Abstract
Objectives
To develop measures representing key constructs of the Transtheoretical Model (TTM) of behavior change as applied to advance care planning (ACP) and to examine whether associations between these measures replicate the relationships posited by the TTM.
Methods
Sequential scale development techniques were used to develop measures for Decisional Balance (Pros and Cons of behavior change), ACP Values/Beliefs (religious beliefs and medical misconceptions serving as barriers to participation), Processes of Change (behavioral and cognitive processes used to foster participation) based on responses of 304 persons age ≥ 65 years.
Results
Items for each scale/subscale demonstrated high factor loading (> .5) and good to excellent internal consistency (Cronbach α .76–.93). Results of MANOVA examining scores on the Pros, Cons, ACP Values/Beliefs, and POC subscales by stage of change for each of the six behaviors were significant, Wilks' λ= .555–.809, η2=.068–.178, p ≤ .001 for all models.
Conclusion
Core constructs of the TTM as applied to ACP can be measured with high reliability and validity.
Practice Implications
Cross-sectional relationships between these constructs and stage of behavior change support the use of TTM-tailored interventions to change perceptions of the pros and cons of participation in ACP and promote the use of certain processes of change in order to promote older persons' engagement in ACP.
1. Introduction
Conceptions of advance care planning (ACP) are changing. Traditionally, ACP has been considered as the process by which individuals can specify the care they wish to receive if they become incapable of participating in medical decision making.(1) The measure of engagement of ACP has been the completion of advance directives (ADs), including living wills and health care proxy designations. However, there are many reasons why these documents alone cannot accomplish the goal of providing patients with their preferred care during times of decisional incapacity. First, the forms are frequently not available when surrogate medical decision-making is required.(2) Second, physicians have difficulty determining whether the instructions for treatment contained in living wills and directives apply to the specific circumstances of individual patients.(3, 4) Third, even when health care proxies have been named, these proxies frequently do not know the patient's treatment preferences.(5, 6) If surrogate decision makers have preferences that differ from the patients or are unprepared to act on patients' wishes, surrogates' preferences may trump those of the patient as expressed in a living will.(4, 7) Finally, a fundamental concern has been raised about the ability of patients to “pre-specify” their wishes regarding their care(4, 8) given that people cannot generally accurately predict their future wishes.(9)
Recognizing the limitations of ADs, many experts in end-of-life care nonetheless have concluded that ACP has an important role in preparing patients and families for the difficult circumstances of serious illness and declining health.(1, 10–12) Although the specific details of the different models of ACP that have been advanced are varied, there appears to be consensus among them regarding the core elements of effective planning.(10, 11, 13–16) This includes the notions that, while not sufficient for ACP, living wills and health care proxies can be useful. However, these documents must be accompanied by enhanced communication, between both patients and loved ones, and patients and clinicians, regarding patients' goals of care.
Conceptions of how individuals engage in ACP are also changing. Traditional approaches to increasing participation focused on providing patients and surrogates with education and planning materials and have had only modest effects on increasing ACP participation.(17, 18) It has been proposed that participation in ACP could be enhanced by providing tailored intervention materials based on individuals' readiness for engagement.(17)
The Transtheoretical Model (TTM) of health behavior change provides a theoretical foundation for the consideration of ACP as a process of behavior change.(19) The TTM has been used to explain and facilitate intervention promoting change across a wide variety of behaviors.(20–24) The central organizing construct of the TTM is Stages of Change, the five stages that people move through as they prepare for and ultimately modify their behavior. These stages include Precontemplation (no intention to change behavior in the near future), Contemplation (thinking about changing behavior in the near future), Preparation (commitment to changing behavior soon), Action (a recent change in behavior), and Maintenance (ongoing behavior change). In prior work, we developed stages of change measures for the key components of ACP characterized as: a) completion of a living will; b) completion of a health care proxy; c) communication between patient and loved ones and between patient and clinicians regarding patients' views about the use of life-sustaining treatment; d) communication between patient and loved ones and between patient and clinicians regarding patients' views about quality versus quantity of life.(25)
The TTM also includes the constructs of Decisional Balance and Processes of Change (POC). Decisional Balance represents an individual's weighing of the Pros and Cons of changing their behavior. Decisional Balance assesses individuals' attitudes toward factors that serve as common barriers to and facilitators of behavior change. Therefore, while Stages of Change assesses intentions and behavior, Decisional Balance assesses attitudes. A predictable pattern has been observed of how the Pros and Cons relate to the Stages of Change. In Precontemplation, the Cons substantially outweigh the Pros. Progression through the subsequent stages is accompanied by a decrease in the Cons and increase in the Pros.(26) POC represent overt and covert activities that people use to progress through the stages of behavior change.(27) Experiential and cognitive processes are used in the earlier stages, and include include consciousness raising (e.g. increasing one's awareness of ACP) and self reevaluation (e.g. reflecting on what it means to be a person who participates in ACP). Behavioral processes are used in the later stages, and include helping relationships (finding support from others to participate in ACP) and self liberation (committing oneself to participating in ACP). The purpose of the current study was to develop measures of Decisional Balance and POC for ACP and to examine whether the associations between these constructs and Stage of Change replicate the relationships posited by the TTM.
2. Methods
2.1. Measurement Development Overview
A sequential approach to measurement development was used.(28) Initial item development and refinement was followed by three phases of analysis, including: 1) exploratory analyses; 2) confirmatory analyses; 3) external validation analyses.
2.2. Initial Item Development and Refinement
Initial item development and refinement was based on literature review supplemented with focus groups and followed by pilot testing. The literature review was focused on identifying articles that included an analysis of barriers to and/or facilitators of participation in ACP.(29–40) The review consisted of both qualitative and quantitative studies. Because these studies generally examined ACP as only completion of ADs, we conducted focus groups to examine barriers to and facilitators of ACP as a broader set of activities.(41) In addition, we used the focus groups to explore the processes that individuals used to engage in the process of ACP. A total of 10 focus groups were conducted with 63 older persons. Details regarding these participants and the conduct of the groups have been previously described.(41) A panel of experts in ACP and the TTM used the results of the literature review and focus groups to draft representative items for each of the TTM constructs.
2.2.1. Decisional balance
A total of 29 items were developed to represent the Pros (14) and Cons (15) of participation in ACP. Participants rated how important each item was in their decision whether or not to participate in ACP on a 5-point scale, ranging from 1 = “not at all important” to 5 = “extremely important.”
2.2.2. ACP values and beliefs
In addition to these factors, the literature review and focus groups revealed that some individuals hold religious beliefs and medical misconceptions that can act as barriers to ACP participation. These beliefs are different from the Cons, which include the potential losses that individuals ascribe to a behavior or decision that are factually true. In contrast, religious and medical beliefs represent ideas that either cannot be proven as true or false (e.g., religious beliefs) or are generally believed to be false but are nonetheless beliefs that are not easily changed (e.g., medical misconceptions). We decided to include these items in their own scale rather than including them as Cons because these items have different implications for intervention. It is likely that interventions will need to develop strategies to promote participation in ACP despite individuals' endorsement of these items rather than working toward decreasing their endorsement. A total of 17 items were developed to represent these beliefs, labeled ACP Values/Beliefs. Participants rated how strongly they agreed or disagreed with each statement on a 5-point scale, ranging from 1 = “strongly agree” to 5 = “strongly disagree”.
2.2.3. Processes of Change (POC)
A total of 17 items were developed to represent five Processes of Change that pilot testing revealed were most easily understood by participants as applicable to ACP. These Processes included two Experiential Processes (Consciousness Raising and Self Reevaluation) and three Behavioral Processes (Helping Relationships, Stimulus Control, and Self Liberation). Participants rated how frequently they used each Process in the past month on a 5-point scale, ranging from 1 = “almost never” to 5 = “almost always”.
2.2.4. Pilot testing and revision
The scales were pilot-tested with a total of 12 persons age 65 years and older recruited from the same population and using the same eligibility criteria as described below. Cognitive interviewing was performed with pilot participants, who were asked to think aloud as they responded to the questions in order to explain what they thought the question meant and how they were choosing their response. Items were extensively revised according to the results of these interviews in order to improve the clarity of instruction sets, items, and response categories.
2.3. Participants
Participants (N=304) for the analytic phase of the study were age 65 years and older recruited from two primary care practices and one senior center. These sites were purposefully selected in order to provide access to a group of older persons with diversity in race, socioeconomic status, and health status. In the primary care practices, letters were sent to sequential persons age ≥ 65 who were screened by their physician as not having a diagnosis of dementia. Persons who agreed (92% and 88% in the two practices) underwent a telephone screen to determine exclusion criteria, which included: non-English speaker (7% and 2%), hearing loss precluding participation in interview (7% and 1%), nursing home resident (0% and 1%), acute episode of illness (8% and 4%), and cognitive impairment, defined as <2/3 recall on a test of short-term memory (7% and <1%). Among eligible participants, 83% and 80% completed interviews. In the senior center, volunteers were solicited for participation. All senior center persons who volunteered were eligible for participation and completed interviews (100%).
2.4. Data Collection
All procedures and surveys for this study were approved for human subject participation by the Yale University Human Investigations Committee. Participants were interviewed in person by trained research assistants. In addition to the items described above, the interview included measures of sociodemographic status (age, ethnicity, race, education, sufficiency of monthly income,(42) marital status, and household composition); health status (self-rated health,(43) quality of life, chronic conditions, instrumental activities of daily living,(44)and stages of change for the six ACP behaviors described in the Introduction.
2.5. Analysis
For the Decisional Balance and ACP Attitudes/Values scales, the overall study cohort of 304 participants was randomly split into two subsamples. For these two scales, exploratory analyses were conducted on the first subsample (n=146), and confirmatory analyses were conducted on the second subsample (n=158). Due to the size and complexity of the POC scale, a single set of analyses was conducted on the full sample (N=304).
2.5.1. Exploratory analyses
Principal components analysis (PCA) with varimax rotation was conducted on each item set within the first subsample. The number of components to retain was based on the minimum average partial procedure (45) and parallel analysis.(46) The aims of these analyses were to: 1) determine the number of components present and estimate the correlation between them; 2) provide estimates of the factor loadings; 3) estimate internal consistency for each component using Cronbach's alpha. Item selection was an iterative process, in which items with loadings on multiple factors and items with poor loadings (<.40) were removed, and analyses were repeated. Final item selection was also determined on the basis of item clarity, lack of redundancy, and conceptual breadth.
2.5.2. Confirmatory analyses
Structural equation measurement modeling on the second subsample for the Decisional Balance and the ACP Values/Beliefs scales was conducted. Five fit indices were calculated, including: 1) the likelihood ratio chi-square statistic; 2) the goodness of fit index (GFI); 3) the comparative fit index (CFI); 4) the average absolute standardized residual statistic (AASR); 5) the root mean squared error of approximation (RMSEA). Traditionally, values of GFI and CFI above .80 indicate good fit, while values above .90 indicate excellent fit (Hu & Bentler, 1998). For the AASR and RMSEA, values below .06 indicate excellent fit (Tabachnik, 2001; Kline, 2005).
2.5.3. Processes of Change
For the POC scale, exploratory analyses were conducted utilizing structural equation measurement modeling. The aims of these analyses were to: 1) provide estimates of the factor loadings and 2) estimate internal consistency for each component using Cronbach's alpha. Item selection was an iterative process, in which items with poor loadings (<.40) were removed, and analyses were repeated. Final item selection was also determined on the basis of item clarity, lack of redundancy, and conceptual breadth.
2.5.4. External validation
The TTM hypothesizes that individuals in different stages of change will differ significantly on their scores for the Pros, Cons and the POC subscales. The challenge for examining this hypothesis is that ACP consists of multiple different behaviors. Our prior work demonstrated that individuals were frequently in different stages for the different behaviors, without any evidence of an ordering or hierarchy in which participants completed the different behaviors(47). Therefore, we could not create a composite staging variable that encompassed all of the different components of ACP. Instead, Multivariate Analysis of Variance (MANOVA) tests were conducted on all TTM variables by stage of change for each of the six behaviors as presented in the Introduction. In order to provide an example of the magnitude of change in the scales and subscales according to stage of change, we examined scale scores for the behavior of living will completion. In order to facilitate comparison in the magnitude of differences in scale scores among the different subscales and between the results of this study and previous studies examining TTM scales,(26) raw scores were converted to T-scores (mean=50, standard deviation [SD] =10).
3. Results
3.1. Initial Item Development and Refinement
Pilot testing revealed several challenges in administering the TTM scales to older persons. First, participants had difficulty understanding the initial response categories for the decisional balance scale. By asking participant how important each item was to their decision to plan for their future medical care, the response format required participants first to decide first whether or not they agreed with the item and then to decide its importance. We found that participants became confused by this task. Based on this and on meta-analytic evidence that response format had a minimal effect on the constructs,(26) we modified the response format to ask participants how strongly they agreed with each item with response categories ranging from 1 = “strongly agree” to 5 = “strongly disagree”. A second change affecting nearly all of the items was the need to refer to advance care planning in each item. The items were originally worded to represent the attitude only. We found that participants did not consistently think about this attitude as it related to advance care planning unless this term was repeated.
3.2. Participants
The participants had a mean age of 75 (sd=7.1) years. The majority were female and white. Participants had a mean of 3.8 (sd=2.2) chronic conditions, and 20% had 1 or more IADL disabilities. All participant characteristics are presented in Table 1.
Table 1.
Descriptive characteristics of participants (N=304) Characteristic
| Mean (sd) | |
|---|---|
| Age | 75 (7.1) |
| Chronic diseases | 3.8 (2.2) |
| % | |
|---|---|
| Female | 73 |
| Non-white ethnicity | 26 |
| > High school education | 73 |
| Married | 46 |
| Lives alone | 46 |
| ≥ 1 IADL disability | 20 |
| Self-rated health - fair/poor | 22 |
| Quality of life- fair/poor | 17 |
3.3. Exploratory Analyses
3.3.1. Decisional Balance
The 28 items were included in a principal components analysis (PCA). MAP and parallel analysis suggested two factors, and three items were eliminated. Through an additional 6 PCAs, the 25 items were further reduced to twelve, equally representing the Pros and Cons. The final PCA demonstrated that all item loadings were >.60, and internal consistencies were high for both the Pros (α = .86) and the Cons (α = .86). These two factors accounted for 59% of the total item variance.
3.3.2. ACP Values/Beliefs
All 17 items were included in a PCA. MAP and parallel analysis suggested a single factor. The 17 items were reduced to seven through a series of 3 additional PCAs, with items removed because of either poor loadings or repetitive content. The final PCA demonstrated that all item loadings were >.60, internal consistency was high (α = .89), and the factor accounted for 60% of the total item variance.
3.4. Confirmatory Analyses
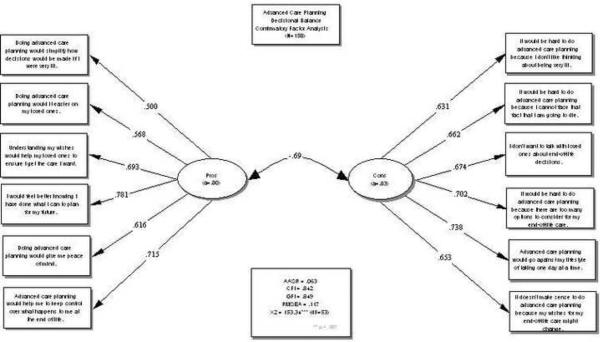
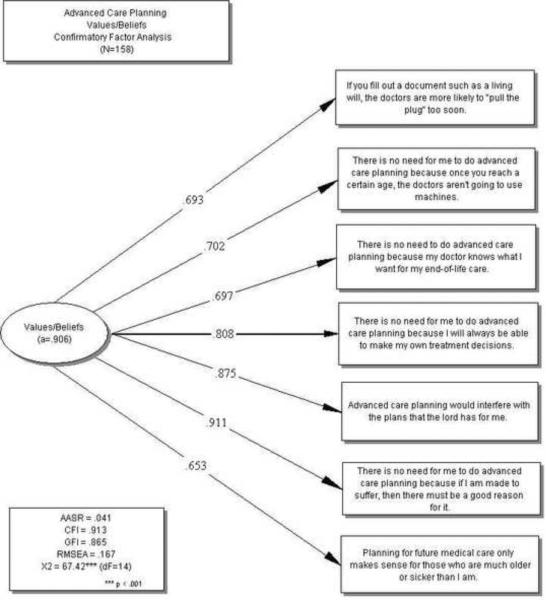
The final items identified in the exploratory analyses were included in confirmatory factor analyses using the second half of the split subsample. The fit for the Decisional Balance measure (Figure 1) was good to excellent, with CFI = .876, GFI = .863, and AASR = .054. The correlation between the two factors (Pros and Cons) in the confirmatory sample was r = −.69. For the ACP Values/Beliefs scale (Figure 2), CFI=.913, GFI = .865, and AASR = .041, also indicating good to excellent fit. Within the entire sample, the correlation between Pros and Cons was r = −.53, between Pros and ACP Values/Beliefs was r = −.51, and between Cons and ACP Values/Beliefs was r = .64.
Figure 1.
Confirmatory factor analysis for Decisional Balance scale. GFI = goodness of fit index; CFI = comparative fit index; 4) AASR = average absolute standardized residual statistic; 5) RMSEA =mean squared error of approximation.
Figure 2.
Confirmatory factor analysis for Values/Beliefs scale. GFI = goodness of fit index; CFI = comparative fit index; 4) AASR = average absolute standardized residual statistic; 5) RMSEA =mean squared error of approximation.
3.5. Processes of Change
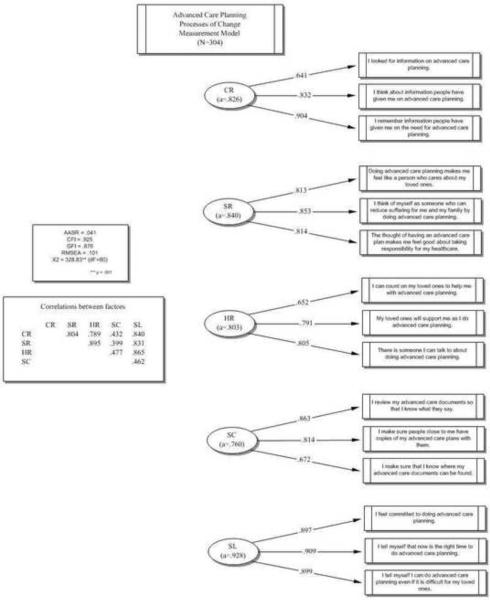
Seventeen items were included in the exploratory structural equation modeling analysis for this measure. Based on loadings and construct breadth, one or two items were eliminated for each Process, resulting in 3 items per scale. Two models were tested: 1) null model (suggesting no latent factors and used as a comparative model) and 2) five correlated factor model. The five-factor correlated model (Figure 3) demonstrated the best fit to the data, χ2(80) =328.83, p < .001; CFI=.925, GFI= .876 and AASR=.041. The internal consistencies were good, with Cronbach's alphas ranging from .76 to .93. Correlations between the scales ranged from .43 to .89 and are shown in Figure 3.
Figure 3.
Measurement model for Processes of Change scale. GFI = goodness of fit index; CFI = comparative fit index; 4) AASR = average absolute standardized residual statistic; 5) RMSEA =mean squared error of approximation.
3.6. External Validation
The results of the MANOVA examining scores on the Pros, Cons, ACP Values/Beliefs, and POC subscales by stage of change for the six behaviors were significant, Wilks' λ= .555–.809, η2=.068–.178, p ≤ .001 for all models (Table 2). The Pros, Cons, and Values/Beliefs scales were significantly associated with stages of change for all of the behaviors. Each of the POC subscales was significantly associated with stages of change for completing a healthcare proxy and living will. Only Self Reevaluation and Helping Relationships were significantly associated with stages of change for talking to loved ones regarding life-sustaining treatment. Self Reevaluation was the only POC associated with talking to loved ones regarding quality vs. quantity of life, and Consciousness Raising was the only POC associated with talking to clinicians regarding life-sustaining treatment.
Table 2.
Stage of Change MANOVA Results for Six ACP Behaviors
| ACP Staging | Stage of Change | Multivariate | Follow-Up ANOVA's | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | η 2* | |||||||||||||
| PC | C | PR | A/M | Wilk's λ* | η 2* | Pros | Cons | V/B | CR | SR | HR | SC | SL | |
| Healthcare proxy | 77 | 53 | 20 | 94 | .619 | .148 | .136 | .177 | .100 | .038 | .076 | .051 | .079 | .088 |
| Living will | 50 | 46 | 11 | 139 | .555 | .178 | .073 | .167 | .076 | .069 | .107 | .085 | .108 | .123 |
| Talking to loved ones- life sustaining treatment | 57 | 22 | 8 | 159 | .776 | .081 | .072 | .153 | .085 | -- | .042 | .041 | -- | -- |
| Talking to loved ones- quality vs. quantity | 80 | 27 | 5 | 133 | .774 | .082 | .092 | .129 | .119 | -- | .054 | -- | -- | -- |
| Talking to MD- life sustaining treatment | 167 | 43 | 9 | 25 | .809 | .068 | .075 | .100 | .057 | .035 | -- | -- | -- | -- |
| Talking to MD- quality vs. quantity | 174 | 49 | 4 | 14 | .799 | .072 | .058 | .119 | .068 | -- | -- | -- | -- | -- |
All reported values significant at p < .05
indicates p ≥ .05
MANOVA = Multivariate analysis of variance; ACP = Advance Care Planning; PC = Pre-Contemplation; C = Contemplation; PR = Preparation; A/M = Action/Maintenance; V/B = Values/Beliefs; CR = Consciousness Raising; SL = Self Liberation; SR = Self Re-evaluation; HR = Helping Relationships; SC = Stimulus Control
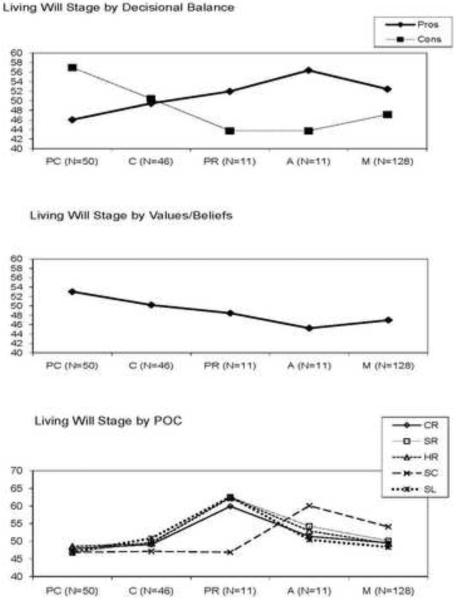
Figure 4 shows the relationships between scale scores and stages of change for completing a living will. The Pros increased by approximately one SD across the stages of Precontemplation (PC) to Action (A), the Cons decreased by > 1 SD, and the ACP Values/Beliefs decreased by approximately 0.9 SD.
Figure 4.
Decisional balance, Values/Beliefs, and Processes of Change scores according to Stage of Change for completing a Living Will. PC = Precontemplation; C = Contemplation; PR = Preparation; A = Action; M = Maintenance.
4. Discussion and Conclusion
4.1. Discussion
Scales measuring the Pros and Cons of ACP, ACP Values/Beliefs, and Processes of Change were developed based on literature review, qualitative research and psychometric analyses, demonstrating both high reliability and validity. Consistent with the hypotheses of the TTM, participants' scores on these scales varied significantly by stage of change, with scores accounting for between about 7% to 18% of the variance for a broad range of ACP behaviors.
Although several studies have previously discussed ACP in terms of health behavior change(48, 49) and have developed measures for stages of change,(50) only two other studies have sought to develop measures for the remaining TTM constructs. Each of these studies conceptualized ACP as a single health behavior of completing advance directive documents.(51, 52) The former study demonstrated high internal reliability for the scales, but it did not examine their validity.(51) The latter focused on decisional balance alone, demonstrating lower internal consistency, but high construct validity.(52)
Because of the growing consensus that ACP ideally consists of a wider group of behaviors, including values clarification and communication with clinicians and surrogates, the current study attempted to identify attitudes and processes that are applicable to all of these behaviors. In addition, the current study created a measure to capture religious beliefs and medical misconceptions that may serve as a barrier to participation in ACP. Misperceptions have also been associated with stages of change for blood donation,(53) supporting the importance of this construct for understanding change in certain complex health behaviors. It is encouraging that many of the measures were associated with stage of change across all of the ACP behaviors, given the results of prior work demonstrating a lack of correlation among the stages for different behaviors.(47) The POC subscales performed less well across the various ACP behaviors, suggesting that processes of change may need to be conceptualized more specifically for a given ACP behavior rather than applicable across behaviors.
The experience with developing measures in this study highlights some additional challenges of applying the TTM to ACP with an older population. Despite including a screen for more severe cognitive impairment, participants had difficulty understanding the usual response format used for the Decisional Balance, which asks participants to rate how important each item is to their decision to participate in ACP. The simplified format used in this study, asking participants how strongly they agreed with each of the items, in combination with the repetition of ACP within each item, may each have been partially responsible for the relatively high correlation between pros and cons. This level of correlation is not typically seen in Decisional Balance scales. It suggests that participants view the pros and cons subscales as if they were two sides of the same coin, rather than two distinct concepts, although the PCAs clearly supported the existence of two separate factors. We had difficulty developing items for several of the Processes of Change subscales, and, because of respondent burden, we elected not to develop a Self-Efficacy measure, which is an additional important TTM construct. The application of the TTM to ACP will need to proceed in an iterative process, with continuing efforts to refine and develop measures that best capture the constructs of the model.
The study's major limitations have been alluded to in the earlier sections of the Discussion. The difficulty participants had with the questions may reflect the failure to include a test of executive function as an exclusion criterion. However, the lack of such a criterion allowed for the development of scales that can be used with a broader range of older persons. The lack of longitudinal data precludes the ability to infer cause-and-effect relationships from these results. Although splitting the sample allowed for exploratory and confirmatory testing in separate groups of participants for the Decisional Balance and ACP Values/Beliefs scales, these participants did come from the same study cohort. For all the scales, and especially for the POC scale, where we were not able to use split-half analyses, these results would be strengthened by confirmatory testing in independent samples.
4.2. Conclusion
The cross-sectional associations between the scales developed in this study and stages of change for multiple components of ACP support the hypothesis that changes in individuals' perceptions of the pros and cons of participation in ACP and use of certain experiential and cognitive processes can increase their readiness for participation. The magnitude of change in the Pros subscale by one SD from Precontemplation to Action for living will completion is consistent with findings across 48 different health behaviors.(26). The magnitude of change in the Cons subscale of > 1 SD is higher than has been found in other studies.(26) The ACP Values/Beliefs scale was also associated with stage of change, however, these values and beliefs are, by their very nature, difficult to modify. A challenge for intervention is how to respond to the ACP values in a manner that is both sensitive and efficacious.
4.3. Practice Implications
The development of scales to measure the constructs of ACP as a health behavior lay the groundwork for TTM-tailored interventions to promote participation in ACP. These interventions are based on expert systems, in which a series of tailoring algorithms are specified to create intervention materials providing feedback only on the subset of scale items that are most important to behavior change at each stage. In addition, when administered in the clinical setting, the scales provide the opportunity for clinicians to gain a more detailed understanding of key factors related to their patients' readiness to participate. Assessment of readiness for participation is a critical first step in the process by which clinicians in primary care and other outpatient settings can guide their patients through the elements of ACP.(54) Clinicians can use patients' responses to the scale items as the basis for individualized discussions and counseling to address barriers to and facilitators of patients' engagement in ACP.
Acknowledgments
This work was supported by the National Institute of Aging at the National Institutes of Health (R01 AG19769, K24 AG28443, P30AG21342.)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gillick MR. Advance care planning. N Engl J Med. 2004;350:7–8. doi: 10.1056/NEJMp038202. [DOI] [PubMed] [Google Scholar]
- 2.Morrison RS, Olson E, Mertz KR, Meier DE. The inaccessibility of advance directives on transfer from ambulatory to acute care settings. JAMA. 1995;274:478–82. [PubMed] [Google Scholar]
- 3.Teno JM, Licks S, Lynn J, Wenger N, Connors AF, Jr., Phillips RS, O'Connor MA, Murphy DP, Fulkerson WJ, Desbiens N, Knaus WA. Do advance directives provide instructions that direct care? Support investigators. Study to understand prognoses and preferences for outcomes and risks of treatment. J Am Geriatr Soc. 1997;45:508–12. doi: 10.1111/j.1532-5415.1997.tb05179.x. [DOI] [PubMed] [Google Scholar]
- 4.Fagerlin A, Schneider CE. Enough. The failure of the living will. Hastings Cent Rep. 2004;34:30–42. [PubMed] [Google Scholar]
- 5.Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: A systematic review. Arch Intern Med. 2006;166:493–7. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 6.Fried TR, Bradley EH, Towle VR. Valuing the outcomes of treatment: Do patients and their caregivers agree? Arch Intern Med. 2003;163:2073–8. doi: 10.1001/archinte.163.17.2073. [DOI] [PubMed] [Google Scholar]
- 7.Hardin SB, Yusufaly YA. Difficult end-of-life treatment decisions: Do other factors trump advance directives? Arch Intern Med. 2004;164:1531–33. doi: 10.1001/archinte.164.14.1531. [DOI] [PubMed] [Google Scholar]
- 8.Dresser R. Precommitment: A misguided strategy for securing death with dignity. Tex Law Rev. 2003;81:1823–47. [PubMed] [Google Scholar]
- 9.Halpern J, Arnold RM. Affective forecasting: An unrecognized challenge in making serious health decisions. J Gen Intern Med. 2008;23:1708–12. doi: 10.1007/s11606-008-0719-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lo B, Steinbrook R. Resuscitating advance directives. Arch Intern Med. 2004;164:1501–06. doi: 10.1001/archinte.164.14.1501. [DOI] [PubMed] [Google Scholar]
- 11.Perkins HS. Controlling death: The false promise of advance directives. Ann Intern Med. 2007;147:51–57. doi: 10.7326/0003-4819-147-1-200707030-00008. [DOI] [PubMed] [Google Scholar]
- 12.Winzelberg GS, Hanson LC, Tulsky JA. Beyond autonomy: Diversifying end-of-life decision-making approaches to serve patients and families. J Am Geriatr Soc. 2005;53:1046–50. doi: 10.1111/j.1532-5415.2005.53317.x. [DOI] [PubMed] [Google Scholar]
- 13.Gillick MR. A broader role for advance medical planning. Ann Intern Med. 1995;123:621–4. doi: 10.7326/0003-4819-123-8-199510150-00009. [DOI] [PubMed] [Google Scholar]
- 14.Kolarik RC, Arnold RM, Fischer GS, Tulsky JA. Objectives for advance care planning. J Pall Med. 2002;5:697–704. doi: 10.1089/109662102320880516. [DOI] [PubMed] [Google Scholar]
- 15.Hammes BJ. What does it take to help adults successfully plan for future medical decisions? J Palliat Med. 2001;4:453–6. doi: 10.1089/109662101753381584. [DOI] [PubMed] [Google Scholar]
- 16.Briggs L. Shifting the focus of advance care planning: Using an in-depth interview to build and strengthen relationships. J Palliat Med. 2004;7:341–49. doi: 10.1089/109662104773709503. [DOI] [PubMed] [Google Scholar]
- 17.Ramsaroop SD, Reid MC, Adelman RD. Completing an advance directive in the primary care setting: What do we need for success? J Am Geriatr Soc. 2007;55:277–83. doi: 10.1111/j.1532-5415.2007.01065.x. [DOI] [PubMed] [Google Scholar]
- 18.Bravo G, Dubois M-F, Wagneur B. Assessing the effectiveness of interventions to promote advance directives among older adults: A systematic review and multi-level analysis. Soc Sci Med. 2008;67:1122. doi: 10.1016/j.socscimed.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 19.Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Rimer BK, Viswanath KV, editors. Health behavior and health education: Theory, research, and practice. 4th edition Jossey-Bass; San Francisco: 2008. pp. 170–222. [Google Scholar]
- 20.Weinstock MA, Rossi JS, Redding CA, Maddock JE. Randomized controlled community trial of the efficacy of a multicomponent stage-matched intervention to increase sun protection among beachgoers. Prev Med. 2002;35:584–92. doi: 10.1006/pmed.2002.1114. [DOI] [PubMed] [Google Scholar]
- 21.Jones H, Edwards L, Vallis TM, Ruggiero L, Rossi SR, Rossi JS, Greene G, Prochaska JO, Zinman B, Diabetes Stages of Change S Changes in diabetes self-care behaviors make a difference in glycemic control: The diabetes stages of change (disc) study. Diabetes Care. 2003;26:732–7. doi: 10.2337/diacare.26.3.732. [DOI] [PubMed] [Google Scholar]
- 22.Johnson SS, Paiva AL, Cummins CO, Johnson JL, Dyment SJ, Wright JA, Prochaska JO, Prochaska JM, Sherman K. Transtheoretical model-based multiple behavior intervention for weight management: Effectiveness on a population basis. Prev Med. 2008;46:238–46. doi: 10.1016/j.ypmed.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greene GW, Fey-Yensan N, Padula C, Rossi SR, Rossi JS, Clark PG. Change in fruit and vegetable intake over 24 months in older adults: Results of the senior project intervention. Gerontologist. 2008;48:378–87. doi: 10.1093/geront/48.3.378. [DOI] [PubMed] [Google Scholar]
- 24.Levesque DA, Cummins CO, Prochaska JM, Prochaska JO. Stage of change for making an informed decision about medicare health plans. Health Serv Res. 2006;41:1372–91. doi: 10.1111/j.1475-6773.2006.00547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fried TR, Tinetti ME, Iannone L. Primary care clinicians' experiences with treatment decision making for older persons with multiple conditions. Arch Intern Med. 2010;171:75–80. doi: 10.1001/archinternmed.2010.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hall KL, Rossi JS. Meta-analytic examination of the strong and weak principles across 48 health behaviors. Prev Med. 2008;46:266–74. doi: 10.1016/j.ypmed.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 27.Prochaska JO, Velicer WF, DiClemente CC, Fava J. Measuring processes of change: Applications to the cessation of smoking. J Consult Clin Psychol. 1988;56:520–8. doi: 10.1037//0022-006x.56.4.520. [DOI] [PubMed] [Google Scholar]
- 28.Redding CA, Maddock JE, Rossi JS. The sequential approach to measurement of health behavior constructs: Issues in selecting and developing measures. Cal J Health Prom. 2006;4:83–101. [Google Scholar]
- 29.Perkins HS, Geppert CMA, Gonzales A, Cortez JD, Hazuda HP. Cross-cultural similarities and differences in attitudes about advance care planning. J Gen Intern Med. 2002;17:48–57. doi: 10.1046/j.1525-1497.2002.01032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shrank WH, Kutner JS, Richardson T, Mularski RA, Fischer S, Kagawa-Singer M. Focus group findings about the influence of culture on communication preferences in end-of-life care. J Gen Intern Med. 2005;20:703–09. doi: 10.1111/j.1525-1497.2005.0151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Porensky EK, Carpenter BD. Knowledge and perceptions in advance care planning. J Aging Health. 2008;20:89–106. doi: 10.1177/0898264307309963. [DOI] [PubMed] [Google Scholar]
- 32.Seymour J, Gott M, Bellamy G, Ahmedzai SH, Clark D. Planning for the end of life: The views of older people about advance care statements. Soc Sci Med. 2004;59:57–68. doi: 10.1016/j.socscimed.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 33.Bullock K. Promoting advance directives among african americans: A faith-based model. J Palliat Med. 2006;9:183–95. doi: 10.1089/jpm.2006.9.183. [DOI] [PubMed] [Google Scholar]
- 34.Johnson KS, Kuchibhatla M, Tulsky JA. What explains racial differences in the use of advance directives and attitudes toward hospice care? J Am Geriatr Soc. 2008;56:1953–58. doi: 10.1111/j.1532-5415.2008.01919.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carr D, Khodyakov D. End-of-life health care planning among young-old adults: An assessment of psychosocial influences. J Gerontol B Psychol Sci Soc Sci. 2007;62:S135–41. doi: 10.1093/geronb/62.2.s135. [DOI] [PubMed] [Google Scholar]
- 36.Morrison RS, Meier DE. High rates of advance care planning in new york city's elderly population. Arch Intern Med. 2004;164:2421–26. doi: 10.1001/archinte.164.22.2421. [DOI] [PubMed] [Google Scholar]
- 37.Schickedanz AD, Schillinger D, Landefeld CS, Knight SJ, Williams BA, Sudore RL. A clinical framework for improving the advance care planning process: Start with patients' self-identified barriers. J Am Geriatr Soc. 2009;57:31–39. doi: 10.1111/j.1532-5415.2008.02093.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carrese JA, Mullaney JL, Faden RR, Finucane TE. Planning for death but not serious future illness: Qualitative study of housebound elderly patients. BMJ. 2002;325:125. doi: 10.1136/bmj.325.7356.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rodriguez KL, Young AJ. Elderly veterans' beliefs concerning life-sustaining treatment and the control of their end-of-life health and health care. J Aging Health. 2006;18:686–706. doi: 10.1177/0898264306293258. [DOI] [PubMed] [Google Scholar]
- 40.Freer JP, Eubanks M, Parker B, Hershey CO. Advance directives: Ambulatory patients' knowledge and perspectives. Am J Med. 2006;119:1088, e9. doi: 10.1016/j.amjmed.2006.02.028. [DOI] [PubMed] [Google Scholar]
- 41.Fried TR, Bullock K, Iannone L, O'Leary JR. Understanding advance care planning as a process of health behavior change. J Am Geriatr Soc. 2009;57:1547–55. doi: 10.1111/j.1532-5415.2009.02396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–56. [PubMed] [Google Scholar]
- 43.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 44.Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 45.Velicer WF. Determining the number of components from the matrix of partial correlations. Psychometrika. 1976;41:321–27. [Google Scholar]
- 46.Horn JL. A rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30:179–85. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- 47.Fried TR, Redding C, Robbins R, Paiva A, O'Leary JR, Iannone L. Stages of change for the component behaviors of advance care planning. J Am Geriatr Soc. 2010 doi: 10.1111/j.1532-5415.2010.03184.x. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pearlman RA, Cole WG, Patrick DL, Starks HE, Cain KC. Advance care planning: Eliciting patient preferences for life-sustaining treatment. Patient Educ Couns. 1995;26:353–61. doi: 10.1016/0738-3991(95)00739-m. [DOI] [PubMed] [Google Scholar]
- 49.Sudore RL, Schickedanz AD, Landefeld CS, Williams BA, Lindquist K, Pantilat SZ, Schillinger D. Engagement in multiple steps of the advance care planning process: A descriptive study of diverse older adults. J Am Geriatr Soc. 2008;56:1006–13. doi: 10.1111/j.1532-5415.2008.01701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Foti ME, Hanrahan-Boshes M. [Accessed at: on September 3, 2009];Reap: Readiness to engage in advance care planning. [Google Scholar]
- 51.Jezewski MA, Finnell DS, Wu YW, Meeker MA, Sessanna L, Lee J. Psychometric testing of four transtheoretical model questionnaires for the behavior, completing health care proxies. Res Nurs Health. 2009;32:606–20. doi: 10.1002/nur.20352. [DOI] [PubMed] [Google Scholar]
- 52.Medvene LJ, Base M, Patrick R, Wescott J. Advance directives: Assessing stage of change and decisional balance in a community-based educational program. Journal of Applied Social Psychology. 2007;37:2298–318. [Google Scholar]
- 53.Burditt C, Robbins ML, Paiva AL, Koblin B, Kessler D, Creeden C. Development of a blood donation myths scale in an african american sample. Ann Behav Med. 2009;37:S126. [Google Scholar]
- 54.Sudore RL, Fried TR. Redefining the “planning” in advance care planning: Preparing for end-of-life decision making. Ann Intern Med. 2010;153:256–61. doi: 10.1059/0003-4819-153-4-201008170-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]