Abstract
Background: Recent studies have shown a strong positive association between individual BMI (in kg/m2) or overweight prevalence and socioeconomic status (SES) in low- and middle-income countries (LMICs). However, it is not clear whether this association is weakening or reversing over time.
Objective: With the use of nationally representative data collected at 2 time points in 37 LMICs, we compared the associations of SES with BMI and of SES with overweight between the earlier surveys and the later surveys.
Design: We conducted a cross-sectional analysis of nationally representative samples of 547,056 ever-married nonpregnant women aged 15–49 y: 208,570 women in the earlier round of surveys conducted between 1991 and 2003 and 338,486 women in the later round conducted between 1998 and 2008. We used linear and modified Poisson analyses with a country fixed effect to obtain a pooled estimate and a country-stratified analysis for country-specific estimates.
Results: In adjusted models, BMI was 2.32 units higher (95% CI: 2.23, 2.41 units) among women in the wealthiest quintile compared with women in the poorest quintile in the earlier surveys and was 3.00 units higher (95% CI: 2.92, 3.07 units) in the later surveys. The association between BMI and wealth was positive in 37 countries in the earlier round of surveys and in 36 countries in the later round. Patterns were similar for overweight prevalence.
Conclusion: The association between SES and BMI or overweight is positive in most LMICs and has not weakened over time. It appears that the burden of overweight is consistently greater among wealthier populations within LMICs.
INTRODUCTION
Increases in the prevalence of overweight and obesity in LMICs4 over the past decade are well documented (1). However, these average trends mask the remarkable variation in weight by SES within LMICs, and ignoring this is problematic from a public health policy and surveillance perspective (2). The most recent data from 54 LMICs show a strong positive association between SES and BMI and the prevalence of overweight in 52 countries (3). We examined the potential changes in the direction of the association between body weight and SES over time. If SES inequalities in weight are weakening over time, with the poor gaining weight rapidly and the rich gaining weight more slowly or not at all, it is likely that overweight and obesity are increasing among the low-SES groups in LMICs. Conversely, no change in the SES-BMI gradient or a sharpening of the gradient would suggest that the changes in social patterning that is hypothesized to occur along with socioeconomic and epidemiologic transitions have yet to occur in LMICs. Furthermore, we expect that changes in the social patterning of BMI will be particularly prominent in younger populations, who have had earlier exposure to changes in nutrition and health behavior. Whereas changes in the association between SES and weight have been examined in individual countries (4–7), studies that appear to show a weakening of the SES gradient do not use data that are nationally representative (7, 8). Using measured BMI (in kg/m2) collected at 2 time periods in representative surveys from 37 LMICs, we assessed trends in the association between individual SES and BMI and the risk of being overweight.
SUBJECTS AND METHODS
Data sources
The data for this study came from a DHS of women of reproductive age (15–49 y) conducted on 2 separate occasions in 37 countries between 1991 and 2008 (Table 1) (9). To select surveys for inclusion in the analysis, we identified the earliest and latest surveys from countries where ≥2 surveys had been fielded after 1990. The DHS is a household sample survey that measures indicators of population, health, and nutrition, with special emphasis on maternal and child health (10). The target population in most of these surveys was all women or ever-married women of reproductive age. Because of its coverage, comparability, and data quality, the DHS is an important data source for studying the health of populations across developing countries (11–13). The DHS uses extensive interviewer training, standardized measurement tools and techniques, an identical core questionnaire, and instrument pretesting to ensure standardization and comparability across diverse sites and time (www.measuredhs.com/pubs/pdf/DHSG4/Recode4DHS.pdf) (14). The DHS uses a multistage stratified design with probabilistic sampling, with each elementary unit having a defined probability of selection (15). Every survey was stratified by urban and rural status and by country-specific geographic or administrative regions. Detailed sampling plans are available from survey final reports at www.measuredhs.com/pubs/search/search_results.cfm?Type=5&srchTp=type&newSrch=1 (16). Response rates ranged from 86.9% (Bolivia, 1993) to 99.6% (Nepal, 1996) of households and from 91.5% (Mozambique, 1997) to 99.3% (Egypt, 1995) of women in the earlier surveys and from 88.4% (Colombia, 2004) to 99.7% (Rwanda, 2005) of households and from 89.1% (Guatemala, 1998) to 99.7% (Egypt, 2008) of women in the later surveys. The details of each survey—country, year, sample sizes, distribution of BMI, prevalence of overweight, percentage change in BMI, and the prevalence of overweight between surveys—are shown in Table 1. A summary of the sample age and the percentage of the sample living in urban areas and with no education, by country, is provided elsewhere (see Supplemental Table 1 under “Supplemental data” in the online issue). The study population and response rates for all surveys are summarized elsewhere (see Supplemental Table 2 under “Supplemental data” in the online issue).
TABLE 1.
Survey year, sample size, mean BMI, annual average percentage change in BMI, percentage overweight/obese, and average annual percentage change in overweight/obese among women in 37 low- to middle-income countries
| BMI | Overweight/obese | |||||||
| Country | Year survey started | No. of subjects | Mean | 95% CI1 | Average annual percentage change2 | Percentage3 | 95% CI1 | Average annual percentage change4 |
| Armenia | 2000 | 4272 | 25.8 | (16.2, 35.3) | 50.0 | (48.5, 51.5) | ||
| Armenia | 2005 | 4219 | 26.5 | (15.8, 37.1) | 0.5 | 55.2 | (53.6, 56.7) | 2.1 |
| Bangladesh | 1996 | 4045 | 18.9 | (13.3, 24.3) | 2.9 | (1.7, 4.0) | ||
| Bangladesh | 2007 | 10,106 | 20.9 | (13.5, 28.1) | 1.0 | 13.7 | (12.8, 14.7) | 34.0 |
| Benin | 1996 | 2300 | 21.1 | (15.0, 27.2) | 8.6 | (6.8, 10.4) | ||
| Benin | 2006 | 11,781 | 22.7 | (14.2, 31.2) | 0.8 | 19.8 | (18.9, 20.7) | 13.0 |
| Bolivia | 1993 | 2198 | 24.3 | (17.1, 31.5) | 33.7 | (31.6, 35.8) | ||
| Bolivia | 2008 | 10,466 | 26.9 | (17.3, 36.4) | 0.7 | 60.2 | (59.3, 61.2) | 5.3 |
| Burkina Faso | 1992 | 3429 | 21.3 | (14.9, 27.7) | 9.9 | (8.3, 11.4) | ||
| Burkina Faso | 2003 | 8673 | 20.9 | (14.1, 27.6) | −0.2 | 9.2 | (8.2, 10.2) | −0.6 |
| Cambodia | 2000 | 4703 | 20.8 | (15.0, 26.5) | 7.7 | (6.5, 9.0) | ||
| Cambodia | 2005 | 5328 | 21.3 | (14.9, 27.5) | 0.5 | 12.1 | (10.9, 13.4) | 11.4 |
| Cameroon | 1998 | 1516 | 22.8 | (15.4, 30.2) | 22.8 | (20.3, 25.2) | ||
| Cameroon | 2004 | 3500 | 23.9 | (15.2, 32.4) | 0.8 | 31.1 | (29.5, 32.8) | 6.1 |
| Chad | 1996 | 3686 | 20.7 | (14.7, 26.5) | 7.0 | (5.6, 8.4) | ||
| Chad | 2004 | 2943 | 21.1 | (14.1, 28.0) | 0.3 | 10.7 | (9.0, 12.3) | 6.6 |
| Colombia | 1995 | 3026 | 24.5 | (16.6, 32.4) | 41.5 | (39.7, 43.3) | ||
| Colombia | 2004 | 23,190 | 25.7 | (16.3, 35.0) | 0.5 | 51.0 | (50.3, 51.6) | 2.6 |
| Cote d'Ivoire | 1994 | 2735 | 22.1 | (15.4, 28.7) | 14.8 | (13.0, 16.6) | ||
| Cote d'Ivoire | 1998 | 1726 | 23.5 | (14.6, 32.3) | 1.5 | 27.5 | (25.1, 29.8) | 21.4 |
| Egypt, Arab Republic | 1995 | 6777 | 26.0 | (15.9, 36.0) | 49.1 | (47.9, 50.3) | ||
| Egypt, Arab Republic | 2008 | 14,840 | 28.9 | (18.1, 39.5) | 0.8 | 76.0 | (75.2, 76.8) | 4.2 |
| Ethiopia | 2000 | 9990 | 20.0 | (14.4, 25.6) | 5.4 | (4.6, 6.2) | ||
| Ethiopia | 2005 | 4352 | 20.4 | (14.2, 26.6) | 0.4 | 6.6 | (5.3, 7.9) | 4.6 |
| Ghana | 1993 | 1735 | 21.8 | (14.7, 28.7) | 12.8 | (10.6, 15.0) | ||
| Ghana | 2008 | 2976 | 24.0 | (14.1, 33.8) | 0.7 | 33.1 | (31.3, 34.9) | 10.6 |
| Guatemala | 1995 | 4898 | 23.9 | (16.5, 31.2) | 31.0 | (29.6, 32.4) | ||
| Guatemala | 1998 | 2340 | 24.7 | (16.4, 32.9) | 1.2 | 39.9 | (37.8, 41.9) | 9.5 |
| Guinea | 1999 | 3273 | 21.8 | (15.0, 28.4) | 12.5 | (10.9, 14.1) | ||
| Guinea | 2005 | 2940 | 21.8 | (15.0, 28.5) | 0.1 | 14.7 | (13.0, 16.4) | 2.9 |
| Haiti | 1994 | 1891 | 21.2 | (14.4, 27.9) | 12.0 | (9.9, 14.1) | ||
| Haiti | 2005 | 3266 | 23.0 | (14.0, 31.8) | 0.7 | 25.7 | (24.0, 27.4) | 10.4 |
| India | 1998 | 77,593 | 20.6 | (13.0, 28.1) | 12.3 | (11.9, 12.6) | ||
| India | 2005 | 84,146 | 21.4 | (13.0, 29.8) | 0.6 | 18.6 | (18.3, 19.0) | 7.4 |
| Jordan | 1997 | 3082 | 27.3 | (16.4, 38.1) | 61.5 | (59.7, 63.3) | ||
| Jordan | 2007 | 4527 | 28.3 | (17.0, 39.6) | 0.4 | 69.6 | (68.1, 71.0) | 1.3 |
| Kazakhstan | 1995 | 2650 | 25.4 | (14.4, 36.3) | 44.3 | (42.4, 46.2) | ||
| Kazakhstan | 1999 | 1641 | 24.8 | (14.2, 35.3) | −0.6 | 38.7 | (36.3, 41.1) | −3.2 |
| Kenya | 1998 | 2929 | 22.0 | (14.6, 29.3) | 15.5 | (13.8, 17.3) | ||
| Kenya | 2008 | 5253 | 23.3 | (13.8, 32.8) | 0.6 | 29.5 | (28.2, 30.9) | 9.0 |
| Madagascar | 1997 | 2396 | 20.5 | (15.6, 25.2) | 4.5 | (2.9, 6.1) | ||
| Madagascar | 2008 | 6160 | 20.6 | (14.4, 26.7) | 0.1 | 7.9 | (6.8, 9.0) | 6.8 |
| Malawi | 1992 | 2268 | 21.8 | (15.8, 27.8) | 10.9 | (9.0, 12.8) | ||
| Malawi | 2004 | 7982 | 22.1 | (15.5, 28.6) | 0.1 | 14.2 | (13.2, 15.3) | 2.6 |
| Mali | 1995 | 4135 | 21.1 | (15.2, 26.9) | 8.8 | (7.4, 10.1) | ||
| Mali | 2006 | 10,832 | 22.5 | (14.2, 30.7) | 0.6 | 20.3 | (19.3, 21.2) | 12.0 |
| Morocco | 1992 | 2890 | 24.1 | (15.4, 32.6) | 32.7 | (30.9, 34.5) | ||
| Morocco | 2003 | 8997 | 25.5 | (16.2, 34.8) | 0.6 | 49.5 | (48.4, 50.5) | 4.7 |
| Mozambique | 1997 | 3079 | 21.7 | (15.8, 27.5) | 10.1 | (8.5, 11.7) | ||
| Mozambique | 2003 | 8543 | 22.4 | (15.1, 29.5) | 0.5 | 16.2 | (15.2, 17.2) | 10.1 |
| Namibia | 1992 | 1407 | 22.5 | (13.7, 31.3) | 20.9 | (18.3, 23.5) | ||
| Namibia | 2006 | 3815 | 24.7 | (12.8, 36.6) | 0.7 | 40.0 | (38.4, 41.6) | 6.5 |
| Nepal | 1996 | 3420 | 19.9 | (15.6, 24.2) | 1.8 | (0.7, 3.0) | ||
| Nepal | 2006 | 7975 | 20.7 | (14.6, 26.8) | 0.4 | 9.3 | (8.3, 10.3) | 40.4 |
| Nicaragua | 1997 | 9231 | 25.4 | (16.1, 34.6) | 46.6 | (45.6, 47.6) | ||
| Nicaragua | 2001 | 8856 | 26.2 | (16.3, 35.9) | 0.8 | 53.4 | (52.4, 54.5) | 3.6 |
| Niger | 1998 | 3410 | 21.0 | (14.4, 27.4) | 9.9 | (8.3, 11.4) | ||
| Niger | 2006 | 3280 | 22.2 | (13.9, 30.4) | 0.7 | 19.9 | (18.3, 21.6) | 12.7 |
| Nigeria | 2003 | 4592 | 22.7 | (13.8, 31.6) | 23.1 | (21.6, 24.5) | ||
| Nigeria | 2008 | 21,297 | 22.7 | (13.7, 31.7) | 0.0 | 23.4 | (22.7, 24.0) | 0.3 |
| Peru | 1991 | 4958 | 24.6 | (17.3, 31.8) | 38.0 | (36.6, 39.4) | ||
| Peru | 2003 | 17,620 | 26.4 | (17.8, 35.0) | 0.6 | 58.5 | (57.8, 59.2) | 4.5 |
| Rwanda | 2000 | 5598 | 22.3 | (16.2, 28.4) | 15.0 | (13.8, 16.3) | ||
| Rwanda | 2005 | 3039 | 22.0 | (16.1, 27.7) | −0.3 | 11.8 | (10.2, 13.5) | −4.2 |
| Tanzania | 1996 | 3535 | 21.9 | (15.4, 28.4) | 13.4 | (11.9, 15.0) | ||
| Tanzania | 2004 | 6733 | 22.5 | (14.6, 30.4) | 0.4 | 19.6 | (18.5, 20.8) | 5.8 |
| Turkey | 1993 | 2417 | 25.9 | (16.2, 35.5) | 51.1 | (49.1, 53.1) | ||
| Turkey | 2003 | 3030 | 26.6 | (16.5, 36.6) | 0.3 | 57.5 | (55.7, 59.3) | 1.3 |
| Uganda | 1995 | 3082 | 21.8 | (15.4, 28.0) | 11.1 | (9.5, 12.7) | ||
| Uganda | 2006 | 1878 | 22.1 | (14.5, 29.6) | 0.2 | 16.4 | (14.2, 18.6) | 4.4 |
| Zambia | 1996 | 3589 | 21.8 | (15.7, 27.8) | 11.9 | (10.4, 13.4) | ||
| Zambia | 2007 | 4450 | 22.8 | (14.7, 30.8) | 0.4 | 21.6 | (20.1, 23.0) | 7.4 |
| Zimbabwe | 1994 | 1835 | 23.0 | (15.6, 30.2) | 21.7 | (19.5, 24.0) | ||
| Zimbabwe | 2005 | 5786 | 23.5 | (15.0, 32.0) | 0.2 | 28.8 | (27.5, 30.1) | 3.0 |
Adjusted to account for design effects.
Represents the change in BMI divided by the mean BMI at time 1 divided by the number of years elapsed between the first and second surveys.
Calculated as the number of women with a BMI (in kg/m2) >25 divided by the total sample and multiplied by 100%.
Represents the change in overweight/obese divided by the percentage overweight/obese at time 1 divided by the number of years elapsed between the first and second surveys, multiplied by 100.
Study population and sample size
The study population included 991,327 women interviewed for the DHS in the 37 countries selected for analysis. Because some surveys only included anthropometric measurements for a subsample of women, height and weight were not measured for 237,170 women. Among those for whom height or weight should have been measured, 6,374 had no height or weight measurement included in the DHS, and an additional 1,148 women had biologically implausible height (<100 cm or >200 cm) or weight (<20 kg or >150 kg) data. An additional 59,169 women reported being pregnant and were excluded from the analysis, and 3011 reported ages <15 y or >45 y. Sixty-six respondents were missing data on covariates. Finally, many surveys excluded never-married women from their samples, particularly in the earlier round of the DHS. For this reason, 137,333 unmarried women were removed from the sample. The final analytic sample included 547,056 ever-married nonpregnant women, 208,570 of whom were interviewed and measured during the earlier round of surveys conducted in 37 countries between 1991 and 2003 and 338,486 of whom were from the later round conducted between 1998 and 2008. A flow diagram representing the generation of the sample for analysis is shown elsewhere (see Supplemental Figure 1 under “Supplemental data” in the online issue). The DHS data collection procedures were approved by the ORC Macro (Calverton, MD) Institutional Review Board and by the relevant body that approves research studies on human subjects in each country. Oral informed consent for the interview/survey was obtained from respondents by the interviewers. The study was reviewed by the Harvard School of Public Health Institutional Review Board and was considered exempt from full review because the study was based on an anonymous public use data set with no identifiable information on the survey participants.
Outcome measures
BMI was the primary outcome considered in this analysis. BMI was calculated as weight (in kg) divided by the square of height (in m). Trained investigators weighed each woman by using a solar-powered scale with an accuracy of ±100 g and measured each woman using an adjustable board calibrated (in mm) and theoretically accurate to 1 mm (14). We chose BMI as the primary outcome for this analysis because this measure more fully captures the spectrum of nutritional status, from under- to overnutrition, within the population. We also considered the proportion of participants overweight (BMI >25) as a secondary outcome to help elucidate the potential changes in chronic disease risk in these populations (17).
Independent variables
Age, education, household wealth, and place of residence were the key independent variables of interest. Education was specified as no education or incomplete primary education, completed primary education, or completed secondary education. For example, a woman with some secondary education, but who did not complete secondary, would have an educational level of “completed primary” by this categorization. We used the DHS wealth index to measure household wealth. This measure compares the wealth of respondents within countries and is calculated by developing z scores for each variable measuring a household's assets and utilities and conducting a factor analysis on these z scores. For each household, the values of the indicator variables were multiplied by the factor loadings and summed to produce a standardized household index value with a mean of 0 and a SD of 1. This standardized score was then divided into quintiles for each country (18–20). Place of residence was defined in terms of whether the household was located in a census-defined urban or rural area.
Analysis
In our analysis, we assessed the association between BMI and overweight and our primary measure of SES, household wealth quintile, after adjustment for respondent age, educational attainment, and urban or rural residence. Using nationally representative data conducted at 2 time points in 37 LMICs, we compared the associations of SES with BMI and of SES with overweight between the earlier surveys and the later surveys. To estimate the association between SES and mean BMI or risk of overweight, we used both time-specific pooled models with a country fixed effect and country- and time-specific analyses. To confirm that our results were robust to differences in the age distribution of the population across time periods and surveys, we used models stratified by country, time, and 5-y age group to measure the association between SES and BMI within each age group. We used a linear regression analysis with robust error variance that accounted for the multistage sampling design to model the association between the independent predictors and BMI. Because overweight was not a rare outcome (P < 10%) in many countries, ORs calculated by using a logistic regression analysis would not provide a reasonable estimate of the RR in the population. For this reason, we used a modified Poisson analysis with robust SEs to model the association between the independent variables and overweight as a binary outcome (21). All models were adjusted to account for the multistage sampling design used in the DHS. All analyses were performed by using Stata/MP 11.1 (22).
RESULTS
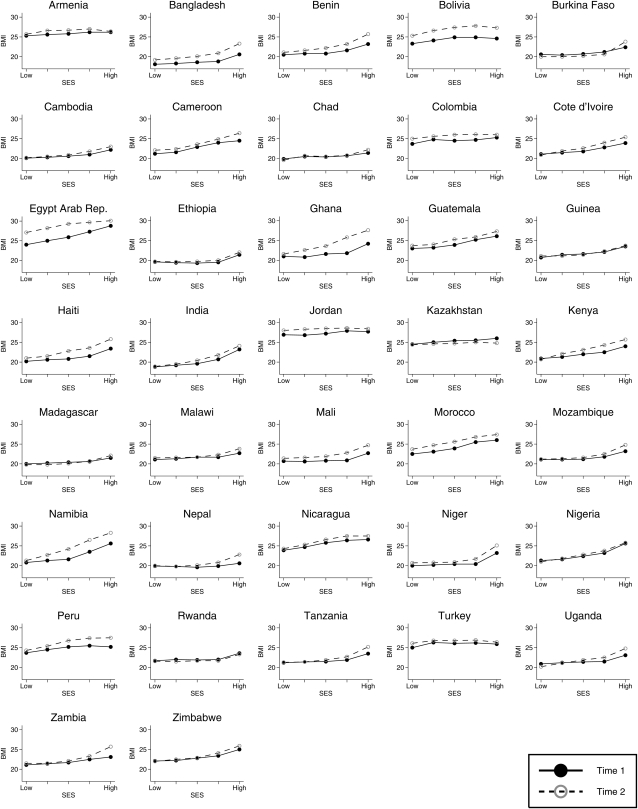
The mean BMI ranged from 18.9 (Bangladesh, 1996) to 27.3 (Jordan, 1997) in the earlier survey included in the analysis, and BMI increased between the earlier and later surveys in 34 of 37 countries (Table 1). The highest annual percentage change in BMI was in Cote d'Ivoire—an increase of 1.5 per year. In 3 countries, the mean BMI declined between the earlier and later surveys, although these declines were small (average annual decrease of 0.2 in Burkina Faso, 0.6 in Kazakhstan, and 0.3 in Rwanda). Similarly, the prevalence of overweight increased in 34 of 37 countries. In the pooled data, BMI and overweight were both positively associated with wealth in both time periods (Table 2). The distribution of BMI by wealth quintile for each country and time period, which indicates a general positive association between wealth and BMI, and the trend toward increasing BMI over time are shown in Figure 1.
TABLE 2.
Frequency distribution of the sample of women, mean BMI, and percentage overweight by independent variables across 37 low- and middle-income countries
| Frequency | BMI | Percentage overweight1 | ||||||||||
| Variables | Time 1 | Time 2 | Time 1: mean | Time 1: CI2 | Time 2: mean | Time 2: CI2 | Percentage change | Time 1: mean | Time 1: SD | Time 2: mean | Time 2: SD | Percentage change |
| Age | kg/m2 | kg/m2 | kg/m2 | kg/m2 | ||||||||
| 15–19 y | 15,222 | 19,151 | 20 | (14.7, 26.1) | 21 | (14.7, 27.3) | 2.8 | 6 | 5.6 | 9.6 | 8.7 | 62.6 |
| 20–24 y | 39,258 | 51,252 | 21 | (14.4, 27.6) | 22 | (14.3, 29.2) | 3.5 | 11 | 9.6 | 16.5 | 13.8 | 52.8 |
| 25–39 y | 45,504 | 64,029 | 22 | (13.9, 29.5) | 23 | (14.0, 31.3) | 4.6 | 17 | 13.9 | 24.8 | 18.7 | 48.7 |
| 30–34 y | 39,087 | 59,382 | 22 | (13.5, 30.9) | 23 | (13.8, 32.9) | 5.2 | 22 | 17.1 | 31.5 | 21.6 | 44.2 |
| 35–39 y | 32,076 | 55,665 | 23 | (13.2, 31.9) | 24 | (13.7, 34.1) | 6.1 | 25 | 18.6 | 36.5 | 23.2 | 47.4 |
| 40–44 y | 22,400 | 48,119 | 23 | (12.9, 32.3) | 24 | (13.6, 35.3) | 8.0 | 26 | 19.4 | 40.6 | 24.1 | 54.7 |
| 45–49 y | 15,023 | 40,888 | 23 | (12.6, 32.5) | 25 | (13.4, 36.1) | 9.7 | 26 | 19.5 | 42.8 | 24.5 | 61.4 |
| Education | ||||||||||||
| No education/incomplete primary | 131,770 | 186,746 | 21 | (13.7, 28.4) | 22 | (13.3, 31.3) | 5.9 | 12 | 10.7 | 21.8 | 17.0 | 79.0 |
| Completed primary | 47,610 | 97,350 | 23 | (13.8, 31.5) | 24 | (13.8, 33.8) | 5.2 | 25 | 18.6 | 34.7 | 22.7 | 41.0 |
| Completed secondary | 29,190 | 54,390 | 24 | (14.6, 33.8) | 26 | (15.8, 35.5) | 5.8 | 39 | 23.7 | 50.9 | 25.0 | 31.7 |
| Wealth quintile | ||||||||||||
| Lowest quintile | 39,801 | 60,995 | 21 | (13.8, 28.0) | 22 | (13.3, 30.3) | 4.3 | 11 | 9.8 | 18.3 | 14.9 | 66.0 |
| Second quintile | 39,228 | 65,283 | 21 | (13.6, 28.8) | 23 | (13.4, 31.6) | 6.1 | 13 | 11.5 | 23.7 | 18.1 | 79.6 |
| Third quintile | 41,156 | 68,747 | 21 | (13.4, 29.5) | 23 | (13.4, 32.7) | 7.5 | 15 | 13.1 | 28.0 | 20.2 | 81.0 |
| Fourth quintile | 42,955 | 69,934 | 22 | (13.5, 30.5) | 24 | (13.8, 33.5) | 7.6 | 19 | 15.7 | 33.4 | 22.2 | 71.2 |
| Highest quintile | 45,430 | 73,527 | 24 | (14.3, 32.8) | 25 | (14.9, 35.1) | 6.2 | 32 | 21.9 | 44.8 | 24.7 | 38.1 |
| Urban-rural | ||||||||||||
| Rural | 137,722 | 194,969 | 21 | (13.8, 28.1) | 22 | (13.5, 30.7) | 5.4 | 12 | 10.2 | 20.2 | 16.1 | 75.8 |
| Urban | 70,848 | 143,517 | 24 | (14.0, 33.1) | 25 | (14.5, 35.2) | 5.3 | 33 | 22.0 | 43.7 | 24.6 | 33.5 |
Calculated as the number of women with a BMI (in kg/m2) >25 divided by the total sample and multiplied by 100%.
Adjusted to account for design effects.
FIGURE 1.
BMI by wealth quintile in the earlier and later surveys. Rep., Republic; SES, socioeconomic status.
In adjusted models, BMI was 2.32 units higher (95% CI: 2.23, 2.41) among women in the wealthiest quintile than among women in the poorest quintile in the earlier surveys and was 3.00 units higher (95% CI: 2.93, 3.07) in the later surveys (Table 3). Coefficients on each wealth quintile compared with the lowest quintile were higher in the later surveys, which suggested that the association between wealth and body weight increased with time across all SES groups. Similar patterns were observed for overweight; the relative prevalence of overweight in the wealthiest group was 2.44 times (95% CI: 2.32, 2.57) that in the earlier surveys and 2.24 times (95% CI: 2.18, 2.29) that in the later surveys. The full results for both BMI and overweight models are shown elsewhere (see Supplemental Table 3 under “Supplemental data” in the online issue).
TABLE 3.
Mutually adjusted associations between wealth quintile and educational attainment and BMI or prevalence of overweight across 37 low- and middle-income countries1
| Adjusted mean (95% CI) | Adjusted RR (95% CI) | |||
| Variables | Time 1 | Time 2 | Time 1 | Time 2 |
| Education | ||||
| No education/primary (reference) | — | — | — | — |
| Secondary | 0.55 (0.50, 0.60) | 0.57 (0.53, 0.61) | 1.33 (1.30, 1.37) | 1.20 (1.18, 1.22) |
| Postsecondary | 0.82 (0.73, 0.92) | 0.11 (0.04, 0.17) | 1.26 (1.22, 1.31) | 1.01 (1.00, 1.03) |
| Wealth quintile | ||||
| Lowest quintile (reference) | — | — | — | — |
| Second quintile | 0.30 (0.25, 0.35) | 0.45 (0.41, 0.50) | 1.17 (1.13, 1.22) | 1.21 (1.18, 1.24) |
| Third quintile | 0.55 (0.50, 0.60) | 0.97 (0.92, 1.03) | 1.32 (1.27, 1.37) | 1.39 (1.35, 1.42) |
| Fourth quintile | 1.05 (0.99, 1.12) | 1.64 (1.59, 1.70) | 1.58 (1.52, 1.65) | 1.64 (1.60, 1.68) |
| Highest quintile | 2.32 (2.23, 2.41) | 3.00 (2.93, 3.07) | 2.44 (2.32, 2.57) | 2.24 (2.18, 2.29) |
| No. of observations | 208,570 | 338,486 | 208,570 | 338,486 |
Results also adjusted for age (5-y categories), urban-rural residence, and country. 95% CIs adjusted for design effect.
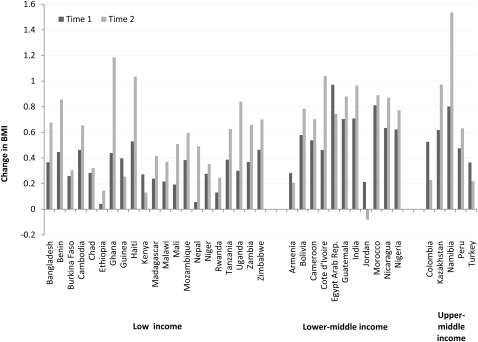
In the earlier and later surveys, the association between BMI and wealth was positive in 37 and 36 countries, respectively (Table 4). The largest positive association with BMI was in Egypt [increase of 0.97 (95% CI: 0.84, 1.11) for each unit difference in the wealth index] in the earlier survey group and in Namibia [increase of 1.54 (95% CI: 1.35, 1.72) for each unit increase in the wealth index] in the later survey. The association was smallest in Ethiopia in the earlier surveys (0.04; 95% CI: −0.01, 0.09) and was negative in Jordan (−0.08; 95% CI: −0.22, −0.06) in the later surveys. In 30 of 37 countries, an increase in the size of the association between wealth and BMI was observed; in the remaining 7 countries, the slope decreased across time points, although in most cases the 95% CIs for the 2 time points overlapped. The RR of overweight was positive in all countries in both the earlier and later surveys. The RR of overweight for an increase in the wealth quintile was highest in Bangladesh (ARR: 1.95; 95% CI: 1.49, 2.55) and lowest in Kenya (ARR: 1.03; 95% CI: 0.99, 1.07) in the earlier surveys. In the later surveys, the RR of overweight for an increase in the wealth quintile was highest in Bangladesh (ARR: 1.65; 95% CI: 1.55, 1.75) and was lowest in Jordan (ARR: 1.00; 95% CI: 0.98, 1.02). A comparison of the change in BMI associated with the change in SES for each country across time periods is shown in Figure 2.
TABLE 4.
Adjusted associations between wealth quintile and BMI or overweight/obesity in 37 low- and middle-income countries1
| Association between wealth quintile on BMI | Association between wealth quintile on overweight/obesity | |||||||||
| Year | Time 1 | Time 2 | Time 1 | Time 2 | ||||||
| Model | Time 1 | Time 2 | Adjusted marginal effect | 95% CI | Adjusted marginal effect | 95% CI | Adjusted RR | 95% CI | Adjusted RR | 95% CI |
| Pooled | — | — | 0.50 | (0.48, 0.52) | 0.70 | (0.68, 0.72) | 1.25 | (1.23, 1.26) | 1.22 | (1.21, 1.23) |
| Armenia | 2000 | 2005 | 0.28 | (0.14, 0.43) | 0.21 | (0.07, 0.35) | 1.07 | (1.04, 1.10) | 1.04 | (1.02, 1.07) |
| Bangladesh | 1996 | 2007 | 0.37 | (0.29, 0.45) | 0.68 | (0.61, 0.74) | 1.95 | (1.49, 2.55) | 1.65 | (1.55, 1.75) |
| Benin | 1996 | 2006 | 0.45 | (0.31, 0.59) | 0.86 | (0.78, 0.94) | 1.43 | (1.24, 1.65) | 1.48 | (1.42, 1.54) |
| Bolivia | 1993 | 2008 | 0.58 | (0.40, 0.76) | 0.79 | (0.66, 0.91) | 1.21 | (1.13, 1.29) | 1.10 | (1.08, 1.12) |
| Burkina Faso | 1992 | 2003 | 0.26 | (0.16, 0.36) | 0.31 | (0.22, 0.39) | 1.41 | (1.21, 1.63) | 1.50 | (1.35, 1.67) |
| Cambodia | 2000 | 2005 | 0.46 | (0.39, 0.54) | 0.65 | (0.58, 0.73) | 1.56 | (1.40, 1.73) | 1.66 | (1.55, 1.77) |
| Cameroon | 1998 | 2004 | 0.54 | (0.35, 0.72) | 0.70 | (0.54, 0.87) | 1.35 | (1.22, 1.51) | 1.24 | (1.17, 1.32) |
| Chad | 1996 | 2004 | 0.28 | (0.17, 0.40) | 0.32 | (0.20, 0.45) | 1.25 | (1.07, 1.45) | 1.28 | (1.11, 1.46) |
| Colombia | 1995 | 2004 | 0.53 | (0.36, 0.70) | 0.23 | (0.17, 0.29) | 1.11 | (1.06, 1.16) | 1.04 | (1.03, 1.05) |
| Cote d'Ivoire | 1994 | 1998 | 0.46 | (0.33, 0.59) | 1.04 | (0.79, 1.29) | 1.40 | (1.28, 1.53) | 1.52 | (1.36, 1.69) |
| Egypt, Arab Republic | 1995 | 2008 | 0.97 | (0.84, 1.11) | 0.74 | (0.65, 0.84) | 1.17 | (1.14, 1.20) | 1.08 | (1.07, 1.09) |
| Ethiopia | 2000 | 2005 | 0.04 | (−0.01, 0.09) | 0.15 | (0.07. 0.22) | 1.45 | (1.19, 1.77) | 1.15 | (0.98, 1.36) |
| Ghana | 1993 | 2008 | 0.44 | (0.28, 0.60) | 1.19 | (1.01, 1.36) | 1.38 | (1.19, 1.61) | 1.40 | (1.32, 1.49) |
| Guatemala | 1995 | 1998 | 0.70 | (0.58, 0.83) | 0.88 | (0.69, 1.08) | 1.30 | (1.24, 1.36) | 1.23 | (1.17, 1.29) |
| Guinea | 1999 | 2005 | 0.40 | (0.29, 0.50) | 0.26 | (0.13, 0.38) | 1.40 | (1.27, 1.55) | 1.27 | (1.15, 1.40) |
| Haiti | 1994 | 2005 | 0.53 | (0.35, 0.71) | 1.04 | (0.88, 1.19) | 1.57 | (1.32, 1.86) | 1.46 | (1.37,1.56) |
| India | 1998 | 2005 | 0.71 | (0.68, 0.74) | 0.97 | (0.93, 1.00) | 1.90 | (1.85, 1.96) | 1.74 | (1.70, 1.77) |
| Jordan | 1997 | 2007 | 0.21 | (0.06, 0.36) | −0.08 | (−0.22, 0.06) | 1.04 | (1.02, 1.06) | 1.00 | (0.98, 1.02) |
| Kazakhstan | 1995 | 1999 | 0.62 | (0.49, 0.74) | 0.97 | (0.85, 1.10) | 1.43 | (1.32, 1.55) | 1.38 | (1.31, 1.46) |
| Kenya | 1998 | 2008 | 0.27 | (0.07, 0.47) | 0.13 | (−0.19, 0.45) | 1.03 | (0.99, 1.07) | 1.05 | (0.97, 1.13) |
| Madagascar | 1997 | 2008 | 0.24 | (0.14, 0.33) | 0.42 | (0.33, 0.50) | 1.24 | (1.06, 1.46) | 1.66 | (1.48, 1.87) |
| Malawi | 1992 | 2004 | 0.22 | (0.12, 0.32) | 0.37 | (0.31, 0.44) | 1.22 | (1.10, 1.35) | 1.33 | (1.26, 1.40) |
| Mali | 1995 | 2006 | 0.19 | (0.10, 0.28) | 0.51 | (0.41, 0.61) | 1.31 | (1.17, 1.47) | 1.33 | (1.26, 1.40) |
| Morocco | 1992 | 2003 | 0.81 | (0.60, 1.02) | 0.89 | (0.76, 1.02) | 1.33 | (1.23, 1.43) | 1.17 | (1.14, 1.20) |
| Mozambique | 1997 | 2003 | 0.38 | (0.28, 0.49) | 0.60 | (0.52, 0.68) | 1.53 | (1.35, 1.72) | 1.51 | (1.42, 1.60) |
| Namibia | 1992 | 2006 | 0.80 | (0.56, 1.04) | 1.54 | (1.35,1.72) | 1.50 | (1.31, 1.71) | 1.38 | (1.32, 1.44) |
| Nepal | 1996 | 2006 | 0.06 | (−0.03, 0.14) | 0.49 | (0.40, 0.58) | 1.30 | (0.98, 1.71) | 1.82 | (1.65, 2.01) |
| Nicaragua | 1997 | 2001 | 0.63 | (0.53, 0.74) | 0.87 | (0.75, 1.00) | 1.14 | (1.11, 1.17) | 1.14 | (1.11,1.17) |
| Niger | 1998 | 2006 | 0.28 | (0.18, 0.37) | 0.35 | (0.22, 0.49) | 1.50 | (1.29, 1.73) | 1.43 | (1.27, 1.60) |
| Nigeria | 2003 | 2008 | 0.62 | (0.48, 0.76) | 0.77 | (0.69, 0.86) | 1.31 | (1.23, 1.40) | 1.35 | (1.30, 1.39) |
| Peru | 1991 | 2003 | 0.48 | (0.35, 0.60) | 0.63 | (0.54, 0.72) | 1.14 | (1.10, 1.19) | 1.11 | (1.09, 1.12) |
| Rwanda | 2000 | 2005 | 0.13 | (0.06, 0.20) | 0.25 | (0.16, 0.33) | 1.12 | (1.04, 1.19) | 1.34 | (1.24, 1.46) |
| Tanzania | 1996 | 2004 | 0.39 | (0.29, 0.49) | 0.63 | (0.53, 0.73) | 1.35 | (1.23, 1.48) | 1.49 | (1.40, 1.59) |
| Turkey | 1993 | 2003 | 0.37 | (0.18, 0.55) | 0.22 | (0.07, 0.37) | 1.08 | (1.04, 1.12) | 1.04 | (1.01, 1.07) |
| Uganda | 1995 | 2006 | 0.30 | (0.21, 0.39) | 0.84 | (0.69, 0.99) | 1.35 | (1.21, 1.50) | 1.57 | (1.41, 1.75) |
| Zambia | 1996 | 2007 | 0.37 | (0.27, 0.47) | 0.66 | (0.51, 0.81) | 1.28 | (1.16, 1.41) | 1.45 | (1.34, 1.57) |
| Zimbabwe | 1994 | 2005 | 0.46 | (0.30, 0.63) | 0.70 | (0.57, 0.83) | 1.27 | (1.14, 1.41) | 1.28 | (1.21, 1.35) |
Overweight/obese respondents were defined as those with a BMI (in kg/m2) >25. 95% CIs (in parentheses) adjusted to account for design effects.
FIGURE 2.
Change in BMI associated with a 1-unit change in wealth quintile in 2 time periods in 37 low- and middle-income countries by national income level. Income designations are based on World Bank income level classifications (23). Rep., Republic.
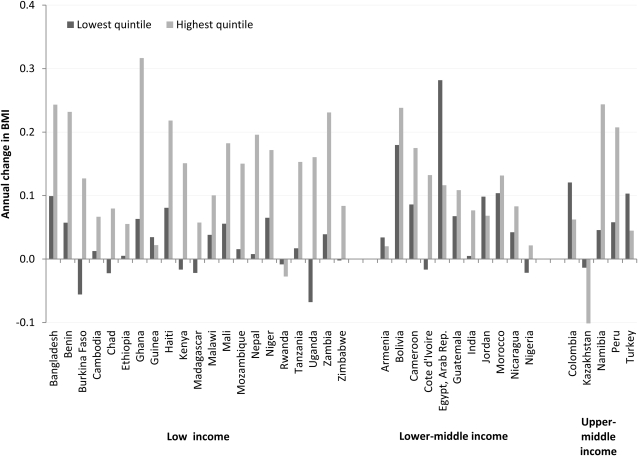
A summary of the average annual rate of change in BMI for respondents in the highest and lowest wealth quartiles is shown in Figure 3. It shows that, whereas BMI was increasing overall, poorer populations were not always seeing higher rates of increase than were wealthier populations. In 27 of 37 countries, BMI was increasing among both the wealthiest and the poorest respondents. Within these countries, 6 had a higher positive annual change in the poorest quintile than in the wealthiest. Eight countries showed a decrease in BMI among the poorest quintile and an increase among the wealthiest, whereas 2 showed a smaller decrease among the poorest than among the wealthiest.
FIGURE 3.
Estimated annual change in BMI among women in the lowest and highest wealth quintiles in 37 low- and middle-income countries by national income level. Income designations are based on World Bank income level classifications (23). Rep., Republic.
Finally, our examination of the changes in the association between wealth and BMI within each age group separately showed a pattern similar to that seen in the analysis of all women. Among women in the 20–24-y age group only, the SES-BMI association was positive in 36 of 37 countries in the earlier time period compared with 35 of 37 in the later period (see Supplemental Table 4 under “Supplemental data” in the online issue). Among this age group, the association was highest in Egypt in the earlier time period (increase in BMI of 0.69 for each unit increase in the wealth quintile; 95% CI: 0.45, 0.93) and in Namibia in the later surveys (increase in BMI of 1.00; 95% CI: 0.58, 1.42). The association was negative in Kazakhstan in the earlier surveys (change in BMI of −0.2; 95% CI: −0.5, 0.1) and in Armenia (change of −0.19; 95% CI: −0.48, −0.10) and Jordan (−0.40; 95% CI: −0.75, −0.05) in the later surveys.
DISCUSSION
A consistent and positive association exists between BMI and SES as measured by wealth in most LMICs. In 36 of 37 countries in the later time period, a positive association was found between SES, as measured by wealth, and BMI after adjustment for age, educational attainment, and urban or rural residence. In all countries, a positive association was found between SES and overweight. This association did not appear to attenuate over time. In all countries and time periods included in the analysis, the unadjusted mean BMI among the highest SES group was higher than the unadjusted mean BMI among the lowest SES group. Whereas our results showed some countries where BMI and overweight are increasing faster among poorer women after the covariates were accounted for, these increases were not large. Overall, these findings do not support a global shift in the direction of the association between SES and BMI in LMICs from positive to negative.
A recent study conducted by Jones-Smith et al (24) used an ecologic analysis of data on BMI and SES from developing countries and found that a lower SES was associated with increased weight gain in 10 of 37 countries. We believe that our results, which showed only 6 countries with accelerated weight gain in the poorer compared with the wealthier, are more robust for several reasons. Jones-Smith et al used data sets that are not nationally representative for 2 countries: Indonesia and China. They also failed to include eligible DHSs from India and Nigeria—2 of the most populous countries included in the DHS. For these reasons, their results may not be generalizable either within the countries included in the survey or globally. Moreover, because their analysis relied on aggregated data, their results are subject to ecologic fallacy, with their group-level results not necessarily applicable to individuals within the population. In contrast, our analysis included only data sets that are nationally representative and involved an individual-level analysis that allows for adjustment of results by age, educational attainment, and urban status and that does not collapse the primary unit of analysis into group prevalence. We believe that this analytic technique allowed us to more carefully assess the association between household-level SES and our outcomes of interest. In addition, the analysis included both measured BMI and overweight as outcomes, which allowed us to assess both the trends in body size over time and the changes in the prevalence of a chronic disease risk factor.
This study had several limitations. Because the surveys used in this analysis were conducted at different times across different countries, we were unable to estimate the change in BMI across all countries for the entire survey period. Although we attempted to account for the differences in the span of time included for each country by providing estimates of average annual change, care must be taken when interpreting trend results. In addition, the wealth index measure used as a proxy for SES was designed to be comparable across countries (20) but does not account for changes in national wealth over time. Because SES and body weight were measured simultaneously, the association between SES and weight should not be interpreted in causal terms. However, the motivation in this study was to describe the social patterning of weight rather than to ascertain causal effects. In addition, our analysis was restricted to women. Studies of the association between SES and body weight in men in developing countries have found mixed results (5, 25), and findings on the association between SES and weight among women cannot be generalized to men. However, reviews of the association between SES and body weight in high-income countries have found that the inverse association between SES and weight first appeared among women (22, 26), which suggested that it was unlikely that the positive gradient among women in LMICs was driven by sex differences in this association. Finally, a given BMI may confer a different risk of obesity-related diseases and mortality among certain populations, such as Asians (26, 27). Although this questions the relevance of a BMI cutoff as a measure of weight status, these cutoffs remain the most widely available measure for studying weight status in populations. Consequently, our findings that use BMI as an outcome, as opposed to the BMI cutoff, are more pertinent.
The strengths of this analysis included the number and variety of countries included in the analysis, the incorporation of multiple years of nationally representative data, and the use of wealth as the primary proxy for SES. Whereas previous analyses of trends in the association between SES and weight have focused on a single country (4, 6–8, 18, 28), the results presented above incorporate multiple years of nationally representative data from a diverse array of LMICs. Thus, our results add to the literature a clearer sense of the variation in the SES-weight association across time and context. Wealth was chosen as the primary indicator of SES in this population, because it is more comparable across countries and because it reflects an individual's access to the material resources needed to obtain food. Although it has been hypothesized that a higher prevalence of overweight among women of higher SES is related to cultural norms favoring fatty body shapes (29), it is likely that SES is also associated with BMI through changes in food-consumption patterns (30). Moreover, food remains expensive in many developing countries, with the poorest remaining unable to afford to increase their energy intake (31).
In summary, our analysis of trends in BMI and SES in 37 LMICs found little evidence to support the contention that body weight increases disproportionately among poorer women. The association between BMI and wealth was positive in 37 countries in the earlier surveys and in 36 countries in the later surveys. Only 6 countries had a faster rate of change in BMI among the poorest than among the wealthiest. Whereas increasing BMI and the prevalence of overweight in a population is an important concern across developing and middle income countries, it appears that the burden of overweight will continue to be greater among wealthier populations in most countries.
Acknowledgments
The authors’ responsibilities were as follows—SVS: conceptualized the study, designed the analysis, and interpreted the results; MN and SVS: co-wrote the manuscript; JEF: led the data analysis and contributed to the interpretation and writing of the manuscript; and GDS: contributed to the conceptualization and interpretation of the results. None of the authors reported a conflict of interest.
Footnotes
Abbreviations used: ARR, adjusted RR; DHS, Demographic and Health Survey; LMIC, low- and middle-income country; SES, socioeconomic status.
REFERENCES
- 1.Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 2011;377:557–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Subramanian SV, Finlay JE, Neuman M. Global trends in body-mass index. Lancet 2011;377:1915–6 [DOI] [PubMed] [Google Scholar]
- 3.Subramanian SV, Perkins JM, Ozaltin E, Davey Smith G. Weight of nations: a socioeconomic analysis of women in low- to middle-income countries. Am J Clin Nutr 2011;93:413–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Subramanian SV, Davey Smith G. Patterns, distribution, and determinants of under- and overnutrition: a population-based study of women in India. Am J Clin Nutr 2006;84:633–40 [DOI] [PubMed] [Google Scholar]
- 5.Subramanian SV, Perkins JM, Khan KT. Do burdens of underweight and overweight coexist among lower socioeconomic groups in India? Am J Clin Nutr 2009;90:369–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dearth-Wesley T, Wang H, Popkin B. Under- and overnutrition dynamics in Chinese children and adults (1991–2004). Eur J Clin Nutr 2008;62:1302–7 [DOI] [PubMed] [Google Scholar]
- 7.Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: the China Health and Nutrition Survey—monitoring and understanding socio-economic and health changes in China, 1989-2011. Int J Epidemiol 2010;39:1435–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monteiro CA, Conde WL, Popkin BM. The burden of disease from undernutrition and overnutrition in countries undergoing rapid nutrition transition: a view from Brazil. Am J Public Health 2004;94:433–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.MEASURE DHS Demographic and health surveys. Calverton, MD: MEASURE DHS, 2010 [Google Scholar]
- 10.Rutstein SO, Rojas G. Guide to DHS statistics. Calverton, MD: ORC Macro, 2003 [Google Scholar]
- 11.Wirth ME, Delamonica E, Sacks E, Balk D, Storeygard A, Minujin A. Monitoring health equity in the MDGs: a practical guide. New York, NY: UNICEF/CIESIN; 2006 [Google Scholar]
- 12.Vaessen M. The potential of the Demographic and Health Surveys (DHS) for the evaluation and monitoring of maternal and child health indicators. : Khlat M, Demographic evaluation of health programs. Paris, France: CICRED/UNFPA, 1996 [Google Scholar]
- 13.Pullum T. An assessment of the quality of data on health and nutrition in the DHS Surveys, 1998-2003. Calverton, MD: Macro International Inc; 2008 [Google Scholar]
- 14.ORC Macro. Demographic and health survey interviewer's manual. Calverton, MD, 2006 [Google Scholar]
- 15.Macro International Inc Sampling manual. Calverton, MD: DHS-III Basic Documentation, 1996 [Google Scholar]
- 16.MEASURE DHS. Available from: http://www.measuredhs.com/pubs/search/search_results.cfm?Type=5&srchTp=type&newSrch=1 (cited 18 June 2011)
- 17.Expert Consultation WHO. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–63 [DOI] [PubMed] [Google Scholar]
- 18.Gwatkin DR, Rutstein SO, Johnson K, Pande R, Wagstaff A. Socioeconomic differences in health, nutrition, and population in India. Washington, DC: World Bank; 2000 [Google Scholar]
- 19.Rutstein SO. The DHS wealth index: approaches for rural and urban areas. Washington, DC:ORC Macro, 2008 [Google Scholar]
- 20.Rutstein SO, Johnson K. The DHS wealth index. DHS comparative report. Calverton, MD: Macro International Inc, 2004 [Google Scholar]
- 21.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–6 [DOI] [PubMed] [Google Scholar]
- 22.StataCorp Statistical software: release 10SE. College Station, TX: Stata Corporation, 2008 [Google Scholar]
- 23.World Bank Countries and economies. Available from: http://data.worldbank.org/country (cited 22 June 2011)
- 24.Jones-Smith JC, Gordon-Larsen P, Siddiqi A, Popkin BM. Cross-national comparisons of time trends in overweight inequality by socioeconomic status among women using repeated cross-sectional surveys from 37 developing countries, 1989-2007. Am J Epidemiol 2011;173:667–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McLaren L. Socioeconomic status and obesity. Epidemiol Rev 2007;29:29–48 [DOI] [PubMed] [Google Scholar]
- 26.Snehalatha C, Viswanathan V, Ramachandran A. Cutoff values for normal anthropometric variables in Asian Indian adults. Diabetes Care 2003;26:1380–4 [DOI] [PubMed] [Google Scholar]
- 27.Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, He J, Gupta PC, Ramadas K, Tsugane S, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med 2011;364:719–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fezeu L, Minkoulou E, Balkau B, Kengne AP, Awah P, Unwin N, Alberti GK, Mbanya JC. Association between socioeconomic status and adiposity in urban Cameroon. Int J Epidemiol 2006;35:105–11 [DOI] [PubMed] [Google Scholar]
- 29.Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull 1989;105:260–75 [DOI] [PubMed] [Google Scholar]
- 30.Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutr Rev 1997;55:31–43 [DOI] [PubMed] [Google Scholar]
- 31.Sen A. The rich get hungrier. New York Times 2008 May 28, A21, col. 0 [Google Scholar]