Abstract
Degenerative lumbar scoliosis is a coronal deviation of the spine that is prevalent in the elderly population. Although the etiology is unclear, it is associated with progressive and asymmetric degeneration of the disc, facet joints, and other structural spinal elements typically leading to neural element compression. Clinical presentation varies and is frequently associated with axial back pain and neurogenic claudication. Indications for treatment include pain, neurogenic symptoms, and progressive cosmetic deformity. Non-operative treatment includes physical conditioning and exercise, pharmacological agents for pain control, and use of orthotics and invasive modalities like epidural and facet injections. Operative treatment should be contemplated after multi-factorial and multidisciplinary evaluation of the risks and the benefits. Options include decompression, instrumented stabilization with posterior or anterior fusion, correction of deformity, or a combination of these that are tailored to each patient. Incidence of perioperative complications is substantial and must be considered when deciding appropriate operative treatment. The primary goal of surgical treatment is to provide pain relief and to improve the quality of life with minimum risk of complications.
Keywords: degenerative scoliosis, adult scoliosis, adult deformity, spinal stenosis, secondary scoliosis
Introduction
Degenerative scoliosis needs to be distinguished from adult scoliosis as it is a result of progressive degeneration of structural spinal elements leading to spinal column malalignment, whereas adult scoliosis is a collective term (inclusive of degenerative scoliosis) comprising of all spinal deformities in a skeletally mature individual. The prevalence of scoliosis in the adult population has been reported as ranging from 2% to 32%; a recent study targeting elderly volunteers showed a prevalence of more than 60% [3, 36, 37]. The prevalence of degenerative scoliosis ranges from 6% to 68% [3, 4, 12–16]. With an aging population in the USA and an increased attention to quality of life versus cost issues in the current healthcare environment, degenerative scoliosis has become a considerable health care concern, not only cosmetically, but also, as a cause of significant pain and disability [6].
Traditionally, significant attention was given to scoliosis of childhood and adolescent, while adult scoliosis was dealt with only by a few surgeons. For reasons of perioperative morbidity, lack of powerful instrumentation, high incidence of neurological deficit, and relative rigidity of the deformity, the risk–benefit curve in the treatment of adults with scoliosis usually tilted towards non-operative modalities [6]. With advancement of surgical techniques and instrumentation, the management of spinal deformity in the adult has gone through a significant evolution during the past decade. This has been supported with the multidisciplinary progress in anesthesia for spinal surgery and radiology by more sophisticated and precise diagnostic imaging and differentiated application of invasive and functional diagnostic tests. Increased patient awareness towards quality of life issues and disinclination to accept their limitations make adult deformity, inclusive of degenerative scoliosis, a much more frequent problem in a general spine practice than idiopathic adolescent scoliosis [6].
Definition
Adult scoliosis is defined as a spinal deformity in a skeletally mature patient with a Cobb angle of more than 10° in the coronal plain [6, 17, 18]. Primary degenerative scoliosis or “De Novo” scoliosis is a deformity developing in a previously straight spine, caused by accelerated degeneration of the spine in middle age with progressive disc and facet degeneration. This leads to generalized spondylosis, which, in some cases, results in instability that leads to vertebral rotation, lateral listhesis, or spondylolisthesis. This should be distinguished from adult idiopathic scoliosis as both have varied etiology, presentation, and choice of treatment.
Classification
Aebi et al. classified adult scoliosis into three major types [6]. Type I scoliosis is the primary degenerative or de novo scoliosis which develops after skeletal maturity and is characterized by minimal structural vertebral deformities, advanced degenerative changes, and a predominance of lower lumbar curves. It results from asymmetric degeneration of disc and facet joints, and osteoporotic compression fractures. The new onset of deformity can be confirmed through obtaining old photographs of the patient and charting their posture. It is best distinguished from adult idiopathic scoliosis by radiographic confirmation of a straight spine during adulthood with subsequent development [6, 22].
Type II scoliosis is the progressive idiopathic deformity that develops before skeletal maturity but becomes symptomatic in adult life. It does not confine itself to the lumbar spine alone. It can involve the cervical and thoracic spine as well, appearing during childhood or adolescence and progressing into adult life. As the patient ages, this preexisting scoliosis can be combined with superimposed secondary degeneration and imbalanced in its natural history. A better understanding is essential before a treatment plan is contemplated as symptomatology, expectations and outcomes may vary [6, 22, 23, 39].
Type III Secondary Degenerative Scoliosis
Scoliosis following idiopathic or other forms of scoliosis or occurring in the context of a pelvic obliquity due to a leg-length discrepancy, hip pathology, or a lumbo-sacral transitional anomaly, mostly located in the thoraco-lumbar, lumbar, or lumbo-sacral [6].
Scoliosis secondary to metabolic bone disease (mostly osteoporosis) combined with asymmetric arthritic disease and/or vertebral fractures [6].
Schwab described a comprehensive clinical impact classification based on analysis of a large adult scoliosis population [3]. This classification permitted a simple approach of radiographic analysis using established markers of disability by outcomes measurement instruments (Scoliosis Research Society (SRS) and ODI) [3].
The etiological and radiological classification systems proposed for adult lumbar spinal deformity has not been agreed upon as each established system had significant limitations in the application to adult spinal deformity to accurately characterize a disorder, to guide treatment and decision-making, and to form a basis for the uniform reporting of results of care that may lead to an evidence-based approach to care. The recognition of symptomatic degenerative changes within the deformity, including stenosis, spondylolisthesis, and rotational subluxation, is critical for an effective classification system in the adult. Similarly, global imbalance of the spine in the sagittal and coronal plane is rare in adolescent idiopathic scoliosis but has an important impact on health status and treatment options in the adult patient. Systems used to describe adolescent idiopathic scoliosis (AIS) are the King and Lenke classifications, but these do not provide any guidelines for treating patients with degenerative lumbar scoliosis [1, 2].
Hence, the SRS classification was proposed to introduce a system for adult deformity that would correctly categorize adults with spinal deformity and to provide an outline that would be useful in comparing treatment and outcomes between centers. The principal role of this classification system is to provide a taxonomy or framework for adult spinal deformity and to enable the comparison of similar cases between centers and their inclusion in multicenter studies. A secondary role of the SRS Adult Deformity Classification System is to present an evidence-based approach to the management of adult deformity and degenerative scoliosis in particular [9].
Standard terminology has been established in a glossary by the SRS, which is available on the SRS web site [1, 2, 5, 19] and serves as a common language for defining spinal deformity. A better understanding of the terminology is with the different classification methods utilized to differentiate between them.
Pathophysiology and Natural History
Degenerative adult scoliosis, specifically in the lumbar spine, takes its origin from asymmetric degenerative disc disease following a vicious cycle. It is consistent in its natural course in a majority of cases, though some patients may have sudden decompensation or extrusion of a desiccated disc fragment leading to a sudden neurologic deficit.
The basic premise of the pathophysiology is asymmetric degeneration of the disc and the facet joints at different levels leading to asymmetric loading of the spinal segment, and consequently, of the lumbar spinal column, manifesting in a three-dimensional deformity. The asymmetric loading, coupled with degeneration, triggers a vicious circle enhancing curve progression. This is fuelled by common metabolic bone disorders like osteoporosis especially in post-menopause female patients leading to further asymmetric deformation and collapse in the weakened osteoporotic vertebra with subsequent curve progression.
The destruction of structural spinal elements like discs, facet joints, and joint capsules responsible for stability leads to uni- or multi-segmental, multi-directional instability and can manifest as spondylolisthesis or translational or rotary olisthesis. The biological reaction is the formation of osteophytes at facet joint and vertebral end plates contributing to increasing narrowing of the spinal canal with facet joint and ligamentum flavum hypertrophy and calcification. Effective narrowing of the spinal canal caliber causes central and lateral recessal spinal stenosis [6, 7]. Instability and collapse of the disc height lead to foraminal stenosis, with radicular pain or neurogenic claudication-type pain.
There are distinct differences between the natural history of untreated AIS and degenerative scoliosis. Unlike the slow progression of AIS, degenerative scoliosis may progress at a rate of 3° or more per year [5]. Factors affecting the rate of curve progression are the curve is greater than 30°, there is more than 30% apical vertebral rotation, 6 mm of lateral listhesis or greater, and degenerative disc disease at the lumbo-sacral junction [5]. The quality of bone is another significant factor in menopausal women.
Clinical Presentation
Scoliosis in adult population presents with pain as the chief complaint in 90% of patients [5, 6, 9, 24]. Pain patterns in these patients may follow a simple or complex pain syndrome; hence, it is of key importance to question the characteristics of pain in every individual suffering from degenerative scoliosis to evaluate the source of pain during their first encounter. It directly impacts the choice of treatment, inclusive of the type of operation if needed, and thus affects the outcome. Malalignment of the column gives rise to axial or central pain located over the convexity of the curve and diffuses in nature. It is believed to be the result of muscle fatigue of the para-spinal musculature and is activity related, often exarcebated with upright posture for longer duration, and relieved by lying down. Back pain can also be a result of obvious or subtle instability of one or more spinal segments. Para-spinal muscle fatigue is a marked symptom of fatback syndrome of the lumbar spine as the column is decompensated and overloaded. Patients often feel as if they are “tipping over.” Sore musculature may result in trigger point pain at muscle insertions around the iliac crest and sacrum or may be diffused over the entire spinal area [6]. The back pain can be combined with radicular leg pain and/or neurogenic claudication and is the second important symptom of adult degenerative scoliosis. Nerve roots are dynamically stretched due to traction along the convexity and compressed by foraminal narrowing in the concavity giving rise to true radicular pain [11]. Coupled with central and recessal stenosis, root compression and/or traction can result in debilitating leg pain on standing or walking [5, 6].
Neurologic deficit may result as an insidious symptom due to curve progression or a sudden event due to a disc fragment herniation or acute curve decompensation. Fortunately, neurological deficit, including sphincter disturbances, is infrequent. Dynamic deficits in the setting of claudication are more frequent.
Degenerative deformities are cosmetically well tolerated in the elderly population, though it can be a presenting complaint. With growing attention to the quality of life issues among aging population, cosmesis may have a significant role in presentation, especially in patients below 40 years of age.
It is worthwhile to consider the differential diagnoses of the complex pain patterns, as they can mislead the physician to an inadequate or inappropriate treatment [5, 6]. Cervical spondylosis, arterial insufficiency, abdominal aortic aneurysm, cholecystitis, or malignancies are conditions which may need to be ruled out in patients with history of back pain. A clinical examination including a neurological exam of the upper extremities, an assessment of the presence of myelopathy, and appropriate diagnostic tests are needed to rule out the other possible diagnoses.
Evaluation and Diagnostics
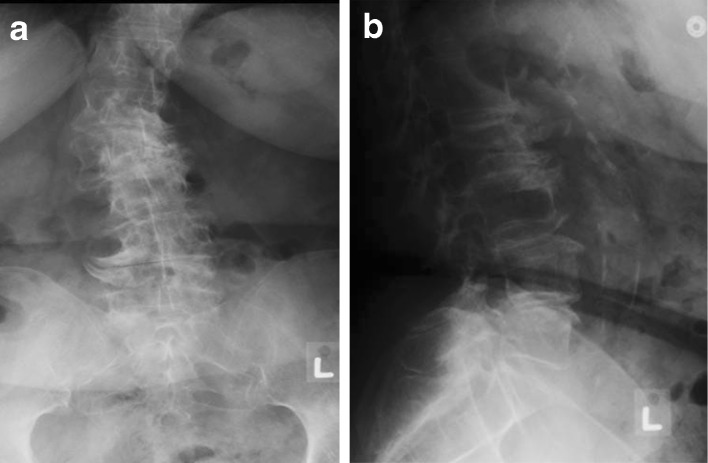
Conventional studies inclusive of standing full-length 36-in. postero-anterior and lateral radiographs are mandatory and may have to be repeated at regular clinical encounters to monitor curve progression (Fig. 1a, b). Cobb angles are measured on these radiographs by using a goniometer in the AP and lateral orientations. Coronal angle of the curve is measured by the Cobb method. This is done by marking perpendicular lines to the end plates of the most angulated vertebrae involved in the curve. Sagittal alignment is assessed by dropping a plumb line through the middle of the C7 vertebral body and the L5/S1 disc space in the lateral projections. In a balanced spine, this line passes through the posterior one third of the superior end plate of S1 vertebral body, although a line up to 4 cm anterior may be considered normal [25]. Dynamic radiographs such as flexion–extension lateral projections may be needed or assessment of instability and spondylolisthesis. Radiographic evaluation assessing the flexibility of the curve is performed when surgery is contemplated. Bending films help assess the extent of curve flexibility and the compensatory ability of the adjacent spinal segments. This major determining factor regarding surgical decision of stand-alone posterior or anterior or a combined approach and curve magnitude varies with the elimination of gravity [5].
Fig. 1.
a, b Antero-posterior and lateral radiographs of degenerative lumbar scoliosis
Further information, regarding bone anatomy, central, recessal, and foraminal stenosis, may be obtained by a CT scan with or/without myelographic evaluation. This is frequently used as a planned preoperative modality [5]. Magnetic resonant imaging scans of the spine can provide additional information about the neural elements, vasculature, soft tissues, and hydration of the discs in detail. MR imaging of degenerative scoliosis is often polymorphic due to the complex three-dimensional pathology and difficult to interpret [6]. Discography may be a useful assessment tool for identifying painful segments, particularly in the lumbar spine (L1–S1), and may help decide which levels to be incorporated in fusion surgery, although controversies exist regarding this modality [4].
Treatment
The selection of appropriate treatment for degenerative scoliosis is challenging because the condition is heterogeneous with diverse presentation of symptoms, and the results are variable. Several factors, such as medical comorbidities, social, and environmental, play significant roles in the outcome and the need for thorough evaluation. Tobacco use, history of asthma or chronic obstructive pulmonary disease, coronary or cerebrovascular disease, diabetes, nutritional deficiency, osteoporosis, depression, and current significant life stressors are shown to correlate with poor clinical outcomes or increased surgical risks. Additionally, a majority of patients have had undergone prior evaluations and several non-operative treatments before referral to a spinal surgeon, with a resultant variable of understanding and expectations of his or her disease. Hence, careful, detailed multidisciplinary counseling is critically important in deciding upon an appropriate treatment plan.
Non-operative Treatment
Many patients are diagnosed when the deformity is noticed on a radiograph performed for other ailments, or in a routine examination. Asymptomatic patients need no treatment, though a periodic follow-up is recommended to monitor curve progression [7]. With the advent of symptoms, it is mandatory to counsel the patient regarding the several modalities of non-operative treatment with a careful review of their outcomes. Some may have experienced treatment modalities before the first visit to a surgeon, and the response to each modality should be noted.
Nonsurgical interventions, often selected empirically, such as pharmacologic agents, physical therapy and exercises, aquatic therapy, chiropractic manipulation, and yoga, are treatment options prescribed by primary care physicians, but have unproven long-term efficacy in adults with scoliosis as this is not well supported in literature [5, 6, 26].
Pharmacologic agents such as non-steroidal anti-inflammatory medication, narcotic analgesics, and muscle relaxants may decrease pain, but have sedative effect and their use is controversial. They are not without adverse effects like gastrointestinal dysfunction and acid-peptic disease. Caution should be used with the administration of chronic narcotic analgesics as this may hasten the development of an irreversible chronic pain syndrome. Tricyclic antidepressants can help with night pain. Gabapentin may help in decreasing neurogenic pain, and it is generally well tolerated in the geriatric population [7].
The use of a lumbo-sacral orthosis or thoraco-lumbo-sacral orthosis may provide temporary pain relief, but long-term use results in muscle deconditioning and has no effect on curve progression [6]. Transcutaneous electrical nerve stimulation units have been prescribed for pain relief in patients with chronic back pain and radicular symptoms [7].
Epidural and facet injections, selective nerve root blocks, and trigger point injections may benefit therapeutically as well as diagnostic if dilemma exist regarding the origin of pain. Invasive modalities, like selective nerve root and facet joint blocks and epidural and trigger point injections, may be both diagnostic and of short-term therapeutic benefit [5, 6].
The objective of non-operative treatment is relief from pain, and a trial should be opted for before embarking upon surgical treatment. The maintenance of a baseline level of physical conditioning in adult deformity patients is important.
Surgical Treatment
The results of surgical treatment of degenerative scoliosis are inconsistent as they are influenced by a number of variables. Patients with degenerative scoliosis with radiculopathy or intractable back pain despite concentrated non-operative therapy and with neurological deficits may be surgical candidates. These patients should be thoroughly evaluated and counseled before surgical treatment.
The surgical plan must not only account for the patients’ symptoms and clinical signs but also for various other factors. The surgical decision is influenced by age, medical comorbidities, and previous surgical history besides social, environmental, and psychological factors and life expectancy. An additional review of the patient’s psychosocial and support mechanism should be evaluated before proceeding with surgical intervention. Since recovery from extensive surgery is prolonged and may involve staying in a nursing facility or a rehabilitation unit with frequent visits to physical therapy centers and office visits to the surgeon, a frank discussion of family or social support required during the recovery period is needed. A preoperative evaluation of bone density and comprehensive nutritional assessment should be performed before contemplating an operation. A multidisciplinary approach in the prevention or treatment of osteoporosis may be required. Balanced diet, cardio-pulmonary exercise, and mineral and vitamin supplements should be encouraged in the early planning period. Pharmacological agents may need to be prescribed for the treatment of osteoporosis.
The indication and the type of procedure may differ among younger healthy and active adults in comparison to debilitated elderly patients with numerous medical problems. No consensus exists regarding indications and surgical plan; hence, a clear understanding of the symptoms and clinical signs is mandatory before an appropriate surgical decision is made. Common indications for surgery are debilitating pain unresponsive to non-operative methods, severely affecting the quality of life, neurological deficit, and rarely cosmetic appearance [6].
The aim of surgical treatment is the decompression of neural elements with restoration and the stabilization of sagittal and coronal balance. Positive sagittal balance of more than 4 cm or flat back syndrome is an important factor in the final outcome [5, 25]. Surgical options include decompression alone and decompression with fusion [5–9, 28–35].
Decompression
Neurogenic claudication in the setting of central and lateral recessal stenosis without significant axial back pain, segmental instability, or progressively worsening deformity would be treated with stand-alone decompression surgery. The procedures inclusive of this operation are laminotomy, laminectomy, foraminal, and extra-foraminal decompression, all being procedures with relatively less morbidity, which may provide short-term symptomatic relief, though they have no effect on curve progression, instability, or axial pain [6, 7]. These may worsen over time, especially after decompression, and may require a second operation hence stand-alone decompression is not frequently indicated. It may still be an attractive option for elderly patients with several associated medical problems [6]. It is relatively not opted for at the apex of the curve, or ends of a rigid curve, as rapid decompensation and destabilization are likely. Patients undergoing stand-alone decompression should be carefully monitored postoperatively with routine evaluations for signs of instability, rapid progression, and worsening of axial pain [9, 10].
Decompression and Instrumented Fusion
The natural history of degenerative scoliosis involves curve progression, instability, and decompensation as the degeneration of the structural spinal elements progresses relentlessly. In an effort to halt the detrimental and disabling sequelae, fusion of the concerned spinal segments coupled with/without decompression is a reasonable surgical option. In more recent published literature, a combination of decompression and fusion using fixation devices yields good results in terms of pain relief, walking ability, and patient satisfaction [6, 9, 10, 29–35].
If back pain is a leading symptom, with or without leg pain, a fusion is usually indicated. Fusion may be obtained without the use of instrumentation (in situ fusion, using bone graft from the decompression and without fixation devices) [20]. This procedure has not been studied in literature, yet it may be a reasonable compromise in elderly patients with minimal symptoms. Fixation devices including pedicular screw and rod systems offer segmental fixation points and tri-planar correction and stabilization of the deformity. Since these curves are rigid in comparison to their adolescent counterparts, an adequate posterior release including facet joint capsules and ligaments is mandatory. More rigid deformities may require additional anterior release including anterior longitudinal ligament and disc–osteophyte complex, with a sequential or staged procedure. Anterior surgery involves interbody fusion with the use of a spacer which may be auto or allograft, or synthetic cages made of titanium or polyetheretherketone with bone graft factors. The restoration of disc height may result in indirect foraminal decompression and restoration of lumbar lordosis.
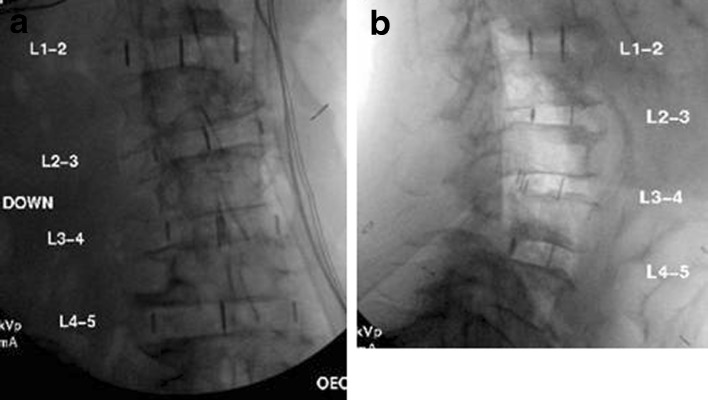
Traditional anterior retroperitoneal approach to the lumbar spine is advantageous as a direct access to the vertebral bodies and better fusion rates, though it carries significant risks of great vessel and visceral organ injury, retrograde ejaculation, and paralytic ileus. Recent advances include lateral lumbar interbody fusion which is a transpsoatic approach through the flank performed with minimally invasive technique (Fig. 2a, b). It carries lesser risks of the traditional procedural complications, but has its own inherent problems such as injury to lumbar plexus and anterior thigh pain [11]. These procedures are coupled with posterior segmental fixation for a secure 360° circumferential arthrodesis (Fig. 3). Newer concepts of “limited” or “selective fusion” involving sequential correction of curve with lateral access, allowing more successful application of short construct fusions, are being evaluated [11].
Fig. 2.
a, b Intraoperative AP and lateral radiographs of lumbar spine after lateral lumbar interbody fusion
Fig. 3.
Antero-posterior radiograph after combined anterior interbody and posterior fusion
Obstacles encountered during fusion operations besides problems associated with advanced age and medical comorbidities are junctional breakdown above or below rigid fusion and pseudoarthrosis. The levels to be included in the fusion can be difficult to determine, most surgeons not opting to stop the fusion at thoraco-lumbar junction as it may lead to decompensation about the construct with progressive kyphosis, warranting additional surgery [6]. Incidence of psuedoarthrosis in degenerative scoliosis surgery is significantly greater than the pediatric population and is up to 24% and highest at the lumbo-sacral junction. Significant risk factors for the development of pseudoarthrosis include a thoraco-lumbar kyphosis, hip osteoarthritis, use of a thoraco-abdominal (versus paramecia) approach, positive sagittal balance greater than 5 cm, age greater than 55 years, and incomplete sacro-pelvic fixation. Osteoporosis is a compounding factor especially in women after menopause [5, 6, 38]. Rapid deterioration of curve with asymmetric collapse of the vertebral bodies may warrant early intervention and may cause technical problems during operation in relation to securing fixation points with instrumentation to the structurally weak bone. Polymethylmethacrylate may be used to augment screw purchase in bone, expandable or large diameter screws may be used [6, 21, 27].
Complication rates are high in most series, ranging from 20% to 40% [7]. Reported complications include pseudoarthrosis, infection, parasthesias, radiculopathy, cerebrospinal fluid fistulas, pulmonary emboli, myocardial infarction, hardware failure, urinary tract infection, compression fractures, adult respiratory distress syndrome, and a high rate of revision surgery [5, 6, 21, 28].
Newer techniques have been introduced in an effort to reduce the perioperative morbidity by adopting minimally invasive methods. Dynamic stabilization with the use of interspinous devices is one of such technique. These devices act as spacers distracting the spinous processes. They are metallic, round to oval shaped, and have straps anchoring them around the spinous processes. They can be implanted with a posterior approach sacrificing the supraspinous ligament or lateral approach preserving it. This procedure has attracted attention partly because most patients with advanced disc disease, being elderly, are prone to morbidity of complicated spinal surgery, and it can be performed with a small incision, possibly with local infiltration anesthesia as a day surgery. Presently, the only FDA-approved interspinous device is the X STOP® (Medtronic; Memphis, TN). The results of a multicenter, prospective, randomized FDA-regulated trial evaluating this device for the treatment of neurogenic intermittent claudication with patients treated non-operatively show that it produced favorable results compared with non-operative care at the end of a 2-year follow-up [40]. Other devices such as DIAM spinal stabilization system (Medtronic, Ltd.) are being evaluated [4].
Conclusion
Characteristically different than other spinal deformities, degenerative scoliosis follows a protracted and benign course, though it can be severely debilitating for the elderly patient. Its natural history follows a vicious cycle of degeneration of structural spinal elements leading to instability and compromise of neural tissue. Although its pathomechanism is uniform in most patients, its treatment needs to be tailored individually accounting for a number of variables including age, symptoms, activity level, disability, medical issues, and social and psychological factors. The goal of the treatment is reduction of pain and discomfort and improvement in the quality of life in terms of functional activity with minimization of complications. A variety of non-operative options are at the physician’s disposal from watchful surveillance to interventions such as injections and blocks.
The goal of surgery includes decompression of neural elements, with restoration and stabilization of spinal balance with arthrodesis. An array of procedures such as decompression and anterior, posterior, or combined fusion with instrumentation may be used. Cobb angle measurement is not representative of the disease as it is in idiopathic curves. The presence of lateral listhesis, spondylolisthesis, and sagittal or coronal decompensation, despite a low Cobb angle, is believed to be more important in decision-making. A detailed counseling of the risk and the benefit of each procedure and its implications on the patient’s psychosocial structure and support system is of primary importance.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Adam S, Kanter MD, Ashok R, Asthagiri MD, Christopher I, Shaffrey MD. Aging Spine: Challenges and Emerging Techniques. Clinical Neurosurgery. 2007;54:10–18. [PubMed] [Google Scholar]
- 2.Aebi M. Adult scoliosis. Therapeutische Umschau. 1987;44:757–763. [PubMed] [Google Scholar]
- 3.Aebi M. The adult scoliosis. Eur Spine J. 2005;14(10):925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 4.Anasetti F, Galbusera F, Aziz HN, Bellini CM, Addis A, Villa T, et al. Spine stability after implantation of an interspinous device: an in vitro and finite element biomechanical study. J Neurosurg Spine. 2010;13(5):568–575. doi: 10.3171/2010.6.SPINE09885. [DOI] [PubMed] [Google Scholar]
- 5.Ascani E, Bartolozzi P, Logroscino CA, Marchetti PG, Ponte A, Savini R, Travaglini F, Binazzi R, Di Silvestre M. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine. 1986;11(8):784–789. doi: 10.1097/00007632-198610000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Avraam Ploumis MD, Ensor E, Transfledt MD, Francis Denis MD. Degenerative lumbar scoliosis associated with spinal stenosis. The Spine Journal. 2007;7(4):428–436. doi: 10.1016/j.spinee.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 7.Benner B, Ehni G. Degenerative lumbar scoliosis. Spine. 1979;4:548. doi: 10.1097/00007632-197911000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Berven SH, Deviren V, Mitchell B, Wahba G, Hu SS, Bradford DS. Operative management of degenerative scoliosis: an evidence-based approach to surgical strategies based on clinical and radiographic outcomes. Neurosurg Clin N Am. 2007;18(2):261–272. doi: 10.1016/j.nec.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Berven SH, Lowe T. The Scoliosis Research Society classification for adult spinal deformity. Neurosurg Clin N Am. 2007;18(2):207–213. doi: 10.1016/j.nec.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Birknes JK, White AP, Albert TJ, Shaffrey CI, Harrop JS. Adult degenerative scoliosis: a review. Neurosurgery. 2008;63(3 Suppl):94–103. doi: 10.1227/01.NEU.0000325485.49323.B2. [DOI] [PubMed] [Google Scholar]
- 11.Boachie-Adjei O, Gupta MC. Adult scoliosis + deformity. AAOS Instructional Course Lectures. 1999;48(39):377–391. [Google Scholar]
- 12.Carter OD, Haynes SG. Prevalence rates for scoliosis in US adults: Results from the first National Health and Nutrition Examination Survey. Int J Epidemiol. 1987;16:537–544. doi: 10.1093/ije/16.4.537. [DOI] [PubMed] [Google Scholar]
- 13.Daffner SD, Vaccaro AR. Adult degenerative lumbar scoliosis. Am J Orthop (Belle Mead NJ) 2003;32(2):77–82. [PubMed] [Google Scholar]
- 14.Epstein JA, Epstein BS, Jones MD. Symptomatic lumbar scoliosis and degenerative changes in the elderly. Spine. 1979;4:542–547. doi: 10.1097/00007632-197911000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Frank Schwab MD, Jean-Pierre Farcy MD, Keith Bridwell MD, Sigurd Berven MD, Steven Glassman MD, John Harrast MS, William Horton MD. A Clinical Impact Classification of Scoliosis in the Adult. Spine. 2006;31(18):2109–2114. doi: 10.1097/01.brs.0000231725.38943.ab. [DOI] [PubMed] [Google Scholar]
- 16.Gelalis ID, Kang JD. Thoracic and lumbar fusions for degenerative disorders: Rationale for selecting the appropriate fusion techniques. Orthop Clin North Am. 1998;29:829–842. doi: 10.1016/S0030-5898(05)70051-1. [DOI] [PubMed] [Google Scholar]
- 17.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30(18):2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 18.Gupta MC. Degenerative scoliosis. Options for surgical management. Orthop Clin North Am. 2003;34(2):269–279. doi: 10.1016/S0030-5898(03)00029-4. [DOI] [PubMed] [Google Scholar]
- 19.Hanley EN., Jr Indications for fusion in the lumbar spine. Bull Hosp Jt Dis. 1996;55:154–157. [PubMed] [Google Scholar]
- 20.Hanley EN., Jr The indications for lumbar spinal fusion with and without instrumentation. Spine. 1995;20(24 suppl):S143–S153. [PubMed] [Google Scholar]
- 21.Kobayashi T, Atsuta Y, Takemitsu M, et al. A prospective study of de novo scoliosis in a community based cohort. Spine. 2006;31:178–182. doi: 10.1097/01.brs.0000194777.87055.1b. [DOI] [PubMed] [Google Scholar]
- 22.Lowe T, Berven SH, Schwab FJ, Bridwell KH. The SRS classification for adult spinal deformity: building on the King/Moe and Lenke classification systems. Spine (Phila Pa 1976) 2006;31(19 Suppl):S119–S125. doi: 10.1097/01.brs.0000232709.48446.be. [DOI] [PubMed] [Google Scholar]
- 23.Marchesi DG, Aebi M. Pedicle fixation devices in the treatment of adult lumbar scoliosis. Spine. 1992;17(8 suppl):S304–S309. doi: 10.1097/00007632-199208001-00016. [DOI] [PubMed] [Google Scholar]
- 24.Nasca RJ. Surgical management of lumbar spinal stenosis. Spine. 1987;12:809–816. doi: 10.1097/00007632-198710000-00019. [DOI] [PubMed] [Google Scholar]
- 25.Oskouian RJ, Jr, Shaffrey CI. Degenerative lumbar scoliosis. Neurosurg Clin N Am. 2006;17(3):299–315. doi: 10.1016/j.nec.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 26.Perennou D, Marcelli C, Herisson C. Adult lumbar scoliosis: Epidemiologic aspects in a low-back pain population. Spine. 1994;19:123–128. doi: 10.1097/00007632-199401001-00001. [DOI] [PubMed] [Google Scholar]
- 27.Postacchini F. Surgical management of lumbar spinal stenosis. Spine. 1999;24:1043–1047. doi: 10.1097/00007632-199905150-00020. [DOI] [PubMed] [Google Scholar]
- 28.Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine. 2005;30:1082–1085. doi: 10.1097/01.brs.0000160842.43482.cd. [DOI] [PubMed] [Google Scholar]
- 29.Schwab F, el-Fegoun AB, Gamez L, Goodman H, Farcy JP. A lumbar classification of scoliosis in the adult patient: preliminary approach. Spine. 2005;30(14):1670–1673. doi: 10.1097/01.brs.0000170293.81234.f0. [DOI] [PubMed] [Google Scholar]
- 30.Scoliosis Research Society. Available at www.SRS.org/professionals/glossary/glossary.asp.
- 31.Sharma AK, Kepler CK, Girardi FP, Cammisa FP, Huang RC, Sama AA. Lateral Lumbar Interbody Fusion: Clinical and Radiographic Outcomes at 1 Year: A Preliminary Report. J Spinal Disord Tech 2010; Pub ahead of print. [DOI] [PubMed]
- 32.Simmons ED., Jr Simmons EH: Spinal stenosis with scoliosis. Spine. 1992;17(6 suppl):S117–S120. doi: 10.1097/00007632-199206001-00009. [DOI] [PubMed] [Google Scholar]
- 33.Transfeldt EE, Topp R, Mehbod AA, Winter RB. Surgical outcomes of decompression, decompression with limited fusion, and decompression with full curve fusion for degenerative scoliosis with radiculopathy. Spine (Phila Pa 1976) 2010;35(20):1872–1875. doi: 10.1097/BRS.0b013e3181ce63a2. [DOI] [PubMed] [Google Scholar]
- 34.Tribus CB. Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg. 2003;11(3):174–183. doi: 10.5435/00124635-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Vaccaro AR, Ball ST. Indications for instrumentation in degenerative lumbar spinal disorders. Orthopedics. 2000;23:260–271. doi: 10.3928/0147-7447-20000301-21. [DOI] [PubMed] [Google Scholar]
- 36.van Dam BE. Nonoperative treatment of adult scoliosis. Orthop Clin North Am. 1988;19:347–351. [PubMed] [Google Scholar]
- 37.Vanderpool DW, James JI, Wynne-Davies R. Scoliosis in the elderly. J Bone Joint Surg Am. 1969;51:446–455. doi: 10.2106/00004623-196951030-00002. [DOI] [PubMed] [Google Scholar]
- 38.Velis KP, Healey JH, Schneider R. Osteoporosis in unstable adultscoliosis. Clin Orthop Relat Res. 1988;237:132–141. [PubMed] [Google Scholar]
- 39.Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:447–455. doi: 10.2106/00004623-198365040-00004. [DOI] [PubMed] [Google Scholar]
- 40.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, et al. A multicenter, prospective, randomized trial evaluating the X STOP interspinous process decompression system for the treatment of neurogenic intermittent claudication: two-year follow-up results. Spine (Phila Pa 1976) 2005;30(12):1351–1358. doi: 10.1097/01.brs.0000166618.42749.d1. [DOI] [PubMed] [Google Scholar]