Abstract
Background: Dietary supplement use is extensive in US adults. Some reports suggested that supplement users had higher nutrient intakes from the diet than did nonusers, but to our knowledge this finding has not been examined in nationally representative survey data.
Objective: In this analysis, we examined mineral intakes from the diet by supplement-use categories and how these supplements contributed to meeting or exceeding Dietary Reference Intakes for selected minerals.
Design: Data from adults (≥19 y of age; n = 8860) who participated in NHANES 2003–2006, a nationally representative, cross-sectional survey, were examined. Supplement use was defined as the participant's self-reported use of a supplement that contained one or more selected minerals.
Results: Dietary intakes of minerals from food sources were higher for magnesium, copper, potassium, and selenium in male supplement users than in nonusers. For women, dietary intakes of minerals from food sources were higher for users than for nonusers for each mineral examined except for selenium. In women, users of calcium-containing dietary supplements were much more likely to meet the Estimated Average Requirement (EAR) than were nonusers. Even after consideration of supplement use, >14% of adults had inadequate intakes for calcium and magnesium on the basis of the percentage of adults with usual intakes less than the EAR. The prevalence of adults who exceeded the tolerable upper intake level (UL) for calcium, zinc, iron, and magnesium was higher in users than in nonusers.
Conclusions: Individuals who used mineral-containing dietary supplements had higher mineral intakes from food sources in the diet than did nonusers. For all minerals examined, and particularly for calcium and magnesium in men and women and iron in women, supplement use decreased the prevalence of intake inadequacy for each respective mineral; however, supplements contributed to risk of potentially excessive intakes for calcium, iron, zinc, and magnesium.
INTRODUCTION
Dietary supplement use is pervasive in the United States, with about one-half of adults and more than one-third of children and adolescents who have reported the use of dietary supplement (1, 2). In adults, it has been well documented that older adults consume more dietary supplements than do younger adults (1, 3, 4). Dietary supplement users also tend to be women (3, 5), less likely to smoke (6, 7), leaner (3, 5), and more physically active (3, 7) than are nonusers. Furthermore, dietary supplement users have higher levels of educational attainment and socioeconomic status than do nonusers (5, 8). Dietary habits of supplement users may also differ from those of nonusers; eg, supplement users have higher intakes of fruit and vegetables (3, 6) and drink more wine (5) than do nonusers.
Some (3, 9) but not all (10) reports suggested that adult users have higher intakes of nutrients from their diets than do nonusers. The prevalence of inadequate total micronutrient intakes (diet plus supplements) is lower in adults who use supplements than in adults who do not use supplements (9, 11, 12). However, total micronutrient intakes of users of supplements may be in excess of UL5 recommendations for certain nutrients because of the large amounts of nutrients contributed by dietary supplements (5). Very little is known about differences in mineral intakes of users and nonusers of supplements in nationally representative survey data (13). It is important for the development of public health policy to understand whether individuals who take dietary supplements have a need for them (eg, to avoid nutrient deficiencies) and whether dietary supplements can be used to meet nutrient requirements safely or if they contribute to risk of excess intakes and toxicity. Therefore, the purpose of this analysis was to examine mineral intakes from the diet and to determine how supplements contribute to meeting or exceeding the DRIs for selected minerals in the NHANES 2003–2006.
SUBJECTS AND METHODS
Study population
The NHANES is a nationally representative, cross-sectional survey of noninstitutionalized, civilian US residents (14). NHANES data are collected by the National Center for Health Statistics of the CDC. Written informed consent was obtained for all participants or proxies, and the survey protocol was approved by the Research Ethics Review Board at the National Center for Health Statistics. Data from NHANES 2003–2004 and 2005–2006 were combined for these analyses (14). The combined sample included 18,063 participants who had complete 24-h dietary intake data. Subjects <19 y of age (n = 7962) and pregnant and/or lactating women (n = 1241) were excluded, which left a final analytic sample of 8860 individuals.
Dietary intakes
Diet
NHANES participants were asked to complete an in-person household interview and a health examination in a mobile examination center that included an in-person 24-h dietary recall. A second 24-h dietary recall was collected via telephone ∼3–10 d after the mobile examination center exam. Both 24-h dietary recalls used the USDA's Automated Multiple-Pass Method (15, 16).
Dietary supplements
Information on dietary supplement use over the past 30 d was obtained as part of the dietary supplement questionnaire (17). Information included the participant's use of vitamins, minerals, herbs, and other dietary supplements. Detailed information, including the type, consumption frequency, duration of use, and amount taken, for each reported dietary supplement was obtained. The average daily intake of nutrients from dietary supplements was calculated for individuals by using the number of days supplement use was reported, the reported amount taken per day, and the serving size unit from the product label. Calcium from antacids was collected as part of the NHANES nonprescription drug questionnaire that participants self-completed at the home interview and was included in supplemental intake calculations.
Operational definitions
Nonusers of dietary supplements were defined as subjects who did not report the consumption of a dietary supplement within the past 30 d; thus, dietary intakes for nonusers were based on intakes from foods alone. Users of dietary supplements were defined as subjects who reported the consumption of a dietary supplement that contained a given mineral within the past 30 d. For example, a calcium user was someone who reported the use of calcium regardless of the source; therefore, the calcium could be from a multivitamin or mineral supplement, a calcium supplement (ie, single nutrient supplement), or an antacid that contained calcium. Dietary intakes (ie, from foods only) of users were compared with those of nonusers. Total mineral intakes were defined for dietary supplement users as mineral intakes from food sources plus mineral intakes from dietary supplements.
The prevalence of inadequate dietary intakes of a group was determined by using the EAR cutoff method for all minerals except iron (18). The probability method and the cutoff method are both approaches that require more than one 24-h dietary recall to adjust for individual variation. The EAR cutoff method assumes that there is no correlation between intakes and requirements, the variance in intakes is greater than the variance of requirements, and the distribution of requirements is symmetrical around the EAR. If these assumptions are met, as was the case for all nutrients examined in this study except iron, the number of individuals with usual intakes below the EAR is proportionate to the prevalence of the group with inadequate intakes. Because the distribution of requirements for iron was skewed (ie, not symmetrical), the cutoff method was not appropriate, and the probability method was applied (18). All analyses were kept at the group level, and interpretation of results were restricted to group-level differences.
Statistical analysis
The NCI method (19) was used to determine estimates of the usual nutrient intake from the diet for nonusers and users of dietary supplements. The usual total nutrient intake (from the diet and supplements combined) was also estimated for users of supplements with the NCI method. Covariates used in the NCI model were as follows: 1) the sequence of the 24-h recall, 2) the day of the week the 24-h recall was collected [dichotomized as weekend (Friday–Sunday) or weekday (Monday–Thursday)], and 3) dietary supplement use. Complete details of the NCI method are shown elsewhere (19), and the SAS macros (SAS, version 9; SAS Institute Inc) necessary to fit this model and to perform the estimation of usual intake distributions are available on the NCI website (20).
DRI age groups were used to compare estimates of mineral intakes to EARs for minerals with established EARs. Potassium does not have an established EAR, and thus, only mean estimates were presented. Because the distribution of requirements was skewed for iron, the probability method was used to determine the prevalence of the population below the EAR (21). The percentage of the population that exceeded the UL was also determined for each of the minerals with an established UL (21–23).
All statistical analyses were performed with SAS software (version 9; SAS Institute Inc). Sample weights were used to account for differential nonresponse and noncoverage and to adjust for the planned oversampling of some groups. Survey weights were also used to generate nationally representative estimates for the US population. We compared mean dietary intakes of minerals between users and nonusers of dietary supplements and the proportion that met the EAR and exceeded the UL by computing a z statistic, which yielded the same result as an unadjusted regression model (24). Significance was set at a Bonferroni-corrected P < 0.003 to ensure that the significance we showed was not due to chance.
RESULTS
Mean intakes by dietary supplement usage category
For men, dietary intakes from food sources of 4 minerals (magnesium, copper, potassium, and selenium) were higher in users than in nonusers of dietary supplements (Table 1). For minerals that did not differ by supplement use (calcium, iron, zinc, and phosphorus), total intakes (food plus supplements) were significantly higher in supplement users than in nonusers. Mineral-containing supplement use did not significantly increase mean phosphorus, potassium, and selenium intakes from intakes from diet alone. In women, dietary intakes of supplement users were significantly higher than those of nonusers for all of minerals examined with the exception of selenium. Phosphorus and potassium supplement use by women did not significantly increase total intakes over intakes from food alone.
TABLE 1.
Mineral intakes from food by subjects who did not use dietary supplements (Nonusers), mineral intakes from food by consumers of dietary supplements (Users-foods), and total mineral intakes (from food and dietary supplements) by consumers of dietary supplements (Users-total) in adults (≥19 y of age) in the United States, 2003–20061
| Men |
Women |
|||||
| Nonusers | Users-foods | Users-total | Nonusers | Users-foods | Users-total | |
| Calcium (mg) | 1005 ± 21a | 1058 ± 22a | 1319 ± 20b | 727 ± 12a | 843 ± 16b | 1331 ± 28c |
| n | 2777 | 1782 | — | 2192 | 2109 | — |
| Iron (mg) | 19.8 ± 0.5a | 18.5 ± 0.2a | 33 ± 1b | 13.0 ± 0.2a | 14.1 ± 0.3b | 27 ± 0.6c |
| n | 3752 | 807 | — | 3199 | 1102 | — |
| Magnesium (mg) | 268 ± 5a | 350 ± 5b | 449 ± 7c | 234 ± 4a | 267 ± 5b | 387 ± 10c |
| n | 1592 | 1459 | — | 3100 | 1459 | — |
| Zinc (mg) | 14.5 ± 0.2a | 15.0 ± 0.2a | 30 ± 0.5b | 12.1 ± 0.1a | 12.6 ± 0.1b | 26 ± 0.7c |
| n | 3190 | 1369 | — | 2756 | 1545 | — |
| Phosphorus (mg) | 1564 ± 19a | 1596 ± 27a,b | 1668 ± 28b | 1096 ± 13a | 1176 ± 21b | 1259 ± 21b |
| n | 3600 | 959 | — | 3317 | 984 | — |
| Copper (mg) | 1.6 ± 0.02a | 1.5 ± 0.02b | 3 ± 0.5c | 1.2 ± 0.02a | 1.1 ± 0.02b | 3.1 ± 0.1c |
| n | 3257 | 1782 | — | 3020 | 1281 | — |
| Potassium (mg) | 3047 ± 30a | 3247 ± 60b | 3338 ± 60b | 2245 ± 25a | 2530 ± 43b | 2618 ± 62b |
| n | 3381 | 1302 | — | 3208 | 1093 | — |
| Selenium (μg) | 129 ± 2a | 133 ± 2b | 184 ± 2b | 78 ± 2a | 84 ± 2a | 141 ± 3b |
| n | 3284 | 1275 | — | 3083 | 1218 | — |
All values are means ± SEs. Different sample sizes existed for each mineral because a user was categorized by the specific use of each mineral. Different superscript letters denote significant differences between categories of use from the diet and differences between dietary and total intakes by using a z statistic (Bonferroni-corrected P ≤ 0.003).
Dietary calcium intakes were significantly higher in supplement users than in nonusers across all age groups for women but not for men (see supplemental Table 1 under “Supplemental data” in the online issue for a presentation of mean dietary intakes by the DRI age and sex groupings of supplement users and nonusers). Magnesium intakes from the diet were significantly higher in male dietary supplement users than in nonusers at all ages but not in women.
Prevalence of inadequate intakes from food sources
In men, when food sources were considered alone, supplement users and nonusers differed only in the prevalence of inadequacy for magnesium and copper (Table 2). No differences between supplement users and nonusers were observed in the prevalence of inadequate intakes from food sources alone for calcium, iron, zinc, phosphorus, or selenium. The prevalence of inadequate iron, phosphorus, and selenium intakes from food sources was very low in men (ie, <0.5%). For all minerals except selenium, women who used dietary supplements had a significantly lower prevalence of inadequate mineral intakes from food sources than did nonusers (see supplemental Table 2 under “Supplemental data” in the online issue for a presentation of age-group differences in the prevalence of inadequate mineral intakes between supplement users and nonusers).
TABLE 2.
Prevalence of inadequate intakes assessed by using the EAR in adults (≥19 y of age) in the United States, 2003–20061
| Men |
Women |
|||||
| Nonusers | Users-foods | Users-total | Nonusers | Users-foods | Users-total | |
| Calcium | 36 ± 2a | 30 ± 2a | 14 ± 1b | 71 ± 2a | 61 ± 2b | 24 ± 2c |
| n | 2777 | 1782 | — | 2192 | 2109 | — |
| Iron | —2 | —2 | 0 ± 0 | 16 ± 1a | 13 ± 1b | 1 ± 0.02c |
| n | 3752 | 807 | — | 3199 | 1102 | — |
| Magnesium | 63 ± 2a | 53 ± 2b | 22 ± 1c | 69 ± 2a | 53 ± 2b | 19 ± 1c |
| n | 1592 | 1459 | — | 3100 | 1459 | — |
| Zinc | 10 ± 1a | 9 ± 1a | 0 ± 0b | 17 ± 2a | 10 ± 1b | 0 ± 0c |
| n | 3190 | 1369 | — | 2756 | 1545 | — |
| Phosphorus | 0.3 ± 0.1a | 0.1 ± 0.1a | 0 ± 0b | 4 ± 1a | 2 ± 0.5b | 0.7 ± 0.3b |
| n | 3600 | 959 | — | 3317 | 984 | — |
| Copper | 1.4 ± 0.3a | 0.3 ± 0.1b | 0 ± 0c | 10 ± 1a | 5 ± 1b | 0.2 ± 0.1c |
| n | 3257 | 1782 | — | 3020 | 1281 | — |
| Selenium | 0.1 ± 0a | 0.1 ± 0a | 0 ± 0a | 2.4 ± 0.6a | 1.2 ± 0.5a | 0 ± 0b |
| n | 3284 | 1782 | — | 3083 | 1218 | — |
All values are percentages ± SEs. Different sample sizes existed for each mineral because a user was categorized by the specific use of each mineral. Different superscript letters denote significant differences between categories of use from the diet and differences between dietary and total intakes by using a z statistic (Bonferroni-corrected P ≤ 0.003). EAR, Estimated Average Requirement.
Prevalence was <0.5%, and estimates were unstable because of large relative SEs.
Prevalence of inadequate total intakes (diet and supplements combined)
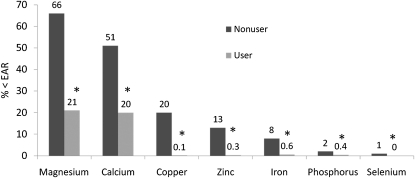
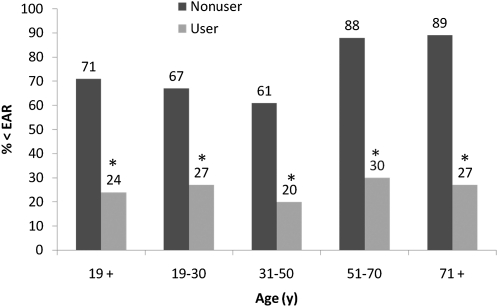
We examined mineral intakes from food sources alone in supplement nonusers and compared these diet-only intakes to total intakes (diet and supplements) of supplement users. As expected, dietary supplement use lowered the prevalence of inadequate total intakes for every mineral examined in adults when sexes were combined (Figure 1). In men, dietary supplement users had a significantly lower prevalence of inadequate total mineral intakes for calcium, iron, magnesium, zinc, phosphorus, and copper but not for selenium (Table 2). The use of dietary supplements lowered the prevalence of inadequate total intakes for each mineral examined in women; the most notable difference between supplement nonusers and users was for calcium intakes. Supplement use dramatically decreased the prevalence of inadequate calcium intake across all age groups of women (Figure 2).
FIGURE 1.
The prevalence of inadequate mineral intakes in adults (≥19 y of age) by dietary supplement users and nonusers in the United States, 2003–2006. *Significant difference between users and nonusers of dietary supplements that contained calcium, P < 0.003. EAR, Estimated Average Requirement.
FIGURE 2.
The prevalence of calcium intakes below the EAR by adult female dietary supplement users and nonusers in the United States, 2003–2006. *Significant difference between users and nonusers of dietary supplements for each respective mineral, P < 0.003. EAR, Estimated Average Requirement.
Prevalence of intakes above the UL
Mineral intakes from food alone that were above the UL were shown in <0.5% of the adults studied. Although the prevalence of the total intake above the UL for minerals was close to zero (data not shown) in dietary supplement users, the prevalence of total intakes above the UL for calcium, iron, zinc, and magnesium was higher (Table 3). In the adult population of supplement users (when sexes were combined), ∼6% of subjects exceeded the UL for calcium, ∼9% of subjects exceeded the UL for iron, ∼9% of subjects exceeded the UL for zinc, and ∼6% of subjects exceeded the UL for magnesium (data not shown). In men who used dietary supplements, ∼5% of subjects exceeded the UL for calcium, ∼12% of subjects exceeded the UL for iron, ∼11% of subjects exceeded the UL for zinc, and ∼4% of subjects exceeded the UL for magnesium. Older men were more likely than were younger men to exceed the ULs for iron, zinc, and magnesium. About 7% of women who used dietary supplements exceeded ULs for calcium, iron, zinc, and magnesium.
TABLE 3.
Prevalence of total intakes above the UL in adult (≥19 y of age) users of dietary supplements in the United States, 2003–20061
| Age | Calcium (n = 3819) | Iron (n = 1909) | Zinc (n = 2914) | Magnesium (n = 3051) |
| Men | ||||
| All ≥19 y | 4.5 ± 0.5 | 12.1 ± 1.3 | 11.2 ± 1.2 | 3.6 ± 0.7 |
| 19–30 y | 2.6 ± 1.0 | 11.0 ± 2.3 | 8.5 ± 2.3 | 2.1 ± 0.8 |
| 31–50 y | 3.1 ± 0.6 | 9.8 ± 1.9 | 8.2 ± 1.3 | 3.3 ± 1.2 |
| 51–70 y | 7.9 ± 1.4 | 13.6 ± 2.1 | 13.4 ± 2.5 | 4.0 ± 1.5 |
| ≥71 y | 2.5 ± 0.8 | 19.1 ± 3.6 | 16.1 ± 1.6 | 6.1 ± 1.1 |
| Women | ||||
| All ≥19 y | 7.0 ± 0.9 | 7.3 ± 0.9 | 7.2 ± 0.8 | 7.2 ± 1.1 |
| 19–30 y | 1.3 ± 0.6 | 10.6 ± 2.3 | 5.7 ± 1.9 | 4.2 ± 2.1 |
| 31–50 y | 2.6 ± 0.8 | 7.0 ± 1.5 | 5.4 ± 1.4 | 5.8 ± 1.4 |
| 51–70 y | 15.5 ± 1.8 | 5.7 ± 1.7 | 7.5 ± 1.8 | 9.3 ± 2.0 |
| ≥71 y | 16 ± 0.5 | 8.0 ± 1.9 | 11.3 ± 1.7 | 7.3 ± 1.9 |
All values are percentages ± SEs. UL, tolerable upper intake level.
DISCUSSION
In general, dietary supplement users tended to have higher usual mean intakes of minerals from their diets than did nonusers, especially in women. In men, mean intakes of magnesium, copper, potassium, and selenium from food sources were significantly higher for users than for nonusers of supplements. However, only the prevalence of inadequate intakes was lower for magnesium and copper. In men, the difference between dietary intakes in users and nonusers of supplements was most notable for magnesium; a clear explanation of this finding was not evident. Stronger associations between higher mineral intakes from foods and a lower prevalence of inadequate intakes were observed in women. Women who used supplements were much less likely to have inadequate magnesium and calcium intakes from food sources than were nonusers. This finding was not surprising because many experts recommend that adult women consume and use supplemental calcium to lower risk of osteoporosis, and it is likely that women who use supplements are making dietary choices aligned with this recommendation.
Calcium is a nutrient of public health concern; recently, DRIs were established on the strong evidence that calcium was related to bone health and risk of falls and fractures, particularly in older women (22). Calcium intakes of US adults remain below the recommended intakes set forth by the DRI panel (22). For women, the EAR and RDA are 1000 and 1200 mg Ca/d, respectively, for individuals >51 y of age. For men, the EAR and RDA is 800 and 1000 mg Ca/d, respectively, for individuals 51–70 y of age, and the EAR and RDA is 1000 and 1200 mg Ca/d, respectively, for individuals >70 y of age. Overall, 71% of nonusers and 24% of users of supplements had intakes below the EAR, including calcium intakes from the use of antacids and calcium that are in the water supply. In subjects >51 y of age, close to 90% of nonusers and ∼30% of users did not meet the EAR (Figure 1). Our data and those of others (9, 25) suggested that the majority of older adults who do not use calcium-containing dietary supplements are not meeting their needs through the diet alone.
When total intakes (diet and supplements) of users were compared with dietary intakes of nonusers, users had significantly higher mean intakes than nonusers did across all age groups and in both men and women. The use of dietary supplements did not substantially contribute to intakes of phosphorus and potassium, primarily because dietary supplements do not typically contain large amounts of these minerals. In supplement users, the prevalence of inadequate total intakes of calcium, iron, magnesium, zinc, and copper was much lower than the prevalence of inadequate intakes from food alone. However, even in users of supplements, ∼20% of US adults reported intakes below the EAR for calcium and magnesium.
Ervin and Kennedy-Stephenson (25) examined NHANES III data (1988–1994) in older adults (≥60 y of age) by mineral supplement use. For calcium, dietary intakes were significantly different for both men and women by supplement-use categories, whereas we only showed differences in women. We could not directly compare our findings to the earlier NHANES III data because we used different age groupings; however, dietary intakes of calcium in our current study were ∼200–300 mg higher than those of older adults in the NHANES III (25).
Ervin and Kennedy-Stephenson (25) also showed significant differences in iron intake from the diet for male supplement users compared with male nonusers, whereas we did not observe these differences . Similar to the earlier report, we showed that dietary zinc intakes in older women supplement users were higher than in nonusers (see supplemental Table 1 under “Supplemental data” in the online issue). In NHANES III and NHANES 2003–2006, total dietary intakes were higher and the prevalence of inadequate intakes were lower in older adults who used supplements than in older adults who did not use supplements.
Approximately 65% of adults who did use dietary supplements reported magnesium intakes from food sources that were below the EAR. Inadequate iron intakes were not an issue in men, regardless of supplement use; however, 13–16% of adult women in the United States reported intakes that do not meet the EAR through the diet alone. For dietary supplement users, the prevalence of inadequate intakes was virtually nonexistent for iron, zinc, phosphorus, copper, and selenium.
The finding that subjects who used mineral-containing supplements already had higher mineral intakes from food sources alone is of public health relevance for 2 important reasons. First, dietary supplements may not be used by individuals with the greatest need (ie, people with lowest dietary intakes). Conversely, supplement users represent a group who may be at risk of exceeding the UL if their supplement intakes greatly exceed RDA amounts. If other studies confirm this finding, educational messages to limit total intakes to RDA amounts may be in order. The use of supplements did not greatly move the distribution of intakes above the UL for phosphorus, copper, and selenium. However, the use of dietary supplements did increase the prevalence of intakes above the UL for calcium, magnesium, iron, and zinc. High doses of calcium and iron may pose problems. The adverse effects of chronic exposure to high calcium intakes are an increase in the prevalence of kidney stones and hypercalcemia (22). Chronic iron excess is particularly problematic because it can accumulate in the tissues and organs once storage sites are saturated (21). However, even at the 90th percentile, users of iron-containing dietary supplements were below the UL for iron (45 mg) for adults with the exception of men ≥71 y of age, whose 90th percentile of total usual iron intake was 75 mg (data not shown). The short-term effects of high zinc intakes are primarily related to gastrointestinal distress, whereas chronic high intakes of zinc may suppress the immune response, decrease HDL-cholesterol concentrations, and may reduce copper status (ie, a decrease in erythrocyte copper-zinc superoxide dismutase). The UL for magnesium was set from supplemental sources only; one cannot exceed the UL from the diet alone. The adverse effects of high intakes of magnesium are primarily related to gastrointestinal distress, such as cramping and diarrhea. It should be noted that the prevalence of intakes above the UL reflects a population perspective. It was not possible in this study to determine whether two 24-h dietary recalls were sufficient to identify individuals who exhibited clinical signs or symptoms of excess.
Dietary supplement use increases with age, whereas most mineral needs do not. Thus, older adults may be more likely to have excessive total intakes for some minerals than do younger persons. Overall, 6% of adults had total usual calcium intakes above the UL; however, the prevalence increased to almost 16% in 51–70-y-old women. In men aged ≥71 y who used mineral-containing dietary supplements, the prevalence of usual intakes above the UL for iron was almost 20%, and it was 16% for zinc. The relatively high usual mineral intakes of these subgroups raise some potential safety concerns.
A limitation of this report is that the estimates relied on self-reported dietary data for both nutrient intakes from foods and dietary supplements. The models that we applied also relied on assumptions that reported nutrient intakes from food sources on the 24-h recalls were unbiased, and the self-reported dietary supplement intake reflected the true long-term supplement intake. Furthermore, estimates of minerals contributed by dietary supplements depended on the label declarations rather than analytic values. The data presented in this manuscript should be interpreted with these limitations in mind.
Dietary supplement use is common, particularly in older adults. The most commonly used dietary supplements in the United States are multivitamin and mineral preparations. Ideally, formulations and amounts of minerals in these types of supplements should be used to help meet, but not exceed, DRI recommendations to best fit the nutrient needs of adults (13). Our results confirmed previous findings that individuals who use supplements tended to have higher mineral intakes from diet alone, and they also had a lower prevalence of inadequate intakes than individuals who did not report the use of mineral supplements. Thus, people who use mineral-containing supplements are, in many cases, already obtaining more of these nutrients from food sources in their diets than are nonusers of mineral-containing supplements. Less than 0.5% of US adults have dietary intakes above the UL recommendations; however, the use of dietary supplements increased the prevalence of total mineral intakes that were above the UL for calcium, zinc, magnesium, and iron. These data support the contention that diets of users of mineral-containing dietary supplements are different from nonusers, and from a public health standpoint, the intakes of users of mineral-containing dietary supplements need to be examined separately to best assess the role of nutrients on disease risk and health outcomes (26).
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—RLB and JTD: contributed to concept development and manuscript preparation; DRK: created data files for demographic data and for food and supplements for the NHANES; VLF: completed analytical and statistical portions of this work; and all authors: read and approved the final version of the manuscript. None of the authors had a personal or financial conflict of interest.
Footnotes
Abbreviations used: DRI, Dietary Reference Intake; EAR, Estimated Average Requirement; NCI, National Cancer Institute; RDA, Recommended Dietary Allowance; UL, tolerable upper intake level.
REFERENCES
- 1.Bailey RL, Gahche JJ, Lentino CV, Dwyer JT, Engel JS, Thomas PR, Betz JM, Sempos CT, Picciano MF. Dietary supplement use in the United States, 2003-2006. J Nutr 2011;141:261–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Picciano MF, Dwyer JT, Radimer KL, Wilson DH, Fisher KD, Thomas PR, Yetley EA, Moshfegh AJ, Levy PS, Nielsen SJ, Marriott BM. Dietary supplement use among infants, children, and adolescents in the United States, 1999-2002. Arch Pediatr Adolesc Med 2007;161:978–85 [DOI] [PubMed] [Google Scholar]
- 3.Foote JA, Murphy SP, Wilkens LR, Hankin JH, Henderson BE, Kolonel LN. Factors associated with dietary supplement use among healthy adults of five ethnicities: the Multiethnic Cohort Study. Am J Epidemiol 2003;157:888–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Radimer K, Bindewald B, Hughes J, Ervin B, Swanson C, Picciano MF. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999-2000. Am J Epidemiol 2004;160:339–49 [DOI] [PubMed] [Google Scholar]
- 5.Rock CL. Multivitamin-multimineral supplements: who uses them? Am J Clin Nutr 2007;85:277S–9S [DOI] [PubMed] [Google Scholar]
- 6.Touvier M, Niravong M, Volatier JL, Lafay L, Lioret S, Clavel-Chapelon F, Boutron-Ruault MC. Dietary patterns associated with vitamin/mineral supplement use and smoking among women of the E3N-EPIC cohort. Eur J Clin Nutr 2009;63:39–47 [DOI] [PubMed] [Google Scholar]
- 7.Harrison RA, Holt D, Pattison DJ, Elton PJ. Are those in need taking dietary supplements? A survey of 21 923 adults. Br J Nutr 2004;91:617–23 [DOI] [PubMed] [Google Scholar]
- 8.Block G, Jensen CD, Norkus EP, Dalvi TB, Wong LG, McManus JF, Hudes ML. Usage patterns, health, and nutritional status of long-term multiple dietary supplement users: a cross-sectional study. Nutr J 2007;6:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sebastian RS, Cleveland LE, Goldman JD, Moshfegh AJ. Older adults who use vitamin/mineral supplements differ from nonusers in nutrient intake adequacy and dietary attitudes. J Am Diet Assoc 2007;107:1322–32 [DOI] [PubMed] [Google Scholar]
- 10.Robson PJ, Siou GL, Ullman R, Bryant HE. Sociodemographic, health and lifestyle characteristics reported by discrete groups of adult dietary supplement users in Alberta, Canada: findings from The Tomorrow Project. Public Health Nutr 2008;11:1238–47 [DOI] [PubMed] [Google Scholar]
- 11.Bailey RL, Dodd KW, Gahche JJ, Dwyer JT, McDowell MA, Yetley EA, Sempos CA, Burt VL, Radimer KL, Picciano MF. Total folate and folic acid intake from foods and dietary supplements in the United States: 2003-2006. Am J Clin Nutr 91:231–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bailey RL, Dodd KW, Goldman JA, Gahche JJ, Dwyer JT, Moshfegh AJ, Sempos CT, Picciano MF. Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr 140:817–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy SP, White KK, Park SY, Sharma S. Multivitamin-multimineral supplements’ effect on total nutrient intake. Am J Clin Nutr 2007;85:280S–4S [DOI] [PubMed] [Google Scholar]
- 14.National Center for Health Statistics About the National Health and Nutrition Examination Survey, 2009. Available from: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm (cited 17 August 2008)
- 15.Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J Nutr 2006;136:2594–9 [DOI] [PubMed] [Google Scholar]
- 16.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA, Staples RC, Cleveland LE. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88:324–32 [DOI] [PubMed] [Google Scholar]
- 17.National Center for Health Statistics National Health and Nutrition Examination Survey. SP questionnaire component: dietary supplements questionnaire data, 2003-2004. Available from: http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/dsq_c.pdf (cited 1 April 2010)
- 18.Food and Nutrition Board Dietary reference intakes applications in dietary assessment. Washington, DC: National Academy Press, 2000 [Google Scholar]
- 19.Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, Guenther PM, Carroll RJ, Kipnis V. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc 2006;106:1575–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Cancer Institute Usual dietary intakes: the NCI method. 2009. Available from: http://riskfactor.cancer.gov/diet/usualintakes/method.html (cited 1 August 2009)
- 21.Food and Nutrition Board Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, molybdenum, nickel, silicon, vanadium and zinc. Washington, DC: National Academy Press, 2001 [PubMed] [Google Scholar]
- 22.Food and Nutrition Board Dietary reference intakes for calcium and vitamin D. Washington, DC: National Academy Press, 2010 [Google Scholar]
- 23.Food and Nutrition Board Dietary reference intakes for vitamin C, vitamin E, selenium, and carotenoids. Washington, DC: National Academy Press, 2000 [PubMed] [Google Scholar]
- 24.Selvin S. Statistical analysis of epidemiologic data. 3rd ed New York, NY: Oxford University Press, 2004; [Google Scholar]
- 25.Ervin RB, Kennedy-Stephenson J. Mineral intakes of elderly adult supplement and non-supplement users in the third national health and nutrition examination survey. J Nutr 2002;132:3422–7 [DOI] [PubMed] [Google Scholar]
- 26.Garriguet D. Combining nutrient intake from food/beverages and vitamin/mineral supplements. Health Rep 2010;21:71–84 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.