Abstract
The occurrence of bilateral extradural hematomas (EDH) is an uncommon consequence of craniocerebral trauma, and acute symmetrical bilateral epidural hematomas are extremely rare. We discuss the technique adopted by us for the management of this rare entity. A 55-year-old patient presented with history of fall of branch of tree on her head. She had loss of consciousness since then and had multiple episodes of vomiting. Examination of the scalp was suggestive of diffuse subgaleal hematoma. Her Glasgow coma scale was nine and there were no lateralizing signs. Her computed tomography scan showed bilateral, symmetrical, parietal EDH with diastases of coronal suture. The patient underwent bicoronal scalp flap well behind the coronal suture running across the junction of anterior two-third and posterior one-third of hematoma to gain bilateral exposure. Initially, left parietal trephine craniotomy was performed and without disturbing the blood clot, left trephine craniotomy was performed and the hematomas were evacuated. Management of bilateral EDH cases requires careful planning, adequate exposure, judicious surgical approach, and time management for good results.
Keywords: Bilateral extradural hematoma, CT scan, double extradural hematoma, extradural hematoma, head injury
INTRODUCTION
The occurrence of bilateral extradural hematomas (EDH) is an uncommon consequence of craniocerebral trauma and its incidence in various studies ranges from 2 to 25%.[1–6] Acute symmetrical bilateral epidural hematoma is rarely reported.[7] We discuss the technique adopted by us for the management of this rare entity.
CASE REPORT
A 55-year-old woman presented with history of fall of branch of tree on her head. She presented to the casualty after about 12 hours of injury. She had loss of consciousness since then and had multiple episodes of vomiting. There was no ear, nasal bleed, or history of convulsions. Her general examination was unremarkable. She had swelling, crepitus, and tenderness of right forearm. Examination of the scalp was suggestive of diffuse subgaleal hematoma. On neurological examination, Glasgow coma scale (GCS) was nine (eye opening to pain-2, groaning to pain-2, and localizing to pain-5). There were no lateralizing signs. Her computed tomography (CT) scan showed bilateral, symmetrical parietal EDH [Figure 1]. Bone window showed diastases of coronal suture. Her X-ray of right forearm showed fracture of right radius. Midline, coronal sutures, and approximate location of EDH (calculated based on CT scan findings) were marked on scalp [Figure 2]. Bicoronal scalp flap well behind the coronal suture running across the junction of anterior two-third and posterior one-third of hematoma was made to gain bilateral exposure [Figure 3]. There were coronal diastases and fracture of the right parietal and temporal bone, with diffuse oozing of blood from fracture lines [Figure 4]. Initially, left parietal trephine craniotomy was performed (to decompress dominant cerebral hemisphere and no fracture) and without disturbing the blood clot, left trephine craniotomy was performed and both hematomas were exposed. Hematomas were evacuated left followed by right and the bleeding from meningeal arteries was controlled with gelfoam and bipolar coagulation. Diffuse ooze from dura was controlled with hydrogen peroxide and gelfoam. Next day morning, patient GCS improved to 15/15 and doing well at follow-up.
Figure 1.
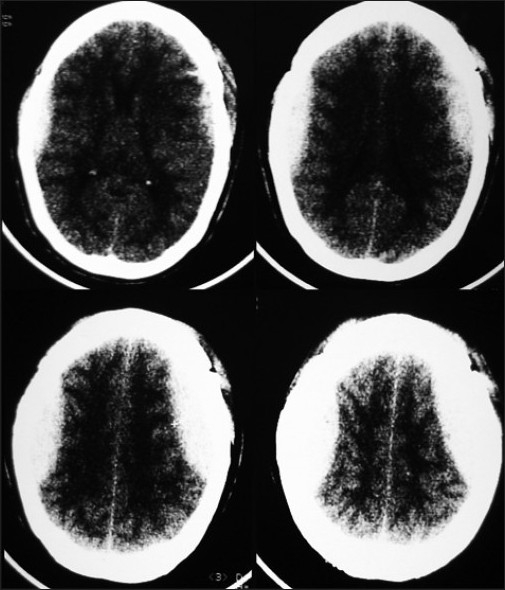
CT scan showing bilateral parietal EDH
Figure 2.

Clinical image showing marking of coronal suture, midline, and approximate location of extradural hematomas
Figure 3.
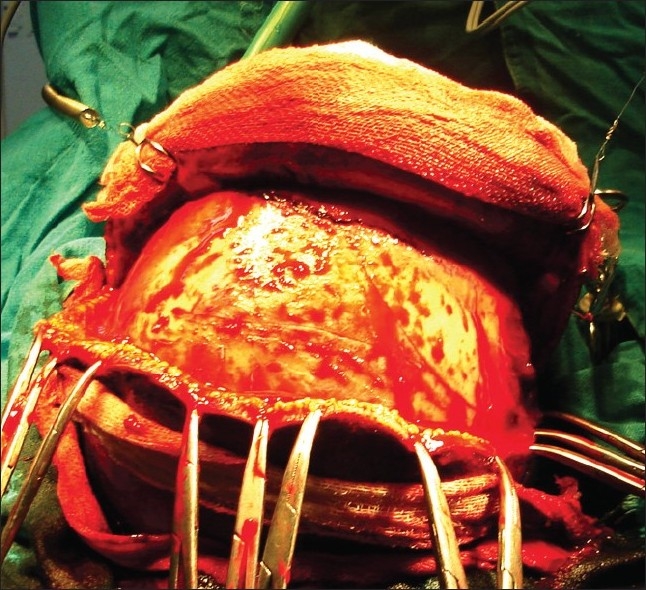
Bicoronal scalp flap showing wide and bilateral exposure of both parietal regions
Figure 4.
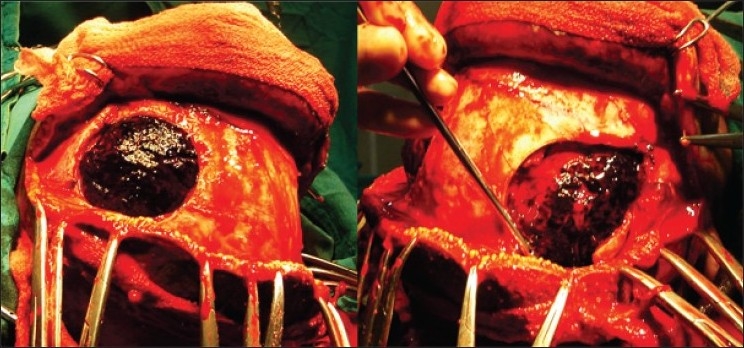
Intraoperative photograph showing bilateral trephine craniotomy and exposure of extradural blood clot
DISCUSSION
It has been suggested that the force of impact to the head can produce bilateral hematomas, particularly when the impact is predominantly more in anteroposterior direction than from the lateral direction.[2] Dura is detached from two locations by a single directed force. Stripping of dura can occur at site of impact by inbending or outbending of skull[2] or due to motion of skull, further aggravated by the negative intracranial pressure found at the antipode of the compression force.[8] Besides that, it can also occur due to extension of fracture line across midline, leading to bilateral EDH under fracture line,[2,9] as was seen in present case. Bilateral epidural hematomas are associated with high mortality,[3,4] as the patients with double EDH less frequently have a lucid interval, have a lower GCS, lateralization is frequently absent, and deteriorate more often than individuals with unilateral hematomas.[2,4,7,10] There are two types of bilateral EDH, and in the commoner first type, the bleeding is venous in nature and occurs as a delayed phenomenon, whereas in the second type, the bleeding is arterial in nature.[2,11] As in present case, injury to the bilateral middle meningeal arteries could be the cause of the bilateral epidural hematomas.[7] Emergency and rapid decompression of the brain, if necessary with bilateral simultaneous craniotomies by the two neurosurgeon-groups, should be performed.[7] Simultaneous bilateral craniotomies and removal of the epidural hematomas will reduce the operating time and will obtain the good result.[7] However, having two operating neurosurgeons may not always be possible and performing bilateral four burr hole conventional craniotomy with two scalp flaps will result in time loss (unless the facilities of power driven cranitome is available). In present case, we could save time by making single bicoronal incision and by performing bilateral trephine craniotomy. Furthermore, two square-shaped scalp flaps that are reflected laterally can result in the vascular compromise of midline scalp strip (as the lesions were close to midline). This issue was solved by bicoronal incision that gave adequate exposure and had scalp flaps with wide base both anteriorly and posteriorly. One more point needs to be remembered that before disturbing the left extradural hematoma, right sided EDH was also exposed. Time consumed in the evacuation of the blood clot and hemostasis could have resulted in the delay in the decompression on the opposite side. Once left sided craniotomy was performed and bone flap was removed, there was decompression of brain parenchyma and we could buy time to perform on the other side. In summary, bilateral EDH are uncommon and symmetrical EDH are extremely rare. Management of these cases requires careful planning, adequate exposure, judicious surgical approach, and time management for good results.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Dharkar SR, Bhargava N. Bilateral epidural hematoma. Acta Neurochir. 1991;110:29–31. doi: 10.1007/BF01402044. [DOI] [PubMed] [Google Scholar]
- 2.Frank E, Berger TS, Jew JM. Bilateral epidural hematoma. Surg Neurol. 1982;17:218–22. doi: 10.1016/0090-3019(82)90285-3. [DOI] [PubMed] [Google Scholar]
- 3.Gorgulu A, Cobanoglu S, Armagan S, Karabagli H, Tevruz M. Bilateral epidural hematoma. Neurosurg Rev. 2000;23:30–3. doi: 10.1007/s101430050028. [DOI] [PubMed] [Google Scholar]
- 4.Huda MF, Mohanty S, Sharma V, Tiwari Y, Choudhary A, Singh VP. Double extradural hematoma: An analysis of 46 cases. Neurol India. 2004;52:450–2. [PubMed] [Google Scholar]
- 5.Krayenbuhi H, Brihaye J, Loew F. Advances and technical standards in Neurosurgery. In: Zander E, Campiche R, editors. Extradural hematoma. Vol. 1. New York: Springer Verlag; 1974. pp. 1231–9. [Google Scholar]
- 6.Rivas JJ, Lobatto RD, Sarabia R, Cordobes F, Cabrera A, Gomez P. Extradural hematoma: Analysis of factors influencing the courses of 161 patients. Neurosurgery. 1988;23:44–51. doi: 10.1227/00006123-198807000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Idei M, Shima T, Nishida M, Yamane K, Mihara C, Hatayama T, et al. Symmetrical bilateral epidural hematoma after head injury in the mid parietooccipital region: Case report. No Shinkei Geka. 2004;32:379–82. [PubMed] [Google Scholar]
- 8.Gurdjian ES. Recent advances in the study of mechanism of impact of injury of the head: A summary. Clin Neurol. 1972;11:1–43. doi: 10.1093/neurosurgery/19.cn_suppl_1.1. [DOI] [PubMed] [Google Scholar]
- 9.Ramzan A, Wani A, Malik AH, Kirmani A, Wani MA. Acute bilateral extradural hematomas. Neurol India. 2002;5:217–8. [PubMed] [Google Scholar]
- 10.Rasmussen GL, Holme S. Bilateral epidural hematomas. Ugeskr Laeger. 1991;154:203–4. [PubMed] [Google Scholar]
- 11.Rochat P, Johannesen HH, Poulsgard L, Bogeskov L. Sequentially evolved bilateral epidural haematomas. Clin Neurol Neurosurg. 2002;105:39–41. doi: 10.1016/s0303-8467(02)00099-9. [DOI] [PubMed] [Google Scholar]