Abstract
Background:
The diabetes electronic medical record (DEMR) has emerged as an effective information management tool with the potential to improve diabetes care and research. This study reports on the usefulness of the DEMR system at Dr. Mohan's Diabetes Specialities Centre (DMDSC), Chennai, India, for clinical and research purposes.
Methods:
The DEMR, set up in 1996 at DMDSC, connects data of nine centers/clinics in different geographical areas in Southern India. The present data analysis is based on a total of 226,228 patients registered in the DEMR system at DMDSC between the years 1991 and 2010.
Results:
The DEMR included data of 139,906 male and 86,322 female patients, of whom 92.6% had type 2 diabetes mellitus (T2DM), 1.4% had type 1 diabetes mellitus (T1DM), and the rest had other types. Patients with T2DM had higher prevalence rates of neuropathy (33.1% vs 13.0%, p < .001), microalbuminuria (25.5% vs 20.0%, p < .001), coronary artery disease (17.5% vs 9.2%, p < .001) and peripheral vascular disease (3.9% vs 2.8%, p = .017) compared with T1DM patients, while prevalence of diabetic retinopathy was similar (37.9% vs 35.7%, p = .06). Prevalence of microvascular and macrovascular complications of diabetes increased with increasing glycated hemoglobin levels (p for trend < .001) and increasing diabetes duration (p for trend < .001).
Conclusions:
The DEMR helps track diabetes care and is a valuable tool for research.
Keywords: Asian Indians, complications, databases, diabetes, electronic medical records, India, South Asians
Introduction
Developing countries such as India are currently facing an epidemic of noncommunicable diseases that threaten the lives of millions of people,1 and unfortunately, they are the very ones that lack resources and robust health care infrastructure.2 According to the International Diabetes Federation Diabetes Atlas, India already has over 50 million people with diabetes. This number is expected to increase to 87 million by the year 2030.3 As diabetes is a chronic illness, it requires coordinated medical care and patient self-management to decrease the risk of long-term complications.4
Modern methods to improve diabetes care include decision support for physicians and/or patients.5 The various types of electronic health information system include electronic medical records (EMRs), disease registries, personal health records, and administrative data. The EMR system is defined as “the computerization of health record content and associated processes usually referring to an electronic medical health record in a physician office setting or a computerized system of files in a hospital.”6 Several studies have employed advanced health information technologies and clinical decision support systems using functions enabled by EMR systems.7–9 There has been a growing recognition of the role of EMR systems in the provision of diabetes care and as an effective manage-ment tool to improve diabetes care.9–11 It is believed that implementation of EMR systems will lead to health care savings, reduced medical errors, improved implementation of care guidelines, and provision of data for decision support to improve the health of individuals with diabetes.12,13 However, there has been little progress toward attaining these goals in developing countries.
Indeed, even in developed nations, the development of EMR systems is still a challenge, as it requires appropriate technologies and adequate resources.14 This article will first review the use of EMRs in diabetes care in general and then specifically deal with the experience with the diabetes electronic medical record (DEMR) system at our chain of diabetes centers in Chennai (formerly Madras) in Southern India.
Electronic Medical Records in Diabetes Care
Several studies have shown that the quality of care provided for diabetes in most clinics is far from adequate.15,16 It is also suggested that well-formulated health care strategies can improve the process of care and outcomes for people with diabetes.17 Outpatient EMR systems are able to improve the documentation of care, communication of clinical information across sites, and measurement of productivity and variations in the care provided.18 Inpatient EMR systems have led to improvements in care in some critical clinical domains.19 Electronic medical records are helpful in adhering to recommendations for proper diabetes management where regular assessment of glycemia, blood pressure, lipid levels, and foot and eye care are essential.20
Weber and colleagues11 have shown that diabetes care improved significantly in response to a multifaceted intervention featuring the use of an EMR-derived registry in an integrated delivery system. Some studies have documented improved diabetes-related patient outcomes after EMR implementation,8,21–23 whereas others have shown improvements only in the processes of diabetes care.23,24 In controlled studies, EMR systems have had limited positive impact on outpatient diabetes care, and data on improvement of outcomes has been inconsistent.7,24,25 The potential factors/reasons for improvements in diabetes care with EMR use were prompts to physicians identifying when tests [glycated hemoglobin (HbA1c), lipids, micro-albuminuria, foot, and retinal examinations] were due and as a reminder of evidence-based goals.23,26
Electronic medical records are “enabling technology,” although they are neither easy to implement nor inexpensive.27 Some studies have shown that a computer-generated clinical data set is a support tool as valuable as the stethoscope, provided data entry is done properly.28,29 A study in Oman, evaluating physician satisfaction with the EMR system, identified a positive impact in areas of communication, data entry and retrieval, patient care, and reduction of medical errors and some negative aspects, including loss of confidentiality of information and software-related problems.30 Currently, only a few diabetes centers worldwide have electronic databases, and where available, they are neither optimally utilized nor written in same language (software). Hence, global linking of EMRs has been a great challenge.
Clinical and Research Applications of Diabetes Electronic Medical Records
The DEMR system can improve the organization as well as the efficiency of diabetes health care delivery. As treatment of diabetes is multifaceted, there is a need to take into account many clinical variables when making therapeutic decisions. The DEMR system is increasingly gaining acceptance as an enabling technology that allows physicians to practice evidence-based medicine.31
With increasing duration of follow-up, patient notes become voluminous, and the accuracy of the information recorded in paper-based medical records becomes difficult to verify and analyze. It is here that the application of EMRs in the management of diabetes becomes very useful as it captures, organizes, analyzes, and helps monitor outcome measures in diabetes care. Through the DEMR, a “patient-centered” approach of providing care is feasible, having the potential for including patient preferences in clinical decision making. Diabetes electronic medical records are undoubtedly valuable resources in conducting medical research.32,33 This is also illustrated in our own examples of research applications shown later in this article. However, the confidentiality of patient data should be ensured to be secure and protected.34
Barriers to Diabetes Electronic Medical Records
Despite the benefits of EMR systems, adoption of the technology has been slow.35 In a study conducted in the United States, the most commonly cited barriers to use of EMR systems in hospitals were inadequate capital for purchase (74%), maintenance costs (44%), resistance on the part of physicians (36%), unclear return on investment (32%), and lack of availability of trained staff (30%). Hospitals that had adopted EMR systems were less likely to cite four of these five concerns (all except physicians' resistance) as major barriers to adoption than were hospitals that had not adopted such systems.36 Other barriers include difficulties in incorporating data from older paper-based records into the electronic system, issues about long-term preservation and storage of data, software problems such as codification and customization, hardware limitations (interfacing with older technology), and issues of security and confidentiality. However, one of the major factors is the reluctance of doctors to use electronic systems.
Diabetes Electronic Medical Records Model at Dr. Mohan's Diabetes Specialities Centre
Dr. Mohan's Diabetes Specialities Centre (DMDSC; formerly M.V.Diabetes Specialities Centre) has state-of-the-art facilities for diabetes and related diseases, currently available at nine centers/clinics of DMDSC in different geographical areas in Southern India [Chennai (Gopalapuram, Annanagar, Tambaram, Adyar, and Vadapalani), Kancheepuram district (Chunampet) and Vellore in Tamilnadu, and Hyderabad (Domalguda and Jubilee Hills) in the state of Andhra Pradesh]. The main center of DMDSC is located at Gopalapuram in the heart of Chennai. Since its inception in 1991, nearly 230,000 patients with diabetes have been registered across various branches of DMDSC with approximately 20% annual growth. The main center and all branches of DMDSC are linked through EMRs and video conferencing facilities (www.drmohansdiabetes.com).
Computerization of health care information was planned at DMDSC even at the time of its inception in 1991. The DMDSC started with stand-alone computers, then moved to computers linked to a local area network system, and finally moved to an online totally computerized system. The online project commenced in late 1996 in collaboration with Novo Nordisk, Denmark. The DMDSC center provided the technical know-how, while CG Maersk Information Technologies developed the software. The project was funded through a generous grant from the Danish Government Private Sector Programme, and the software was initially owned by Novo Nordisk.
The DEMR was designed based on the existing paper medical records at the time but was made more manageable, maintainable, upgradable, retrievable, and user-friendly. The program was designed with Power Builder as the frontend database and structured query language (SQL) server as the backend database. In 2000, the entire DEMR was redesigned and upgraded with the inclusion of billing and in-hospital functions, and DMDSC assumed ownership of the software. Currently, the frontend of the DEMR is designed with Visual Basic and the backend database with SQL server. The present software is more user-friendly, and more functions and modules are continuously being added. Currently, 320 computers across all centers of DMDSC are linked to the DEMR system. All centers are interlinked with leased lines, and there are several servers to support all these activities. Data entries made in various departments are randomly checked at the end of the day for completeness and accuracy of data at the respective centers. Each center has a Microsoft SQL server that is connected to our main server where data are extracted by the Microsoft SQL analyzer. This method is simple and less time consuming, and data are extracted in forms of tables.
The databases are backed up internally and stored auto-matically in the hard disk every day on the Microsoft SQL server using a scheduler in the server. In addition, periodical tape backups are made and sent for off-site storage at regular intervals. The initial cost to install and set up this DEMR system in India is over 90,000 U.S dollars, and the annual cost to operate it (i.e., run, time spent on data entry, extraction, maintenance, time to educate the users) would be approximately 50,000 U.S. dollars.
Various Modules in Diabetes Electronic Medical Records
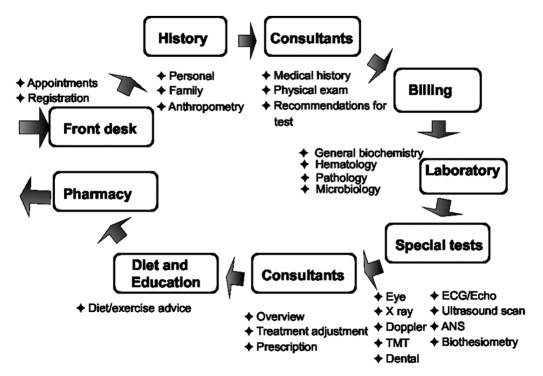
The modules in our DEMR system include registration, medical and personal history/anthropometry, test advice, diet advice, physical examination, billing, laboratory, special tests, and in-patient as shown in Figure 1. Our preliminary experience with DEMRs has been published previously.37
Figure 1.
Modules in the DEMR at DMDSC. TMT, treadmill test; ECG, electrocardiogram; ANS, autonomic nervous system.
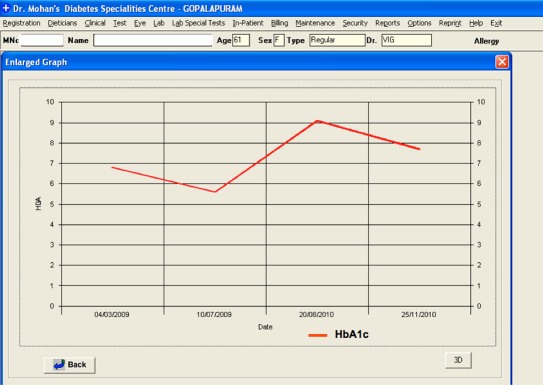
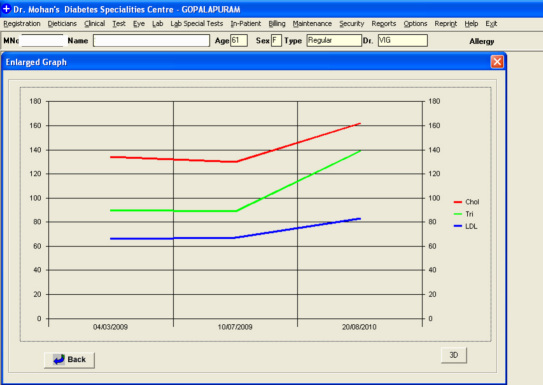
By providing a unique medical registration number to patients, the DEMR helps us reduce one of the most common, but preventable, medical errors that arises due to wrong identity of the patient. Figures 2 and 3 show two of the illustrative screens viewable by our consultants in the DEMR module. It can be observed that the diabetes control (HbA1c) and status of lipid control during the past visits can be viewed in graphical manner, which makes clinical decision making easier.
Figure 2.
Glycated hemoglobin screen viewed by consultant.
Figure 3.
Lipid screen viewed by consultant.
In addition, for security and audit trail, a unique user identification and password is given to each individual who uses the DEMR. The user of one department cannot view the modules of another department unless authorized. This helps protect patients' confidentiality.
Clinical and Research Applications: The Dr. Mohan's Diabetes Specialities Centre DEMR Model
Population Characteristics
Clinical
The DMDSC DEMR provides patient-specific assessments and helps clinicians make clinical decisions by flagging the patients who are at high risk for complications, have drug allergies, and need preventive care. By effectively managing a patient's demographics, medical history, medications, test results, diet advice, and physical activity, the DEMR plays a crucial role in providing comprehensive diabetes care.
Of the 226,228 patients registered at our center, 188,030 had different types of diabetes and glucose intolerance. Table 1 provides the breakdown of various types of diabetes and glucose intolerance.38 It shows that 92.6% of the patients had type 2 diabetes mellitus (T2DM), 1.4% had type 1 diabetes mellitus (T1DM), 0.5% had gestational diabetes, 0.4% had fibrocalculous pancreatic diabetes, 0.2% had maturity onset diabetes of young, 0.3% had impaired fasting glucose, 3.9% had impaired glucose tolerance, and 0.7% comprised other types.
Table 1.
Breakdown of Various Types of Diabetes and Glucose Intolerance among the Registered Diabetes Patients at Dr. Mohan's Diabetes Specialities Centrea
| Type of diabetes/glucose intolerance | Male (n = 120,836) n (%) | Female (n = 72,306) n (%) | Total (n = 188,030) n (%) |
|---|---|---|---|
| T2DMb | 109,208 (90.4) | 64,861 (89.7) | 174,069 (92.6) |
| T1DMb | 1554 (1.3) | 1119 (1.5) | 2673 (1.4) |
| Gestational diabetes mellitusb | — | 904 (1.3) | 904 (0.5) |
| Fibrocalculous pancreatic diabetes | 719 (0.6) | 250 (0.3) | 787 (0.4) |
| Maturity onset diabetes of the young | 216 (0.2) | 176 (0.2) | 392 (0.2) |
| Impaired fasting glucoseb | 392 (0.3) | 208 (0.3) | 600 (0.3) |
| Impaired glucose toleranceb | 4700 (3.9) | 2587 (3.6) | 7287 (3.9) |
| Others | 4047 (3.3) | 2201 (3.0) | 1318 (0.7) |
T2DM includes known diabetes and newly detected diabetes based on oral glucose tolerance test, T1DM includes known diabetes and newly detected diabetes based on C-peptide and glutamic acid decarboxylase assay, gestational diabetes was diagnosed based on oral glucose challenge test, maturity onset diabetes of the young was diagnosed based on genetic analysis, impaired fasting glucose was diagnosed based on fasting glucose, and impaired glucose tolerance was diagnosed based on oral glucose tolerance test. Others include tropical chronic pancreatitis, early glucose tolerance, and neonatal diabetes.
World Health Organization Criteria.38
The DEMR helps assess the quality of diabetes care by measuring adherence to guidelines for complications screening in patients with diabetes. Table 2 provides the percentage of review patients (n = 44,295) who met the diabetes screening guidelines during the year 2010 at DMDSC. It was observed that 94.5% of patients adhered to two of four guidelines for screening complications while 64.8% of patients adhered to all guidelines. Part of this may be related to the fact that DMDSC is a private center where patients pay for their services, and some may have refused to undergo certain investigations because of financial or other constraints.
Table 2.
Percentage of Review Patients Who Met the Diabetes Screening Guidelines in the Year 2010: Data from the Diabetes Electronic Medical Records of Dr. Mohan's Diabetes Specialities Centre
| Parameters | Diabetes patients (n = 44,295) n (%) |
|---|---|
| HbA1c assessed within past 6 months | 42,184 (95) |
| Urine microalbumin assessed within past 12 months | 32,878 (74) |
| Lipids assessed within past 12 months | 40,468 (91.4) |
| Retinal examination done within past 12 months | 36,306 (82) |
| Two of four guidelines met | 41,865 (94.5) |
| All four guidelines met | 28,702 (64.8) |
Research
The DEMR serves as a rich database for answering research questions. Using the DEMR database of DMDSC, several retrospective, cross-sectional, and follow-up studies have been published.39–48 Some of these are briefly reviewed here. Studies have been performed to determine the prevalence of, and risk factors for, diabetic retinopathy (DR),40 proteinuria,41 microalbuminuria,42 and neuropathy.43 Premalatha and associates44 compared the specificity and sensitivity of ankle-brachial index (ABI) measured by peripheral Doppler with the color duplex ultrasound for diagnosis of peripheral vascular disease (PVD). The sensitivity and specificity of ABI in this study was 70.6 % and 88.5%, respectively. Deepa and coworkers46 studied 725 T2DM patients with and without diabetic complications to determine the relation of lipoprotein(a) with microvascular and macrovascular complications. The study concluded that lipoprotein(a) were higher in those with coronary artery disease (CAD) and proteinuria but not associated with retinopathy or PVD in our T2DM patients.
A retrospective study conducted by Rema and colleagues48 in 5000 T2DM patients who underwent a retinal examination between 1995 and 1999 at DMDSC reported that, of the 261 eyes of 160 patients who underwent panretinal photocoagulation, 73% of 191 eyes with good visual acuity (6/9) at baseline maintained the same vision at 1-year follow-up. Of the 53 eyes with visual acuity of 6/12–6/36 at baseline, 58.5% maintained same vision and 18.9% improved their vision at follow-up. Of the 17 eyes with visual acuity ≤6/60 at baseline, 12 maintained the same vision and the remaining 5 improved their vision. This is an example of how DEMR helps to assess outcomes in diabetes patients.
Current Analysis of Diabetes Electronic Medical Records Data
The analysis reported in this section includes a total of 226,228 patients registered in the DEMR system at DMDSC between the years 1991 and 2010. All statistical analyses were performed using SAS statistical package (version 9.0; SAS Institute, Inc., Cary, NC). Numbers are expressed as mean ± standard deviation. Student's t test was used to compare groups for continuous variables. Chi square test was used to compare proportions among groups. For all statistical tests, p value < .05 was considered as the level of significance.
Table 3 presents the baseline (first visit) clinical and biochemical characteristics of the 139,906 male patients and 86,322 female patients. Of the 226,228 registered patients, lipid values were missing for 13%, blood pressure data was missing for 11%, and fasting blood sugar values were missing for 9%. Female patients had higher fasting plasma glucose (179.8 ± 76.9 vs 172.4 ± 71.3 mg/dl, p < .001), serum cholesterol levels (196.2 ± 44.7 vs 186.8 ± 43.6 mg/dl, p < .001), serum high-density lipoprotein cholesterol (44.9 ± 10.5 vs 39.8 ± 9.3 mg/dl, p < .001), and serum low-density lipoprotein cholesterol (117.6 ± 36.7 vs 111.9 ± 35.7 mg/dl, p < .001), body mass index (BMI; 26.6 ± 4.5 vs 25.1 ± 3.6, p < .001) compared with male patients.
Table 3.
Baseline Clinical and Biochemical Characteristics of Male and Female Patients Registered at Dr. Mohan's Diabetes Specialities Centrea
| Variables | Male (n = 139,906) | Female (n = 86,322) | P value |
|---|---|---|---|
| Age (years) | 51.1 ± 12.3 | 51.0 ± 12.7 | 0.015 |
| Height (cm) | 167.1 ± 7.1 | 153.6 ± 6.7 | <0.001 |
| Weight (kg) | 70.3 ± 13.1 | 63.5 ± 12.7 | <0.001 |
| Body mass index (kg/m2) | 25.1 ± 3.9 | 26.6 ± 4.5 | <0.001 |
| Systolic blood pressure (mm Hg) | 131.8 ± 18.4 | 133.3 ± 19.3 | <0.001 |
| Diastolic blood pressure (mm Hg) | 82.4 ± 9.1 | 81.4 ± 8.8 | <0.001 |
| Fasting plasma glucose (mg/dl) | 172.4 ± 71.3 | 179.8 ± 76.9 | <0.001 |
| Duration of diabetes (years)b | 7.3 ± 7.3 | 6.7 ± 6.6 | <0.001 |
| HbA1c (%) | 8.6 ± 2.2 | 8.7 ± 2.3 | <0.001 |
| Cholesterol (mg/dl) | 186.8 ± 43.6 | 196.2 ± 44.7 | <0.001 |
| Triglycerides (mg/dl) | 179.4 ± 150.2 | 167.2 ± 117.0 | <0.001 |
| High-density lipoprotein cholesterol (mg/dl) | 39.8 ± 9.3 | 44.9 ± 10.5 | <0.001 |
| Low-density lipoprotein cholesterol (mg/dl) | 111.9 ± 35.7 | 117.6 ± 36.7 | <0.001 |
| Creatinine (mg/dl) | 0.97 ± 0.46 | 0.77 ± 0.32 | <0.001 |
Data presented as mean ± standard deviation.
Only in T1DM and T2DM patients.
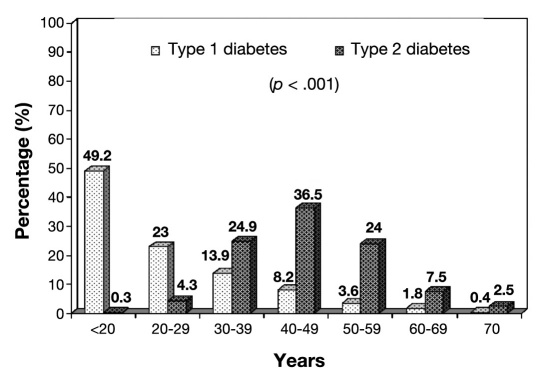
Figure 4 shows the percentage distribution of age at diagnosis of T1DM and T2DM patients (for known diabetes patients, it is obtained through the patient's history, while for newly diagnosed diabetes patients, it is the respective age at which they are diagnosed at DMDSC). It can be seen that, while frequency of T1DM is higher (as expected) at lower ages, it is still seen in older age groups. The converse is true for T2DM, where the peak age at onset in our patients occurs between 40 and 49 years of age.
Figure 4.
Percentage distribution of the age at onset of diabetes among T1DM and T2DM patients.
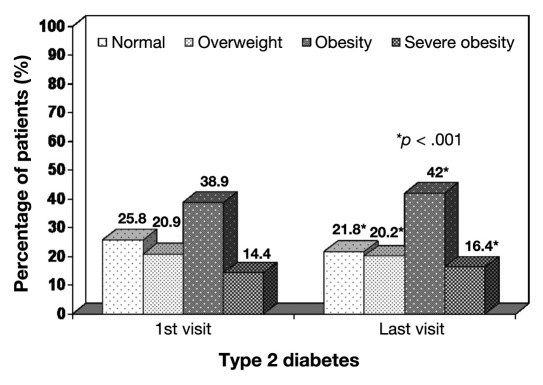
Figure 5 shows the grades of obesity among T2DM patients during the first and last visit to DMDSC, the average follow-up visits being 5.0 ± 8.25. Grades of obesity were defined using the World Health Organization Asia Pacific guidelines for Asian Indians.49 The prevalence of severe obesity (BMI ≥ 30 kg/m2) and obesity (BMI ≥ 25 kg/m2) increased during the final visit compared with the first visit to DMDSC (16.4% vs 14.4%, p < .001, and 42.0% vs 38.9%, p < .001, respectively). The prevalence of overweight (BMI 23–24.9 kg/m2) decreased from 20.9% to 20.2% (p < .001) during the final visit compared with the first.
Figure 5.
Grades of obesity among T2DM patients. Normal, BMI < 23; overweight, BMI 23–24.9; obesity, BMI 25–29.9; severe obesity, BMI ≥ 30.49
The prevalence of various microvascular and macro-vascular complications of diabetes at the first visit to this center was also analyzed. The criteria for diagnosis of DR was the presence of microaneurysms in any field photographed in either eye.50 Neuropathy was diagnosed if the vibratory perception threshold of the right great toe measured by biothesiometry was ≥20.51 Microalbuminuria was diagnosed if the albumin excretion was between 30 and 299 mg/mg of creatinine.42 Peripheral vascular disease was diagnosed if ABI < 0.9,52 and CAD was diagnosed based on a past history of documented myo-cardial infarction and/or electrocardiographic evidence of Q wave and/or ST segment changes.53 Table 4 shows that, compared with T1DM patients, T2DM patients had higher prevalence rates of neuropathy, micro-albuminuria, CAD, and PVD, while prevalence of DR was similar in both T1DM and T2DM patients.
Table 4.
Overall Prevalence of Complications among Type 1 and Type 2 Diabetes Patients Registered at Dr. Mohan's Diabetes Specialities Centre
| Complications | T1DM (%) | T2DM (%) | P value |
|---|---|---|---|
| Neuropathy (biothesiometry: T1DM, n = 1524; T2DM, n = 117,577 ) | 13.0 | 33.1 | <0.001 |
| Retinopathy (gradable retinal photographs: T1DM, n = 1691; T2DM, n = 117,359) | 35.7 | 37.9 | 0.06 |
| Microalbuminuria (estimation of urine microalbumin: T1DM, n = 1633; T2DM, n = 117,498) | 20.0 | 25.5 | <0.001 |
| CAD (electrocardiogram + past history myocardial infarction: n = 93,187) | 9.2 | 17.5 | <0.001 |
| PVD (Doppler: T1DM, n = 1592; T2DM, n = 123,563) | 2.8 | 3.9 | 0.017 |
The prevalence of diabetic complications in relation to duration of diabetes is presented in Table 5. There was a significant increase in the prevalence of diabetic complications with increase in duration of diabetes: 21.5% of the patients with duration of diabetes <5 years had neuropathy, which increased to 68.9% in those with ≥20 years of duration (p for trend < .001). Similarly, 21.0% of patients with duration of diabetes <5 years had DR, which increased to 70.7% in those with ≥20 years of duration (p for trend < .001). With respect to micro-albuminuria, the prevalence increased from 21.0% to 37.7% when the duration of diabetes increased from <5 years to ≥20 years (p for trend < .001). Macrovascular complications, both CAD and PVD, also increased with increasing diabetes duration (p for trend < .001).
Table 5.
Prevalence of Complications in Relation to Duration of Diabetes among Diabetes Patients Registered at Dr. Mohan's Diabetes Specialities Centre
| Complications | Duration of diabetes (years) | |||||
|---|---|---|---|---|---|---|
| <5 (%) | 5–9 (%) | 10–14 (%) | 15–19 (%) | ≥ 20 (%) | Trend χ2p value | |
| Neuropathy | 21.5 | 33.5 | 44.8 | 54.3 | 68.9 | <0.001 |
| Retinopathy | 21.0 | 42.2 | 59.5 | 69.7 | 70.7 | <0.001 |
| Microalbuminuria | 21.0 | 26.3 | 31.2 | 35.2 | 37.7 | <0.001 |
| CAD | 13.7 | 17.5 | 20.2 | 26.1 | 32.8 | <0.001 |
| PVD | 2.5 | 3.8 | 4.8 | 6.7 | 11.3 | <0.001 |
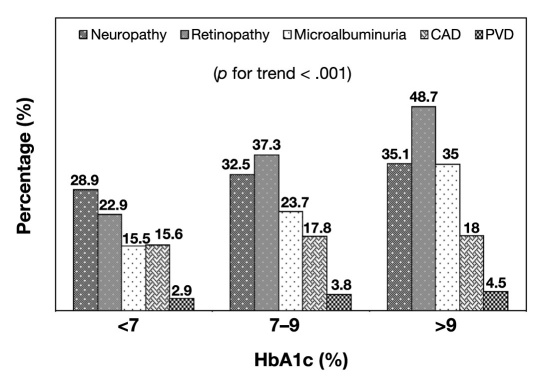
Figure 6 shows the prevalence of diabetic complications computed in relation to HbA1c levels (using HbA1c levels assessed during their first visit). The prevalence of all complications increased while HbA1c levels increased (p for trend < .001).
Figure 6.
Prevalence of complications in relation to HbA1c levels.
Potential Advantages and Disadvantages of the Dr. Mohan's Diabetes Specialities Centre Diabetes Electronic Medical Records System
The factors that influenced the successful implementation and acceptance of a DEMR system at DMDSC included intensive training of all users to bring them to an appropriate level of familiarity with the DEMR system software, an efficient information technology team with a DEMR problem solver, and baseline levels of computer knowledge among the users. Based on the lessons learned with the use of DEMR at our center, the advantages and disadvantages of the DEMR are summarized in Table 6.
Table 6.
Advantages and Disadvantages of Diabetes Electronic Medical Records
| Advantages of DEMRs | Disadvantages of DEMRs |
|---|---|
| 1. Enhances speed of clinical workflow. | 1. Expensive'both initially as well as maintenance costs |
| 2. Helps in standardization of various procedures like medical and clinical examination, and the automation has increased the ability for continuous improvement. | 2. Some doctors and other health care providers find it difficult to use computers. |
| 3. Provides a comprehensive, lifetime digital record for every patient. | 3. If the system fails, it may slow down activities of the center. |
| 4. Efficient delivery of care with streamlined clinical workflow. | 4. Sometimes can affect doctor–patient interaction, as the doctor may be spending more time working at a computer than interacting with a patient. |
| 5. Clinical decisions can be made rapidly, leading to better and faster medical intervention, thus increasing doctor productivity. | 5. Problems may crop up both in software and hardware. |
| 6. Data entered is secure and can be shared between multiple providers to improve quality of care. | |
| 7. Prevents medical errors by having complete patient history on hand. | |
| 8. Complete follow-up data are available, providing a wealth of information at a glance, and moreover, the information is available all the time on the desktop. | |
| 9. Retrieval of past results is easier. | |
| 10. Improves customer service, administrative database such as appointments, registration, billing, and patient follow-up. | |
| 11. Potential data for research |
Conclusions
The DEMR is a valuable tool for both clinical and research applications. The DEMR system has helped DMDSC standardize various procedures and has enhanced the quality assurance program, leading to the center's ISO 9001:2008 certification and the laboratory's accreditation by the National Accreditation Board for Testing and Calibration Laboratories and College of American Patho-logists. We have shown some of the potential benefits of the DEMR system in the current diabetes care system. A strategy focused on financial support, multiple networking, and training of technical support staff may be necessary to promote broader adoption of the DEMR system by medical service providers in India and other developing countries.
Abbreviations
- (ABI)
ankle-brachial index
- (BMI)
body mass index
- (CAD)
coronary artery disease
- (DEMR)
diabetes electronic medical record
- (DMDSC)
Dr. Mohan's Diabetes Specialities Centre
- (DR)
diabetic retinopathy
- (EMR)
electronic medical record
- (HbA1c)
glycated hemoglobin
- (PVD)
peripheral vascular disease
- (SQL)
structured query language
- (T1DM)
type 1 diabetes mellitus
- (T2DM)
type 2 diabetes mellitus
References:
- 1.Wayne Taylor D. Hamilton: The Cameron Institute; 2010. The burden of non-communicable diseases in India. [Google Scholar]
- 2.Raviglione MC, Gupta R, Dye CM, Espinal MA. The burden of drug-resistant tuberculosis and mechanisms for its control. Ann N Y Acad Sci. 2001;953:88–97. doi: 10.1111/j.1749-6632.2001.tb11364.x. [DOI] [PubMed] [Google Scholar]
- 3.International Diabetes Federation diabetes atlas. IDF diabetes atlas. In: Unwin N, Whiting D, Gan D, Jacqmain O, Ghyoot G, editors. 4th ed. Belgium: International Diabetes Federation; 2009. p. 12. [Google Scholar]
- 4.Kristian F, Hanssen KF. The determinants of microvascular complications in diabetics: an overview. In: Pickup J, Williams G, editors. Textbook of diabetes mellitus. Vol. 2. London: Blackwell Scientific Publishers; 1991. [Google Scholar]
- 5.Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, Sundaram V, Rushakoff RJ, Owens DK. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296(4):427–440. doi: 10.1001/jama.296.4.427. [DOI] [PubMed] [Google Scholar]
- 6.Wu RC, Straus SE. Evidence for handheld electronic medical records in improving care: a systematic review. BMC Med Inform Decis Mak. 2006;6:26. doi: 10.1186/1472-6947-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meigs JB, Cagliero E, Dubey A, Murphy-Sheehy P, Gildesgame C, Chueh H, Barry MJ, Singer DE, Nathan DM. A controlled trial of web-based diabetes disease management: the MGH diabetes primary care improvement project. Diabetes Care. 2003;26(3):750–757. doi: 10.2337/diacare.26.3.750. [DOI] [PubMed] [Google Scholar]
- 8.O'Connor PJ, Crain AL, Rush WA, Sperl-Hillen JM, Gutenkauf JJ, Duncan JE. Impact of an electronic medical record on diabetes quality of care. Ann Fam Med. 2005;3(4):300–306. doi: 10.1370/afm.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Selby JV, Karter AJ, Ackerson LM, Ferrara A, Liu J. Developing a prediction rule from automated clinical databases to identify high-risk patients in a large population with diabetes. Diabetes Care. 2001;24(9):1547–1555. doi: 10.2337/diacare.24.9.1547. [DOI] [PubMed] [Google Scholar]
- 10.Barahona P, Azevedo F, Veloso M, Estêvão N, Gallego R. Computerising a guideline for the management of diabetes. Int J Med Inf. 2001;64(2-3):275–284. doi: 10.1016/s1386-5056(01)00191-5. [DOI] [PubMed] [Google Scholar]
- 11.Weber V, Bloom F, Pierdon S, Wood C. Employing the electronic health record to improve diabetes care: a multifaceted intervention in an integrated delivery system. J Gen Intern Med. 2008;23(4):379–382. doi: 10.1007/s11606-007-0439-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bodenheimer T, Grumbach K. Electronic technology: a spark to revitalize primary care? JAMA. 2003;290(2):259–264. doi: 10.1001/jama.290.2.259. [DOI] [PubMed] [Google Scholar]
- 13.Conway PH, Clancy C. Transformation of health care at the front line. JAMA. 2009;301(7):763–765. doi: 10.1001/jama.2009.103. [DOI] [PubMed] [Google Scholar]
- 14.Brisset PR, Gilman CS, Morgan MT, Shabot MM, Hallman E. Who are your CPOE users and how do you train them? Lessons learned at Cedars-Sinai Health System. Medinfo. 2004:1536. [Google Scholar]
- 15.Peters AL, Legorreta AP, Ossorio RC, Davidson MB. Quality of outpatient care provided to diabetic patients. A health maintenance organization experience. Diabetes Care. 1996;19(6):601–606. doi: 10.2337/diacare.19.6.601. [DOI] [PubMed] [Google Scholar]
- 16.Ho M, Marger M, Beart J, Yip I, Shekelle P. Is the quality of diabetes care better in a diabetes clinic or in a general medicine clinic? Diabetes Care. 1997;20(4):472–475. doi: 10.2337/diacare.20.4.472. [DOI] [PubMed] [Google Scholar]
- 17.Morris AD, Boyle DI, MacAlpine R, Emslie-Smith A, Jung RT, Newton RW, MacDonald TM; DARTS/MEMO Collaboration. The diabetes audit and research in Tayside Scotland (DARTS) study: electronic record linkage to create a diabetes register. BMJ. 1997;315(7107):524–528. doi: 10.1136/bmj.315.7107.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sandiford P, Annett H, Cibulskis R. What can information systems do for primary health care? An international perspective. Soc Sci Med. 1992;34(10):1077–1087. doi: 10.1016/0277-9536(92)90281-t. [DOI] [PubMed] [Google Scholar]
- 19.Brailer DJ. Management of knowledge in the modern health care delivery system. J Qual Improv. 1999;25(1):6–19. [Google Scholar]
- 20.Ahman AJ. Guideline and performance measures for diabetes. Am J Manag Care. 2007;13:S41–S46. [PubMed] [Google Scholar]
- 21.Nease DE, Jr, Green LA. ClinfoTracker: a generalizable prompting tool for primary care. J Am Board Fam Pract. 2003;16(2):115–123. doi: 10.3122/jabfm.16.2.115. [DOI] [PubMed] [Google Scholar]
- 22.Renders CM, Valk GD, Griffin S, Wagner EH, Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev. 2001;(1):CD001481. doi: 10.1002/14651858.CD001481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Montori VM, Dinneen SF, Gorman CA, Zimmerman BR, Rizza RA, Bjornsen SS, Green EM, Bryant SC, Smith SA, Translation Project Investigator Group The impact of planned care and a diabetes electronic management system on community-based diabetes care: the Mayo Health System Diabetes Translation Project. Diabetes Care. 2002;25(11):1952–1957. doi: 10.2337/diacare.25.11.1952. [DOI] [PubMed] [Google Scholar]
- 24.O'Connor PJ. Electronic medical records and diabetes care improvement: are we waiting for Godot? Diabetes Care. 2003;26(3):942–943. doi: 10.2337/diacare.26.3.942. [DOI] [PubMed] [Google Scholar]
- 25.Kerr EA, Gerzoff RB, Krein SL, Selby JV, Piette JD, Curb JD, Herman WH, Marrero DG, Narayan KM, Safford MM, Thompson T, Mangione CM. Diabetes care quality in the Veterans Affairs health care system and commercial managed care: the TRIAD study. Ann Intern Med. 2004;141(4):272–281. doi: 10.7326/0003-4819-141-4-200408170-00007. [DOI] [PubMed] [Google Scholar]
- 26.Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. JAMA. 1998;280(15):1339–1346. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- 27.Miller RH, Sim I. Physicians' use of electronic medical records: barriers and solutions. Health Aff (Millwood) 2004;23(2):116–126. doi: 10.1377/hlthaff.23.2.116. [DOI] [PubMed] [Google Scholar]
- 28.Gorman C, Looker J, Fisk T, Oelke W, Erickson D, Smith S, Zimmerman B. A clinically useful diabetes electronic medical record: lessons from the past; pointers toward the future. Eur J Endocrinol. 1996;134(1):31–42. doi: 10.1530/eje.0.1340031. [DOI] [PubMed] [Google Scholar]
- 29.Gandhi TK, Sequist TD, Poon EG, Karson AS, Murff H, Fairchild DG, Kuperman GJ, Bates DW. Primary care clinician attitudes towards electronic clinical reminders and clinical practice guidelines. AMIA Annu Symp Proc. 2003:848. [PMC free article] [PubMed] [Google Scholar]
- 30.Ganesh A, Al-Mujaini A. Electronic medical record system: have we bitten off more than we can chew? OMJ. 2009;24(1):1–3. doi: 10.5001/omj.2009.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lehmann ED. Electronic medical records in clinical diabetes care. Diabetes Technol Ther. 1999;1(4):555–557. doi: 10.1089/152091599317107. [DOI] [PubMed] [Google Scholar]
- 32.Collen MF. Clinical research databases–a historical review. J Med Syst. 1990;14(6):323–344. doi: 10.1007/BF00996713. [DOI] [PubMed] [Google Scholar]
- 33.Judd RM, Kim RJ. Electronic medical records and medical research databases'can they be synonymous? www.touchcardiology.com/files/article_pdfs/Judd.pdf. Accessed November 23, 2010. [Google Scholar]
- 34.National Cancer Institute Confidentiality, data security, and cancer research: perspectives from the National Cancer Institute. www3.cancer.gov/confidentiality.html. Accessed November 23, 2010.
- 35.Miller RH, Sim I. Physicians' use of electronic medical records: barriers and solutions. Health Aff (Millwood) 2004;23(2):116–126. doi: 10.1377/hlthaff.23.2.116. [DOI] [PubMed] [Google Scholar]
- 36.Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, Shields A, Rosenbaum S, Blumenthal D. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360(16):1628–1638. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 37.Mohan V, Deepa R, Rema M, Natarajan A, Devanathan S. Diabetes electronic medical record system – experience at a M.V.Diabetes Specialities Centre, Chennai India. Int Diabetes Monit. 2000;5:35–39. [Google Scholar]
- 38.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO Consultation. Diabet Med. 1998;15(7):539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 39.Mohan V, Vijayaprabha R, Rema M, Premalatha G, Poongothai S, Deepa R, Bhatia E, Mackay IR, Zimmet P. Clinical profile of lean NIDDM in South India. Diabetes Res Clin Pract. 1997;38(2):101–108. doi: 10.1016/s0168-8227(97)00088-0. [DOI] [PubMed] [Google Scholar]
- 40.Rema M, Deepa R, Mohan V. Prevalence of retinopathy at diagnosis among type 2 diabetic patients attending a diabetic centre in South India. Br J Ophthalmol. 2000;84(9):1058–1060. doi: 10.1136/bjo.84.9.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mohan V, Meera R, Premalatha G, Deepa R, Miranda P, Rema M. Frequency of proteinuria in Type 2 diabetes mellitus seen at a diabetes centre in southern India. Postgrad Med J. 2000;76(899):569–573. doi: 10.1136/pmj.76.899.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Varghese A, Deepa R, Rema M, Mohan V. Prevalence of micro-albuminuria in type 2 diabetes mellitus at a diabetes centre in southern India. Postgrad Med J. 2001;77(908):399–402. doi: 10.1136/pmj.77.908.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ashok S, Ramu M, Deepa R, Mohan V. Prevalence of neuropathy in type 2 diabetic patients attending a diabetes centre in South India. J Assoc Physicians India. 2002;50:546–550. [PubMed] [Google Scholar]
- 44.Premalatha G, Ravikumar R, Sanjay R, Deepa R, Mohan V. Comparison of colour duplex ultrasound and ankle-brachial pressure index measurements in peripheral vascular disease in type 2 diabetic patients with foot infections. J Assoc Physicians India. 2002;50:1240–1244. [PubMed] [Google Scholar]
- 45.Mohan V, Deepa R, Rema M. Correlation between fasting plasma glucose and two-hour plasma glucose during oral glucose tolerance test in South Indians. Metabolism. 2000;49(4):455–457. doi: 10.1016/s0026-0495(00)80008-6. [DOI] [PubMed] [Google Scholar]
- 46.Deepa R, Mohan A, Rema M, Haranath SP, Saravanan G, Mohan V. Lipoprotein(a) in South Indian type 2 diabetic subjects in relation to diabetic vascular complications. J Assoc Physicians India. 2002;50(5):657–661. [PubMed] [Google Scholar]
- 47.Kanta Barman K, Padmanabhan M, Premalatha G, Deepa R, Rema M, Mohan V. Prevalence of diabetic complications in fibrocalculous pancreatic diabetic patients and type 2 diabetic patients: a cross-sectional comparative study. J Diabetes Complications. 2004;18(5):264–270. doi: 10.1016/S1056-8727(03)00074-6. [DOI] [PubMed] [Google Scholar]
- 48.Rema M, Sujatha P, Pradeepa R. Visual outcomes of pan-retinal photocoagulation in diabetic retinopathy at one-year follow-up and associated risk factors. Indian J Ophthalmol. 2005;53(2):93–99. doi: 10.4103/0301-4738.16171. [DOI] [PubMed] [Google Scholar]
- 49.World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment. www.wpro.who.int/internet/resources.ashx/.../Redefining+obesity.pdf. Accessed April 21, 1011.
- 50.Early Treatment of Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs–an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology. 1991;98(5 Suppl):786–806. [PubMed] [Google Scholar]
- 51.Pradeepa R, Rema M, Vignesh J, Deepa M, Deepa R, Mohan V. Prevalence and risk factors for diabetic neuropathy in an urban south Indian population: the Chennai Urban Rural Epidemiology Study (CURES-55) Diabet Med. 2008;25(4):407–412. doi: 10.1111/j.1464-5491.2008.02397.x. [DOI] [PubMed] [Google Scholar]
- 52.Premalatha G, Shanthirani S, Deepa R, Markovitz J, Mohan V. Prevalence and risk factors of peripheral vascular disease in a selected South Indian population: the Chennai Urban Population Study. Diabetes Care. 2000;23(9):1295–1300. doi: 10.2337/diacare.23.9.1295. [DOI] [PubMed] [Google Scholar]
- 53.Mohan V, Deepa R, Rani SS, Premalatha G, Chennai Urban Population Study (CUPS No.5) Prevalence of coronary artery disease and its relationship to lipids in a selected population in South India: the Chennai Urban Population Study (CUPS No. 5) J Am Coll Cardiol. 2001;38(3):682–687. doi: 10.1016/s0735-1097(01)01415-2. [DOI] [PubMed] [Google Scholar]