Abstract
Individuals who abuse drugs show higher delay discounting (DD) rate and impulsiveness scores compared to controls; however, it is unclear if DD rate covaries with severity of the addiction, or if an individual’s discounting rate can be changed by effective substance abuse treatment. This study compared methadone maintenance patients (MMT; n=30), who had not used illegal drugs for two years, to drug-using MMT patients (n=30), and controls (n=25) in terms of addiction severity, DD rate and impulsiveness. Methadone patients abstinent from illegal drugs scored significantly lower on a number of addiction severity measures than the drug-using methadone patients. In addition, both groups of MMT patients showed significantly higher rates of DD and impulsiveness than the control group; however, no differences in DD rate or impulsiveness were found between the groups of patients. Results suggest that DD rate and impulsiveness may not covary with indicators of addiction severity in MMT patients.
Keywords: delay-discounting, impulsiveness, addiction severity, opioids, methadone, maintenance
1. Introduction
Individuals with substance abuse disorders often seem to behave impulsively, choosing small immediate rewards associated with drug use over ostensibly larger but delayed rewards such as good health, freedom from incarceration, and good family relations. Delay-discounting (DD) refers to the loss of subjective value of a reward as a function of delay to the reward. In general, studies on DD have shown that given an objectively defined reward (such as money), as delay to the reward increases, the subjective value of the reward decreases (Rachlin and Green, 1972). This appears to be true for the general population and in addition, a growing number of studies have revealed that substance abusers consistently exhibit higher delay discounting rates than non-abusing controls (e.g., Bickel et al., 2006; Kirby et al,. 1999; Madden et al., 1997; Odum and Bauman, 2010; Petry and Cassarella, 1999; Reynolds et al., 2004; Richards et al., 1999; Vuchinich and Simpson, 1998). In light of these findings, it has been suggested that a better understanding of delay discounting rate may have important implications for the prevention and treatment of substance abuse.
Studies on discounting by delay originated in the field of operant intertemporal choice (Ainslie, 1974; 1975; Mazur, 1987; Rachlin and Green, 1972). Mazur (1987) found that when pigeons are given a choice between smaller amounts of food delivered immediately, and a larger amount of food delivered after some delay, their choices are best described by the following hyperbolic model:
| (1) |
where vd is the current subjective value of a delayed reward (the indifference point), V is the nominal value of the delayed reward, d is the delay duration, and k is an empirically derived constant proportional to the degree of DD. Thus, the higher the value of k, the more rapidly the subjective value of a reward decays as a function of time to its delivery.
In 1991, Rachlin, Rainieri and Cross demonstrated hyperbolic discounting of hypothetical cash rewards in humans. In that study, volunteers were asked to choose between a constant amount of cash ($1,000) to be delivered after some delay (e.g., 1 month), and cash amounts ($1 to $1,000) to be delivered immediately. The subjective value of the delayed amount was defined as the indifference point (vd), or the point at which an individual switches from choosing a smaller immediate amount to a larger delayed amount. By repeating the choice procedure over a range of delay intervals, Rachlin obtained discounting functions that are best described by hyperbolic models (Killeen, 2009; Mazur, 1987; McKerchar et al., 2008). Importantly, similar discounting functions have been obtained when real or hypothetical rewards are used (Johnson and Bickel, 2002; Madden et al., 2003). Estimation of DD rate has now been extended to various populations of substance users and, to date, there is overwhelming evidence that users of tobacco, alcohol, opioids, cocaine, and methamphetamine discount by delay significantly more than matched non-using controls (for comprehensive reviews see Bickel et al., 2006, Green and Myerson, 2004, Reynolds, 2006, and Yi et al., 2010).
1.1 Delay discounting and severity of the drug problem
In addition to the observed differences in DD rate between drug users and non users, a number of studies have found that the magnitude of discounting as a function of delay covaries with severity of the substance abuse problem. For example, in two studies, Vuchinich and Simpson (1998) compared light social drinkers with problem drinkers, and with heavy social drinkers, and found higher rates of delay-discounting in heavy social drinkers and problem drinkers than in light social drinkers. Bretteville-Jensen (1999) compared active injecting amphetamine and/or heroin abusers with past abusers of amphetamine and/or heroin and non using controls, and found that both, active and past abusers discounted the value of delayed monetary rewards more than the controls; in addition, their group of active abusers discounted delayed rewards more than past abusers. Petry (2001) compared active alcoholics with abstinent alcoholics and with control subjects without a history of alcohol dependence on their rate of discounting of money ($1000 and $100), and alcohol (150 and 15 bottles of an alcoholic beverage) as a function of delay. Petry’s study showed that the two groups of alcoholics discounted money at higher rates than the control group. In addition, with exception of the $1000 condition, active alcoholics discounted at a higher rate than the alcohol-abstinent group. In other words, in three out of four comparisons, the most rapid discounting was observed in active, followed by abstinent alcoholics, followed by controls. Then, in a study comparing DD rate between controls and samples of drug users, Kirby and Petry (2004) found that DD rates were increasingly higher for controls, abstinent heroin users, and active heroin users. Bickel, Odum, and Madden (1999) compared delay discounting of hypothetical monetary outcomes by current, never, and ex-smokers of cigarettes. They found that current smokers discounted the value of delayed money more than did both comparison groups, and that never-and ex-smokers did not differ in their discounting of money. Taken together, these cross-sectional studies suggest that DD rate and drug use may be related in one of three ways. DD rate may either a) change as a function of severity of the substance use, increasing when the drug abuse problems are more severe and decreasing as a consequence of abstinence, b) be a preexisting condition predicting the likelihood of drug use and/or recovery from drug use, or c) result from an interaction of both processes. In addition, it is possible that both, substance use and DD might be predicted by a third variable such as IQ (Black and Rosen, 2011; de Wit, 2009; Perry and Carroll, 2008; Robles, 2010).
In support of the second proposition (b), some prospective studies have shown that preexisting differences in delay discounting rate may play a defining role in recovery from substance use. For example, Tucker and collaborators (Tucker et al., 2002; Tucker et al., 2006; Tucker et al., 2009) using the Alcohol-Savings Discretionary Expenditure (ASDE) index found that allocation of monetary expenditures to either alcoholic beverages or savings -which presumably reflects relative preference for immediate vs. delayed rewards- predicted abstinence from alcohol in nontreated problem drinkers at the 2-year follow-up. In addition, data pooled from three studies using the ASDE index revealed that the index incrementally predicted future rates of abstinence from alcohol in recently resolved treated and nontreated problem drinkers (Tucker et al., 2009). Regarding smokers, a number of studies show that preexisting DD rate can predict abstinence following cessation treatment. Krishnan-Sarin and collaborators (2007) found that scores on the experiential delay discounting test (EDT, Reynolds and Schiffbauer, 2004) predicted abstinence from smoking in adolescents who participated in a cessation program, although scores on Kirby’s delay discounting measure (Kirby et al., 1999) did not. Recently, MacKillop and Kahler (2009) found that, among treatment seeking smokers (who were also heavy drinkers), delay discounting rate predicted the number of days to first relapse to cigarette smoking after cessation treatment, independently of degree of nicotine dependence. Similarly, Yoon and collaborators (2007) found that the individual rate of DD predicted postpartum relapse to cigarette smoking among women who had discontinued smoking during pregnancy. Importantly, the study also showed that DD rate did not change over time regardless of their smoking status at 24 weeks postpartum. Finally, a prospective longitudinal study was recently published on the relationship between baseline DD rate and the probability of taking up smoking among a large cohort of volunteers followed from 15 to 21 years of age. In that study, Audrain-McGovern and collaborators (2009) found that degree of DD was relatively stable when measured repeatedly over 3 years; that higher DD rate at baseline predicted a heightened probability to take up smoking; and that having taken up smoking did not affect DD rate. To our knowledge, theirs is the first prospective study clearly showing DD rate acting as a stable preexisting variable predicting initiation of substance use, rather than changing as a consequence of it.
On the other hand, some studies have found no differences in DD rate associated with abstinence. For example, a recent a study that measured discounting rate for marijuana and hypothetical cash in self-reported current marijuana dependents, former marijuana dependents, and controls found no significant differences in DD rate between the groups (Johnson et al., 2010). Also, Kirby and Petry (2004) compared groups of self-reported 14-day abstinent and current users, and found lower DD rate among abstinent opiate abusers compared with active users, but did not find differences between abstinent alcoholics and abstinent cocaine users compared to active alcohol and cocaine users. Then, Heil and collaborators (2006) compared DD rate among cocaine dependent patients who were either currently using or had maintained abstinence from cocaine for 30 consecutive days, as well as a group of non-using community controls. Their study showed no differences in discounting rate between cocaine using and cocaine abstinent subjects although, consistent with previous studies, both groups showed higher rates of DD than the group of community controls. Taken together, these studies (Kirby and Petry, 2004; Heil et al., 2006) show, as Heil points out, that abstinence of up to 30 days from cocaine may not have a sufficient effect on delay-discounting rate to be detectable, or that abstinence from cocaine or alcohol for up to 30 days may not be stable enough to be predicted by a higher preexisting DD rate.
1.2 Effects of cognitive skills on delay discounting
Impulsiveness can be defined as the tendency to act without proper regard for the long-term consequences of those acts. Properly pondering the long-range consequences of our behavior, however, requires adequate cognitive skills as well as an environment suitable to such decision making. It seems fair to assume, therefore, that the lack of cognitive skills and a favorable environment might lead to errors and impulsive choices. Supporting this view, some studies have found that IQ scores correlate negatively with DD rate (de Wit et al. 2007; Shamosh and Gray, 2008; Reynolds et al., 2009). A meta-analysis of 24 studies on the relation between IQ score and DD rate found a significant negative relation between these variables, independently of the tests used to measure IQ and DD (Shamosh and Gray, 2008). Moreover, a study by de Wit et al. (2007) with a large sample of healthy adults showed that both, DD rate and nonplanning impulsiveness, correlated negatively with IQ scores independently of the subjects’ socioeconomic status and educational attainment. In addition, it has been reported that deficits in working memory (Bechara and Martin, 2004) and concentration during assessment of DD (Hinson et al., 2003; Upton et al., 2009) increase estimates of DD rate. While IQ is a relatively stable measure, to the extent that lower DD rate might depend on a person’s ability to properly ponder future events, it may be possible for some individuals to acquire the skills to choose in less impulsive ways. Recent studies have shown that interventions to enhance memory skills (Bickel et al., 2011) and to improve money management skills (Black and Rosen, 2011) can decrease estimates of DD rate in stimulant abusers; in addition, Black and Rosen found the changes in DD to be associated with a greater likelihood of drug abstinence. Taken together, these studies suggest that cognitive skills, particularly those involved in planning and decision making may be important predictors of both delay discounting rate and drug use.
1.1 Purpose of the study
This study was conducted to assess the effects of prolonged and confirmed abstinence from illegal drugs on impulsiveness and delay discounting rate. The study compared rate of DD between methadone maintenance treatment (MMT) patients who had submitted urine samples free from illicit drugs during 24 or more consecutive months, MMT patients who continued to use illicit drugs, and a sample of non drug-using community controls matched on age, sex and race.
2. Materials and Methods
2.1 Participants
Sixty MMT patients attending a university-affiliated substance abuse treatment clinic participated in the study. Half of the patients (n=30) had continued to use illicit opioids and other drugs after at least 4 weeks of treatment. The remaining 30 MMT patients qualified for the study because according to the clinic’s random urine testing program, they had remained abstinent from drugs of abuse (opiates, cocaine, amphetamines, benzodiazepines, PCP, propoxyphene, barbiturates, and THC) continuously for the previous 24 months. Regular drug testing at the clinic was conducted through a computerized selection of patients at least once per month. All urinalyses were conducted by a certified commercial laboratory. For all clinical and research purposes, missing urine samples were considered drug-positive. In addition to the patients, 26 non drug-using volunteers were recruited and assigned to the control group. Qualifying candidates were men and women between 18 and 65 years old, without current diagnosis for mental illness (e.g., schizophrenia) that might affect their ability to respond to the assessments. Control subjects were recruited through advertisements posted at various locations in the community. Initial qualification for participation in the study was determined through a brief telephone interview and, in the case of consenting MMT patients, through evaluation of their urinalysis records. All participating volunteers signed a consent form approved by the institution’s review board. Study participants were compensated with $50 for completion of the assessments.
Demographic information for the study sample is presented in Table 1. The groups were similar in age, sex and racial composition. In the table, significant differences between the groups are identified in the last column by letters (a, b, and c) corresponding to drug using patients, drug abstinent patients, and controls. On average, control participants completed more years of education (15.3) than drug-using (12) and drug-abstinent (11) MMT patients. More control participants were employed full-time (95%) than in both groups of patients (33.3%). There were no unemployed control participants, while 60% and 67% of the drug-using and drug-abstinent patients, respectively, were unemployed at the time of the study. Monthly income differed significantly between the drug-using patients and the control participants only, with controls reporting a higher income. Significantly more patients in both MMT groups than control participants smoked cigarettes. Significantly more drug-using patients were on probation (17%) than abstinent patients (6%) or control participants (none). Both groups of MMT patients reported a higher number of life DWI arrests than control participants; and a significantly higher number of arrests (all kinds) during the previous year were reported by the drug-using patients than by either abstinent patients or controls.
Table 1.
Characteristics of the study sample
| Study Sample | Drug-Using Patientsa | Drug-Abstinent Patientsb | Controlsc | p ≤ .05* |
|---|---|---|---|---|
| N | 30 | 30 | 26 | |
| Age (SE) | 43.32 (1.43) | 46.63 (0.91) | 40.90 (1.65) | N/S |
| Male (%) | 53.33 | 56.67 | 40.00 | N/S |
| White (%) | 93.10 | 77.40 | 75.00 | N/S |
| Years of Education (SD) | 12.16 (0.31) | 11.2 (0.35) | 15.35 (0.51) | ac, bc |
| Full-Time Employed (%) | 33.33 | 33.33 | 95.00 | ac, bc |
| Unemployed (%) | 60.00 | 66.67 | 0.00 | ac, bc |
| Median Monthly Income (IQR) | $750 (150 –1410) | $1550 (711 – 2425) | 2000 (1400 – 2500) | |
| On Parole (%) | 3.33 | 0.00 | 0.00 | N/S |
| On Probation (%) | 16.67 | 6.67 | 0.00 | ab, ac |
| Life DWI Arrests (SD) | 1.43 (0.52) | 0.83 (0.19) | 0.05 (0.05) | ab, ac |
| All Past-Year Arrests (SD) | 0.66 (0.18) | 0.03 (0.03) | 0.00 | ab, ac |
| Cigarettes per Day (SD) | 18.93 (2.17) | 16.5 (2.37) | 1.4 (1.01) | ac, bc |
| Current Recreational Drug Use (%) | 53.33 | 0 | 0.00 | ab, ac |
| Past Alcohol Problems (%) | 56.67 | 50.00 | 0.00 | ac, bc |
Differences between groups are indicated by the letters a, b, and c in the last column, corresponding to group columns.
2.2 Assessments
In addition to a questionnaire designed to collect demographic information and history of drug use, assessments included a computerized delay-discounting task (Robles, 2001; Robles and Vargas 2007), Eysenck’s I7 Impulsiveness Inventory (Eysenck, 1993, Eysenck et al., 1985), the Shipley Living Scale (Zachary, 1991) intelligence test and, among methadone patients only, a self-administered computer-aided form of the Addiction Severity Index (ASI, McLellan et al., 1985). In addition, on the day the assessments were performed, all participants provided a urine sample collected at the study site that was tested for opiates, cocaine, benzodiazepines, amphetamines and THC. These samples underwent qualitative analysis by a certified commercial laboratory. Data collection for each subject was conducted during a single session lasting approximately 2 hours for patients, and 1 hour for participants in the control group. The session duration differed due to the extra time required to complete the ASI.
2.2.1
Eysenck’s I7 Impulsiveness Inventory is a 54-item (true/false) questionnaire composed of the impulsiveness, venturesomeness, and empathy subscales, with reliability of α = 0.77 (Eysenck et al., 1985).
2.2.2
The Shipley Institute of Living Scale is a brief self-administered instrument that yields IQ estimates strongly correlated with the WAIS-R (Zachary, 1991; Zachary et al., 1985). The test is composed of two scales: vocabulary and abstraction.
2.2.3
The Addiction Severity Index (ASI, McLellan et al., 1985) is an instrument that assesses the degree of severity of an individual’s substance abuse problem during the past month in seven relevant areas: medical, psychiatric, legal, and employment status, as well as drug use, alcohol use, and family/social relationships. Composite scores are derived from responses to items within each of these areas, and range from 0.00 to 1.00, with higher scores indicating more severe problems. A computer-assisted self-administered form of the ASI was used (Butler et al., 2001). The composite scores obtained with the self-administered form of the ASI correlate moderately to strongly with those obtained with the interview (0.47– 0.87), and both forms have similar reliability (Rosen et al., 2000).
2.2.4 Delay Discounting
A computerized abbreviated task (Robles and Vargas, 2008) was used to estimate individual rates of DD. The program showed a series of computer screens depicting two index cards, one for the immediate and one for the delayed reward. Placement of the cards on the screen was counterbalanced (left-right) across delay values. Participants chose between the two cards by clicking on the “Select” button within each card. Once a choice was made, a full screen marked the 2-second intertrial interval (ITI), and prevented multiple responses. After the ITI, the next choice was presented and the cycle continued until the end of the assessment. All choices were between hypothetical cash amounts. The magnitude of the delayed reward was $1,000, and the delay intervals tested were 6 h, 1 day, 1 week, 2 months, 6 months, 1 year, 5 years, and 25 years (after Madden et al., 1997). The values of immediate rewards (all US dollars) tested were 1000, 999, 995, 990, 960, 940, 920, 850, 800, 750, 700, 650, 600, 550, 500, 450, 400, 350, 300, 250, 200, 150, 100, 80, 60, 40, 20, 10, 5 and 1. In this task, the immediate rewards were presented in descending order and once a subject showed indifference (i.e., switched from choosing the immediate to the delayed amount), the rest of the trials in the delay series were omitted. The complete DD procedure took approximately 20 minutes. Before the assessment, the experimenter showed each participant how to use the computer mouse; all but one were already familiar with it. Then, participants were given the following instructions:
“This program will show you a series of screens where you will be asked to choose between an amount of money available now, and $1,000 available after some delay. The amount of money available now and the delay between now and the time when you could receive the $ 1,000 will vary from screen to screen. Although the money described in this program is hypothetical, “pretend money”, I need you to make the decisions as if you were really going to get the amounts you choose, and honestly select the alternative you prefer. I don’t expect you to choose one or the other; please don’t choose what you think I might want you to choose, but click on the alternative you really prefer. The program will automatically go on to the next screen, and it will tell you when you are done”.
2.3 Data Analysis
The data are summarized by either the mean and standard error (SE) or the median and interquartile range (IQR). Group comparisons of categorical data were made with the chi-square test. Due to non-normality of the data, comparison of other demographic characteristics, IQ scores, and urine test results were made with Kruskal-Wallis one-way ANOVA with a Bonferroni adjustment for post hoc comparisons. Comparisons of ASI scores were made with Mann-Whitney Rank Sum tests. Individual indifference points were obtained, and DD rates (k) were estimated by nonlinear regression using Mazur’s hyperbolic model (see Equation 1.). Due to non-normality of k, log transformed k values were used in the analyses. Trait impulsiveness between the groups was compared with ANOVA and Tukey’s HSD post hoc test.
3. Results
3.1 Delay-Discounting Rate
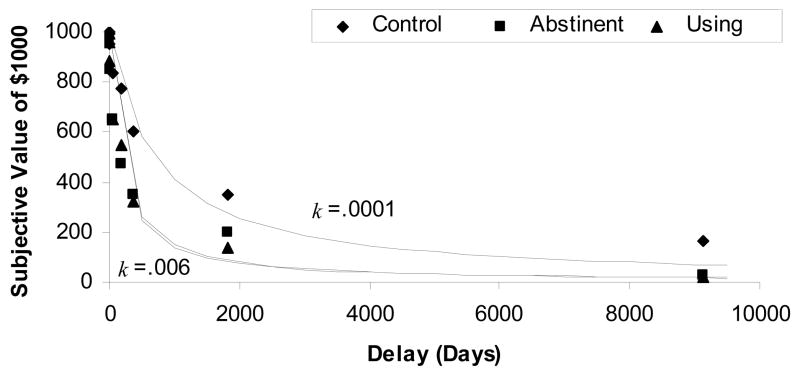
Congruent with previous reports, Mazur’s hyperbolic model described the data well, accounting for 96%, 98%, and 96% of the variance for MMT non users, MMT drug users, and the general population group, respectively (see Fig. 1). Using IQ, years of education, and income as covariates, significant differences in delay discounting rate (k) by group were detected (F(2, 83) = 20.63, p < .02). Post hoc comparisons (Tukey) revealed that the two groups of methadone maintenance patients (mean ln(k) = −4.97 and −5.13) discounted delayed money at significantly higher rates (p = 0.001) than the control group (mean ln(k) = −7.07), while no differences in rate of delay-discounting were found between the two groups of MMT patients.
Figure 1.
Rate of delay-discounting (k) for drug abstinent patients, drug-using patients, and the control group, respectively. Symbols represent group median delay discounting rates. Lines depict functions predicted by the hyperbolic model using the empirically derived k values.
3.2 Trait Impulsiveness
A one-way ANOVA of scores on Eysenck’s I7 Impulsiveness Inventory detected differences among the three groups (F(2, 83) = 10.4, p < 0.001). Post hoc analysis (Tukey) showed that both, the drug-abstinent (mean= 4.4) and drug-using (mean=5.36) groups of MMT patients scored higher on trait impulsiveness than the control group (mean=2.9; both comparisons p < 0.05), and that the two groups of patients did not differ on impulsiveness scores.
Based on a potential relationship revealed by the graphic distribution of scores, the relationship between impulsiveness and years of education was assessed. A Pearson’s Product Moment test showed a significant negative correlation (r = − 0. 24, p < .03) between subjects’ impulsiveness scores and years of education.
3.3 Intelligence
Analysis of variance on ranks of IQ scores obtained on the Shipley Living Scale revealed significant differences among the groups (H = 12.98, df = 2, p = 0.002). Post hoc comparisons showed significantly higher IQ scores among control participants [median IQ= 110 (104 –115)] compared to drug-using [median IQ= 103 (89 – 111)] and abstinent [median IQ= 96 (89 –106); p < 0.001] MMT patients; IQ scores for drug abstinent MMT patients were not significantly different from drug-using patients (p > .84).
3.4 Addiction Severity Index (ASI)
Composite scores for both groups of patients are shown in Table 2. In all domains, the drug-using patients attained equal or higher severity scores than the abstinent patients. Statistically significant differences between the two groups of MMT patients were observed on the legal (p = 0.03), psychiatric (p ≤ 02), drug use (p =.02), and alcohol use (p = .01) domains.
Table 2.
Median (IQR) ASI Composite Scores for MMT Patients
| Mann Whitney Comparison | |||
|---|---|---|---|
| Domain | Drug-Abstinent | Drug-Using | p |
| Medical Status | .528 (.178 – .833) | .531 (.188 – .808) | .70 |
| Employment Status | .500 (.163 – .500) | .500 (.243 – .748) | .38 |
| Alcohol Use | .192 (.000 – .280) | .238 (.168 – .405) | .01 |
| Drug Use | .169 (.124 – .322) | .278 (.192 – .367) | .02 |
| Legal Status | .000 (.000 –.113) | .150 (.000 – .210) | .03 |
| Family Status | .261 (.200 – .384) | .326 (.206 – .484) | .10 |
| Psychiatric Status | .114 (.450 –.347) | .379 (.131 – .521) | .02 |
3.5 Smoking
A multiple logistic regression analysis was performed with current smoking status (yes/no) as the outcome and DD rate [ln(k)], impulsiveness score, IQ, years of education, and income as predictors among all study participants. Only DD rate (Odds Ratio= 1.364, 95% CI = 1.038 – 1.791) and years of education (Odds Ratio = .741, 95% CI= .571 – .961) significantly (p < .05) contributed to the resulting model.
3.6 Urinalysis
All study participants submitted a urine sample immediately before completing the study assessments. As expected, all urinalysis tests for the control group were negative for all drugs, and all tests for patients in the drug-abstinent group were negative for illegal drugs. On the other hand, urine tests for drug using MMT patients were positive for cocaine (23%), THC (23%), non-prescribed opiates (10%), benzodiazepines (16%), and amphetamines (3%). None of the participants appeared intoxicated at the time of the assessments.
4. Discussion
Results from this study show that, controlling for IQ, years of education, and income, MMT patients who had been continuously abstinent from illicit drugs for at least 2 years did not differ in degree of delay discounting from a group of MMT patients who continued to use illicit drugs. In addition, consistent with previous reports, rates of delay discounting for the control group were lower than the rates observed among both groups of MMT patients. Parallel results were observed on impulsiveness scores; the two groups of MMT patients scored significantly higher than the control participants on trait impulsiveness, while no differences were observed between the two groups of MMT patients. These findings are important, considering that the two groups of methadone patients clearly differed in addiction severity as indicated by their ASI scores, the consistency of their urinalysis results and adherence to MMT procedures over 2 years, and the urinalysis results obtained during the study. In other words, significant drug abstinence and increased personal stability were not associated with lower impulsiveness scores or DD rates in our sample of MMT patients. Finally, consistent with previous reports, this study showed significant differences in IQ between the groups, with MMT patients scoring lower than controls.
Our findings differ from several reports showing covariation between DD rate and addiction severity in relation to smoking, alcohol, and cocaine. (e.g., Bickel et al., 1999; Bretteville-Jensen, 1999; Kirby and Petry, 2004; Petry, 2001; Tucker et al., 2009). However, the present findings are consistent with studies showing no relationship between DD rate and addiction severity among alcohol, tobacco, marijuana, and cocaine users (e.g., Bickel et al., 1999; Heil et al., 2006; Johnson et al., 2010; Kirby and Petry, 2004; Reynolds, 2004); with studies showing that elevated rates of delay discounting may precede drug use (e.g., Adrienne-McGovern et al., 2009; Krishnan-Sarin et al., 2007; MacKillop and Kahler; 2009; Tucker et al., 2002; Tucker et al., 2006; Tucker et al., 2009; Yoon et al., 2007), with studies showing that DD may be unaffected by drug use and abstinence (e.g., Audrain-McGovern et al., 2009; Heil et al., 2006); and with studies showing differences in DD rate between drug users and nonusing controls (e.g., Bickel et al., 2006; Kirby et al,. 1999; Madden et al., 1997; Odum and Bauman, 2010; Petry and Cassarella, 1999; Reynolds et al., 2004; Richards et al., 1999; Vuchinich and Simpson, 1998).
One viable hypothesis of how DD rate and drug use are functionally related proposes that DD rate changes as a consequence of drug use, increasing with more drug use and decreasing with drug abstinence. Our finding that addiction severity but not DD rate or impulsiveness differed between the groups of patients does not support that hypothesis, at least in MMT patients. Rather, it appears that neither discounting rate nor impulsiveness scores were modified by efficacious MMT in this study. An alternative hypothesis states that DD rate may be a preexisting condition acting as a risk factor for drug use and/or or predicting the likelihood of recovery from drugs. Because we found no differences in DD rate between groups of patients that clearly differed in addiction severity, our data suggest that among MMT patients the rate of DD (as a preexisting condition) may be a risk factor for drug use, but it is not always be a reliable predictor of recovery from drug use. It is also possible that DD rates among our sample of patients might have changed over the course of treatment; however, because no baseline measurement of DD rate was obtained in this study, that possibility cannot be directly assessed.
Compared to other populations in which degree of DD has been studied such as current and ex- users of tobacco and alcohol, there are potentially critical differences with MMT patients that could explain the discrepancy in results regarding addiction severity and DD rate. For example, in contrast with abstinent smokers and drinkers, who are not exposed to nicotine and alcohol, MMT patients remain chronically exposed to opioids. To date, it is not known if chronic exposure to opioids might have an increasing effect on DD rate.
In addition, compared to ex-smokers and abstinent drinkers, MMT patients may not require the same level of relapse prevention skills in order to remain abstinent. On the one hand, tobacco and alcohol are legally and readily available and, on the other, methadone dramatically reduces opioid craving and reward. In other words, it is possible that patients receiving efficacious drug treatment that does not involve prolonged substitution therapy may be forced to develop better self control skills than patients receiving substitution therapy in order to remain abstinent; in turn, having better self-control skills should result in lower estimates of DD rate.
Finally, it seems reasonable to think of higher IQ as a proxy for better cognitive functioning (e.g., memory, concentration) and skills (e.g., general quantitative ability, financial planning ability), both of which have been shown to affect DD rate. It is possible, then, that the differences in delay discounting and impulsiveness observed between patients and controls in this study may reflect the differences observed in IQ scores.
Previous research has shown that smokers discount at higher rates than nonsmokers. In addition, the literature suggests that a higher rate of delay discounting is a risk factor for smoking, and that taking up smoking or relapsing do not affect delay discounting rate. Because in our sample both groups of MMT patients smoked more than the control group, we conducted a multiple logistic regression analysis to determine the extent to which DD rate, impulsiveness, IQ, years of education and income might predict smoking status in our samples of patients and controls. Supporting previous findings, our analysis revealed that only two variables were significant predictors of smoking: DD rate (a risk factor) and number of years of education (a protecting factor).
In our sample as a whole, income was not correlated with IQ, years of education, DD rate, or impulsiveness scores. However, control participants reported higher income, more years of education, and lower rate of unemployment than both groups of patients. Our results leave open the possibility that a number of factors including lower IQ, lower educational attainment, low SES, and unemployment (all of which tend to covary), along with chronic exposure to opioids and other drug use may account for the differences in DD rate observed between the MMT patients and control volunteers.
While this and other cross-sectional studies shed light on our understanding of DD rate and its potential role in preventing and treating substance abuse problems, prospective studies and randomized controlled trials are still needed to unequivocally establish the nature of the relationships between delay discounting rate, addiction severity, cognitive skills, and effective substance abuse treatment.
Acknowledgments
This study was supported by a National Institute on Drug Abuse grant (1R03DA13692-01) to Elias Robles, and by a grant from the Arkansas Bureau of Alcoholism and Drug Abuse Prevention.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Elias Robles, Division of Social & Behavioral Sciences, Arizona State University, Glendale, Arizona.
B. Emma Huang, Commonwealth Scientific and Industrial Research Organisation, St. Lucia, Australia.
Pippa M. Simpson, Translational and Biomedical Center, Children’s Research Institute, 8701 Watertown Plank Road, Milwaukee, Wisconsin.
Donald E. McMillan, Department of Pharmacology, University of Arkansas for Medical Sciences, Little Rock, Arkansas.
References
- Ainslie G. Impulse control in pigeons. Journal of the Experimental Analysis of Behavior. 1974;21:485–489. doi: 10.1901/jeab.1974.21-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainslie G. Specious reward: a behavioral theory of impulsiveness and impulse control. Psychological Bulletin. 1975;82:463–494. doi: 10.1037/h0076860. [DOI] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Epstein LH, Cuevas J, Rodgers K, Wyleyto EP. Does delay discounting play an etiological role in smoking or is it a consequence of smoking? Drug and Alcohol Dependence. 2009;103:99–106. doi: 10.1016/j.drugalcdep.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechara A, Martin EM. Impaired decision making related to working memory deficits in individuals with substance addictions. Neuropsychology. 2004;18:152–162. doi: 10.1037/0894-4105.18.1.152. [DOI] [PubMed] [Google Scholar]
- Bickel W, Marsch L. Toward a behavioral economic understanding of drug dependence: delay discounting processes. Addiction. 2001;96:73–86. doi: 10.1046/j.1360-0443.2001.961736.x. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Kowal BP, Gatchalian KM. Understanding Addiction as a Pathology of Temporal Horizon. The Behavior Analyst Today. 2006;7:32–46. [Google Scholar]
- Bickel WK, Odum AL, Madden GJ. Impulsiveness and cigarette smoking: delay discounting in current, never, and ex-smokers. Psychopharmacology. 1999;146:447–454. doi: 10.1007/pl00005490. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Yi R, Landes RD, Hill PF, Baxter C. Remember the future: working memory training decreases delay discounting among stimulant addicts. Biological Psychiatry. 2011;69:260–265. doi: 10.1016/j.biopsych.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black MC, Rosen MI. A money management-based substance use treatment increases valuation of future rewards. Addictive Behaviors. 2011;36:125–128. doi: 10.1016/j.addbeh.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bretteville-Jensen AL. Addiction and discounting. Journal of Health Economics. 1999;18:393–407. doi: 10.1016/s0167-6296(98)00057-5. [DOI] [PubMed] [Google Scholar]
- Butler SF, Budman SH, Goldman RJ, Newman FL, Beckley KE, Trottier D, Cacciola JS. Initial validation of a computer-administered Addiction Severity Index: The ASI-MV. Psychology of Addictive Behaviors. 2001;15:4–12. doi: 10.1037/0893-164x.15.1.4. [DOI] [PubMed] [Google Scholar]
- de Wit H. Impulsivity as a determinant and consequence of drug use: A review of underlying processes. Addiction Biology. 2009;14:22–31. doi: 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit H, Flory JD, Acheson A, McCloskey M, Manuck SB. IQ and nonplanning impulsiveness are independently associated with delay discounting in middle-aged adults. Personality and Individual Differences. 2007;42:111–121. [Google Scholar]
- Eysenck HJ, Eysenck SBG. Eysenck Personality Inventory. San Diego, CA: Educational and Industrial Testing Srvice; 1968. [Google Scholar]
- Eysenck SBG. The I7: Development of a measure of impulsiveness and its relationship to the superfactors of personality. In: McCown WG, Johnson JL, Shure MB, editors. The impulsive client. Wasington, DC: American Psychological Association; 1993. pp. 141–149. [Google Scholar]
- Eysenck SB, Pearson PR, Easting G, Allsopp JF. Age norms for impulsiveness, venturesomeness and empathy in adults. Personality and Individual Differences. 1985;6:613–619. [Google Scholar]
- Giordano LA, Bickel WK, Loewenstein G, Jacobs EA, Marsch L, Badger GJ. Mild opioid deprivation increases the degree that opioid-dependent outpatients discount delayed heroin and money. Psychopharmacology. 2002;163:174–182. doi: 10.1007/s00213-002-1159-2. [DOI] [PubMed] [Google Scholar]
- Green L, Myerson J. A discounting framework for choice with delayed and probabilistic rewards. Psychological Bulletin. 2004;130:769–772. doi: 10.1037/0033-2909.130.5.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heil SHT, Johnson MW, Higgins ST, Bickel WK. Delay discounting in currently using and currently abstinent cocaine-dependent outpatients and non-drug-using matched controls. Addictive Behaviors. 2006;31:1290–1294. doi: 10.1016/j.addbeh.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Hinson JM, Jameson TL, Whitney P. Impulsive decision making and working memory. Journal of Experimental Psychology: Learning, Memory and Cognition. 2003;29:298–306. doi: 10.1037/0278-7393.29.2.298. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. Within-subject comparison of real and hypothetical money rewards in delay discounting. Journal of the Experimental Analysis of Behavior. 2002;77:129–146. doi: 10.1901/jeab.2002.77-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK, Baker F, Moore BA, Badger GJ, Budney AJ. Delay discounting in current and former marijuana-dependent individuals. Experimental and Clinical Psychopharmacology. 2010;18:99–107. doi: 10.1037/a0018333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killeen PR. An additive-utility model of delay discounting. Psychological Review. 2009;116:602–619. doi: 10.1037/a0016414. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM. Heroin and cocaine abusers have higher discount rates for delayed rewards than alcoholics or non-drug-using controls. Addiction. 2004;99:461–471. doi: 10.1111/j.1360-0443.2003.00669.x. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General. 1999;128(1):78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, Cavallo DA, Carroll KM, Potenza MN. Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug and Alcohol Dependence. 2007;88:79–82. doi: 10.1016/j.drugalcdep.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Kahler CW. Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug and Alcohol Dependence. 2009;104:197–203. doi: 10.1016/j.drugalcdep.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG. A behavioral economic measure of demand for alcohol predicts brief intervention outcomes. Drug and Alcohol Dependence. 2007;89:197–203. doi: 10.1016/j.drugalcdep.2007.01.002. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Begotka AM, Raiff BR, Kastern LL. Delay discounting of real and hypothetical rewards. Experimental and Clinical Psychopharmacology. 2003;11:139–145. doi: 10.1037/1064-1297.11.2.139. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Petry NM, Badger GJ, Bickel WK. Impulsive and self-control choices in opioid-dependent patients and non-drug-using control participants: drug and monetary rewards. Experimental and Clinical Psychopharmacology. 1997;5:256–262. doi: 10.1037//1064-1297.5.3.256. [DOI] [PubMed] [Google Scholar]
- Mazur JE. An adjusting procedure for studying delayed reinforcement. In: Commons ML, Mazur JE, Nevin JA, Rachlin H, editors. Quantitative Analysis of Behavior: Vol. 5. The effect of delay and of intervening events on reinforcement value. Hillsdale, NJ: Erlbaum; 1987. pp. 57–73. [Google Scholar]
- McKerchar TL, Green L, Myerson J, Pickford TS, Hill JC, Stout SC. A comparison of four models of delay discounting in humans. Behavioural Processes. 2008;81:256–259. doi: 10.1016/j.beproc.2008.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr HL. New data from the Adiction Severity Index: reliability and validity in three centers. Journal of Nervous and Mental Disorders. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- Odum AL, Bauman AAL. Delay discounting: State and trait variable. In: Madden GJ, Bickel WK, editors. Impulsivity: The behavioral and neurological science of discounting. Washington, DC: American Psychological Association; 2010. [Google Scholar]
- Petry NM, Cassarella T. Excessive discounting of delayed rewards in substance abusers with gambling problems. Drug and Alcohol Dependence. 1999;56:25–32. doi: 10.1016/s0376-8716(99)00010-1. [DOI] [PubMed] [Google Scholar]
- Perry JL, Carroll ME. The role of impulsive behavior in drug abuse. Psychopharmacology. 2008;200:1–26. doi: 10.1007/s00213-008-1173-0. [DOI] [PubMed] [Google Scholar]
- Rachlin H, Green L. Commitment, choice and self-control. Journal of the Experimental Analysis of Behavior. 1972;17:15–22. doi: 10.1901/jeab.1972.17-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachlin H, Rainieri A, Cross D. Subjective probability and delay. Journal of the Experimental Analysis of Behavior. 1991;55:233–244. doi: 10.1901/jeab.1991.55-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds B. A review of delay-discounting research with humans: Relations to drug use and gambling. Behavioral Pharmacology. 2006;17:651–667. doi: 10.1097/FBP.0b013e3280115f99. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Leraas K, Collins C, Melanko S. Delay discounting by the children of smokers and nonsmokers. Drug and Alcohol Dependence. 2009;99:350–353. doi: 10.1016/j.drugalcdep.2008.07.015. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Richards JB, Horn K, Karraker K. Delay discounting and probability discounting as related to cigarette smoking status in adults. Behavioural Processes. 2004;65:35–42. doi: 10.1016/s0376-6357(03)00109-8. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Schiffbauer R. Measuring state changes in human delay discounting: an experiential discounting task. Behavioural Processes. 2004;67:43–56. doi: 10.1016/j.beproc.2004.06.003. [DOI] [PubMed] [Google Scholar]
- Richards JB, Zhang L, Mitchell SH, De Witt H. Delay or probability discounting in a model of impulsive behavior: effect of alcohol. Journal of the Experimental Analysis of Behavior. 1999;71:121–143. doi: 10.1901/jeab.1999.71-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles E. Delay and loss of subjective value. Journal of Behavior, Health, and Social Issues. 2010;2:105–118. [Google Scholar]
- Robles E, Vargas PA. Parameters of delay discounting assessment tasks: Number of trials, effort, and sequential effects. Behavioural Processes. 2008;78:285–290. doi: 10.1016/j.beproc.2007.10.012. [DOI] [PubMed] [Google Scholar]
- Rosen CS, Henson BR, Finney JW, Moos RH. Consistency of self-administered and interview-based Addiction Severity Index composite scores. Addiction. 2000;95:419–425. doi: 10.1046/j.1360-0443.2000.95341912.x. [DOI] [PubMed] [Google Scholar]
- Shamosh NA, Gray JR. Delay discounting and intelligence: A meta-analysis. Intelligence. 2008;6:289–305. [Google Scholar]
- Tucker JA, Vuchinich RE, Rippens PD. Predicting natural resolution of alcohol-related problems: a prospective behavioral economic analysis. Experimental and Clinical Psychopharmacology. 2002;10:248–257. doi: 10.1037//1064-1297.10.3.248. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Vuchinich RE, Black BC, Rippens PD. Significance of a behavioral economic index of reward value in predicting drinking problem resolution. Journal of Consulting and Clinical Psychology. 2006;74:317–326. doi: 10.1037/0022-006X.74.2.317. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Roth DL, Vignolo MJ, Westfall AO. A behavioral economic reward index predicts drinking resolutions: moderation revisited and compared with other outcomes. Journal of Consulting and Clinical Psychology. 2009;77:219–228. doi: 10.1037/a0014968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upton J, Brackett E, Crone-Todd D, Lambert N. The effect of time constraints on the area under the curve using a delay discounting task. Presented at the 33rd Annual Conference of the Society for the Quantitave Analysis of Behavior; San Antonio, TX. May 27–29..2010. [Google Scholar]
- Vuchinich RE, Simpson CA. Hyperbolic temporal discounting in social drinkers and problem drinkers. Experimental and Clinical Psychopharmacology. 1998;6:292–305. doi: 10.1037//1064-1297.6.3.292. [DOI] [PubMed] [Google Scholar]
- Yi R, Mitchell SH, Bickel WK. Delay discounting and substance abuse. In: Madden GJ, Bickel WK, editors. Impulsivity: The behavioral and neurological science of discounting. Washington, DC: American Psychological Association; 2010. [Google Scholar]
- Yoon JH, Higgins ST, Heil SH, Sugarbaker RJ, Thomas CS, Badger GJ. Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Experimental and Clinical Psychopharmacology. 2007;15:176–186. doi: 10.1037/1064-1297.15.2.186. [DOI] [PubMed] [Google Scholar]
- Zachary RA. Shipley Institute of Living Scale: Revised Manual. Western Psychological Services; Los Angeles, CA: 1991. [Google Scholar]
- Zachary RA, Crumpton E, Spiegel DE. Estimating WAIS-R IQ from the Shipley Institute of Living Scale. Journal of Clinical Psychology. 1985;41:532–540. doi: 10.1002/1097-4679(198511)41:6<820::aid-jclp2270410616>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]