Abstract
Background
Cervical radiculopathy is defined as a syndrome of pain and/or sensorimotor deficits due to compression of a cervical nerve root. Understanding of this disease is vital for rapid diagnosis and treatment of patients with this condition, facilitating their recovery and return to regular activity.
Purpose
This review is designed to clarify (1) the pathophysiology that leads to nerve root compression; (2) the diagnosis of the disease guided by history, physical exam, imaging, and electrophysiology; and (3) operative and non-operative options for treatment and how these should be applied.
Methods
The PubMed database was searched for relevant articles and these articles were reviewed by independent authors. The conclusions are presented in this manuscript.
Results
Facet joint spondylosis and herniation of the intervertebral disc are the most common causes of nerve root compression. The clinical consequence of radiculopathy is arm pain or paresthesias in the dermatomal distribution of the affected nerve and may or may not be associated with neck pain and motor weakness. Patient history and clinical examination are important for diagnosis. Further imaging modalities, such as x-ray, computed tomography, magnetic resonance imaging, and electrophysiologic testing, are of importance. Most patients will significantly improve from non-surgical active and passive therapies. Indicated for surgery are patients with clinically significant motor deficits, debilitating pain that is resistant to conservative modalities and/or time, or instability in the setting of disabling radiculopathy. Surgical treatment options include anterior cervical decompression with fusion and posterior cervical laminoforaminotomy.
Conclusion
Understanding the pathophysiology, diagnosis, treatment indications, and treatment techniques is essential for rapid diagnosis and care of patients with cervical radiculopathy.
Keywords: cervical radiculopathy, disc herniation, ACDF, ADF, posterior cervical laminoforaminotomy, posterior cervical foraminotomy
Introduction
Cervical radiculopathy is a pain and/or sensorimotor deficit syndrome that is defined as being caused by compression of a cervical nerve root [1–4]. The compression can occur as a result of disc herniation, spondylosis, instability, trauma, or rarely, tumors. Patient presentations can range from complaints of pain, numbness, and/or tingling in the upper extremity to electrical type pains or even weakness. The clinical overlap between cervical radiculopathy and peripheral nerve entrapment syndromes and their nearly ubiquitous nature makes understanding of and identification of these entities mandatory for all practitioners.
The purpose of this review is to facilitate the understanding of this disease by addressing several questions. What is the underlying pathophysiology that leads to the development of the clinical syndrome of cervical radiculopathy? How is the diagnosis of cervical radiculopathy made and how can it be differentiated from common peripheral nerve entrapment syndromes? What are the current non-surgical treatment options for the patient with cervical radiculopathy and how does the underlying pathophysiology guide the treatment choice? What are the current surgical treatment options for the patient with cervical radiculopathy and what are the determining factors for how they should be employed?
Cervical radiculopathy can be a debilitating disease that can cause patients significant impairment. The toll on this population can be significant both economically, from lost work and wages, and psychologically, from prolonged pain and impaired social functioning. The goal for clinicians should be the rapid diagnosis and treatment of this condition in order to facilitate the return of the patient to their normal state of health.
Methods
To accomplish the goal of this review, the PubMed database was searched for publications from January 2000 through January 2011. The search was limited to English language articles. Initially, the database was searched using the term “cervical radiculpathy.” This search returned a total of 1,978 articles; when narrowed to full text, there were a total of 374 articles. This subgroup was then searched for the keywords “surgery,” “pathophysiology,” “diagnosis,” and “treatment”. The resulting articles were screened by title and abstract for relevance to this review. A total of 84 relevant resources were identified. All relevant full-text manuscripts found on the PubMed database using the mentioned keywords were reviewed by independent authors and the results are concisely presented here.
Results
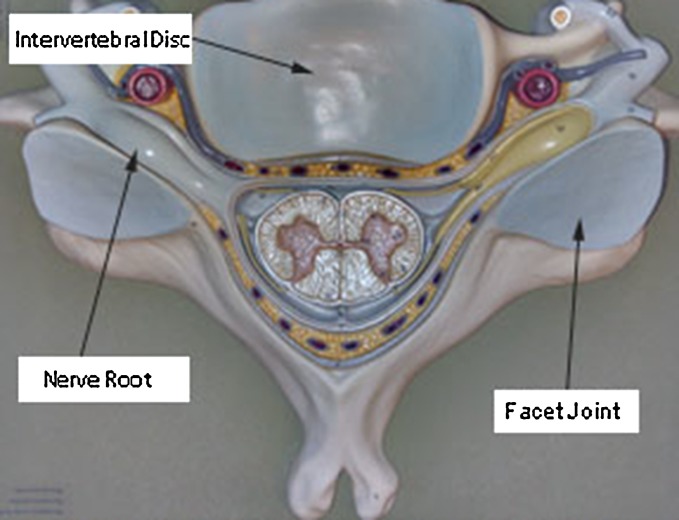
The cervical spinal nerves exit the spinal cord and are oriented obliquely toward their respective neural foramen (Fig. 1). The cervical spinal nerves are named corresponding to the vertebral body below the nerve. The C8 nerve exits between C7 and T1 [5]. The neural foramen is made up of the facet joint posteriorly and the intervertebral disc anteriorly. The superior and inferior borders are comprised of the pedicles of the vertebral bodies above and below, respectively. The foramina are largest in the upper cervical spine and gradually narrow distally, with the C7/T1 foramina being the most narrow. The most common causes of nerve root compression are spondylosis of the facet joint and herniation of the intervertebral disc [6]. Hypermobility of the facet joint leads to ligamentous hypertrophy as well as bony hypertrophy. An increase in the size of the superior articulating process from the distal vertebra causes compression of the nerve. Intervertebral disc herniations can also cause nerve root compression from the anterior aspect of the foramen [7]. Disc herniations can either be acute or chronic. Chronic herniations occur when the intervertebral disc becomes degenerated and desiccated. This causes collapse of the disc space and bulging of the annulus into the neural foramen. Chronic herniations and facet spondylosis generally cause symptoms with an insidious onset that tend to be less severe. An acute herniation occurs when a fragment of the nucleus pulposus extrudes through a defect in the annulus fibrosis. This generally is associated with the sudden onset of severe symptoms, in contrast to those associated with a chronic disc herniation [4, 8]. Researchers hypothesize that pain syndromes and deficits arise as a result of both ischemia and inflammation notions that would explain why acute insults tend to result in more profound symptoms than slow, adaptable processes [9].
Fig. 1.
Axial representation of C5 vertebra looking cephalad to caudal
The patient history alone can diagnose cervical radiculopathy in over 75% of cases [10]. The most common symptom associated with radiculopathy is arm pain or paresthesias in the dermatomal distribution of the affected nerve. Various different nerve compression syndromes are well described (Table 1). Cervical radiculopathy may or may not be associated with neck pain. In rheumatoid arthritis, atlanto-axial settling can lead to C2 radicular pain which can manifest itself as eye and/or ear pain and headache. C3 and C4 symptoms tend to be vague neck pain and trapezious pain. C5 pain occurs in the shoulder and radiates down the ventral arm to below the elbow. C6 radiculopathy is associated with pain down the superior lateral aspect of the arm into the first two digits. Commonly, there is overlap in the pain presentation of C6 radiculopathy and carpal tunnel syndrome. In carpal tunnel syndrome, patients often report worse symptoms in the morning. If present, the motor component of the two clinical entities is quite different. Classically, carpal tunnel syndrome motor deficit is gauged by strength assessment of the abductor pollicis brevis which is innervated by the recurrent branch of the median nerve (which has a take-off point distal to the transverse carpal ligament). Clinically, patients with advanced carpal tunnel syndrome will have thenar atrophy. In contrast, the C6 nerve root provides motor innervations in a shared fashion to elbow flexors and wrist extensors. On clinical examination, Spurling’s maneuver will exacerbate C6 radicular pain, but not median nerve entrapment. Tinel’s at the wrist, Durken’s median nerve test, and wrist flexion will exacerbate carpal tunnel syndrome [11]. C7 pain radiates down the dorsal aspect of the arm, through the elbow and into the third digit. C8 symptoms move down the inferior medial aspect of the arm into the fourth and fifth digits and are often confused with the pain of ulnar neuropathy [12]. Again, maneuvers such as Sperling’s test, Tinel’s at the elbow, and elbow flexion test can distinguish the two clinical entities. Sensory examination can distinguish between a C8 radiculopathy and ulnar neuropathy, as there will be splitting of the hypalgesia in either the third or fourth digit with ulnar neuropathy. With C8 radiculopathy, the entire digit will be affected. Motor examination may or may not show a grade of weakness in the myotome that corresponds to the pathologic nerve. No myotome corresponds to the upper four cervical nerve roots. C5 radiculopathy may show weakness in the deltoids; C6 will show weakness in the biceps and flexor carpi ulnaris (evaluated by testing for wrist extension); C7 weakness occurs in the triceps, as well as the brachioradialis; C8 pathology causes weakness in the intrinsic muscles of the hand, as evaluated by finger abduction and grip. Muscle stretch reflexes also tend to be decreased in the setting of radiculopathy. Biceps hyporeflexia is indicative of C6 radiculopathy, while decrease in the triceps and brachioradialis reflexes corresponds to pathology at C7. The neurologic examination has moderately strong intraobserver reliability with a kappa value between 0.4 and 0.64 according to Viikari-Juntura [13]. The neurologic findings on exam were highly correlated to the pathology found during surgery according to Yoss et al. [14].
Table 1.
Patterns of nerve root compression syndromes
| Nerve root | Pain pattern | Weakness | Reflexes |
|---|---|---|---|
| C2 | Occipital, eyes | ||
| C3 | Neck, trapezius | ||
| C4 | Neck, trapezius | ||
| C5 | Shoulder, lateral UE | Deltoid | |
| C6 | Lateral forearm, first two digits | Biceps | Biceps absent |
| C7 | Posterior forearm, third digit | Triceps | Triceps absent |
| C8 | Medical forearm, fourth and fifth digit | Finger abduction, grip |
Cervical range of motion is often tested in patients who complain of neck pain and radicular symptoms [15]. Patients often have impairment in their range of motion and limitation in their function. This is most commonly seen in extension, since the foramina tend to narrow significantly when the spine is extended. This has been shown by both anatomic in vitro studies as well as CT studies of the spine in vivo [4].
As mentioned, provocative testing can also clarify a diagnosis during the physical examination. Five such tests have been identified in the literature: Spurling’s test, the valsalva maneuver, the shoulder abductor sign, the upper limb tension test, and neck distraction. Spurling’s test is designed to reproduce symptoms and is performed by laterally flexing, rotating, and compressing the patient’s head toward the side of the symptoms. This effectively causes the pathologic foramen to close and should reproduce the symptoms. This test is very reproducible and extremely specific, but is not sensitive. The valsalva maneuver is another test that should reproduce the patient’s symptoms. However, its mechanism of action and reproducibility has not been clearly defined. The upper limb tension test is designed to stretch the affected nerve root and thereby reproduce the patient’s symptoms. The reproducibility of this test is relatively poor and its sensitivity and specificity has not been studied. The shoulder abductor sign and neck distraction are designed to open the affected foramen, decompress the nerve, and relieve the patient’s symptoms. The shoulder abductor sign test is carried out by having the patient rest the hand of the affected extremity on the head. Neck traction is generally done with the patient in the supine position and the practitioner applies gentle tractions to the cervical spine (up to 30 lbs). Both of these tests have moderate intraobserver reliability, poor sensitivity, and high specificity [10, 13]. As mentioned, patients may suffer from peripheral median or ulnar nerve entrapment syndromes that masquerade as cervical radiculopathy (or vice versa). Having a clear understanding of how to diagnose each entity is essential in making the final correct diagnosis. Complicating matters further is that commonly, a “double crush” phenomena exists in which patients have neural compression both at the level of the cervical spine and at the level of the peripheral nerve. Maneuvers such as the Spurling’s test for radiculopathy as well as Tinel’s at the elbow and wrist, median nerve compression test, and wrist and elbow flexion tests can help distinguish C6 and C8 radiculopathies from median and ulner nerve entrapment, respectively. Ultimately, electromyogram/nerve conduction studies (EMG/NCS) is a helpful adjunct.
Imaging modalities and electrophysiologic testing play an important role in the diagnosis and localization of cervical radiculopathy. The first test that is typically done is plain x-ray. AP and lateral views are useful for demonstrating the overall alignment of the spine as well as the presence of any obvious spondolytic changes. Lateral flexion and extension views are helpful to diagnose any instability that may be present and not seen on a static radiograph. Computed tomography is the most sensitive test for examination of the bony structures of the spine. This can be used to identify any insidious process that may cause bony destruction or abnormal bone formation, such as ossification of the posterior longitudinal ligament. The bony opening of the foramina can also be examined for any osteophyte formation that may cause nerve root impingement. CT, when combined with, myelography, has the ability to delineate the nerve root in relation to bony structures. By inference, when contrast cannot be seen entering the nerve root sleeve, there is compression of that nerve. The limitations of myelography are that it has a poor ability to show soft tissue structures and it is an invasive test that is not without risk or side effects. Therefore, the preferred imaging modality is MRI. This has the greatest ability to show the soft tissue structures as well as course of the nerve as it exits the foramen. Several studies have correlated MR findings to outcome postoperatively, particularly with T2 hyperintesity/T1 hypointesity of the spinal cord being associated with less relief of symptoms following surgical decompression [13, 16–19]. EMG is another tool that the practitioner can use to aid in diagnosis of radiculopathy. By itself, EMG has a relatively poor predictive capacity in showing nerve root compression. In a study by Ashkan et al., only 42% of patients with a positive EMG finding had compression at the time of surgery, while 93% of those with positive MRI findings had pathology. EMG is most valuable as a supplement to imaging modalities in helping to localize the appropriate level in patients with vague symptoms or inconclusive imaging [19]. Additionally, as discussed, it is a useful adjunct when considering peripheral neuropathy in the differential diagnosis.
The majority of patients diagnosed with cervical radiculopathy (75–90%) will improve with non-operative management according to two large prospective studies that evaluated treatment modalities [20, 21]. The remaining minority of patients fail to achieve acceptable recovery with conservative modalities alone. Additionally, urgent surgery is indicated in a subset of patients. Patients who have an acute profound neurologic deficit with obvious pathology generally require surgery in an urgent manner. Traumatic injury or instability, generally, requires swift attention. No exact criteria have been defined that obviate the patient to this course of action, nor have any large studies been performed that show the long-term outcome of emergent decompression for non-traumatic injury. There is evidence supporting early decompression for traumatic spinal cord injury and central cord syndrome and a general correlation with more positive outcomes with early decompression in the setting of motor radiculopathy [22–24]. Non-operative treatments can include both active and passive therapy [25]. Passive therapy consists of collar immobilization and rest from activities that aggravate the condition. Three studies that compared immobilization to active therapy showed no difference in long-term outcome, but those treated more aggressively tended to improve more quickly. There is widespread indication that prolonged use of the collar leads to deconditioning of the neck musculature and tissue damage and should be avoided. Active interventions are more favored in the literature [26–28]. The majority of studies that describe non-operative therapy document the usage of multiple modalities of treatment. One such study compared range of motion exercises, ergonomic neck instruction, neck relaxation, and superficial heat to manual cervical traction [27]. The group receiving traction had significantly better pain scores and range of motion following a 6-week treatment period. Other studies include the usage of TENS, cervical pillow, massage, acupuncture, and ultrasound. Cervical traction is one physical therapy modality that has been studied separately from the others. Five studies have looked at traction as a treatment for radiculopathy [29–33]. All five showed that traction was temporarily efficacious in relieving patients’ symptoms; however, none of the studies included standardized outcome measures. While there is no evidence to suggest the superiority of one treatment modality over another, the literature suggests that a combination of therapies aids in the recovery of patients as compared to passive non-operative therapy. While invasive, epidural steroid injection (ESI) falls in the realm of non-operative therapy. Five studies were identified that studied the efficacy of epidural injection [26, 34–39]. All five showed that ESI improved symptoms; however, none of the studies used validated outcome measures to assess long-term benefit. Data that was measured primarily relied on visual analogue scale (VAS) and non-standardized pain scales. Three of the five studies reported complications, all of which were minor and did not require any further intervention. The rate of complication ranged from 3% to 35% in these studies. There have been case reports of more catastrophic complications, including epidural hematomas that needed to be emergently decompressed and spinal cord infarction, particularly in the setting of severe central stenosis [40]. Due to these complications and the technical difficulty of the injection, physiatrists and pain management professionals are moving away from performing this procedure. Chiropractic manipulation is described in two prospective case series for the treatment of cervical radiculopathy [41, 42]. Neither series is adequately powered to show the superiority of manipulation over other non-operative treatments. Both series report on the use of high-velocity, low-amplitude manipulation. In the larger series, 27 patients were studied with 80% reporting improvement of VAS at 9 months. While this series reported no complications, a smaller series showed worsening of radiculopathy in two of eight patients undergoing manipulation. Any patient undergoing chiropractic manipulation must have a proper workup prior to treatment. Any instability or mass lesions are absolute contraindications to manipulation and can have disastrous consequences. Vertebral artery injury is another commonly reported complication that can lead to catastrophic outcomes [43]. Given the risks involved with manipulation and the paucity of evidence showing any benefit, this therapy cannot be recommended as a predictable treatment option. Chiropractor treatments should focus on the use of gentle range of motion exercises and directed massage.
When patients fail non-operative management or otherwise meet inclusion criteria for surgery, there are multiple options available for the operative intervention of cervical radiculopathy. General practice deems that patients with clinically significant motor deficits, debilitating pain that is resistant to conservative modalities and/or time, or instability in the setting of disabling radiculopathy are indicated for surgery. Spinal alignment, stability, balance, and surgeon’s preferred technique, all play a role in the decision of which operation to perform [44]. Surgical interventions can be broken down into two large categories: anterior and posterior approaches to the spine.
Anterior surgery affords the surgeon the ability to restore cervical lordosis, stabilize the spine, and predictably decompress the nerve roots. This is accomplished by opening a plane between the carotid artery and the esophagus and following this to the anterior aspect of the spine [45, 46]. The intervertebral disc is then removed in its entirety along with any osteophytes at the posterior aspect of the vertebral body. Historically, the evacuated disc was then replaced by either bone graft material or nothing. [47–52] More recently, surgeons have favored restoring the normal height of the disc segment with structural grafts or cages. Some describe opening the foramen from the anterior approach, while performing only enough discectomy to reach the pathologic foramen [53–55]. Matz et al. [50] reviewed multiple studies describing various techniques for anterior decompression of the nerve. These included anterior cervical decompression and fusion, cervical discectomy alone without fusion, and anterior cervical foramenotomy without complete discectomy. The conclusion of the studies showed that there was very good evidence that patients got immediate and long-term relief of symptoms from anterior cervical discectomy with fusion (ACDF) and anterior cervical discectomy alone (ACD). Multiple prospective studies showed that these procedures provide symptomatic relief significantly faster than physical therapy [52, 56, 57]. This relief is maintained throughout a 12-month follow-up period. The evidence was not as strong in support of performing anterior foramenotomy alone. Most studies of this procedure showed variable outcome, between 54% and 95% symptom relief, and none of the studies used standardized validated outcome measures. Currently, most surgeons choose to perform ACDF rather than ACD for several reasons [58]. Insertion of a graft increases the rate of fusion [59] and increases the degree of postoperative lordosis [22]. Furthermore, insertion of a graft allows for indirect decompression of the neural foramen by increasing the cephalocaudal height of the space [60]. ACDF allows for a predictable outcome, with relief of symptoms in up to 90% of patients with radiculopathy [61].
Surgeons have several choices of material for cages that contain the graft as well as several choices of graft material. Cages can be titanium, polyetheretherketone, carbon fiber polymer, or structural allograft. All of these materials have been shown to be effective [23, 48]; however, no clear advantage has been seen for one specific material. The same can be said for graft material [8], no specific advantage has been found to iliac crest autograft versus allograft bone [62]. The inclusion of an anterior plate for single-level or two-level fusions is another controversial topic. Several studies have shown that the inclusion of a plate increases fusion rate, decreases postoperative kyphosis, and decreases graft subsidence, as well as prevents catastrophic cage/graft migration [63, 64]. For more than two levels, use of an anterior plate is mandatory for graft safety as well as to achieve predictable fusion rates [65]. Historically, anterior cervical corpectomy was advocated for two-level disease by a large number of surgeons. However, data has suggested a worse outcome for patients undergoing corpectomy compared to those undergoing two-level ACDF [66]. Corpectomy patients tended to have a greater rate of kyphosis, hardware failure, and pseudoarthrosis. More recently, even three- and four-level ACDF has been shown to have predictable, successful outcome with the evolution of more advanced anterior plating systems.
Total disc arthroplasty is a newer technique for anterior surgery in the setting of radiculopathy that maintains segment height while maintaining motion. These devices have been shown to have similar efficacy to ACDF, with patient outcomes similar to that of ACDF [67]. Developers hypothesize that this would decrease the rate of adjacent segment degeneration. However, a study by Jawahar et al. in 2010 has shown this not to be the case [63]. This is an area of ongoing research and interest.
Anterior surgery is not without its drawbacks. Surgeons who are not comfortable performing the Smith–Robinson approach to the anterior spine may require an otolaryngologist for the approach. Recurrent laryngeal nerve injury is reported in 0–25% of cases depending on the series. This rate may be confounded by local neuroproxia or ischemic injury to the vocal cords, rather than to the nerve itself. Dysphagia and odynophagia are known complications of the approach as well, although most of these complications are temporary and resolve within 3 months. Patients with prior surgery, radiation, or infection can present the surgeon with significant difficulty as well [49, 52, 68, 69].
Another option for decompression of cervical nerves is to perform a posterior cervical laminoforaminotomy [70]. This is performed by exposing the junction of the lamina and facet joint at the affected level. A high-speed burr is then used to open a window in the lamina and remove the medial one third of the facet joint, thus exposing the affected nerve. If necessary, the nerve can be carefully and gently retracted to expose and remove a fragment of herniated disc. However, Korinth et al. in 2006 studied 293 patients comparing anterior and posterior procedures for soft disc herniations and found superiority with the anterior technique [71]. The posterior operation has the benefit of maintaining spinal alignment and not requiring a fusion. This, theoretically, prevents the breakdown of the adjacent level; however, the literature is not complete on this subject. The primary complication with this procedure is neck pain, presumably secondary to muscle dissection [72]. Certain risk factors, such as advanced age, cervical kyphosis, and previous surgery may predispose patients to progressive degeneration and spinal deformity [73]. One of the most important limitations to the posterior surgery is the amount of bony decompression that can safely be achieved. Since this procedure does not allow for indirect decompression via distraction, the nerve must be directly decompressed. If there is a large amount of bony foraminal stenosis, this may not be possible without destabilization of the facet and the need for a fusion [74]. Therefore, this technique may be best applied to soft disc fragments causing neural foraminal stenosis. Heary et al. [50] reviewed the literature regarding this procedure as applied to cervical disc herniations and found a significant number of case series that describe the use of this procedure for radiculopathy. The literature describes between 75% and 98% positive outcome. The large number of patients treated, as well as the consistent results, led the authors to recommend laminoforaminotomy in the appropriate clinical setting despite most studies lacking validated measures and blinded studies. A classic paper by Herkowitz et al. [75] compared the efficacy of anterior cervical decompression and fusion with posterior cervical laminoforminotomy in 33 patients. This group was then followed for a mean of 4.2 years. The authors alternated procedures on a comparable patient population and found that 95% of the patients in the ACDF group had positive outcomes, while 75% of the posterior surgery group had positive outcomes. The difference was not statistically significant and therefore showed that both anterior and posterior procedures for cervical radiculopathy have excellent efficacy when indicated correctly.
Discussion
Cervical radiculopathy is a clinical syndrome manifested by compression of a spinal nerve in the neck. This syndrome is typically characterized by upper extremity pain and, occasionally, sensorimotor deficits in the area supplied by the affected nerve. Patients who suffer from this disease are often debilitated, losing time from work and social obligations. It is essential for clinicians to rapidly diagnose and appropriately treat these patients. In the course of this review, the authors sought to ask and answer four vital questions:
What is the underlying pathophysiology that leads to the development of the clinical syndrome of cervical radiculopathy?
How is the diagnosis of cervical radiculopathy made and how can it be differentiated from common peripheral nerve entrapment syndromes?
What are the current non-surgical treatment options for the patient with cervical radiculopathy and how does the underlying pathophysiology guide the treatment choice.
What are the current surgical treatment options for the patient with cervical radiculopathy and what are the determining factors for how they should be employed?
While these four questions have been enumerated and answered with the available literature, there are several questions that remain:
What is the economic impact of this disease and how do the different treatment modalities affect this impact?
How does time of onset of neurologic injury coupled with the time to decompression of the nerve affect the outcome of that injury?
The literature reflects that the C5 nerve is more sensitive to injury than the other nerves in the cervical spine [76]. What is the pathophysiologic mechanism related to this sensitivity and what issues should surgeons be aware of when dealing with this nerve?
Given the prevalence of cervical radiculopathy, studies of patients with this disease should not be difficult to accomplish. A large cohort of patients can be studied prospectively to determine the time it takes to return to work. Likewise, the same cohort can be studied to determine the return of neurologic function following decompression. The study of the C5 nerve may require more intensive scrutiny of imaging, electrophysiologic testing, and intraoperative observations. This also may be an area where cadaveric studies of the relationship of the nerve to its surrounding structures might provide benefit.
The knowledge and understanding of cervical radiculopathy continues to evolve. Nerve root compression, as reviewed in the pathophysiology section, is caused by disc herniation, degeneration, and facet hypertrophy. Diagnosis can be made by history and physical examination, while confirmation with MRI can be supplemented by CT scans and electrophysiologic testing. Treatment typically begins with non-operative management, such as active and passive physical therapy. Pain management techniques, such as ESIs, can provide symptom relief but have risks. If non-operative management fails, or if the patient has an acute functional impairment, surgical decompression of the nerve root may be necessary.
Conclusion
Cervical radiculopathy is a common clinical entity. Understanding the pathophysiology, diagnosis, treatment indications, and treatment techniques will lead to rapid diagnosis and improved patient care. This knowledge is important for all practitioners. Rapid diagnosis and treatment will lead, ultimately, to a greater chance for early recovery for the patient affected by this condition.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005;353(4):392–399. doi: 10.1056/NEJMcp043887. [DOI] [PubMed] [Google Scholar]
- 2.Ellenberg MR, Honet JC, Treanor WJ. Cervical radiculopathy. Arch Phys Med Rehabil. 1994;75(3):342–352. doi: 10.1016/0003-9993(94)90040-X. [DOI] [PubMed] [Google Scholar]
- 3.Fouyas IP, Statham PF, Sandercock PA. Cochrane review on the role of surgery in cervical spondylotic radiculomyelopathy. Spine (Phila Pa 1976) 2002;27(7):736–747. doi: 10.1097/00007632-200204010-00011. [DOI] [PubMed] [Google Scholar]
- 4.Humphreys SC, Chase J, Patwardhan A, Shuster J, Lomasney L, Hodges SD. Flexion and traction effect on C5-C6 foraminal space. Arch Phys Med Rehabil. 1998;79(9):1105–1109. doi: 10.1016/S0003-9993(98)90179-4. [DOI] [PubMed] [Google Scholar]
- 5.Drake RL, Gray H. Gray’s atlas of anatomy. 1. Philadelphia: Churchill Livingstone; 2008. [Google Scholar]
- 6.Benzel EC. Spine surgery : techniques, complication avoidance, and management. 2005.
- 7.Bush K, Chaudhuri R, Hillier S, Penny J. The pathomorphologic changes that accompany the resolution of cervical radiculopathy. A prospective study with repeat magnetic resonance imaging. Spine (Phila Pa 1976) 1997;22(2):183–186. doi: 10.1097/00007632-199701150-00009. [DOI] [PubMed] [Google Scholar]
- 8.Buttermann GR. Prospective nonrandomized comparison of an allograft with bone morphogenic protein versus an iliac-crest autograft in anterior cervical discectomy and fusion. Spine J. 2008;8(3):426–435. doi: 10.1016/j.spinee.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Devereaux M. Neck pain. Med Clin North Am. 2009;93(2):273–284. doi: 10.1016/j.mcna.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Wainner RS, Gill H. Diagnosis and nonoperative management of cervical radiculopathy. J Orthop Sports Phys Ther. 2000;30(12):728–744. doi: 10.2519/jospt.2000.30.12.728. [DOI] [PubMed] [Google Scholar]
- 11.Petiot P, Bernard E. Diagnostic pitfalls in carpal tunnel syndrome. Rev Neurol (Paris). 2011;167(1):64–71. doi: 10.1016/j.neurol.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 12.DeMyer W. Technique of the neurologic examination : a programmed text. 3. New York: McGraw-Hill; 1980. [Google Scholar]
- 13.Viikari-Juntura E, Porras M, Laasonen EM. Validity of clinical tests in the diagnosis of root compression in cervical disc disease. Spine (Phila Pa 1976) 1989;14(3):253–257. doi: 10.1097/00007632-198903000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Yoss RE, Corbin KB, Maccarty CS, Love JG. Significance of symptoms and signs in localization of involved root in cervical disk protrusion. Neurology. 1957;7(10):673–683. doi: 10.1212/WNL.7.10.673. [DOI] [PubMed] [Google Scholar]
- 15.Youdas JW, Carey JR, Garrett TR. Reliability of measurements of cervical spine range of motion--comparison of three methods. Phys Ther. 1991;71(2):98–104. doi: 10.1093/ptj/71.2.98. [DOI] [PubMed] [Google Scholar]
- 16.Alrawi MF, Khalil NM, Mitchell P, Hughes SP. The value of neurophysiological and imaging studies in predicting outcome in the surgical treatment of cervical radiculopathy. Eur Spine J. 2007;16(4):495–500. doi: 10.1007/s00586-006-0189-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jagannathan J, Shaffrey CI, Oskouian RJ, et al. Radiographic and clinical outcomes following single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. J Neurosurg Spine. 2008;8(5):420–428. doi: 10.3171/SPI/2008/8/5/420. [DOI] [PubMed] [Google Scholar]
- 18.Mochida K, Komori H, Okawa A, Muneta T, Haro H, Shinomiya K. Regression of cervical disc herniation observed on magnetic resonance images. Spine (Phila Pa 1976) 1998;23(9):990–995. doi: 10.1097/00007632-199805010-00005. [DOI] [PubMed] [Google Scholar]
- 19.Nardin RA, Patel MR, Gudas TF, Rutkove SB, Raynor EM. Electromyography and magnetic resonance imaging in the evaluation of radiculopathy. Muscle Nerve. 1999;22(2):151–155. doi: 10.1002/(SICI)1097-4598(199902)22:2<151::AID-MUS2>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 20.Radhakrishnan K, Litchy WJ, O’Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117(Pt 2):325–335. doi: 10.1093/brain/117.2.325. [DOI] [PubMed] [Google Scholar]
- 21.Sampath P, Bendebba M, Davis JD, Ducker T. Outcome in patients with cervical radiculopathy. Prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976) 1999;24(6):591–597. doi: 10.1097/00007632-199903150-00021. [DOI] [PubMed] [Google Scholar]
- 22.Aarabi B, Alexander M, Mirvis SE, et al. Predictors of outcome in acute traumatic central cord syndrome due to spinal stenosis. J Neurosurg Spine. Dec 17 2010. [DOI] [PubMed]
- 23.Fehlings MG, Rabin D, Sears W, Cadotte DW, Aarabi B. Current practice in the timing of surgical intervention in spinal cord injury. Spine (Phila Pa 1976) 2010;35(21 Suppl):S166–S173. doi: 10.1097/BRS.0b013e3181f386f6. [DOI] [PubMed] [Google Scholar]
- 24.Lenehan B, Fisher CG, Vaccaro A, Fehlings M, Aarabi B, Dvorak MF. The urgency of surgical decompression in acute central cord injuries with spondylosis and without instability. Spine (Phila Pa 1976) 2010;35(21 Suppl):S180–S186. doi: 10.1097/BRS.0b013e3181f32a44. [DOI] [PubMed] [Google Scholar]
- 25.Arnasson O, Carlsson CA, Pellettieri L. Surgical and conservative treatment of cervical spondylotic radiculopathy and myelopathy. Acta Neurochir (Wien). 1987;84(1–2):48–53. doi: 10.1007/BF01456351. [DOI] [PubMed] [Google Scholar]
- 26.Dreyer SJ, Boden SD. Nonoperative treatment of neck and arm pain. Spine (Phila Pa 1976) 1998;23(24):2746–2754. doi: 10.1097/00007632-199812150-00016. [DOI] [PubMed] [Google Scholar]
- 27.Jette DU, Jette AM. Physical therapy and health outcomes in patients with spinal impairments. Phys Ther. 1996;76(9):930–941. doi: 10.1093/ptj/76.9.930. [DOI] [PubMed] [Google Scholar]
- 28.Tan JC, Nordin M. Role of physical therapy in the treatment of cervical disk disease. Orthop Clin North Am. 1992;23(3):435–449. [PubMed] [Google Scholar]
- 29.Anonymous. Pain in the neck and arm: a multicentre trial of the effects of physiotherapy, arranged by the British Association of Physical Medicine. Br Med J. Jan 29 1966;1(5482):253–258. [DOI] [PMC free article] [PubMed]
- 30.Swezey RL, Swezey AM, Warner K. Efficacy of home cervical traction therapy. Am J Phys Med Rehabil. 1999;78(1):30–32. doi: 10.1097/00002060-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Valtonen EJ, Kiuru E. Cervical traction as a therapeutic tool. A clinical anlaysis based on 212 patients. Scand J Rehabil Med. 1970;2(1):29–36. [PubMed] [Google Scholar]
- 32.van der Heijden GJ, Beurskens AJ, Koes BW, Assendelft WJ, de Vet HC, Bouter LM. The efficacy of traction for back and neck pain: a systematic, blinded review of randomized clinical trial methods. Phys Ther. 1995;75(2):93–104. doi: 10.1093/ptj/75.2.93. [DOI] [PubMed] [Google Scholar]
- 33.Wong AM, Lee MY, Chang WH, Tang FT. Clinical trial of a cervical traction modality with electromyographic biofeedback. Am J Phys Med Rehabil. 1997;76(1):19–25. doi: 10.1097/00002060-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Bush K, Hillier S. Outcome of cervical radiculopathy treated with periradicular/epidural corticosteroid injections: a prospective study with independent clinical review. Eur Spine J. 1996;5(5):319–325. doi: 10.1007/BF00304347. [DOI] [PubMed] [Google Scholar]
- 35.Castagnera L, Maurette P, Pointillart V, Vital JM, Erny P, Senegas J. Long-term results of cervical epidural steroid injection with and without morphine in chronic cervical radicular pain. Pain. 1994;58(2):239–243. doi: 10.1016/0304-3959(94)90204-6. [DOI] [PubMed] [Google Scholar]
- 36.Kwon JW, Lee JW, Kim SH, et al. Cervical interlaminar epidural steroid injection for neck pain and cervical radiculopathy: effect and prognostic factors. Skeletal Radiol. 2007;36(5):431–436. doi: 10.1007/s00256-006-0258-2. [DOI] [PubMed] [Google Scholar]
- 37.Lee JW, Park KW, Chung SK, et al. Cervical transforaminal epidural steroid injection for the management of cervical radiculopathy: a comparative study of particulate versus non-particulate steroids. Skeletal Radiol. 2009;38(11):1077–1082. doi: 10.1007/s00256-009-0735-5. [DOI] [PubMed] [Google Scholar]
- 38.van Gijn J, Reiners K, Toyka KV, Braakman R. Management of cervical radiculopathy. Eur Neurol. 1995;35(6):309–320. doi: 10.1159/000117174. [DOI] [PubMed] [Google Scholar]
- 39.Waldman SD. Complications of cervical epidural nerve blocks with steroids: a prospective study of 790 consecutive blocks. Reg Anesth. 1989;14(3):149–151. [PubMed] [Google Scholar]
- 40.Benny B, Azari P, Briones D. Complications of cervical transforaminal epidural steroid injections. Am J Phys Med Rehabil. 2010;89(7):601–607. doi: 10.1097/PHM.0b013e3181e2d07c. [DOI] [PubMed] [Google Scholar]
- 41.Beneliyahu DJ. Chiropractic management and manipulative therapy for MRI documented cervical disk herniation. J Manipulative Physiol Ther. 1994;17(3):177–185. [PubMed] [Google Scholar]
- 42.Hubka MJ, Phelan SP, Delaney PM, Robertson VL. Rotary manipulation for cervical radiculopathy: observations on the importance of the direction of the thrust. J Manipulative Physiol Ther. 1997;20(9):622–627. [PubMed] [Google Scholar]
- 43.Di Fabio RP. Manipulation of the cervical spine: risks and benefits. Phys Ther. 1999;79(1):50–65. [PubMed] [Google Scholar]
- 44.Fessler RG, Sekhar LN. Atlas of neurosurgical techniques : spine and peripheral nerves. New York: Thieme; 2006. [Google Scholar]
- 45.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15(6):602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 46.Estridge MN, Smith RA. Anterior Cervical Fusion; Solution of a Particular Problem. J Neurosurg. 1963;20:441–444. doi: 10.3171/jns.1963.20.5.0441. [DOI] [PubMed] [Google Scholar]
- 47.Abd-Alrahman N, Dokmak AS, Abou-Madawi A. Anterior cervical discectomy (ACD) versus anterior cervical fusion (ACF), clinical and radiological outcome study. Acta Neurochir (Wien). 1999;141(10):1089–1092. doi: 10.1007/s007010050487. [DOI] [PubMed] [Google Scholar]
- 48.Barlocher CB, Barth A, Krauss JK, Binggeli R, Seiler RW. Comparative evaluation of microdiscectomy only, autograft fusion, polymethylmethacrylate interposition, and threaded titanium cage fusion for treatment of single-level cervical disc disease: a prospective randomized study in 125 patients. Neurosurg Focus. 2002;12(1):E4. doi: 10.3171/foc.2002.12.1.5. [DOI] [PubMed] [Google Scholar]
- 49.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. Sep. 1993;75(9):1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 50.Heary RF, Ryken TC, Matz PG, et al. Cervical laminoforaminotomy for the treatment of cervical degenerative radiculopathy. J Neurosurg Spine. 2009;11(2):198–202. doi: 10.3171/2009.2.SPINE08722. [DOI] [PubMed] [Google Scholar]
- 51.Madawi AA, Powell M, Crockard HA. Biocompatible osteoconductive polymer versus iliac graft. A prospective comparative study for the evaluation of fusion pattern after anterior cervical discectomy. Spine (Phila Pa 1976) 1996;21(18):2123–2129. doi: 10.1097/00007632-199609150-00013. [DOI] [PubMed] [Google Scholar]
- 52.Watters WC, 3rd, Levinthal R. Anterior cervical discectomy with and without fusion. Results, complications, and long-term follow-up. Spine (Phila Pa 1976) 1994;19(20):2343–2347. doi: 10.1097/00007632-199410150-00016. [DOI] [PubMed] [Google Scholar]
- 53.Jho HD. Microsurgical anterior cervical foraminotomy for radiculopathy: a new approach to cervical disc herniation. J Neurosurg. 1996;84(2):155–160. doi: 10.3171/jns.1996.84.2.0155. [DOI] [PubMed] [Google Scholar]
- 54.Jho HD, Kim MH, Kim WK. Anterior cervical microforaminotomy for spondylotic cervical myelopathy: part 2. Neurosurgery. 2002;51(5 Suppl):S54–S59. [PubMed] [Google Scholar]
- 55.Johnson JP, Filler AG, McBride DQ, Batzdorf U. Anterior cervical foraminotomy for unilateral radicular disease. Spine (Phila Pa 1976) 2000;25(8):905–909. doi: 10.1097/00007632-200004150-00002. [DOI] [PubMed] [Google Scholar]
- 56.Boakye M, Mummaneni PV, Garrett M, Rodts G, Haid R. Anterior cervical discectomy and fusion involving a polyetheretherketone spacer and bone morphogenetic protein. J Neurosurg Spine. 2005;2(5):521–525. doi: 10.3171/spi.2005.2.5.0521. [DOI] [PubMed] [Google Scholar]
- 57.Davis RA. A long-term outcome study of 170 surgically treated patients with compressive cervical radiculopathy. Surg Neurol. 1996;46(6):523–530. doi: 10.1016/S0090-3019(96)00278-9. [DOI] [PubMed] [Google Scholar]
- 58.McGuire KJ, Harrast J, Herkowitz H, Weinstein JN. Geographic Variation in the Surgical Treatment of Degenerative Cervical Disc Disease: American Board of Orthopedic Surgery (ABOS) Quality Improvement Initiative; Part II Candidates. Spine (Phila Pa 1976). Feb 4 2011. [DOI] [PMC free article] [PubMed]
- 59.Fraser JF, Hartl R. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine. 2007;6(4):298–303. doi: 10.3171/spi.2007.6.4.2. [DOI] [PubMed] [Google Scholar]
- 60.Samartzis D, Shen FH, Lyon C, Phillips M, Goldberg EJ, An HS. Does rigid instrumentation increase the fusion rate in one-level anterior cervical discectomy and fusion? Spine J. 2004;4(6):636–643. doi: 10.1016/j.spinee.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 61.Peolsson A, Peolsson M. Predictive factors for long-term outcome of anterior cervical decompression and fusion: a multivariate data analysis. Eur Spine J. 2008;17(3):406–414. doi: 10.1007/s00586-007-0560-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Park HW, Lee JK, Moon SJ, Seo SK, Lee JH, Kim SH. The efficacy of the synthetic interbody cage and Grafton for anterior cervical fusion. Spine (Phila Pa 1976) 2009;34(17):E591–E595. doi: 10.1097/BRS.0b013e3181ab8b9a. [DOI] [PubMed] [Google Scholar]
- 63.Jawahar A, Cavanaugh DA, Kerr EJ, 3rd, Birdsong EM, Nunley PD. Total disc arthroplasty does not affect the incidence of adjacent segment degeneration in cervical spine: results of 93 patients in three prospective randomized clinical trials. Spine J. 2010;10(12):1043–1048. doi: 10.1016/j.spinee.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 64.Song KJ, Choi BW, Kim GH, Song JH. Usefulness of polyetheretherketone (PEEK) cage with plate augmentation for anterior arthrodesis in traumatic cervical spine injury. Spine J. 2010;10(1):50–57. doi: 10.1016/j.spinee.2009.08.458. [DOI] [PubMed] [Google Scholar]
- 65.Papadopoulos EC, Huang RC, Girardi FP, Synnott K, Cammisa FP., Jr Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Spine (Phila Pa 1976) 2006;31(8):897–902. doi: 10.1097/01.brs.0000209348.17377.be. [DOI] [PubMed] [Google Scholar]
- 66.Uribe JS, Sangala JR, Duckworth EA, Vale FL. Comparison between anterior cervical discectomy fusion and cervical corpectomy fusion using titanium cages for reconstruction: analysis of outcome and long-term follow-up. Eur Spine J. 2009;18(5):654–662. doi: 10.1007/s00586-009-0897-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Coric D, Nunley PD, Guyer RD, et al. Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex|C artificial disc investigational device exemption study with a minimum 2-year follow-up. J Neurosurg Spine. Jun 24 2011. [DOI] [PubMed]
- 68.Caspar W, Geisler FH, Pitzen T, Johnson TA. Anterior cervical plate stabilization in one- and two-level degenerative disease: overtreatment or benefit? J Spinal Disord. 1998;11(1):1–11. doi: 10.1097/00002517-199802000-00001. [DOI] [PubMed] [Google Scholar]
- 69.Kozak JA, Hanson GW, Rose JR, Trettin DM, Tullos HS. Anterior discectomy, microscopic decompression, and fusion: a treatment for cervical spondylotic radiculopathy. J Spinal Disord. 1989;2(1):43–46. doi: 10.1097/00002517-198903000-00006. [DOI] [PubMed] [Google Scholar]
- 70.Ducker TB, Zeidman SM. The posterior operative approach for cervical radiculopathy. Neurosurg Clin N Am. 1993;4(1):61–74. doi: 10.1016/S1042-3680(18)30608-9. [DOI] [PubMed] [Google Scholar]
- 71.Korinth MC, Kruger A, Oertel MF, Gilsbach JM. Posterior foraminotomy or anterior discectomy with polymethyl methacrylate interbody stabilization for cervical soft disc disease: results in 292 patients with monoradiculopathy. Spine (Phila Pa 1976) 2006;31(11):1207–1214. doi: 10.1097/01.brs.0000217604.02663.59. [DOI] [PubMed] [Google Scholar]
- 72.Witzmann A, Hejazi N, Krasznai L. Posterior cervical foraminotomy. A follow-up study of 67 surgically treated patients with compressive radiculopathy. Neurosurg Rev. 2000;23(4):213–217. doi: 10.1007/PL00011957. [DOI] [PubMed] [Google Scholar]
- 73.Jagannathan J, Sherman JH, Szabo T, Shaffrey CI, Jane JA. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: a single-surgeon experience with a minimum of 5 years’ clinical and radiographic follow-up. J Neurosurg Spine. 2009;10(4):347–356. doi: 10.3171/2008.12.SPINE08576. [DOI] [PubMed] [Google Scholar]
- 74.Grieve JP, Kitchen ND, Moore AJ, Marsh HT. Results of posterior cervical foraminotomy for treatment of cervical spondylitic radiculopathy. Br J Neurosurg. 2000;14(1):40–43. doi: 10.1080/02688690042898. [DOI] [PubMed] [Google Scholar]
- 75.Herkowitz HN, Kurz LT, Overholt DP. Surgical management of cervical soft disc herniation. A comparison between the anterior and posterior approach. Spine (Phila Pa 1976) 1990;15(10):1026–1030. doi: 10.1097/00007632-199015100-00009. [DOI] [PubMed] [Google Scholar]
- 76.Campbell PG, Yadla S, Malone J, et al. Early complications related to approach in cervical spine surgery: single-center prospective study. World Neurosurg. 2010;74(2–3):363–368. doi: 10.1016/j.wneu.2010.05.034. [DOI] [PubMed] [Google Scholar]