Abstract
The purpose of the present study is to describe the technique of margin convergence for U-shaped rotator cuff tears and report the clinical outcomes and ultrasonography with a minimum of 2 years follow-up. Three hundred eleven patients with a rotator cuff tear were prospectively enrolled in a registry at one institution. Inclusion criteria included any patient undergoing arthroscopic margin convergence for a rotator cuff tear. Exclusion criteria included open or mini-open rotator cuff repairs or suture anchor fixation to the cuff insertion without margin convergence. The outcome measurements included physical examination, manual muscle testing, the American Shoulder and Elbow Surgeons (ASES) score, and ultrasonography. Nineteen patients met the study criteria and 13 were available for 2-year follow-up (68.4%). The mean age of this cohort was 62.2 ± 7.5 years with a mean pre-operative rotator cuff tear size of 4.0 ± 1.6 cm. The ASES score increased significantly from 50.0 ± 17.7 before surgery to 83.3 ± 19.5 at 2 years (P = 0.01). The active forward elevation also improved from 156.2 ± 11.9° before surgery to 168.0 ± 12.1 at 2 years (P = 0.03). The active external rotation 54.4 ± 14.5 at baseline and improved to 57.1 ± 19.1 at 2 years (P = 0.04). The strength also increased significantly from 6.7 ± 6.4 to 10.6 ± 4.9 lb at 1 year (P = 0.048). The post-operative ultrasound demonstrated that 46.2% of rotator cuff tears were healed at 2 years. In conclusion, margin convergence is a useful technique for U-shaped tears that are difficult to mobilize.
Keywords: margin convergence, rotator cuff, shoulder arthroscopy
Introduction
In 1944, McLaughlin et al. advocated a combination of side-to-side tendon-to-tendon sutures and end-on tendon-to-bone sutures for the repair of U-shaped rotator cuff tears. However, this repair technique did not become mainstream in orthopedics because the trend became medial-to-lateral cuff repair regardless of the shape of the tear. This trend changed when Burkhart et al. recognized that massive mobilization of large U-shaped tears created excessive tension at the apex of the tear. Due to these findings, they described the incredible mechanical advantage from side-to-side closure and coined the term margin convergence [2]. This repair technique enhances the security of fixation by decreasing the mechanical strain at the margins of the tear.
In 2001, Burkhart et al. published the long-term functional results of 59 patients that underwent arthroscopic rotator cuff repair and analyzed the results based on the repair technique (margin convergence versus direct tendon-to-bone repair) [3]. Preoperative and postoperative function was assessed by means of a modified University of California at Los Angeles (UCLA) scoring system. In the earlier cases in this series, margin convergence was used alone if the converged margin came to rest solidly over the prepared tuberosity making tendon-to-bone healing possible. However, in the later cases, the converged margin was repaired to bone with suture anchors in order to maximize tendon-to-bone fixation. This study included 25 patients that underwent margin convergence (15 with margin convergence only and 10 with margin convergence plus anchors). Crescent-shaped tears were repaired directly to bone without margin convergence. This study demonstrated that U-shaped tears repaired by margin convergence have results comparable to those of crescent-shaped tears repaired directly by a tendon-to-bone technique [3]. One of the limitations of this study is that the rotator cuff integrity was not assessed.
Investigations into the integrity of the rotator cuff have included the use of ultrasonography [1, 8, 9, 13, 15, 17], magnetic resonance imaging [11, 12], and arthrography [12]. The purpose of the present study is to describe the technique and indications for the use of margin convergence in the treatment of U-shaped tears and to report the clinical outcomes and rate of healing by post-operative ultrasound.
Materials and Methods
Three hundred and eleven patients with a rotator cuff tear were prospectively enrolled in a registry at one institution over a 3-year period and followed in a prospective fashion. The study proposal was approved by the hospital institutional review board and informed consent was obtained for all patients prior to the procedure by the study coordinator. The inclusion criteria for the present study were any patient who had undergone arthroscopic margin convergence of a rotator cuff tear. The exclusion criteria were patients who had undergone open or mini-open rotator cuff repairs, suture anchor fixation to the cuff insertion without margin convergence, revision rotator cuff repair, or glenohumeral osteoarthritis.
Patients that met the study criteria and completed the informed consent completed a preoperative questionnaire, which included a demographic and social history, surgical history, and detailed medical history. Demographic information, use of pain medications (anti-inflammatories and narcotics), smoking history, onset and duration of symptoms, and number of steroid injections of the affected shoulder were recorded. The intra-operative factors included both diagnostic information as well as concomitant procedures that were performed at the time of surgery. Intra-articular data included chondral lesions (location, size, and depth), labral pathology (location and size), and biceps tear (none, incomplete, or complete).
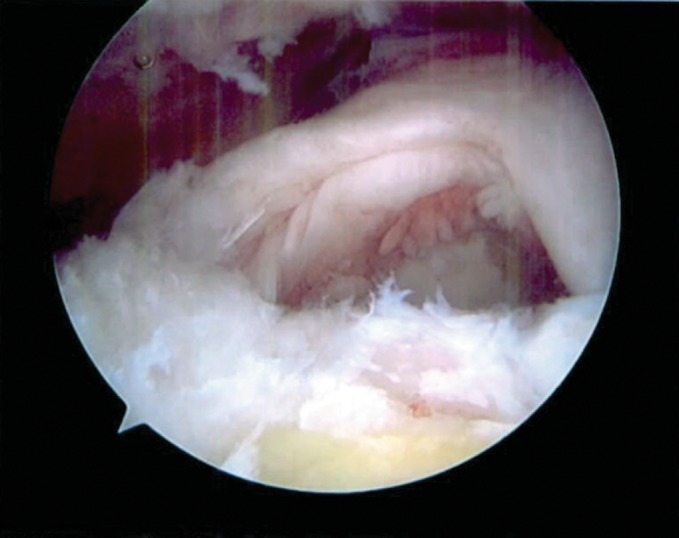
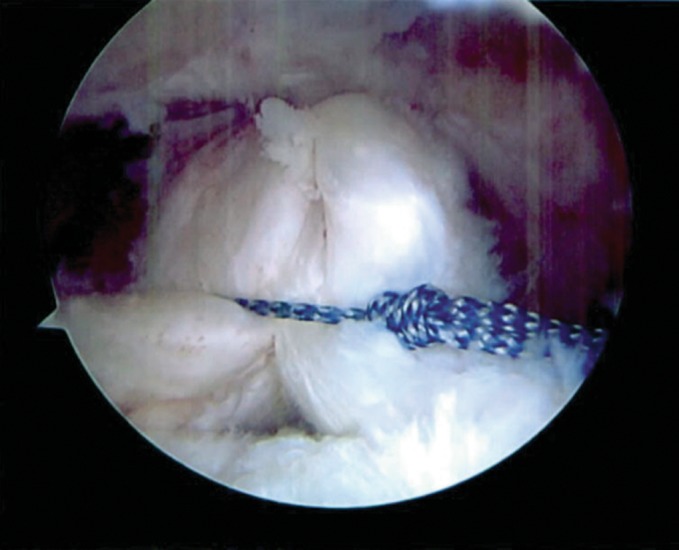
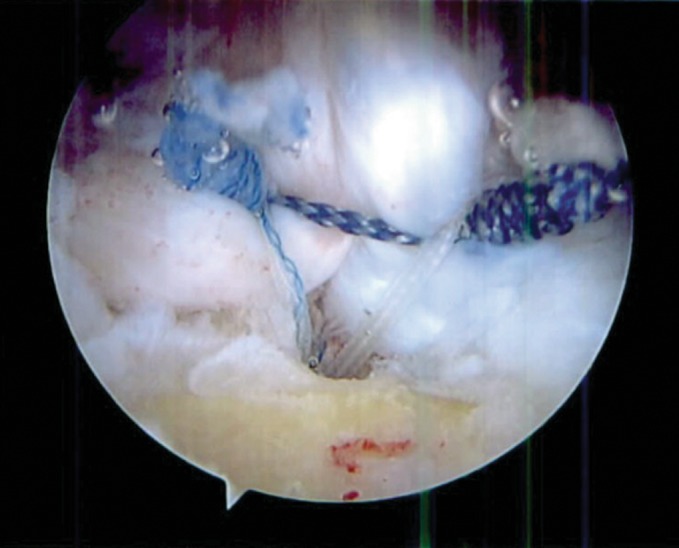
All tears in this study had attempted rotator cuff tear in the standard fashion using direct tendon-to-bone fixation with suture anchors. A tendon grasper was used to assess the direction of maximum mobility of the tear in order to determine if a relatively tension-free repair to bone could be achieved. The U-shaped tears were difficult to mobilize and thus repaired by margin convergence with side-to-side sutures (Fig. 1). This was performed by using a combination of Penetrator™ and BirdBeak™ suture passers (Arthrex Inc, Naples, FL, USA). While viewing with the scope in a lateral subacromial position, permanent braided sutures were passed through the posterior and anterior leaves of the cuff tear (Fig. 2). Most of the cuff tears in this study required two to four side-to-side sutures which were tied sequentially from medial to lateral to achieve margin convergence. The free margin of the rotator cuff tear was then repaired to bone with a variable number of suture anchors according to surgeon preference (Figs. 3 and 4).
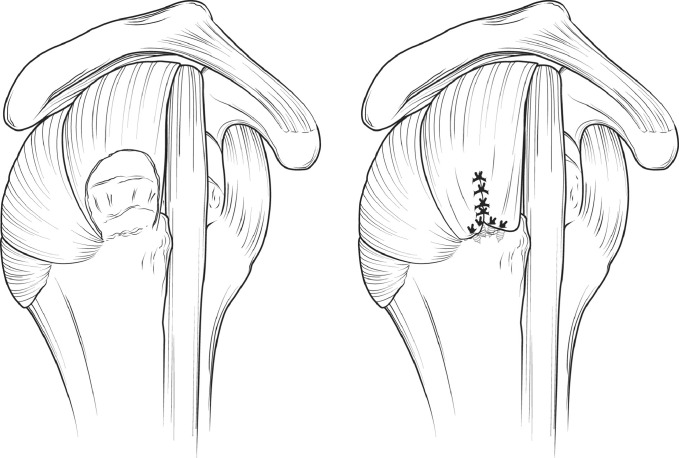
Fig. 1.
Arthroscopic image of a U-shaped rotator cuff tear while viewing from the lateral portal
Fig. 2.
Arthroscopic image while viewing from the lateral portal demonstrating side-to-side suture passage as part of the margin convergence technique
Fig. 3.
Arthroscopic image while viewing from the lateral portal demonstrating the final repair after side-to-side sutures have been placed combined with suture anchor repair
Fig. 4.
Artist’s depiction of a rotator cuff tear with a U-shaped configuration. Margin convergence has been performed with side-to-side sutures and then a variable number of suture anchors are used for tendon-to-bone healing depending on surgeon preference
Rotator cuff pathology was described in terms of tear thickness (full or partial), lesion size, and tendon(s) involved (single or multiple). The details of the arthroscopic rotator cuff repair included information regarding suture anchor row configuration (single or double), number of suture anchors, tissue quality (normal or poor), and any additional procedures were also recorded including acromioplasty (yes or no), superior glenoid labrum lesions (none, debridement, or repair), acromioclavicular (AC) joint (none, AC joint coplane, distal clavicle excision), or biceps (none, debridement, tenotomy, or tenodesis). A physical examination including range of motion and strength testing and the American Shoulder and Elbow Surgery (ASES) score, a validated shoulder-specific outcome assessment instrument [14], were completed pre-operatively and post-operatively at 1 and 2 years. Strength testing was performed with a handheld dynamometer (Lafayette Manual Muscle Test System; Lafayette Instrument Company, Lafayette, IN, USA). A limited targeted ultrasound of the shoulder was performed at 1 and 2 years after arthroscopic rotator cuff repairs and was interpreted by a single musculoskeletal radiologist. The ultrasound images were stored digitally on a workstation (ALI, Toronto, Canada) and healing status (intact or defect), tendon involvement, and surface area of defect were recorded. All other collected data was stored using under the direction of the study coordinator using System for Collaborative Transitional Research (SCTR). SCTR is both 21 Clinical Review Panel (CRP) part 11 and Health Insurance Portability and Accountability Act compliant.
Results
Nineteen patients underwent rotator cuff repair with margin convergence and 13 (68.4%) patients completed 2-year follow-up. The mean age of the patients was 62.2 ± 7.5 years. There were six males (46.2%) and seven females (53.8%).
At the index procedure, the rotator cuff tear and associated pathology were recorded. The mean rotator cuff tear size was 4.0 ± 1.6 cm, a single tendon tear occurred in 42.1% and a multiple tendon tear occurred in 57.9% of cases. The surgeons also determined the quality of the torn rotator cuff to be normal in 26.4% of patients and degenerative in 73.7% of patients. The suture anchor configuration was single row in 35.7% and double row in 64.3%. The average number of suture anchors per case was 2.2 (range 2–4). Any additional pathology underwent concomitant surgical treatment at the time of the arthroscopic rotator cuff repair. The bicep tendon was debrided in 26.3% of cases and a tentomy was performed in 21.1% of cases. The acromioclavicular joint underwent AC joint co-plane in 26.3% of cases and distal clavicle excision was performed in 36.8% of cases.
The ASES score increased significantly from 50.0 ± 17.7 before surgery to 83.3 ± 19.5 at 2 years (P = 0.01). The strength also increased significantly from 6.7 ± 6.4 to 10.6 ± 4.9 lb at 1 year (P = 0.048). The active forward elevation also improved from 156.2 ± 11.9° before surgery to 168.0 ± 12.1 at 2 years (P = 0.03). The active external rotation 54.4 ± 14.5 at baseline and improved to 57.1 ± 19.1 at 2 years (P = 0.04). The post-operative ultrasound demonstrated that 46.2% of the rotator cuff repairs were healed at 2 years.
Discussion
Burkhart coined the term “margin convergence” and demonstrated how this technique decreases strain by increasing the cross-sectional area and decreasing the length of the tear [2]. In addition, if the cuff margin is subsequently repaired to bone, the side-to-side repair should be protective of the repaired margin to bone. Theoretically, this reduced strain should lead to an increased rate of healing based on postoperative ultrasound examinations.
Although rotator cuff repairs are known to have good functional results, arthrographic or ultrasonographic data have shown a defect rate ranging from 25% to 94.4% [4, 5, 7, 8]. The relationship of clinical outcome and tendon healing remains controversial. Several studies have demonstrated that healed rotator cuff tendons provide increased range of motion and strength [6, 8, 10, 18, 19]. Other studies have demonstrated that clinical outcome is independent of tendon healing [11, 12].
Harryman et al. evaluated the results of 105 operative repairs of tears of the rotator cuff of the shoulder with an average of follow-up of 5 years [8]. Based on postoperative ultrasound, 68% of cuffs remained intact. Patients with an intact rotator cuff had significantly better strength, active range of motion, and function in terms of the patient’s ability to perform activities of daily living. They concluded that the integrity of the rotator cuff at the time of follow-up, not the size of the tear at the time of the repair, is the major determinant of the outcome of an operative repair of a rotator cuff tear.
Galatz et al. evaluated 18 patients who had a complete arthroscopic repair of a tear measuring >2 cm in the transverse dimension [5]. Based on ultrasound evaluation, recurrent tears were seen in 94.4% of patients. However, despite the high rate of recurrent defects, 88.9% of patients had excellent pain relief and improvement in the ability to perform activities of daily living at 12 month follow-up. These results deteriorated slightly after 2 years with only 63.2% of patients having an ASES score ≥80 [5].
Huijsmans et al. evaluated 264 patients that underwent an arthroscopic rotator cuff repair with double-row fixation and performed ultrasonography to assess the integrity of the cuff [10]. Overall, the ultrasonagraphy demonstrated an intact rotator cuff in 83% of patients. Based on tear size, 47% of the massive cuff tears, 78% of the large tears, 93% of the medium tears, and 88% of the small tears healed. In the group with an intact tear based on ultrasonography, there was a significant increase in strength and active elevation. However, there was no difference between groups with regards to pain scores.
Large and massive rotator cuff tears pose a challenging problem for orthopedic surgeons. Over the past several years, there has been emerging technology and more advanced techniques to optimize the biomechanical fixation of arthroscopically repaired rotator cuff tears including margin convergence, massive cuff stitch, double-row suture anchor configuration, transosseous equivalent suture bridge, etc. We found a defect rate of 46.2% after arthroscopic rotator cuff repair with margin convergence and the majority of cases utilized double-row suture anchor configuration. The difference between those that are able to heal is likely related to the degree of rotator cuff degeneration and the patients in the present study represent a group with advanced rotator cuff pathology. The mean cuff tear size was 4.0 cm with 57.9% multiple tendon tears which have been shown to have a ninefold increased likelihood of tendon defect based on post-operative ultrasonography [16]. Rotator cuff tears in the setting of tissue degeneration, acromioclavicular joint pathology, and bicep pathology are also at a three-, four-, and 11-fold increased risk of a tendon defect, respectively [16]. Given the degree of rotator cuff degeneration and associated pathology of this cohort, a 46.2% tendon defect at 2 years is not surprising. Even though the biomechanical construct has been maximized, an intact tendon is largely dependent on biologic healing of the tendon-to-bone junction. Rotator cuff degeneration is a complex process and in order to improve the rate of healing in the future, potential therapeutic modalities need to be developed. Until adjuvant biologic modalities are developed to augment tendon healing, the authors advocate early repair of rotator cuff tears in order to increase likelihood of tendon healing and successful clinical outcomes.
There are several limitations to this study. First, despite exhaustive attempts to contact patients, only 68.4% of patients completed 2-year follow-up. Second, the clinical outcomes or post-operative healing rate by ultrasound cannot be solely attributed to the margin convergence technique because multiple surgical techniques were combined with the margin convergence such as single- and double-row usage of suture anchors.
This study describes the technique of margin convergence for rotator cuff repair in U-shaped tears. This can be a useful technique to decrease strain and help obtain a relatively tension-free repair. The moderate rate of healing in this study is likely related to chronicity of the tear, large tear size, bicep pathology, acromioclavicular joint pathology, and poor quality of rotator cuff tendon. Long-term studies are necessary in order to determine if patients with persistent rotator cuff tears are associated with deteriorating clinical outcomes.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of this study, that all investigations were conducted in conformity with ethical principles of research.
Level of Evidence: Level IV: Case Series
References
- 1.Bretzke CA, Crass JR, Craig EV, Feinberg SB. Ultrasonography of the rotator cuff. Normal and pathologic anatomy. Invest Radiol. 1985;20:311–5. doi: 10.1097/00004424-198505000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart SS, Athanasiou KA, Wirth MA. Margin convergence: a method of reducing strain in massive rotator cuff tears. Arthroscopy. 1996;12:335–8. doi: 10.1016/S0749-8063(96)90070-5. [DOI] [PubMed] [Google Scholar]
- 3.Burkhart SS, Danaceau SM, Pearce CE. Arthroscopic rotator cuff repair: analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy. 2001;17:905–12. doi: 10.1053/jars.2001.26821. [DOI] [PubMed] [Google Scholar]
- 4.Calvert PT, Packer NP, Stoker DJ, Bayley JI, Kessel L. Arthrography of the shoulder after operative repair of the torn rotator cuff. J Bone Joint Surg Br. 1986;68:147–50. doi: 10.1302/0301-620X.68B1.3941132. [DOI] [PubMed] [Google Scholar]
- 5.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–24. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–15. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 8.Harryman DT, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982–9. doi: 10.2106/00004623-199173070-00004. [DOI] [PubMed] [Google Scholar]
- 9.Hodler J, Fretz CJ, Terrier F, Gerber C. Rotator cuff tears: correlation of sonographic and surgical findings. Radiology. 1988;169:791–4. doi: 10.1148/radiology.169.3.3055040. [DOI] [PubMed] [Google Scholar]
- 10.Huijsmans PE, Pritchard MP, Berghs BM, van Rooyen KS, Wallace AL, de Beer JF. Arthroscopic rotator cuff repair with double-row fixation. J Bone Joint Surg Am. 2007;89:1248–57. doi: 10.2106/00004623-200706000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Klepps S, Biship J, Lin J, Cahlon O, Strauss A, Hayes P, Flatow EL. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32:1716–22. doi: 10.1177/0363546504265262. [DOI] [PubMed] [Google Scholar]
- 12.Liu SH, Baker CL. Arthroscopically assisted rotator cuff repair: correlation of functional results with integrity of the cuff. Arthroscopy. 1994;10:54–60. doi: 10.1016/S0749-8063(05)80293-2. [DOI] [PubMed] [Google Scholar]
- 13.Mack LA, Nyberg DA, Matsen FA., 3rd Sonographic evaluation of the rotator cuff. Radiol Clin North Am. 1988;26:161–77. [PubMed] [Google Scholar]
- 14.Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11:587–94. doi: 10.1067/mse.2002.127096. [DOI] [PubMed] [Google Scholar]
- 15.Middleton WD, Reinus WR, Totty WG, Melson CL, Murphy WA. Ultrasonographic evaluation of the rotator cuff and biceps tendon. J Bone Joint Surg Am. 1986;68:440–50. doi: 10.2106/00004623-198668030-00020. [DOI] [PubMed] [Google Scholar]
- 16.Nho S, Shindle MK, Adler RS, Warren RF, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: subgroup analysis. J Shoulder Elbow Surg. 2009;18:697–704. doi: 10.1016/j.jse.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 17.Packer NP, Calvert PT, Bayley JI, Kessel L. Operative treatment of chronic ruptures of the rotator cuff of the shoulder. J Bone Joint Surg Br. 1983;65:171–5. doi: 10.1302/0301-620X.65B2.6826624. [DOI] [PubMed] [Google Scholar]
- 18.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997;344:275–83. doi: 10.1097/00003086-199711000-00027. [DOI] [PubMed] [Google Scholar]
- 19.Wilson FV, Hinov V, Adams G. Arthroscopic repair of full-thickness tears of the rotator cuff: 2- to 14-year follow-up. Arthroscopy. 2002;18:136–44. doi: 10.1053/jars.2002.30443. [DOI] [PubMed] [Google Scholar]