Abstract
Deep venous thrombosis is extremely rare after arthroscopic shoulder surgery. In this report, we describe one such case in a patient with a history of cardiac pacemaker placement. He presented with complaints of pain and swelling in the operated extremity several days after rotator cuff surgery and underwent ultrasound evaluation that confirmed thrombosis of the axillary vein with extension into the brachial and basilic veins, down to the level of the elbow. He was treated with Coumadin, as well as enoxaparin (Lovenox) at therapeutic dosages until INR levels were in the therapeutic range. Follow-up ultrasound at 6 months demonstrated successful recanalization of the affected vessels and no further complications were noted. This is the first report we are aware of that documents axillary vein thrombosis in the setting of arthroscopic shoulder surgery. Though the patient had several risk factors for hypercoagulability, including diabetes and hypertension, we suggest that his cardiac pacemaker leads may have contributed to a thrombogenic environment and cite medical literature that reports an association with thrombosis in the axillary and subclavian veins with pacemakers and defibrillators.
Keywords: deep venous thrombosis, shoulder, arthroscopy, rotator cuff
Introduction
Deep venous thrombosis (DVT) is a commonly associated complication of open lower extremity surgery, especially hip and knee arthroplasty, with rates as high as 60% in those not treated with either mechanical or pharmacologic prophylaxis [7, 13, 16, 18]. The rates of DVT or pulmonary embolus (PE) after arthroscopic surgery, however, appear to be significantly lower, with numbers ranging from 1.5% to 17.9% [10, 11, 22, 24]. These lower rates are usually attributed to the minimally invasive nature of arthroscopic surgery which may limit the risk of thrombogenic complications.
Although DVT and PE are well-documented complications of lower extremity arthroscopic procedures, DVT or PE after shoulder arthroscopy has not been well characterized. The rate of upper extremity DVT or PE after arthroscopic shoulder surgery is not completely known, but one series of 263 arthroscopic rotator cuff repairs noted just one occurrence (0.38%) of ipsilateral upper extremity DVT(exact site unspecified) [4]. Another series of 439 patients over 10 years that underwent shoulder arthroscopy showed no cases of postoperative DVT [5].
In the recent literature, there exist case reports describing DVTs in the subclavian, basilic, and cephalic veins after arthroscopic shoulder surgery [1, 2, 5, 9, 14, 21]. However, we are aware of no published studies which describe ipsilateral axillary vein thrombosis after rotator cuff repair. In this report, we describe one such case in a patient with a history of cardiac pacemaker placement that presented several days after arthroscopic rotator cuff surgery with complaints of extremity pain and swelling and was ultimately diagnosed and treated for upper extremity DVT.
Case Report
A 68-year-old Caucasian male initially presented to the office of the senior author with a chief complaint of left shoulder pain of over 1 year and limited range of motion. The pain was most noticeable after golfing and was localized to the top of the shoulder. Night pain was noted as well. Past medical history was significant for non-insulin-dependent diabetes mellitus, hypertension, cardiac dysrhythmia, gout, and benign prostatic hyperplasia (BPH). He had previously undergone surgical treatment for appendicitis, hernia repair, and diverticulitis without complication. He also underwent placement of a cardiac pacemaker approximately 8 years prior with successful replacement 5 years after the index procedure. The patient denied tobacco and drug use, and only drank caffeine substances on an infrequent basis. Medications included anti-hypertensives, oral hypoglycemic medications, a medication for gout, and a medication for BPH.
On physical examination, the acromioclavicular joint was non-tender. Overall elevation was to 160° with minimal shrugging. Good eccentric control was present without drop-arm. Slight loss of terminal internal and external rotation was noted along with positive impingement signs. Elevation and external rotation power demonstrated just trace weakness. Lift-off test was negative.
MRI of the shoulder was precluded due to the cardiac pacemaker; therefore, the patient underwent ultrasound examination of the left shoulder. Ultrasound demonstrated bicipital tendon sheath effusion with synovial debris; a partial thickness deep surface tear of the subscapularis tendon measuring approximately 10 mm in greatest longitudinal dimension; a partial tear of the infraspinatus tendon; and a partial tear of the supraspinatus which appeared to possibly extend into the rotator interval.
After failing conservative treatment, including a prior subacromial injection that did not provide much relief, he was indicated for arthroscopic surgery and rotator cuff repair.
Surgery was performed using the “beach chair” position with supraclavicular regional anesthesia. Intravenous antibiotics were given preoperatively.
The posterior portal was first established, followed by an anterior portal. Diagnostic arthroscopy was performed demonstrating moderately diffuse synovitis. Synovectomy was carried out. A gentle manipulation under anesthesia was performed. A high-grade partial thickness tear of the biceps tendon was identified and the decision was made to proceed with biceps tenodesis. Two sutures were shuttled through the long head of the biceps tendon and a tenotomy was performed. Next, attention was turned to the subacromial space. Significant amounts of proliferative tissue were detected and the coracoacromial ligament was noted to be hypertrophied. A subacromial decompression was then conducted, including bursectomy with a shaver and acromioplasty. A standard amount of bone (approximately 6 mm) was removed from the acromion with an arthroscopic shaver, such that the undersurface of the acromion was made flat. Once the decompression was completed, attention was returned to the rotator cuff and the supraspinatus tear was identified. A single FASTIN® RC 5-mm anchor with ORTHOCORD suture (Depuy Mitek Inc., Raynham, MA, USA) was placed at the edge of the articular margin. The supraspinatus tear was then repaired with sutures in horizontal mattress fashion. Next, attention was returned to the biceps tendon sutures. Soft tissue tenodesis of the long head of the biceps to the undersurface of the rotator interval capsular tissue was done by passing the biceps tendon sutures through the rotator interval tissue. The tenodesis was completed by tying the sutures on top of the rotator interval tissue. At the conclusion of the procedure, the extremity was placed in a shoulder immobilizer. The patient was discharged home the same day. The patient began passive range of motion of the shoulder as well as active motion of the distal extremity on postoperative day #1.
Approximately 6 days later, the patient reported the development of swelling in the ipsilateral extremity, especially the hand. On physical examination, the patient demonstrated diffuse swelling throughout the left upper extremity. There was mild tenderness to palpation, particularly along the medial aspect of the upper arm just above the antecubital fossa. Shoulder pain was minimal. His neurovascular examination was unremarkable. The arthroscopic portal sites were healing well. An ultrasound examination was performed which demonstrated a large clot extending from the axillary vein into the brachial and basilic veins, down to the level of the elbow (Figs. 1, 2 and 3). Flow was present in the internal jugular and subclavian veins. He was admitted to the hospital for anticoagulation. He was started on coumadin with therapeutic dosage lovenox as a bridge (lovenox was to be discontinued once INR was therapeutic). Coagulation profile results obtained upon admission were within normal laboratory limits (INR = 0.99, prothrombin time [PT] = 10.3 s, activated partial thrombin time [apt] = 29.0 s platelet count = 211/nl.) He was also seen and evaluated by a hematologist.
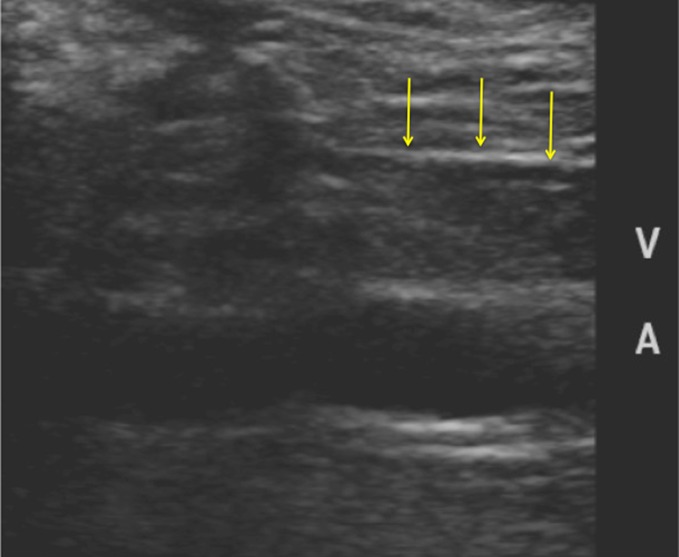
Fig. 1.
AP X-ray of left shoulder taken postoperatively demonstrating presence of cardiac pacemaker
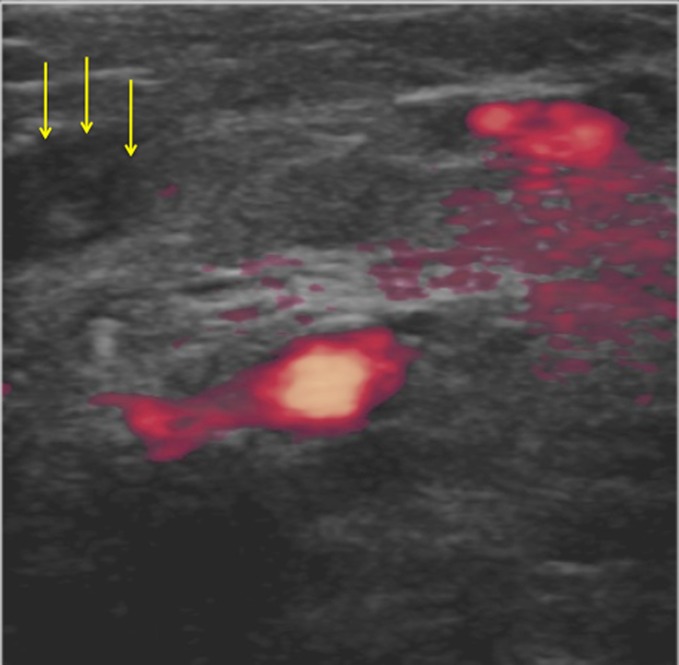
Fig. 2.
Doppler ultrasound study obtained at time of initial postoperative admission demonstrating hyperechoic material consistent with thrombus in axillary vein (arrows point to thrombus in vein)
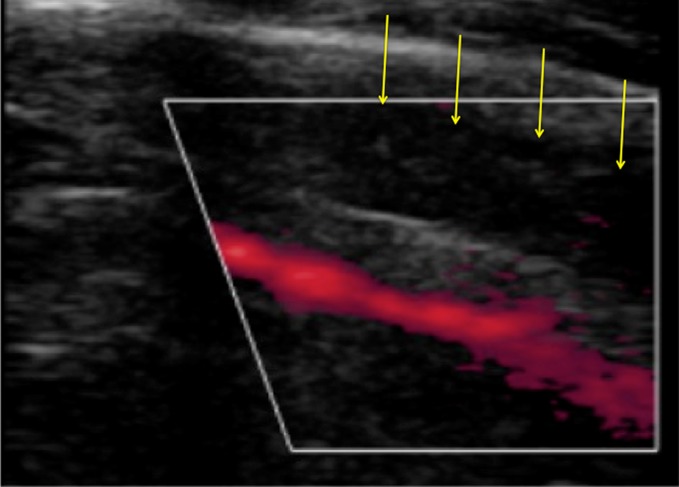
Fig. 3.
Power Doppler ultrasound study taken at time of initial postoperative admission demonstrating thrombosed brachial vein (seen in cross-section; arrows highlight thrombus)
The patient was discharged home within 1 day and scheduled to return to the office for follow-up. At the next postoperative visit 10 days after surgery, the patient noted the pain in the shoulder was improved, as was the swelling in the extremity. The patient was instructed to continue with the physical therapy program (purely passive motion with no active motion at this point).
At 6 weeks after surgery the arm swelling was noted to be much improved. The incisions were well healed. The tenderness along the medial aspect of the arm had resolved.
At 12 weeks after surgery, inspection of the upper extremity demonstrated no swelling. There was no tenderness to palpation. Range of motion and motor strength was appropriate for his stage of recovery. At 6 months postoperatively, repeat Doppler ultrasound demonstrated recanalization of the affected veins in the extremity (Fig. 4).
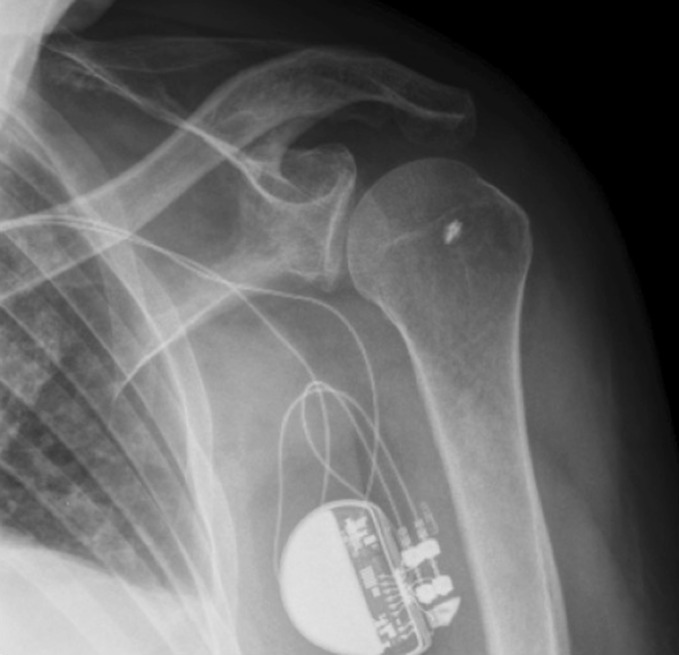
Fig. 4.
Power Doppler ultrasound study at 6 months after diagnosis of axillary vein thrombosis demonstrating recanalization of the vein (arrows point to axillary vein; arterial blood flow highlighted in red)
Discussion
This report is the first documented instance of ipsilateral axillary vein thrombosis, with extension to the basilic and brachial veins, after arthroscopic rotator cuff repair. Upper extremity vein thrombosis after an arthroscopic shoulder procedure is an uncommon complication, with only a handful of cases having been reported thus far [1, 2, 4, 9, 14, 21]. In Burkhart’s original report [5], basilic and innominate vein thrombosis was discovered in a 32-year-old male with asymptomatic Hodgkin’s lymphoma who had undergone shoulder arthroscopy in the lateral decubitus position. Cephalic vein thrombosis was noted in a separate case of an overweight male with diabetes who had a pulmonary embolus after shoulder arthroscopy was performed in the lateral decubitus position [21]. Though patient positioning has been implicated as a possible cause, other reports also note postoperative thrombosis in patients that underwent surgery in the beach chair position [8, 9]. The beach chair positioning and surgical approach used in this case are standard at our institution. The ipsilateral extremity is secured to an arm holder taking care that no portion of the extremity is placed under significant compression. Immediate after care included standard treatment such as placement in a shoulder immobilizer, and physical therapy limited to Codman/pendulum exercises. The surgery and immediate postoperative treatment in this case were, therefore, considered routine.
No systematic reviews are currently available in the literature on this topic and therefore, the risk factors for thrombosis after arthroscopy are not completely known. However, as Burkhart pointed out [5], DVT after shoulder arthroscopy should raise suspicion of a hypercoagulable state or an extrinsic mass causing venous occlusion. Bongiovanni et al. [2] provide evidence to support the notion that some of these patients with DVT after shoulder arthroscopy may have heritable thrombophilia. Their series of three patients showed mutations of key factors in the thrombotic cascade of two patients as well as elevated levels of IgG anticardiolipins, suggesting antiphospholipid antibody syndrome in another.
Paget–von Schroetter disease, often described as “spontaneous” axillosubclavian vein thrombosis (ASVT) or “effort” thrombosis, has been previously described but is often observed in physically active individuals who perform strenuous activities of the arm and shoulder. The subclavian vein is susceptible as it passes by the junction of the first rib and clavicle and repetitive forces and activities can lead to scarring and intrinsic damage [15]. However, this is a distinct clinical entity and based on the history and examination/imaging findings likely does not play a major role in the pathogenesis of the majority of the patients that undergo arthroscopic surgery and sustain a DVT in the postoperative period.
ASVT has also been associated with vein catheters and electrodes for pacemakers [3, 6, 12, 19, 20, 23]. Our particular patient had a medical history significant for pacemaker placement with subsequent replacement, approximately 3 years prior to the arthroscopic shoulder procedure. Prior to the shoulder surgery he was asymptomatic but the pacemaker electrodes, nevertheless, may have contributed to a hyercoagulable state. One prospective study noted a 14% rate of asymptomatic new obstructive venous lesions in patients that underwent pacemaker or defibrillator placement at 6 months post placement [17].
The patient’s medical history was also significant for diabetes mellitus (non-insulin-dependent type) and hypertension, which may have elevated his clotting risk. Polzhofer et al. [21] suggested that irritation of the subclavian vein by the motorized shaver may have contributed to their patient’s development of DVT and PE after arthroscopic shoulder surgery. Although this may be a plausible explanation for some cases of DVT, it is also likely that simple manipulation and positioning of the arm may lead to thrombus formation in a susceptible individual.
In conclusion, this report details a thrombotic complication in the postoperative period following arthroscopic shoulder surgery. Though it is not the first report of DVT in the ipsilateral limb after shoulder arthroscopy, it is the first report we are aware of that documents axillary vein thrombosis and attempts to raise the possibility of the contribution of pacemaker leads to this complication. Though this is still somewhat speculative, nevertheless we hope it stimulates a discussion that may lead to the development of future prevention strategies. Prospective studies are needed to better delineate risk factors for upper extremity DVT after arthroscopic surgery as well as guidelines for effective treatment and prevention.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of this case, that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Amarasekera SS, van Dalen J, Thompson TJ, Osman M. Pulmonary embolism after acromioplasty and rotator cuff repair. J Shoulder Elbow Surg. 2008;17(5):e13–e14. doi: 10.1016/j.jse.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Bongiovanni SL, Ranalletta M, Guala A, Maignon GD. Case reports: heritable thrombophilia associated with deep venous thrombosis after shoulder arthroscopy. Clin Orthop Relat Res. 2009;467(8):2196–2199. doi: 10.1007/s11999-009-0895-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Breuls NP, Res JC. Acute subclavian or axillary vein occlusion during biventricular pacemaker implantation. Pacing Clin Electrophysiol. 2006;29(10):1170–1173. doi: 10.1111/j.1540-8159.2006.00509.x. [DOI] [PubMed] [Google Scholar]
- 4.Brislin KJ, Field LD, Savoie FH., 3rd Complications after arthroscopic rotator cuff repair. Arthroscopy. 2007;23(2):124–128. doi: 10.1016/j.arthro.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Burkhart SS. Deep venous thrombosis after shoulder arthroscopy. Arthroscopy. 1990;6(1):61–63. doi: 10.1016/0749-8063(90)90100-R. [DOI] [PubMed] [Google Scholar]
- 6.Carter R, Dickerson SC, Berry R. Axillary–subclavian vein thrombosis as a complication of permanent transvenous cardiac pacing. Va Med. 1978;105(7):515–518. [PubMed] [Google Scholar]
- 7.Clagett GP, Anderson FA, Jr, Levine MN, Salzman EW, Wheeler HB. Prevention of venous thromboembolism. Chest. 1992;102(4 Suppl):391S–407S. doi: 10.1378/chest.102.4_Supplement.391S. [DOI] [PubMed] [Google Scholar]
- 8.Cortes ZE, Hammerman SM, Gartsman GM. Pulmonary embolism after shoulder arthroscopy: could patient positioning and traction make a difference? J Shoulder Elbow Surg. 2007;16(2):e16–e17. doi: 10.1016/j.jse.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 9.Creighton RA, Cole BJ. Upper extremity deep venous thrombosis after shoulder arthroscopy: a case report. J Shoulder Elbow Surg. 2007;16(1):e20–e22. doi: 10.1016/j.jse.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Cullison TR, Muldoon MP, Gorman JD, Goff WB. The incidence of deep venous thrombosis in anterior cruciate ligament reconstruction. Arthroscopy. 1996;12(6):657–659. doi: 10.1016/S0749-8063(96)90166-8. [DOI] [PubMed] [Google Scholar]
- 11.Demers C, Marcoux S, Ginsberg JS, Laroche F, Cloutier R, Poulin J. Incidence of venographically proved deep vein thrombosis after knee arthroscopy. Arch Intern Med. 1998;158(1):47–50. doi: 10.1001/archinte.158.1.47. [DOI] [PubMed] [Google Scholar]
- 12.Friedman SA, Berger N, Cerruti MM, Kosmoski J. Venous thrombosis and permanent cardiac pacing. Am Heart J. 1973;85(4):531–533. doi: 10.1016/0002-8703(73)90499-7. [DOI] [PubMed] [Google Scholar]
- 13.Geerts WH, Heit JA, Clagett GP, Pineo GF, Colwell CW, Anderson FA, Jr, Wheeler HB. Prevention of venous thromboembolism. Chest. 2001;119(1 Suppl):132S–175S. doi: 10.1378/chest.119.1_suppl.132S. [DOI] [PubMed] [Google Scholar]
- 14.Hariri A, Nourissat G, Dumontier C, Doursonian L. Pulmonary embolism following thrombosis of the brachial vein after shoulder arthroscopy. A case report. Rev Chir Orthop Traumatol. 2009;95(5):377–379. doi: 10.1016/j.otsr.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 15.Illig KA, Doyle AJ. Paget-Schroetter syndrome: A comprehensive review. J Vasc Surg. 2010;51(6):1538–1547. doi: 10.1016/j.jvs.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 16.Kakkar VV, Howe CT, Flanc C, Clarke MB. Natural history of postoperative deep-vein thrombosis. Lancet. 1969;2(7614):230–232. doi: 10.1016/S0140-6736(69)90002-6. [DOI] [PubMed] [Google Scholar]
- 17.Korkeila P, Nyman K, Ylitalo A, Koistinen J, Karjalainen P, Lund J, et al. Venous obstruction after pacemaker implantation. Pacing Clin Electrophysiol. 2007;30(2):199–206. doi: 10.1111/j.1540-8159.2007.00650.x. [DOI] [PubMed] [Google Scholar]
- 18.Lieberman JR, Geerts WH. Prevention of venous thromboembolism after total hip and knee arthroplasty. J Bone Joint Surg Am. 1994;76(8):1239–1250. doi: 10.2106/00004623-199408000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Malerba M, Radaeli A, Ragnoli B. Upper extremity deep vein thrombosis as an uncommon complication of pacemaker implantation: a case report. J Biol Regul Homeost Agents. 2009;23(4):273–275. [PubMed] [Google Scholar]
- 20.Polo-Romero FJ, Galvez-Hernandez G, Andreu-Plaza J, Atienza-Ayala SV. Axillary thrombosis and pulmonary embolism alter pacemaker implantation. An Med Interna. 2008;25(3):150–151. doi: 10.4321/s0212-71992008000300011. [DOI] [PubMed] [Google Scholar]
- 21.Polzhofer GK, Petersen W, Hassenpflug J. Thromboembolic complication after arthroscopic shoulder surgery. Arthroscopy. 2003;19(9):E129–E132. doi: 10.1016/j.arthro.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 22.Schippinger G, Wirnsberger GH, Obernosterer A, Babinski K. Thromboembolic complications after arthroscopic knee surgery. Incidence and risk factors in 101 patients. Acta Orthop Scand. 1998;69(2):144–146. doi: 10.3109/17453679809117615. [DOI] [PubMed] [Google Scholar]
- 23.Swinkels BM, Ophuis AJ, Zegers ES, Hertzberger DP, Meursing BT. Recurrent pacemaker lead induced axillary subclavian vein thrombosis. Pacing Clin Electrophysiol. 2001;24(5):910–911. doi: 10.1046/j.1460-9592.2001.00910.x. [DOI] [PubMed] [Google Scholar]
- 24.Wirth T, Schneider B, Misselwitz F, Lomb M, Tuylu H, Egbring R, Griss P. Prevention of venous thromboembolism after knee arthroscopy with low-molecular weight heparin (reviparin): results of a randomized controlled trial. Arthroscopy. 2001;17(4):393–399. doi: 10.1053/jars.2001.21247. [DOI] [PubMed] [Google Scholar]