Abstract
Limited data are available about the incidence of hypertension over the 5-yr in non-hypertensive subjects. The study subjects were 1,806 subjects enrolled in a rural area of Daegu, Korea for a cohort study from August to November 2003. Of them, 1,287 (71.3%) individuals had another examination 5 yr later. To estimate the incidence of hypertension, 730 non-hypertensive individuals (265 males; mean age = 56.6 ± 11.1 yr-old) at baseline examination were analyzed in this study. Hypertension was defined as either a new diagnosis of hypertension or self-reports of newly initiated antihypertensive treatment; prehypertension was if the systolic blood pressure was 120-139 mmHg and/or diastolic blood pressure was 80-89 mmHg. During the 5-yr follow-up, 195 (26.7%) non-hypertensive individuals developed incident hypertension. The age-adjusted 5-yr incidence rates of hypertension were 22.9% (95% confidence interval [CI] = 19.9-29.0) in overall subjects, 22.2% (95% CI = 17.2-27.2) in men, and 24.3% (95% CI = 20.4-28.2) in women. The incidence rates of hypertension significantly increased with age. In the multivariate analysis, prehypertension (Odds ratio [OR] 2.25; P < 0.001) and older age (OR 2.26; P = 0.010) were independent predictors for incident hypertension. In this rapidly aging society, population-based preventive approach to decrease blood pressure, particularly in subjects with prehypertension, is needed to reduce hypertension.
Keywords: Hypertension, Blood pressure, Incidence, Population
INTRODUCTION
Hypertension is now a major public health problem that affects approximately one billion individuals worldwide (1). It is widely acknowledged that blood pressure and the prevalence of hypertension increases with age in adults living in western societies (2, 3). Therefore, as the population ages, the prevalence of hypertension will increase even more. Hypertension is a major risk factor for coronary heart disease, heart failure, cerebrovascular disease and chronic renal failure (4-6). The high incidences of these diseases and the high prevalence of hypertension in most developed and developing countries make it the single most important cause of cardiovascular morbidity and mortality (7).
The prevalence of hypertension in various regions of the world has been widely reported (8-10). However, much less is known about the incidence of newly developed hypertension than about its prevalence (11-13). Asians comprise the largest ethnic group in the world and the fastest growing minority ethnic group within the United States (US) (14, 15). The prevalence of hypertension in most Asian groups is similar to that of non-Asians (10). Although numerous cross-sectional studies and cohort studies have provided important information on hypertension prevalence and incidence in various ethnic groups (8-13), only a few studies regarding the prevalence of hypertension have been conducted in Korea (16, 17). The previous studies were conducted more than 8 yr ago. Furthermore, previous studies were crosssectional studies, and the incidence of hypertension was not addressed. Accordingly, limited data is available about the incidences of hypertension in Korea. Therefore, the purpose of this study is to estimate the incidence of hypertension over 5 yr in non-hypertensive Koreans from the HYpertension-Diabetes Daegu Initiative (HYDDI) study.
MATERIALS AND METHODS
Study population
The HYDDI study is a community-based health survey conducted from August to November 2003 in a rural area, Dalseong-gun, in Daegu, Korea. The target population of the present study was the residents aged 20 yr and older living in rural area covered by community health primary health care posts (the basic healthcare unit in rural area) of the Dalseong-gun. According to the resident registration, 21,011 residents were eligible for screening. Two to four villages from the area covered by each primary health care post were randomly selected, totaling 26 villages (n = 2,680). Of the 2,680 candidate subjects, 1,806 subjects finally agreed to participate in this health survey including a complete medical history, anthropometric measurements, and the collection of fasting blood samples. All participants visited community health centers to take the examination. During the 5-yr follow-up, 518 subjects died or moved out from their previous residents and 1,287 (71.3%) individuals attended the 5-yr follow-up examination. At baseline examination, 1,034 subjects (57%) did not have hypertension. Of these non-hypertensive subjects, 730 (70.6%) had the 5-yr follow-up examination and finally included in this analysis.
Questionnaires survey, measurement of anthropometric, and laboratory parameters
The structured questionnaires covered the personal demographic data and medical history, and family history of chronic diseases. The frequency and duration of alcohol consumption and smoking habits, and the frequency of physical exercise were recorded. Alcohol consumption was classified as either a drinker, ex-drinker, or a non-drinker from the self-administered questionnaire. Smoking was classified as either current, ex- (not for at least 1 yr), or a non-smoker. Physical exercise was defined with the frequency of physical activity: none, 1-2 times per week, or 3 times or more per week. Anthropometric measurements including height, weight, waist circumferences, and hip circumferences were also measured by practitioners. Body weight was measured in light clothing, and height was measured in a standing position. Waist circumference was measured at the midpoint between the lower rib margin and the iliac crest. Body mass index (BMI) was calculated as weight divided by height squared (kg/m2). Blood sample was drawn in the state of at least 8 hr overnight fasting. The fasting plasma glucose and serum concentration of total cholesterol, triglyceride, and high-density lipoprotein cholesterol were measured by enzymatic methods using the Dimension AR system (Dade Behring, Inc., Deerfield, IL, USA).
Definition of hypertension
Systolic and diastolic blood pressures were measured in the sitting position using a sphygmomanometer after a 5-min rest. Two blood pressure readings were averaged, and it was used for analyses. According to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VII) criteria, hypertension was defined as systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, or current use of antihypertensive medication; prehypertension was if the systolic blood pressure was 120 to 139 mmHg and/or diastolic blood pressure was 80 to 89 mmHg; and normal was if the systolic blood pressure was < 120 mmHg and diastolic blood pressure was < 80 mmHg. Incident cases of hypertension were defined as either a new diagnosis or a self-report of a newly initiated antihypertensive treatment.
Statistical analyses
Data are expressed as the mean ± SD for continuous variables and as percentages for categorical variables. Comparisons between the baseline variables were made with the Student's t-test for continuous variables and the Pearson's chi-square test for categorical variables. The incidence of hypertension (per 100 persons) was calculated as the number of subjects who developed hypertension during the follow-up divided by the total number of those at risk at the baseline. The age-adjusted incidence rates of hypertension for each of the blood pressure groups were determined via the direct adjustment standardization method. National Census data in 2005 from the Korea National Statistical Office was used to determine the standards for the Korean population. Logistic regression analysis was used to calculate the relative risk for prehypertension associated with the development of hypertension. For all analyses, a two-sided P < 0.05 was considered statistically significant. Statistical analysis was performed using SAS software, version 9.1.
Ethics statement
This study protocol was approved by the institutional review board of the Kyungpook National University Hospital (No. 74005-1541). Written informed consent was obtained from all participants.
RESULTS
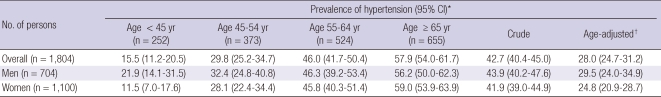
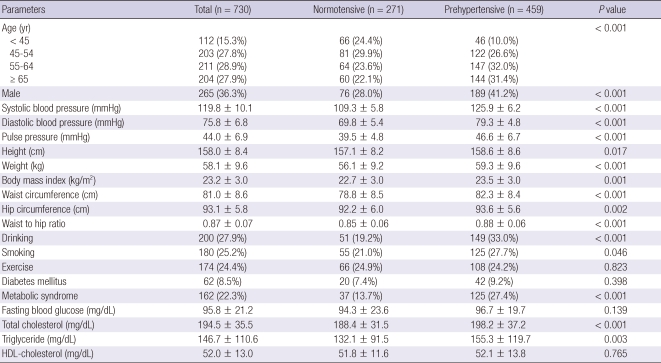
According to JNC VII criteria, the crude prevalence of hypertension in subjects (n = 1,804, excluding two with missing data) who provided blood pressure data was 42.7% (43.9% in men and 41.9% in women) in 2003 (Table 1). The age-adjusted prevalence of hypertension was 28.0% (29.5% in men and 24.8% in women) in 2003. Baseline characteristics of 730 non-hypertensive subjects (265 males; mean age = 56.6 ± 11.1 yr-old) are shown in Table 2. The prehypertension was present in 35.7% (n = 459). Prehypertensive individuals were older, more likely to be male, and had higher systolic and diastolic blood pressure, higher body mass index and waist to hip ratio, and higher total cholesterol and triglyceride levels.
Table 1.
Prevalence of hypertension according to baseline blood pressure categories
*Rates are per 100 persons; †Age was adjusted using the direct standardization method based on the 2005 national census obtained from the Korea National Statistical Office.
Table 2.
Baseline characteristics of study subjects
Data are mean ± SD for continuous variables and percentages for categorical variables. HDL, high-density lipoprotein.
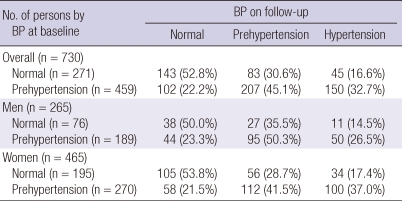
Table 3 shows the changes in blood pressure category of subjects during the follow-up according to their baseline blood pressure category. During the 5-yr follow-up, 195 (26.7%) non-hypertensive subjects developed hypertension, including 45 (16.6%) of subjects with normal blood pressure and 150 (32.7%) of subjects with prehypertension. There was no significant difference in the incidence rate of hypertension by gender (23.0% in men and 28.8% in women, P = 0.089).
Table 3.
The changes in blood pressure category on follow-up according to baseline blood pressure category
BP, blood pressure.
Progression to hypertension was determined on the basis of an increase in systolic blood pressure alone in 90 subjects (46.2%); diastolic blood pressure alone in 33 (16.9%); both systolic and diastolic blood pressure in 35 (17.9%); and on the basis of start of antihypertensive agents in 37 (19.0%).
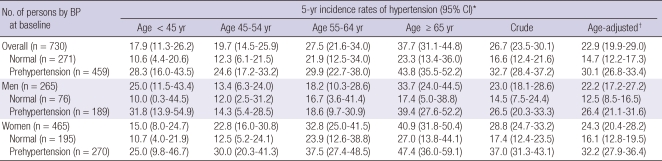
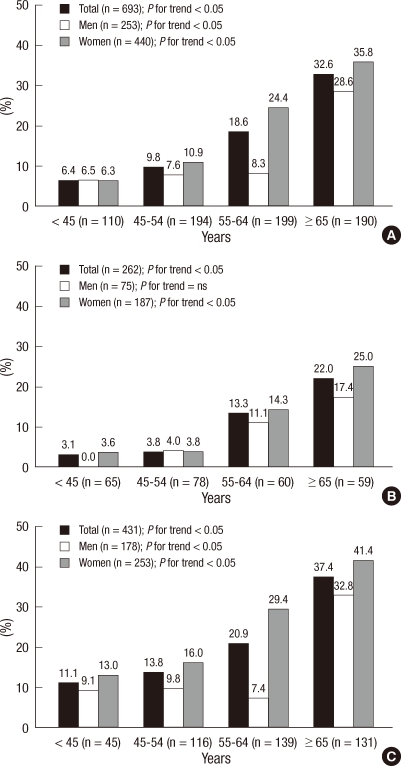
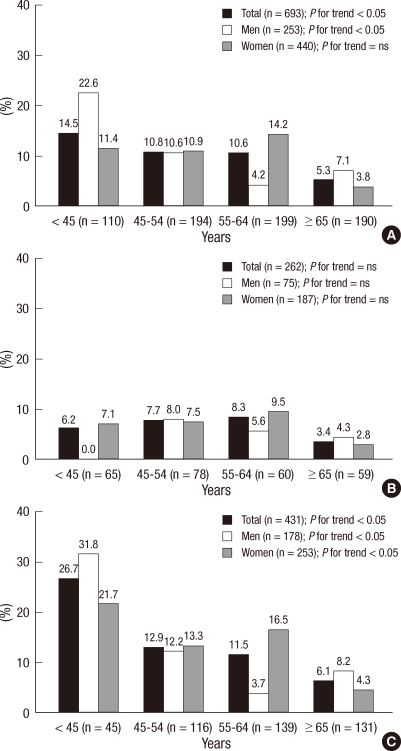
The crude 5-yr incidence of hypertension was 26.7% (95% confidence interval [CI], 23.5-30.1) in overall subjects, 23.0% (95% CI, 18.1-28.6) in men, and 28.8% (95% CI, 24.7-33.2) in women (Table 4). The age-adjusted 5-yr incidence of hypertension was 22.9% (95% CI, 19.9-29.0) in overall subjects, 22.2% (95% CI, 17.2-27.2) in men, and 24.3% (95% CI, 20.4-28.2) in women. The incidence rates of hypertension significantly increased with age (17.9% in the age of < 45 yr, 19.7% in 45-54 yr, 27.5% in 55-64 yr, and 37.7% in 65 or more years; P for trend < 0.001). The crude 5-yr incidence rates of hypertension in normotensive subjects were 16.6% (14.5% in men and 17.4% in women). The age-adjusted 5-yr incidence rates of hypertension in normotensive subjects were 14.7% (95% CI, 12.2-17.3) in overall subjects, 12.5% (95% CI, 8.5-16.5) in men, and 16.1% (95% CI, 12.8-19.5) in women. The crude 5-yr incidence rates of hypertension in prehypertensive subjects were 32.7% (26.5% in men and 37.0% in women). The age-adjusted 5-yr incidence rates were 30.1% (95% CI, 26.8-33.4) in overall subjects, 26.4% (95% CI, 21.1-31.6) in men, and 32.2% (95% CI, 27.9-36.4) in women. The incidence rate of systolic hypertension significantly increased with age (P for trend < 0.05) (Fig. 1), whereas the incidence rate of diastolic hypertension significantly decreased with age (P for trend < 0.05) (Fig. 2).
Table 4.
Five-year incidence rates of hypertension according to baseline blood pressure categories
*Rates are per 100 persons; †Age was adjusted using the direct standardization method based on the 2005 national census obtained from the Korea National Statistical Office. BP, blood pressure.
Fig. 1.
Incidence of systolic hypertension by age and gender in overall (A), normotensive (B), and prehypertensive subjects (C).
Fig. 2.
Incidence of diastolic hypertension by age and gender in overall (A), normotensive (B), and prehypertensive subjects (C).
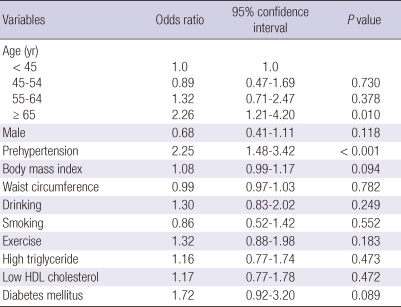
In multivariate logistic regression analysis, prehypertension (Odds ratio [OR] 2.25; 95% CI, 1.48-3.42, P < 0.001) and older age (OR 2.26; 95% CI, 1.21-4.20, P = 0.010) were independent predictors for incident hypertension after adjustment for sex, BMI, waist circumference, drinking, current smoking, exercise, high triglyceride levels, low high density lipoprotein cholesterol levels, and the presence of diabetes mellitus (Table 5).
Table 5.
Multivariate logistic regression analysis for incident hypertension
HDL, high-density lipoprotein.
DISCUSSION
In this community-based health survey in rural area of Korea, the age-adjusted prevalence of hypertension was 28.0% (29.5% in men and 24.8% in women) in 2003. The crude 5-yr incidence of hypertension was 26.7% (23.0% in men, and 28.8% in women) and the incidence of hypertension increased with age. Pre-hypertensive individuals were twice as likely to develop hypertension as the normotensive individuals.
In our study, the age-adjusted prevalence of hypertension is higher than 19.8% of year 1990, but similar to 28.6% of the Ansan study (year 1999-2000) (16, 17). In previous reports, the prevalence of hypertension tends to be higher in Western countries than in Asian countries although different study populations and different methodologies among surveys regarding the number of blood pressure measurements and the time interval between measurements may have contributed to observed differences (8-10). Over the past decade, the prevalence of hypertension has remained stable or decreased in developed countries, whereas it has shown a tendency to increase in developing countries (8). A significant downward trend in the prevalence of hypertension was observed in the US during 1960-1991 and Finland during 1982-1997 (18, 19). However, the third Chinese national hypertension survey reported that the prevalence of hypertension increased by approximately 25% during 1980-1991 (20). Furthermore, a recent study reported that there were no significant cross-sectional differences between developed and developing countries in hypertension indices (10). High economic development, changes in lifestyle and diet, and an increase in the prevalence of obesity, in part, may explain the rapid increase in the prevalence of hypertension in Korea. Another important factor is an increase in life expectancy in Korea over the past decade. According to the US International Population Reports, only 18 yr (2000-2018) will be required for percent of Korean population aged 65 and over to rise from 7 percent (aging society) to 14 percent (aged society) (21).
Several previous epidemiological studies have evaluated the incidence rates of hypertension in the community (11-13). However, information on the short-term rates of development of hypertension in non-hypertensive blood pressure categories is limited. The Framingham heart study has provided information on short-term incidence of hypertension according to JNC VI and the World Health Organization-International Study of Hypertension blood pressure categories (13). Although the Framingham heart study has been regarded as a representative US cohort study, there are some differences in the study period, the timeframe for follow-up, and the age distribution of the sample compared with the present study. The incidence of hypertension in the Framingham cohort increased with age and that the extent of this age-related increase depends on the initial value of blood pressure. Over a follow-up of 4 yr, 1,907 (19%) of 9,845 participants developed hypertension including 6% of subjects with optimal blood pressure, 20% of those with normal blood pressure, and 43% of subjects with high normal blood pressure. Hypertension incidence among participants in each of the three non-hypertensive categories increased with age. However, few studies have been conducted in Asia and cross-national comparisons of incidence rates of hypertension are still limited due to the differences in methodology. In a recent investigation, the crude 2-yr incidence of hypertension according to JNC VI criteria was 12.2% (13.0% in men and 11.6% in women) in middle-aged Korean adults (22). Unfortunately, however, comparison of incidence rate of hypertension among these studies is difficult, since the age-adjusted incidence rate was not reported in the previous studies. In the present study, the crude 5-yr incidence of hypertension was 26.7% (23.0% in men and 28.8% in women). When the annual probability of a progression to hypertension was calculated based on the assumption of the constant risks, the rate in the present study was 5.3%, which was higher than that in the Framingham heart study (4.8%) but was lower than that in middle-aged Korean adults (6.3%) (13, 22). Ratio of mortality from coronary heart disease in men aged 35-44 between Korea and the US has diminished substantially from 9 in 1985 to 2.4 in 1992 (23). The rapid increase in coronary heart disease mortality in Korea could be attributed, in part, to by the high incidence rates of hypertension.
In the present study, prehypertension in addition to old age (age > 65) were independent predictors for incident hypertension, as has been reported previously (13, 22, 24, 25). One of the potential reasons for high incidence of hypertension in prehypertensive individuals is that risk factors for hypertension (such as baseline age, higher body mass index, and higher total cholesterol levels) were more common in prehypertensive individuals (26). These findings support the recommendation of the JNC VII for prehypertensive individuals, lifestyle modification and multiple risk factor reduction, for the Asian prehypertensive individuals as well.
This study has several potential limitations. The first limitation is the variation in the blood pressure measurements. The present study was based on measurements taken during a single day. Incidence rates of hypertension among non-hypertensive individuals in the community are likely to vary depending on the variance of blood pressure measurements. Previous studies reported that the incidence rates of hypertension could be different due to repeated measurements on several occasions, instead of a single day of reading (27, 28). Accordingly, multiple measurements obtained on two or more occasions have been recommended for assessment of blood pressure status (1). However, most epidemiological studies have adopted the standardized methodologies based on measurements during a single day. Second, we were unable to exclude the possibility of selection bias. The loss to follow-up rate in this study exceeded 20%, a conventional standard beyond which the potential for bias increases if the pattern of missing subjects was not at random (29). Finally, the target population of the present study is confined to the residents in the rural area of Daegu City. As it is quite difficult to maintain a cohort in urban area, a rural area was selected for this cohort study. Therefore, our results could not be generalized.
In conclusion, this study provides the first information on the short-term incidence rates of hypertension according to JNC VII criteria from a cohort study of general population in a rural area of Korea, which is a representative developing country in Asia. In this rapidly aging society, population-based preventive approach to decrease blood pressure, particularly in subjects with prehypertension, is needed to reduce hypertension.
Footnotes
This study was published as an abstract in the ESC congress 2010, Stockholm, Sweden.
This study was partially supported by grant of Daegu metropolitan city.
AUTHOR SUMMARY
Incidence of Hypertension in Korea: 5-Year Follow-up Study
Jang Hoon Lee, Dong Heon Yang, Hun Sik Park, Yongkeun Cho, Jae Eun Jun, Wee Hyun Park, Byung Yeol Chun, Ji-Yeon Shin, Dong Hoon Shin, Kyeong Soo Lee, Kee-Sik Kim, Kwon-Bae Kim, Young Jo Kim, Shung Chull Chae, and the HYpertension-Diabetes Daegu Initiative Study Investigators
One thousand two hundreds eighty-seven Koreans in a rural area were examined twice with 5-yr interval. After the 5-yr follow-up, 195 (26.7%) of the 730 non-hypertensive individuals developed incident hypertension. The age-adjusted 5-yr incidence of hypertension were 22.9% (22.2% in men, 24.3% in women). The incidence of hypertension significantly increased with age. In the multivariate analysis, prehypertension and older agewere independent predictors for incident hypertension.
References
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez BL, Labarthe DR, Huang B, Lopez-Gomez J. Rise of blood pressure with age: new evidence of population differences. Hypertension. 1994;24:779–785. doi: 10.1161/01.hyp.24.6.779. [DOI] [PubMed] [Google Scholar]
- 3.Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, Horan MJ, Labarthe D. Prevalence of hypertension in the US adult population: results from the third national health and nutrition examination survey, 1988-1991. Hypertension. 1995;25:305–313. doi: 10.1161/01.hyp.25.3.305. [DOI] [PubMed] [Google Scholar]
- 4.D'Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 5.Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Ford CE, Shulman NB, Stamler J. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334:13–18. doi: 10.1056/NEJM199601043340103. [DOI] [PubMed] [Google Scholar]
- 6.Stokes J, 3rd, Kannel WB, Wolf PA, D'Agostino RB, Cupples LA. Blood pressure as a risk factor for cardiovascular disease. The Framingham Study: 30 years of follow-up. Hypertension. 1989;13(5 Suppl):I13–I18. doi: 10.1161/01.hyp.13.5_suppl.i13. [DOI] [PubMed] [Google Scholar]
- 7.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 8.Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22:11–19. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 10.Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009;27:963–975. doi: 10.1097/hjh.0b013e3283282f65. [DOI] [PubMed] [Google Scholar]
- 11.Cornoni-Huntley J, LaCroix AZ, Havlik RJ. Race and sex differentials in the impact of hypertension in the United States. The National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Arch Intern Med. 1989;149:780–788. [PubMed] [Google Scholar]
- 12.Kannel WB, Garrison RJ, Dannenberg AL. Secular blood pressure trends in normotensive persons: the Framingham Study. Am Heart J. 1993;125:1154–1158. doi: 10.1016/0002-8703(93)90129-w. [DOI] [PubMed] [Google Scholar]
- 13.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–1686. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 14.Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat. World population prospects: the 2008 revision. New York: UN Secretariat; 2009. [Google Scholar]
- 15.Le CN. "Population Statistics & Demographics" Asian-Nation: The Landscape of Asian America. [accessed 16 June, 2010]. Available at http://www.asian-nation.org/population.shtml.
- 16.Kim JS, Jones DW, Kim SJ, Hong YP. Hypertension in Korea: a national survey. Am J Prev Med. 1994;10:200–204. [PubMed] [Google Scholar]
- 17.Jo I, Ahn Y, Lee J, Shin KR, Lee HK, Shin C. Prevalence, awareness, treatment, control and risk factors of hypertension in Korea: the Ansan study. J Hypertens. 2001;19:1523–1532. doi: 10.1097/00004872-200109000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Burt VL, Cutler JA, Higgins M, Horan MJ, Labarthe D, Whelton P, Brown C, Roccella EJ. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population: data from the health examination surveys, 1960 to 1991. Hypertension. 1995;26:60–69. doi: 10.1161/01.hyp.26.1.60. [DOI] [PubMed] [Google Scholar]
- 19.Kastarinen MJ, Salomaa VV, Vartiainen EA, Jousilahti PJ, Tuomilehto JO, Puska PM, Nissinen AM. Trends in blood pressure levels and control of hypertension in Finland from 1982 to 1997. J Hypertens. 1998;16:1379–1387. doi: 10.1097/00004872-199816090-00019. [DOI] [PubMed] [Google Scholar]
- 20.Wu X, Duan X, Gu D, Hao J, Tao S, Fan D. Prevalence of hypertension and its trends in Chinese populations. Int J Cardiol. 1995;52:39–44. doi: 10.1016/0167-5273(95)02443-z. [DOI] [PubMed] [Google Scholar]
- 21.Kinsella K, He W. U.S. Census Bureau, International Population Reports, P95/09-1, An Aging World: 2008. Washington DC: U.S.: Government Printing Office; 2009. [Google Scholar]
- 22.Kim J, Kim E, Yi H, Joo S, Shin K, Kim J, Kimm K, Shin C. Short-term incidence rate of hypertension in Korea middle-aged adults. J Hypertens. 2006;24:2177–2182. doi: 10.1097/01.hjh.0000249694.81241.7c. [DOI] [PubMed] [Google Scholar]
- 23.Sekikawa A, Kuller LH, Ueshima H, Park JE, Suh I, Jee SH, Lee HK, Pan WH. Coronary heart disease mortality trends in men in the post World War II birth cohorts aged 35-44 in Japan, South Korea and Taiwan compared with the United States. Int J Epidemiol. 1999;28:1044–1049. doi: 10.1093/ije/28.6.1044. [DOI] [PubMed] [Google Scholar]
- 24.Hong KS. Prehypertension. Korean Circ J. 2008;38:1–6. [Google Scholar]
- 25.Kim YM, Hong KS, Choi YH, Choi MG, Jeong JY, Lee JM, Kim DH. Rates and related factors of progression to hypertension among prehypertensive local residents aged 45 or over in Chuncheon City: Hallym Aging Study from a Community-Based Cross-Sectional Study. Korean Circ J. 2008;38:43–50. [Google Scholar]
- 26.Natali A, Muscelli E, Casolaro A, Nilsson P, Melander O, Lalic N, Ferrannini E, Petrie JR. Metabolic characteristics of prehypertension: role of classification criteria and gender. J Hypertens. 2009;27:2394–2402. doi: 10.1097/HJH.0b013e3283316c31. [DOI] [PubMed] [Google Scholar]
- 27.Perry HM, Jr, Miller JP. Difficulties in diagnosing hypertension: implications and alternatives. J Hypertens. 1992;10:887–896. [PubMed] [Google Scholar]
- 28.Weissfeld JL, Kuller LH. Methodologic evaluation of incidence rates for hypertension: calculated for Pittsburgh's MRFIT usual care men. J Chronic Dis. 1985;38:915–925. doi: 10.1016/0021-9681(85)90127-4. [DOI] [PubMed] [Google Scholar]
- 29.Kristman V, Manno M, Côté P. Loss to follow-up in cohort studies: how much is too much? Eur J Epidemiol. 2004;19:751–760. doi: 10.1023/b:ejep.0000036568.02655.f8. [DOI] [PubMed] [Google Scholar]