Abstract
Background
It is widely believed that a deep implant infection leads to poor functional and emotional outcomes following total hip arthroplasty.
Questions/Purpose
The purpose of this retrospective comparative review was to determine if patients who undergo two-stage, septic revision hip arthroplasty will have decreased emotional and general health scores, in addition to decreased function, compared to the aseptic revision group.
Patients and Methods
One hundred forty-five of 195 patients who underwent aseptic total hip revision for aseptic loosening (mean follow-up = 61 months) and 45 of 73 patients who underwent two-stage, septic revision hip arthroplasty (mean follow-up = 48 months) met the inclusion criteria and had a technically successful outcome. All patients were retrospectively evaluated using Harris Hip Scores (HHS), ad hoc questions, and the SF-36 Health Survey.
Results
The average HHS were 73.2 ± 20.5 (aseptic) and 57.4 ± 20.6 (septic). Significant differences in the SF-36 Health Survey were found between the two groups in: physical functioning (p = 0.026) and role limitations due to physical health (p = 0.004). No significant difference in SF-36 scores was seen in: Energy/Fatigue, General Health Perception, Personal or Emotional Problems, Role Limitations due to Emotional Well Being, Social Functioning, and Bodily Pain.
Conclusions
Two-stage, septic revision produces a poor functional outcome compared to aseptic revision; however, the overall impact of a septic revision emotionally and socially was not significantly different than patients undergoing aseptic revision.
Keywords: septic, aseptic, revision, outcomes, hip arthroplasty
Introduction
Due to an increasing number of primary total hip arthroplasties (THA) performed and an increasing life expectancy in the USA, the number of patients undergoing revision hip arthroplasty is on the rise [10]. Although a highly successful operation, the most common reasons for failure following a primary total hip replacement are instability/dislocation (22.5%), mechanical loosening (19.7%), and infection (14.8%) [2]. Thus, revision THA is generally subclassified as being either aseptic (e.g., for instability or mechanical loosening) or septic. The difference in functional and emotional outcomes in patients undergoing aseptic as opposed to septic revision THA is largely unknown.
The majority of the current literature on aseptic revision THA focuses on the long-term success or survival of a specific type of implant or procedure, using improvements in the Harris Hip Score as the primary outcome [3, 5, 6, 8, 9, 11–13, 15–20, 22, 23]. As a result, the general health of these patients has not been adequately studied. Furthermore, although patients with a deep implant infection are thought to have a poor functional outcome [1, 21], the emotional outcome and overall health of these patients are understudied, and publications on the topic are limited by small numbers of patients [14]. It was our expectation that patients undergoing two-stage septic revision hip arthroplasty will have a lower emotional well-being and general health as a result of poor function, when compared to patients undergoing aseptic revision total hip arthroplasty.
Thus, the objective of the current study was to compare the functional, emotional, and general health outcomes between a large cohort of patients undergoing aseptic total hip revision, and two-stage septic revision. Specifically, we wished to compare an assessment of hip function using the Harris Hip Score, and an assessment of overall health as reflected by the SF-36 Health Survey between these groups of patients. We also aimed to compare these patients' subjective assessment of their outcome as reflected by their description of pain, ability to use transportation, walk distances, and sit.
Materials and Methods
This retrospective comparative review analyzed patients who underwent revision total hip arthroplasty between 1996 and 2002. One hundred ninety-five consecutive patients underwent an aseptic total hip revision, and 73 consecutive patients had a two-stage, septic revision hip arthroplasty. Two-stage revision included an irrigation and thorough debridement of the infected hip, followed by explantation of the acetabular and femoral components, cement spacer placement, interval intravenous antibiotics, and replantation of the components after confirmation of a cleared infection. All aseptic revisions were performed for aseptic loosening of the femoral, acetabular, or both components, whereas all the septic revisions were performed because of deep implant infection and thus required explant and revision of both the femoral and acetabular components in all patients. There were no differences between the aseptic and septic revision groups with regard to age, body mass index, and number of prior total hip arthroplasties (p > 0.05) (Table 1).
Table 1.
Demographic data
| Aseptic | Septic | |
|---|---|---|
| Males/females | 83/112 | 37/36 |
| Age (range in years) | 62 (16–87) | 67 (57–76) |
| BMI (range in kg/m2) | 27 (18–51) | 27 (16–49) |
| Prior arthroplasties | 1.7 | 2.1 |
| Average follow-up (range in months) | 61 (24–116) | 48 (24–112) |
Patients were retrospectively evaluated using Harris Hip Scores and RAND SF-36 Health Surveys obtained from patient's charts, which were completed at the patient's last follow-up visit at the senior author's office (CG). Both the SF-36 scores and the Harris Hip Scores were manually calculated by one of the authors (FB). The exclusion criteria included recurrent infection in the septic group, new infection in the aseptic group, further aseptic revisions during the follow-up period in both groups, and death. Of the 73 patients in the septic group, 9 patients had a recurrent infection, 4 patients underwent aseptic revision(s), and 15 patients died. Of the 195 patients undergoing aseptic revision surgery, 1 patient had an infection, 33 patients underwent a subsequent aseptic revision, and 16 patients died during the follow-up. Therefore, 45 patients with a septic revision and 145 patients with an aseptic revision were included in the study analysis.
In addition to the HHS and SF-36 Health Survey, all patients were given a list of ad hoc questions with predetermined responses to determine the extent of their pain (none, mild, moderate to severe), the mode of public transportation they could use (car, bus, train, plane), the distance they could walk (unlimited, 200–600 m, in house only), and their ability to sit (unlimited, high chair <30 min, unable).
The data were analyzed using the nonparametric Mann–Whitney test to compare mean Harris Hip Scores between the two groups, and the nonparametric Kruskal–Wallis test to assess variance across the groups in regard to their Harris Hip Scores and SF-36 results. p values of <0.05 were considered statistically significant.
Results
At the final follow-up, patients who had undergone aseptic revision had better HHS than those undergoing septic revision (p < 0.001). Those undergoing aseptic revision had an average Harris Hip Score of 73.2 ± 20.5 (range, 18 to 100) compared to an average score of 57.4 ± 20.6 (range, 12 to 100) in the septic group. The Kruskal–Wallis test showed a statistically significant difference in the Harris Hip Scores between the two groups (p < 0.01).
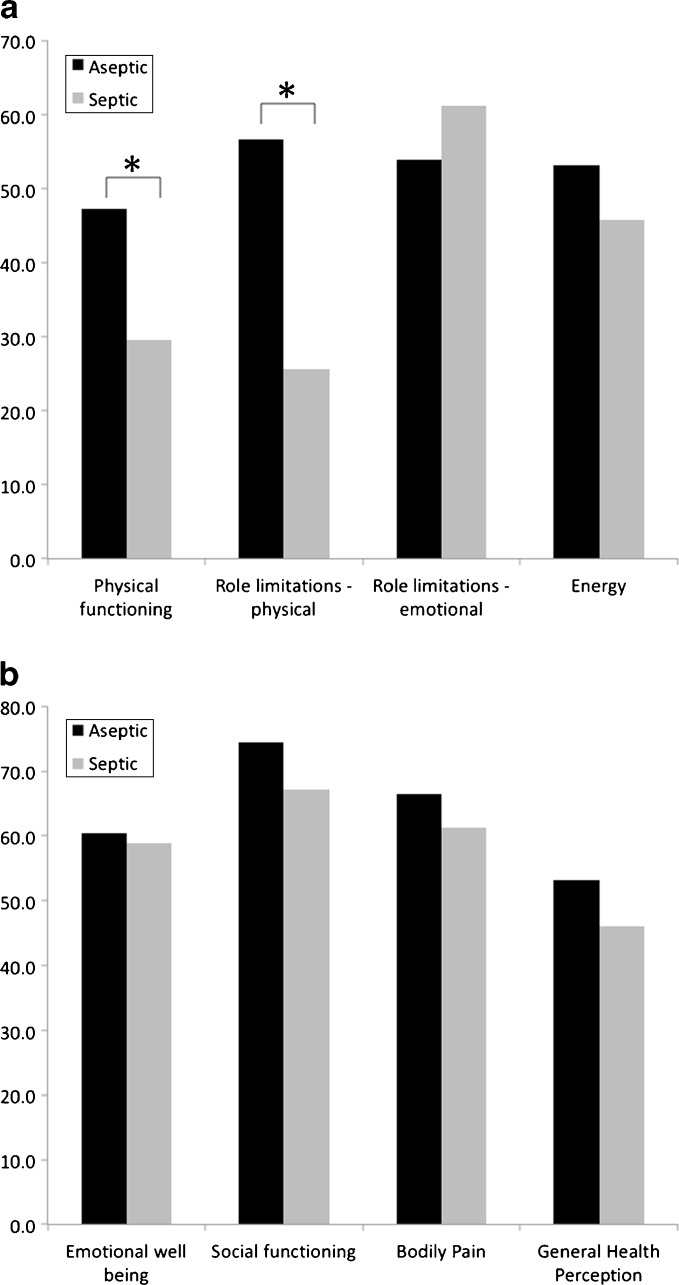
In regard to the RAND SF-36 Health Survey, statistically significant differences were found between the aseptic and septic groups in the categories of physical functioning (p = 0.026) and role limitations due to physical health (p ≤ 0.004). However, there was no difference in role limitations due to emotional or personal problems (p = 0.323), emotional well-being (p = 0.942), social functioning (p = 0.552), energy/fatigue (p = 0.188), general health (p = 0.069), and bodily pain (p = 0.658) (Fig. 1a, b).
Fig. 1.
The components of the RAND SF-36-item Health Survey. a Physical Functioning, Role Limitations due to Physical Health Problems, Role Limitations due to Personal or Emotional Problems, and Energy/Fatigue. b Emotional Well-Being, Social Functioning, Bodily Pain, and General Health Perception. *p < 0.05 (significant differences found between the two-stage septic and aseptic revision patients)
As an observation in regard to the ad hoc questions, patients in the aseptic group had improved pain and sitting ability, could walk farther, and were able to use more modes of transportation than the septic group (Table 2).
Table 2.
Ad hoc questions
| Aseptic | Septic | |
|---|---|---|
| Pain scale | ||
| None | 43.00% | 32.60% |
| Mild | 32.50% | 28.20% |
| Moderate to severe | 24.50% | 39.20% |
| Walking ability | ||
| Unlimited | 45.20% | 21.70% |
| 200–600 m | 35.50% | 40.30% |
| In house | 19.30% | 38.00% |
| Sitting ability | ||
| Unlimited | 86.70% | 67.40% |
| High chair <30 min | 8.90% | 28.30% |
| Unable | 4.40% | 4.30% |
| Mode of transportation able to use | ||
| Car | 94.40% | 70.60% |
| Bus | 68.40% | 44.10% |
| Train | 60.70% | 29.40% |
| Plane | 37.60% | 17.60% |
Discussion
The objective of the current study was to compare the functional, emotional, and general health outcomes in patients undergoing two-stage septic revision and aseptic revision hip arthroplasty using Harris Hip Scores, SF-36 Health Surveys, and ad hoc questions. Our hypothesis was that functional, emotional, and general health outcomes would be worse in patients undergoing two-stage septic revision total hip arthroplasty compared to patients undergoing aseptic revision for loosening. Functional outcomes, as measured by the Harris Hip Scores, functional components of the SF-36 survey, and observation of ad hoc questions were in fact significantly worse in patients undergoing septic revision hip arthroplasty; however, the emotional and social outcomes, as assessed by the emotional, social, and general health components of the SF-36 survey, were similar between patients undergoing revision for deep implant infection and patients undergoing aseptic revision in medium-term follow-up.
There are several other limitations to our study. First of all, our study is retrospective, and thus, has all the inherent flaws of this study design. Secondly, all of the surgeries were performed before 2002. Therefore, there is a possibility that had these surgeries been performed recently, given the recent improvements of implants and surgical technique over the last 9 years, patients might have had better functional outcomes in all groups. Furthermore, comorbidities were not assessed in this study, which may have had an impact on SF-36 scores.
By the year 2026, the number of people undergoing revision hip arthroplasty is expected to double [7]. While most patients undergoing primary total hip arthroplasty can expect an excellent outcome with a Harris Hip Score >90, the average Harris Hip Scores for revision total hip arthroplasty is <90 in most reports [4]. However, the data are limited regarding the difference in outcomes following aseptic and septic revision THA. In a smaller cohort of patients, using Harris Hip Scores and SF-12 scores, Romano et al. [14] found no significant difference in outcomes between two-stage revision hip arthroplasty and aseptic revision [14]. In the current study, differences existed between the two groups with regard to their physician-reported and self-reported functional outcome, which is in accordance with the general perception that patients who have had a deep implant infection have a less predictable functional outcome [1, 21]. As a result of a lack of physical function, it was hypothesized that a revision for deep implant infection would negatively impact a patient emotionally and socially more than an aseptic revision. However, like Romano et al., we found this not be true [14]. Still, we did find that “physical functioning” and “role limitations due to physical health” were significantly different between the two groups.
In summary, the current study highlights that although septic revisions have a worse functional outcome compared to aseptic revisions, similar to prior published literature, the emotional and general health outcomes are comparable to aseptic revisions in medium-term follow-up.
Acknowledgments
This study was partially funded by the Eduardo Salvati Resident Research Grant (MBC).
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participating in the study was obtained.
This work was performed at the Münster University Hospital.
Level of evidence: Level III therapeutic study. See levels of evidence for a complete description.
References
- 1.Barrack RL, Engh G, Rorabeck C, Sawhney J, Woolfrey M. Patient satisfaction and outcome after septic versus aseptic revision total knee arthroplasty. J Arthroplasty. 2000;15:990–993. doi: 10.1054/arth.2000.16504. [DOI] [PubMed] [Google Scholar]
- 2.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 3.Gallo J, Rozkydal Z, Sklensky M. Reconstruction of severe acetabular bone defects using Burch-Schneider cage. Acta Chir Orthop Traumatol Cech. 2006;73:157–163. [PubMed] [Google Scholar]
- 4.Hozack WJ, Rothman RH, Albert TJ, Balderston RA, Eng K. Relationship of total hip arthroplasty outcome to other orthopaedic procedures. Clin Orthop Relat Res. 1997;344:88–93. doi: 10.1097/00003086-199711000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Ito H, Matsuno T, Aok Y, Minami A. Total hip arthroplasty using an omniflex modular system: 5 to 12 years follow-up. Clin Orthop Relat Res. 2004;419:98–106. doi: 10.1097/00003086-200402000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Korovessis P, Repantis T. High Medium-term Survival of Zweymuller SLR-Plus((R)) Stem Used in Femoral Revision. Clin Orthop Relat Res. 2009;467:2032–2040. doi: 10.1007/s11999-009-0760-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005-2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 8.Lai KA, Shen WJ, Yang CY, Lin RM, Lin CJ, Jou IM. Two-stage cementless revision THR after infection. 5 recurrences in 40 cases followed 2.5–7 years. Acta Orthop Scand. 1996;67:325–328. doi: 10.3109/17453679609002324. [DOI] [PubMed] [Google Scholar]
- 9.Ochs BG, Volkmann R, Eingartner C, Ludolph I, Weller S, Weise K, Ochs U. Treatment of large femoral bone defects–15-year experiences with the cementless Bicontact revision stem with distal interlocking. Z Orthop Unfall. 2007;145(Suppl 1):S34–S39. doi: 10.1055/s-2007-965658. [DOI] [PubMed] [Google Scholar]
- 10.Ong KL, Mowat FS, Chan N, Lau E, Halpern MT, Kurtz SM. Economic burden of revision hip and knee arthroplasty in Medicare enrollees. Clin Orthop Relat Res. 2006;446:22–28. doi: 10.1097/01.blo.0000214439.95268.59. [DOI] [PubMed] [Google Scholar]
- 11.Ornstein E, Linder L, Ranstam J, Lewold S, Eisler T, Torper M. Femoral Impaction bone grafting with the Exeter stem - the Swedish experience: survivorship analysis of 1305 revisions performed between 1989 and 2002. J Bone Joint Surg Br. 2009;91:441–446. doi: 10.1302/0301-620X.91B4.21319. [DOI] [PubMed] [Google Scholar]
- 12.Park KS, Yoon TR, Song EK, Lee KB. Cementless Acetabular Socket Revisions Using Metasul Metal-on-Metal Bearings. J Arthroplasty. 2010;25:533–537. doi: 10.1016/j.arth.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 13.Parratte S, Argenson JN, Flecher X, Aubaniac JM. Acetabular revision for aseptic loosening in total hip arthroplasty using cementless cup and impacted morselized allograft. Rev Chir Orthop Reparatrice Appar Mot. 2007;93:255–263. doi: 10.1016/S0035-1040(07)90247-0. [DOI] [PubMed] [Google Scholar]
- 14.Romano CL, Romano D, Logoluso N, Meani E. Septic versus aseptic hip revision: how different? J Orthop Traumatol. 2010;11:167–174. doi: 10.1007/s10195-010-0106-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schlegel UJ, Bitsch RG, Pritsch M, Aldinger PR, Mau H, Breusch SJ. Acetabular reinforcement rings in revision total hip arthroplasty: midterm results in 298 cases. Orthopade. 2008;37(904):906–913. doi: 10.1007/s00132-008-1314-5. [DOI] [PubMed] [Google Scholar]
- 16.Schlegel UJ, Bitsch RG, Pritsch M, Clauss M, Mau H, Breusch SJ. Mueller reinforcement rings in acetabular revision: outcome in 164 hips followed for 2–17 years. Acta Orthop. 2006;77:234–241. doi: 10.1080/17453670610045966. [DOI] [PubMed] [Google Scholar]
- 17.Stedry V, Dungl P, Hajny P. Revision of total hip replacement operations at the Orthoedic Clinic IPVZ in Prague, 1999. Acta Chir Orthop Traumatol Cech. 2001;68:18–23. [PubMed] [Google Scholar]
- 18.Tamvakopoulos GS, Servant CT, Clark G, Ivory JP. Medium-term follow-up series using a modular distal fixation prosthesis to address proximal femoral bone deficiency in revision total hip arthroplasty. A 5–9 year follow-up study. Hip Int. 2007;17:143–149. doi: 10.1177/112070000701700304. [DOI] [PubMed] [Google Scholar]
- 19.Tarasevicius S, Zegunis V, Tarasevicius R, Kalesinskas RJ, Janusonis V. Hip revision arthroplasty (long-term results) Med (Kaunas) 2004;40:332–337. [PubMed] [Google Scholar]
- 20.Tulic G, Dulic B, Vucetic C, Todorovic A. Our first experience with extended proximal femoral osteotomy for revision hip surgery. Hip Int. 2007;17:224–229. doi: 10.1177/112070000701700406. [DOI] [PubMed] [Google Scholar]
- 21.Wang CJ, Hsieh MC, Huang TW, Wang JW, Chen HS, Liu CY. Clinical outcome and patient satisfaction in aseptic and septic revision total knee arthroplasty. Knee. 2004;11:45–49. doi: 10.1016/S0968-0160(02)00094-7. [DOI] [PubMed] [Google Scholar]
- 22.Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;22(6 Suppl 2):151–155. doi: 10.1016/j.arth.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 23.Wu LD, Xiong Y, Yan SG, Yang QS, Dai XS. Femoral Component Revision using extensively porous-coated cementless stem. Chin J Traumatol. 2005;8:358–363. [PubMed] [Google Scholar]