Abstract
Diabetes has emerged as a major public health concern in developing nations. Health systems in most developing countries are yet to integrate effective prevention and control programs for diabetes into routine health care services. Given the inadequate human resources and underfunctioning health systems, we need novel and innovative approaches to combat diabetes in developing-country settings. In this regard, the tremendous advances in telecommunication technology, particularly cell phones, can be harnessed to improve diabetes care. Cell phones could serve as a tool for collecting information on surveillance, service delivery, evidence-based care, management, and supply systems pertaining to diabetes from primary care settings in addition to providing health messages as part of diabetes education. As a screening/diagnostic tool for diabetes, cell phones can aid the health workers in undertaking screening and diagnostic and follow-up care for diabetes in the community. Cell phones are also capable of acting as a vehicle for continuing medical education; a decision support system for evidence-based management; and a tool for patient education, self-management, and compliance. However, for widespread use, we need robust evaluations of cell phone applications in existing practices and appropriate interventions in diabetes.
Keywords: cell phones, decision support system, diabetes, mHealth, wireless
Introduction
Diabetes is currently a major public health problem in developing nations. Of the 284.6 million people with diabetes globally, more than 70% live in low- and middle-income countries.1 Large populous nations such as China and India are witnessing an increase in the burden of diabetes with rapid urbanization and aging of the population.1 Countries in the African and Middle-Eastern nations also have a growing burden of diabetes. It is estimated that global expenditures on diabetes will be at least $316 billion in 2010 and at least $490 billion in 2030.1 The monetary value associated with disability and loss of life as a result of diabetes itself and its related complications account for the largest economic burden.1
Changing to a healthy diet and increasing physical activity has the potential to prevent more than 60% of new-onset diabetes.1 Similarly, a healthy diet, maintaining a normal weight, regular physical activity, and not smoking are central to diabetes management to maintain optimal blood glucose, lipid, and blood pressure levels in order to reduce the risk of future complications, particularly cardiovascular diseases.1 Even in low-resource settings, there is much that can be done to detect undiagnosed cases from the community and provide care and support that will produce and sustain the desired improvements in the health of persons with diabetes. However, public health systems in most developing counties are yet to integrate effective prevention and control programs for diabetes into routine health care services. This brings into focus the tremendous advances in telecommunication technology, which can be harnessed to improve diabetes care. In order to combat the increasing burden of diabetes and its consequences, innovative approaches are needed. The scope of cell phones as a multipurpose portable device for use by both health care providers and patients for diabetes care is discussed in this article.
Importance of Cell Phones in Health Care
The versatility and high levels of accessibility of mobile phone technologies provide enormous potential for novel uses to promote health globally (termed mHealth within the broader eHealth movement). The American Medical Informatics Association Global Partnership Program, the 2008 Rockefeller Foundation month-long conference on eHealth, and the creation of the mHealth Alliance by the United Nations all indicate the extent of importance of mHealth. Two-thirds of all mobile phone users live in low-income and low–middle-income nations,2 and the user base is growing fast. This easy-to-use technology is widely accessed by the illiterate and poor.3 Mobile phones and other mobile technologies require fewer infrastructures than other eHealth systems,4 making them a promising investment for developing countries to strengthen and transform their weak health systems5 and to overcome health care worker shortages.3 Further, many features [e.g., short messaging service (SMS), digital camera, capability of running custom software applications] of cell phone technology can strengthen health services through removing physical barriers to care and service delivery and by improving choice, evidence-based care, management, supply systems, and communication. In addition, it is likely that high-end cell phone (smartphone) prices will continue to drop and capabilities continue to increase (e.g., more sophisticated 3G networks capable of fast Internet connectivity), making them highly cost-effective.
Cell Phones in Diabetes Care
Similar to many other chronic diseases, diabetes requires multidisciplinary care, and patients require education on self-care such as blood-sugar monitoring, adherence to recommendations on diet, exercise, and regular foot inspection. A growing body of evidence suggests that diabetes-management programs need an information technology (IT) backbone in order to be effective.6 From a health system perspective, high-quality data on disease trends, cost, and quality of care are vital to developing, monitoring, and evaluating diabetes prevention and control programs. Increasing the computing power of high-end cell phones, i.e., smartphones, and the rollout of 3G and 4G networks have a positive impact on increasing the access to the Internet in developing countries, particularly in rural areas. This low-cost communication platform is capable of addressing the data requirements of the health system and continued care for people with diabetes as well. The benefits from the application of cell phones in diabetes care falls into three domains: benefits for the health system, benefits for physicians, and benefits for patients (Table 1). A description of each of these domains is discussed here.
Table 1.
Application of Cell Phones in Diabetes Care
| Domains | Application of cell phones |
|---|---|
| • Development of real-time diabetes registries | |
| • Screening (targeted) of undiagnosed diabetes at primary health care settings | |
| • Health promotion messages using SMS | |
| Health system | • Promoting evidence-based management through decision-support software applications |
| • Integrating laboratory/diagnostic applications | |
| • Remote patient monitoring | |
| Physicians | • Tool for CME |
| • Medical reference | |
| Patients | • Patient education |
| • Tool for self-management and reminders for drug intake and follow-up visits |
Benefits to the Health System from the Application of Cell Phones in Health Care
Development of Diabetes Registries
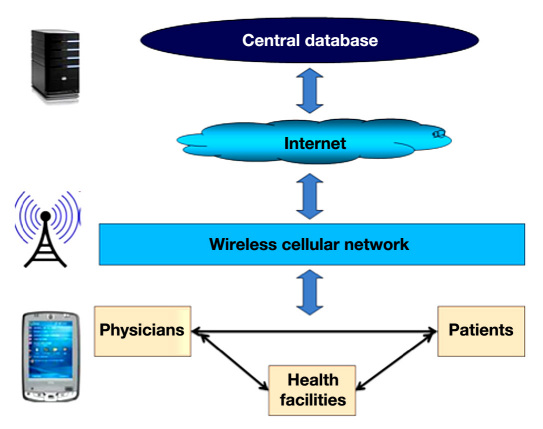
There has been much interest in using information services to systematically collect and manage an individual's or population's health care records in electronic form, i.e., electronic health records (EHR) in order to reduce medical errors and improve quality of care and promote evidence-based medicine. These systems are resource intensive due to the huge investment required for procuring and maintaining computer hardware and networking. However, Internet-capable smartphones can host a limited, basic version of EHR in selected health facilities in developing countries at minimal cost. Such smartphone-based diabetes registries improve diabetes control programs in a number of ways. Data from these facilities will provide long-term tracking of patient data, trends in prescription/management and quality of care, and surveillance data. Unlike paper-based systems, a smartphone-based system can act as a real-time information system, providing high-quality data for planning and monitoring diabetes control programs. A schematic diagram on the architecture of a cellphone-based health information system for diabetes is shown in Figure 1.
Figure 1.
Schematic of the architecture of a cellphone-based health information system for diabetes.
Use of Cell Phones in Screening of Undiagnosed Diabetes
Undiagnosed diabetes accounted for 70–85% of those with diabetes in studies from Africa1 and 71% in India.7 Early detection and treatment could help reduce the burden of complications due to diabetes.1 There are several simple, noninvasive clinical risk score tools available for screening to identify people at high risk of diabetes in the Indian,8–10 Chinese,11 and Thai12 populations. These clinical risk scores utilize noninvasive parameters for computing clinical risk. Custom-made software applications that run on mobile phones can help health workers to compute the risk scores to predict subjects with diabetes or those at high risk for developing diabetes. Mobile phones with integrated glucometers are available in the market.13,14 Interpretation of these screening systems can facilitate a targeted screening approach, which can cut costs tremendously. For example, the health workers can initially screen individuals using the mobile phone, and those predicted to have diabetes or at high risk for diabetes can undergo glucometer screening in the next step. In addition to screening individuals, integrating the screening information from the mobile phone by synchronizing it to the health management information system will help in patient tracking and generating diabetes incidence data in low- and middle-income countries. Such a stepwise approach could also help reduce costs of screening where large populations are involved.15
Cell Phones as a Medium for Information Dissemination
Traditional mass awareness programs rely on news-papers, television, or radio programs. Cell phones, being ubiquitous and portable, are an alternate medium for propagating simple messages on understanding of the signs and symptoms, risk factors, long-term complications, and ways to live with diabetes. Short messaging services can be used effectively for this purpose. Many tele-communication operators and handset manufacturers offers SMS in regional languages. For illiterate groups, voice and picture messaging are alternate options.
Another application of cell phones is in computing calorie consumption, which is often a difficult task. Several mobile phone applications are already on the market that help people with diabetes to make healthier meal choices with information on carbohydrates, portion size, and food labels.16 The challenge will be in making this application affordable and accessible, particularly among those with a low level of education.
Use of Cell Phones in Supporting Evidence-Based Management
Management of diabetes revolves around maintaining optimal control of blood pressure, lipids, and glucose to defined targets. However, in most developing-country settings, a wide gap exists between practice recommenda-tions and delivery of diabetes care. For example, several reports from India have highlighted the suboptimal use of various evidence-based drugs (angiotensin-converting enzyme inhibitors, statins, and hypoglycemic medications) at all levels of care.17–20 Similarly, the Diabcare-China surveys that compared the differences in subject characteristics, glycemic control, diabetes complications, and treatment between 1998 and 2006 in persons with type 2 diabetes in China has highlighted the large gap between guidelines and their actual use.21 These facts highlight the importance of decision support systems to facilitate evidence-based medicine and improve the quality of care. Quinn and colleagues22 carried out a pilot trial to examine the health care provider's adherence to prescribing guidelines using a cell-phone-based diabetes management tool. The results from this study were encouraging, as it facilitated treatment decisions, provided organized data, and reduced logbook review time for analyzing patient data trends. Evidence from effectiveness trials are required to assess the effect size on glycemic control of subjects with diabetes. Furthermore, if found successful, such cell-phone-based decision support systems could help nonphysician health workers in managing uncomplicated cases of diabetes in developing countries where severe shortages of trained physicians is a constraint.
Cell Phones and Laboratory/Diagnostic Applications
Historically, rural areas in developing countries have been deprived of laboratory facilities and expensive manpower such as physicians, thereby seriously affecting access to diabetes care. Bluetooth-enabled glucometers integrated into cell phones is a newer innovation. As discussed earlier, health workers in developing-country settings could use such novel diagnostic tools at the community level for screening and detecting people with undiagnosed diabetes. Because this method reduces the dependence on laboratory facilities for diagnosis, the outreach of diabetes care can be improved even through nonphysician health workers.
Another innovation is the application of cell phone cameras. Digital mobile eye fundus camera for screening of persons with type 2 diabetes mellitus was introduced in the Finnish county of South Ostrobothnia. This study showed feasibility of covering fundus examination in 87% of individuals with diabetes in their nearest health center in a short timeframe.23 In developing-country settings, health workers could be trained to examine these pictures to identify changes due to diabetic retinopathy. Alternatively, picture messages can be sent to physicians for assessments and management.
Remote Monitoring
Remote monitoring is another application for cell phones in diabetes care.14,24 Rami and associates24 evaluated the feasibility of a telemedical support program and its effect on glycemic control in adolescents with type 1 diabetes mellitus. Patients sent their daily data (date, time, blood glucose, insulin dosage) via mobile phone to a central server, and diabetologists sent back their advice via SMS once a week. Glycemic control improved during the telemedical phase compared to the control phase in which the participants used a paper diary for daily monitoring.
Logan and coworkers,25 in another similar study with a before-and-after design, assessed the effect of remote monitoring of uncontrolled ambulatory hypertension in 233 patients. The remote diabetes monitoring system comprised a Bluetooth-enabled home blood pressure monitor, a mobile phone to receive and transmit data, and a central server for data processing. In this pilot study, 24 h ambulatory blood pressure fell significantly. The participants also felt the system was acceptable and effective.
Cell phone applications can also help in remote monitoring of difficult carbohydrate counting. Diabetes Interactive Diary is a novel program designed to be used on a mobile phone.26 This application facilitates the communication between a dietitian and diabetes subjects, particularly in type 1 diabetes, by using a SMS so that the dietitian can monitor glycemic control and suggest insulin doses that correspond directly with the amount of carbohydrate consumed.26 Clinical trial data on effectiveness of this tool are yet to be published.
Benefits to Physicians from the Application of Cell Phones in Health Care
Clinical guidelines and advice and alerts for physicians can be easily delivered through cell phones to stay informed about recent developments.27 This information could complement continuing medical education (CME). There are several cell phone applications currently available for CME: Skyscape CME STAT, MedPage Today, and QuantiaMD. For example, Skyscape, a medical information service provider, offers CME through its Web site Skyscape CME STAT. Registered account holders of CME STAT will receive CME activities on any platform mobile device, personal digital assistant, smartphone, or laptop. A CME article (e.g., articles by experts in the field, news briefs and published journal articles, and reports from conferences and medical meetings) on specialty subjects can be chosen, which is followed by a set of multiple-choice questions. Such services have the potential to provide convenient and widespread availability of CME programs.
Medical reference is another domain where cell phone application could provide solutions for information-intensive clinical practice. For example, Epocrates, an online medical reference company, provides drug reference for clinicians through a mobile platform that is reported to be reducing medical errors and saving time in pharmacy-related queries.27,28
Benefits to Patients from the Application of Cell Phones in Health Care
Patient education and self-management are important components of good diabetes care. Simple-to-follow and always-with-you information will have the maximum influence on subjects with diabetes to make positive choices on diet, physical activity, and compliance to therapy. Cell phones can host software applications that are programmed to provide encouraging messages to remind them of adherence to medication, food intake, physical activity information, and more.
A systematic review that evaluated the evidence on the impact of cell phone interventions for persons with diabetes in improving health outcomes has found that cell phones were useful tools for not only providing general information on diabetes and weight reduction, but also for providing educational intervention and support tailored to an individual care plan.29 The care plan includes monitoring and advice based on individual blood sugar measurements, medications, insulin dose information, diet, weight, and physical activities.29 Most of these studies relied on SMS and voice calls as tools for providing these services. For example, one study compared two groups of individuals with diabetes in which one group was requested to input their blood glucose levels weekly for 3 months to a Web site using their cell phone.30 This group received weekly optimal recommendations for 3 months using SMS while the other group received usual care. Participants in the intervention group had a significant mean change in the 2 h postmeal glucose level while those in the control group had no difference.30
Potential Opportunities of Business-Driven Sustainable Solution
Advances in nanotechnology and biomedical engineering will transform cell phones into an integrated point-of-care solution. As cell phones morph into low-cost smartphones and software applications develop high capabilities that can incorporate advanced functionalities for handling complex disease diagnostic and management solutions at low cost, business opportunities will arise for telecom network providers. In a competitive market, the cost of mobile phone solutions for diabetes will come down, enabling the poor and rural populations to access such services. Government regulation to enforce compliance by the industry to various standards (e.g., context-specific practice guidelines and data standards for interoperability) are essential to avoid the chaotic nature of these IT solutions in future.
Drawbacks of Cell Phone Solutions
The major obstacle in scaling up of mHealth infra-structure is the lack of clear evidence of its benefits. The reasons include lack of well-designed randomized control trials, small size of studies, the quasi-experimental and pre–post design, and inadequate power to evaluate effectiveness and cost-effectiveness.31–33 The small size of the display screen and keypad are other impediments. But advances in technology to produce low-cost, large display screens with touchpad capabilities could improve these bottlenecks in future.
Conclusion
Cell phones offer exciting possibilities to serve as a tool for diabetes prevention and management in developing countries. Given the positive results so far from feasibility trials and the increasing uptake of mobile technologies, cell phones may improve existing practices and inter-ventions in diabetes. However, effectiveness trials as well as evaluation of cost-effectiveness of this technology need to be carried out for providing robust evidence to scale this technology in the prevention and management of diabetes in developing countries.
Acknowledgments
This publication was made possible by award no. HHSN268200900026C from the National Heart, Lung and Blood Institute at the U.S. National Institutes of Health. Vamadevan S. Ajay is supported through the Welcome Trust Capacity Strengthening Strategic Award to the Public Health Foundation of India and a consortium of U.K. universities.
Abbreviations
- (CME)
continuing medical education
- (EHR)
electronic health records
- (ID)
international dollars
- (IT)
information technology
- (SMS)
short messaging service
References
- 1.International Diabetes Federation. 4th ed. Brussels: International Diabetes Federation; 2009. IDF diabetes atlas. [PubMed] [Google Scholar]
- 2.United Nations Department of Economic and Social Affairs. Mobile applications on health and learning. New York: United Nations; 2007. Compendium of ICT applications on electronic government. Vol 1. [Google Scholar]
- 3.Vital Wave Consulting. Washington DC: UN Foundation–Vodafone Foundation Partnership; 2009. mHealth for development: the opportunity of mobile technology for healthcare in the developing world. [Google Scholar]
- 4.Curioso WH. New technologies and public health in developing countries: the Cell PREVEN project. In: Murero M, Rice R, editors. The Internet and health care: theory, research and practice. Mahwah: Lawrence Erlbaum; 2006. [Google Scholar]
- 5.Curioso WH, Mechael PN. Enhancing ‘M-health’ with south-to-south collaborations. Health Aff (Millwood) 2010;29(2):264–267. doi: 10.1377/hlthaff.2009.1057. [DOI] [PubMed] [Google Scholar]
- 6.Bu D, Pan E, Johnston D, Walker J, Adler-Milstein J, Kendrick D, Hook JM, Cusack CM, Bates DW, Middleton B. Boston: Center for Information Technology Leadership; 2007. The value of information technology-enabled diabetes management. [DOI] [PubMed] [Google Scholar]
- 7.Sadikot SM, Nigam A, Das S, Bajaj S, Zargar AH, Prasannakumar KM, Sosale A, Munichoodappa C, Seshiah V, Singh SK, Jamal A, Sai K, Sadasivrao Y, Murthy SS, Hazra DK, Jain S, Mukherjee S, Bandyopadhay S, Sinha NK, Mishra R, Dora M, Jena B, Patra P, Goenka K, DiabetesIndia The burden of diabetes and impaired glucose tolerance in India using the WHO 1999 criteria: prevalence of diabetes in India study (PODIS) Diabetes Res Clin Pract. 2004;66(3):301–307. doi: 10.1016/j.diabres.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Ramachandran A, Snehalatha C, Vijay V, Wareham NJ, Colagiuri S. Derivation and validation of diabetes risk score for urban Asian Indians. Diabetes Res Clin Pract. 2005;70(1):63–70. doi: 10.1016/j.diabres.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 9.Mohan V, Deepa R, Deepa M, Somannavar S, Datta M. A simplified Indian Diabetes Risk Score for screening for undiagnosed diabetic subjects. J Assoc Physicians India. 2005;53:759–763. [PubMed] [Google Scholar]
- 10.Chaturvedi V, Reddy KS, Prabhakaran D, Jeemon P, Ramakrishnan L, Shah P, Shah B. Development of a clinical risk score in predicting undiagnosed diabetes in urban Asian Indian adults: a population-based study CVD Prevention Control. 2008;3:141–151. [Google Scholar]
- 11.Ko G, So W, Tong P, Ma R, Kong A, Ozaki R, Chow C, Cockram C, Chan J. A simple risk score to identify Southern Chinese at high risk for diabetes. Diabet Med. 2010;27(6):644–649. doi: 10.1111/j.1464-5491.2010.02993.x. [DOI] [PubMed] [Google Scholar]
- 12.Aekplakorn W, Bunnag P, Woodward M, Sritara P, Cheepudomwit S, Yamwong S, Yipintsoi T, Rajatanavin R. A risk score for predicting incident diabetes in the Thai population. Diabetes Care. 2006;29(8):1872–1877. doi: 10.2337/dc05-2141. [DOI] [PubMed] [Google Scholar]
- 13.Cho JH, Lee HC, Lim DJ, Kwon HS, Yoon KH. Mobile communication using a mobile phone with a glucometer for glucose control in type 2 patients with diabetes: as effective as an Internet-based glucose monitoring system. J Telemed Telecare. 2009;15(2):77–82. doi: 10.1258/jtt.2008.080412. [DOI] [PubMed] [Google Scholar]
- 14.Istepanian RS, Zitouni K, Harry D, Moutosammy N, Sungoor A, Tang B, Earle KA. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. J Telemed Telecare. 2009;15(3):125–128. doi: 10.1258/jtt.2009.003006. [DOI] [PubMed] [Google Scholar]
- 15.Mohan V, Pradeepa R, Deepa M, Anjana RM, Unnikrishnan RI, Datta M. How to detect the millions of people in India with undiagnosed diabetes cost effectively. In: Rao MS, editor. Medicine update. The Association of Physicians of India; 2010. [Google Scholar]
- 16.theMobileHealthCrowd. Sensei mobile phone diabetes guidance application. http://www.themobilehealthcrowd.com/?q=node/240. Accessed November 26, 2010.
- 17.Nagpal J, Bhartia A. Quality of diabetes care in the middle- and high-income group populace: the Delhi Diabetes Community (DEDICOM) survey. Diabetes Care. 2006;29(11):2341–2348. doi: 10.2337/dc06-0783. [DOI] [PubMed] [Google Scholar]
- 18.Nagpal J, Bhartia A. Cardiovascular risk profile of subjects with known diabetes from the middle- and high-income group population of Delhi: the DEDICOM survey. Diabet Med. 2008;25(1):27–36. doi: 10.1111/j.1464-5491.2007.02307.x. [DOI] [PubMed] [Google Scholar]
- 19.Sharma KK, Gupta R, Agrawal A, Roy S, Kasliwal A, Bana A, Tongia RK, Deedwania PC. Low use of statins and other coronary secondary prevention therapies in primary and secondary care in India. Vasc Health Risk Manag. 2009;5:1007–1014. doi: 10.2147/vhrm.s8017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xavier D, Pais P, Devereaux PJ, Xie C, Prabhakaran D, Reddy KS, Gupta R, Joshi P, Kerkar P, Thanikachalam S, Haridas KK, Jaison TM, Naik S, Maity AK, Yusuf S, CREATE registry investigators Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371(9622):1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 21.Pan C, Yang W, Jia W, Weng J, Tian H. Management of Chinese patients with type 2 diabetes, 1998-2006: the Diabcare-China surveys. Curr Med Res Opin. 2009;25(1):39–45. doi: 10.1185/03007990802586079. [DOI] [PubMed] [Google Scholar]
- 22.Quinn CC, Clough SS, Minor JM, Lender D, Okafor MC, Gruber-Baldini A. WellDoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther. 2008;10(3):160–168. doi: 10.1089/dia.2008.0283. [DOI] [PubMed] [Google Scholar]
- 23.Lemmetty R, Mäkelä K. Mobile digital fundus screening of type 2 diabetes patients in the Finnish county of South-Ostrobothnia. J Telemed Telecare. 2009;15(2):68–72. doi: 10.1258/jtt.2008.080804. [DOI] [PubMed] [Google Scholar]
- 24.Rami B, Popow C, Horn W, Waldhoer T, Schober E. Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. Eur J Pediatr. 2006;165(10):701–705. doi: 10.1007/s00431-006-0156-6. [DOI] [PubMed] [Google Scholar]
- 25.Logan AG, McIsaac WJ, Tisler A, Irvine MJ, Saunders A, Dunai A, Rizo CA, Feig DS, Hamill M, Trudel M, Cafazzo JA. Mobile phone-based remote patient monitoring system for management of hypertension in diabetic patients. Am J Hypertens. 2007;20(9):942–948. doi: 10.1016/j.amjhyper.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 26. ClinicalTrials.gov. Assessing the effectiveness of diabetes inter-active diary (DID) in diabetes management. http://clinicaltrials.gov/show/NCT00482443. Accessed November 26, 2010.
- 27.Sarasohn-Kahn J. Oakland: California Healthcare Foundation; 2010. How smatphones are changing health care for consumers and providers. [Google Scholar]
- 28. Epocrates Inc. http://www.epocrates.com/. Accessed November 26, 2010.
- 29.Krishna S, Boren SA. Diabetes self-management care via cell phone: a systematic review. J Diabetes Sci Technol. 2008;2(3):509–517. doi: 10.1177/193229680800200324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim HS. Effects of Web-based diabetic education in obese diabetic patients. Taehan Kanho Hakhoe Chi. 2005;35(5):924–930. doi: 10.4040/jkan.2005.35.5.924. [DOI] [PubMed] [Google Scholar]
- 31.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health. 2009;15(3):231–240. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 32.Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Global Health. 2006;2:9. doi: 10.1186/1744-8603-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blaya JA, Fraser HS, Holt B. E-health technologies show promise in developing countries. Health Aff (Millwood) 2010;29(2):244–251. doi: 10.1377/hlthaff.2009.0894. [DOI] [PubMed] [Google Scholar]