simplicity of a closed platysmotomy cannot be compared with the routine conventional treatment for recurring platysma bands after face-lifts, which requires both a greater surgical capacity and submental incisions and dissections, whether it is combined with other maneuvers or not.
We have not yet observed any relationship between myotomy of the platysma bands and ptosis of the salivary glands. However, we believe in the need for a careful, local, physical examination to register any previous indications of this situation and to advise the patient concerning the possibility of aggravating any tendency toward ptosis.
Attempts to “cut” the platysma bands with flexible threads, some designed especially for this purpose, have been made. The thread encircles the platysma band through the same process described earlier before performance of a back and forth movement, “sawing” of the platysma band [16]. We abandoned this idea after several attempts when we realized that the maneuver always made cuts with greater bleeding and that the “sawing” movement caused traumas to the wire exit holes, primarily when wider cuts (4 or 5 cm) were indicated, transforming the tiny point-like hole into a wider wound. These holes, when they are no longer point-like, lead to unattractive scarring, which is more visible.
Attempts to perform mini-incisions (2 to 3 mm) with a no. 11 blade or similar scalpel to create access to the platysma bands with miniature scissors always have led to unacceptable results because the scars, no matter how small, become undesirable, indelible marks in the cervical region. For the closed platysmotomy to be valid, the access ways must remain point-like (Table 1).
Table 1.
Patient data
| Case | Age (years) | Sex | Procedure | Postop months | Result |
|---|---|---|---|---|---|
| 1 | 74 | F | Only platysma | 8 | No recurrence |
| 2 | 72 | M | Face-lift + platysma | 13 | No recurrence |
| 3 | 44 | F | Only platysma | 13 | No recurrence |
| 4 | 41 | F | Only platysma | 14 | No recurrence |
| 5 | 36 | F | Only platysma | 15 | No recurrence |
| 6 | 36 | F | Only platysma | 15 | No recurrence |
| 7 | 52 | F | Face-lift + platysma | 15 | No recurrence |
| 8 | 45 | F | Face-lift + platysma | 16 | No recurrence |
| 9 | 58 | F | Only platysma | 16 | No recurrence (after face-lift 18 months earlier) |
| 10 | 42 | F | Only platysma | 16 | No recurrence |
| 11 | 49 | F | Only platysma | 17 | No recurrence |
Postop postoperative
The introduction of the platysmotome provides the following conditions. Because the wires pass through the 1.5-mm hole, they remain together during the whole process of pulling the loop, guaranteeing that the exit hole remains only the size of a pin prick. Furthermore, the steel loop, tightly pulled by the lever of the platysmotome, cuts the band by crushing it, producing the least amount of bleeding in virtually all the cuts. If bleeding of the veins occurs, it is easily stopped by simple bidigital compression for a few minutes, while the surgeon continues with the next cuts, avoiding loss of time. Only the no. 5 flexible steel wire (diameter, 0.5 mm) gives us an excellent response without breaking during the process. We have tried various other flexible threads but have been unable to find any other that can resist the strong lever tractioning.
In certain cases, immediately after the myotomies, small “steps” between the sectioned muscle segments were felt under palpation. This effect is not externally visible and normally disappears within the first week.
We did not have any complications other than the occasional occurrence of small ecchymoses. The patients did report any pain or discomfort. The absence of complications is easily understood because the procedure is performed in areas without any anatomic structures of greater importance. However, the following important structures, although outside the area of operation, are nearby and worthy of attention: (1) the anterior jugular vein, which is too deep to be reached by this method; (2) the external jugular vein, which although very far to the side of the area of operation, should be marked in advance to avoid the vein in cases that require wider cuts (5 cm); and (3) the mentonian nerve, a branch of the facial nerve that is more superficial along its distal path, which must be avoided when cuts are made to the bands in the suprahyoid region. Although we have not had any intercurrences, it is necessary to bear in mind its anatomy, which is marked by the presence of the facial artery, where it begins to become superficial.
Conclusions
The closed platysmotomy is a specific technique for treating platysma bands and deactivating their muscular action, whether used as an isolated procedure when appropriately indicated or in conjunction with face-lifting. In both situations, it presents good results with the advantage that it avoids scarring and submental dissection. It is a contribution to cases in which platysma bands have recurred after conventional face-lifting. It is the treatment of choice because in addition to the advantages previously mentioned, it avoids another surgery.
The platysmotome, both the original and the simplified model, has proved to be efficient in achieving the desired results. It permits the execution of multiple wide parallel band sections, deactivating the bands while preserving the point-like access ways created by the needle without widening them. This is indispensable for the rapid disappearance of the holes and the excellent results obtained. Because it is a low-cost, simple, outpatient intervention, it can be repeated in the event of recurrence. The results are very encouraging and also have an excellent cost–benefit ratio.
Acknowledgments
Conflicts of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Cronin TD, Biggs TM. The T-Z-plasty for the male “turkey gobbler” neck. Plast Reconstr Surg. 1971;47:534–538. doi: 10.1097/00006534-197106000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Guerrerosantos J, Spaillat L, Morales F. Muscular lift in cervical rhytidoplasty. Plast Reconstr Surg. 1974;54:127–131. [PubMed] [Google Scholar]
- 3.Connell BC. The value of platysma muscle flaps. Ann Plast Surg. 1978;1:34–43. doi: 10.1097/00000637-197801000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Aston SJ. Platysma muscle in rhytidectomy. Ann Plast Surg. 1979;3:529–539. doi: 10.1097/00000637-197912000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Aston SJ. Platysma-SMAS cervical rhytidectomy. Clin Plast Surg. 1983;10:507–520. [PubMed] [Google Scholar]
- 6.Vistnes LM, Souther J. The platysma muscle: anatomic considerations for aesthetic surgery of the anterior neck. Clin Plast Surg. 1983;66:441–448. [PubMed] [Google Scholar]
- 7.Biggs TM, Koplin L. Concepts of neck-lift. Clin Plast Surg. 1983;10:367–373. [PubMed] [Google Scholar]
- 8.McKinney P, Tresley EE. The “maxi-SMAS” management of the platysma bands in rhytidectomy. Plast Reconstr Surg. 1984;122:60–67. doi: 10.1097/00000637-198403000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Cardoso de Castro C. The value of the anatomical study of the platysma muscle in cervical lifting. Aesthetic Plast Surg. 1984;8:7–11. doi: 10.1007/BF01572778. [DOI] [PubMed] [Google Scholar]
- 10.Feldman JJ. Corset platysmoplasty. Plast Reconstr Surg. 1990;85:333–343. doi: 10.1097/00006534-199003000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Daher JC (2008) Personal communication: Closed platysmotomy: New procedure to treat platysma bands without skin dissection. 45th National Congress–Brazilian Society of Plastic Surgery, Brasilia, 12–15
- 12.Nahai F. Reconsidering neck suspension sutures. Aesthetic Surg J. 2004;24:365–367. doi: 10.1016/j.asj.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Nahai F, Nahai FR, food DT. Applied anatomy of the face and neck in facial plastic surgery. In: Nahai F, editor. The art of aesthetic surgery: principles and technique. 1. St.Louis, MO: Quality Medical Publishing; 2005. pp. 828–986. [Google Scholar]
- 14.Fogli A. Skin and platysma muscle anchoring. Aesthetic Plast Surg. 2008;32:531–541. doi: 10.1007/s00266-007-9111-9. [DOI] [PubMed] [Google Scholar]
- 15.Mitz V, Peyronie M. The superficial muscle aponeurotic system (SMAS) in the parotid and check area. Plast Reconstr Surg. 1976;58:80–88. doi: 10.1097/00006534-197607000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Fournier PF, Carrera C. Closed section of anterior platysma ribbons under local anesthesia. Rev Chir Esthetic. 2005;131:29–40. [Google Scholar]