Abstract
Background
To provide protection against sexually transmitted infections (STIs) and pregnancy, condoms must be used consistently and correctly. However, a significant proportion of couples in the United States fail to do so. Our objective was to determine the demographic and behavioral correlates of inconsistent and incorrect condom use among sexually active, condom-using women.
Methods
Analysis of baseline data from a prospective cohort of sexually active, condom-using women in the Contraceptive CHOICE Project (n = 2,087) using self-reported demographic and behavioral characteristics. Poisson regression was used to determine the relative risk of inconsistent and incorrect condom use after adjusting for variables significant in the univariate analysis.
Results
Inconsistent and incorrect condom use was reported by 41% (n = 847) and 36% (n = 757) of women, respectively. A greater number of unprotected acts was most strongly associated with reporting 10 or more sex acts in the past 30 days, younger age at first intercourse, less perceived partner willingness to use condoms, and lower condom use self-efficacy. Incorrect condom use was associated with reporting 10 or more sex acts in the past 30 days, greater perceived risk for future STIs, and inconsistent condom use.
Conclusions
Inconsistent and incorrect condom use is common among sexually active women. Targeted educational efforts and prevention strategies should be implemented among women at highest risk for STIs and unintended pregnancies to increase consistent and correct condom use.
Keywords: Condom use, contraception, women, self-efficacy, sexual behavior
INTRODUCTION
Women and men use male condoms to prevent sexually transmitted infections (STIs), unintended pregnancies, or both; however, effective protection is achieved only if condoms are used consistently and correctly [1]. There are an estimated 19 million new STI cases in the United States each year [2], and approximately one million individuals are infected with human immunodeficiency virus (HIV) [3]. Condom use has been shown to be effective in preventing STIs and HIV [4]; however, inconsistent condom use increases exposures to STIs and is associated with higher odds of contracting an STI [5, 6].
The prevalence of unintended pregnancies among U.S. women is also alarmingly high. In 2001, 49% of pregnancies were unintended, 42% of which resulted in abortion [7]. It is estimated that, by the time an American women reaches the age of 45, about one in every two women will have had an unintended pregnancy [8], and one in every three will have had an abortion [9]. The risk of unintended pregnancies rises with inconsistent and incorrect condom use, with typical-use condom failure rates of approximately 15% [10]. Among condom-using women, inconsistent condom use was cited as the most common reason for an unintended pregnancy resulting in abortion [11].
According to the National Survey of Family Growth, 39% of unmarried, sexually active women reported any condom use, and only 29% reported consistent condom use during every episode of sexual intercourse [12]. Similarly, only 54% of sexually active female high school students surveyed in the 2009 Youth Risk Behavior Surveillance System reported condom use during their last intercourse [13]. Even among consistent condom users, there may be instances of incorrect condom use, such as genital contact prior to or after condom use, as well as condom breakage, slippage, or leakage.[14] Published data suggest that incorrect condom use can be as high as 40–50% among condom users [15–17].
Based on previous literature regarding self-reported condom use among young women, [18–21], we hypothesized that inconsistent condom use is associated with the frequency of intercourse and low condom use self-efficacy. In this analysis, our primary aim was to determine the demographic characteristics and sexual behaviors associated with inconsistent and incorrect condom use among sexually active women at high risk for unintended pregnancies and STIs.
MATERIALS AND METHODS
The Contraceptive CHOICE Project (CHOICE) is an ongoing prospective cohort study that plans to enroll 10,000 women. The methods of this study have been described in detail elsewhere [22]. Briefly, women ages 14 to 45 years are offered contraceptive counseling, their preferred method of reversible contraception for 3 years, and baseline and annual screening for STIs at no cost. Women who are sexually active with a male partner within the previous 6 months or anticipate sexual activity within the next 6 months, have not had a tubal ligation or hysterectomy, do not desire a pregnancy within the next year, and are willing to initiate use of a new contraceptive method are eligible to participate. Standardized surveys are administered by trained personnel at baseline and at 3 months, 6 months, and then every 6 months during a 3-year follow-up period. The CHOICE protocol was approved by the Human Research Protection Office at the Washington University in St. Louis School of Medicine prior to participant recruitment.
We analyzed the baseline survey data collected from the first 5,087 women enrolled in CHOICE from August 2007 through December 2009. Because only 7% of participants reported concurrent sexual partners in the last 30 days, we focused our analyses on women who reported both sexual activity and at least one instance of condom use with a main sexual partner within the 30 days prior to their enrollment dates. We collected basic demographic information (i.e., race, ethnicity, age, marital status, education level, socioeconomic status), and interviewed participants regarding their sexual history and behaviors. Women reported number of lifetime sexual partners, age at first intercourse, duration of relationship with their main partner, contraceptive use at time of enrollment, number of sex acts in the past 30 days with and without condom use, and the number of condom problems in the past 30 days. Women reported a mean number of 9 sex acts in the past 30 days, and therefore we dichotomized the frequency of intercourse as fewer than 10 vs. more than 10 sex acts for our analysis. Condom problems were defined as condom breakage or slippage, genital contact before or after condom use, or wearing the condom inside-out and flipping it over for re-use. Using Likert scales, participants also rated their perceived STI risk in the next 3 months and their perceived partner willingness to use condoms. Participants were asked about their reasons for condom use, perceived control over condom use, and about their condom use self-efficacy. We defined condom use self-efficacy as “a participant’s confidence in her ability to negotiate condom use successfully with her partner across different challenging situations” [18]. Condom use self-efficacy questions were based on the 5-item version of the Confidence in Safer Sex scale (i.e., “How sure are you that you would use condoms even when you are a little drunk or high? When your partner gets annoyed about using condoms? When you are really sexually excited? When you feel depressed? When the disease risk seems low?”) [23]. Scores on each of the 5 condom use self-efficacy questions were summed for each participant (range 5–25), with higher scores reflecting higher condom use self-efficacy; based on their summed scores, participants were grouped into quartiles for analysis. At enrollment participants were screened for sexually transmitted infections using self-collected vaginal swabs; Chlamydia trachomatis and Neisseria gonorrhoeae using the BD ProbeTec ET (Becton Dickinson, Sparks, MD) and Trichomonas vaginalis using the InPouch™ TV (BioMed Diagnostics, White City, Oregon).
Condom use was treated as count data and represented the number of unprotected sexual acts within the past 30 days. Incorrect condom use was dichotomized and defined as the incidence of one or more condom problems during the past 30 days. In this analysis, we compared the demographic and behavioral characteristics of consistent versus inconsistent condom users, and correct versus incorrect condom users. We performed chi-square and Student’s t-tests for comparisons of categorical and continuous variables, respectively. Independent predictors of inconsistent and incorrect condom use were identified from the literature or via univariate analyses (unadjusted alpha of 0.05) and included in multivariable regression. We used Poisson regression to estimate the risk of the number of unprotected sexual acts by multiple independent variables. Because the prevalence of incorrect condom use was greater than 10% we used Poisson regression with robust error variance for more conservative relative risk estimates [24]. Multicollinearity was examined using the variance inflation factor (VIF) for all variables considered in the model; all variables considered had a VIF of less than 10. Statistical analyses were performed using SAS Software (v9.2, SAS Institute, Cary, NC) and STATA 11 (College Station, TX).
RESULTS
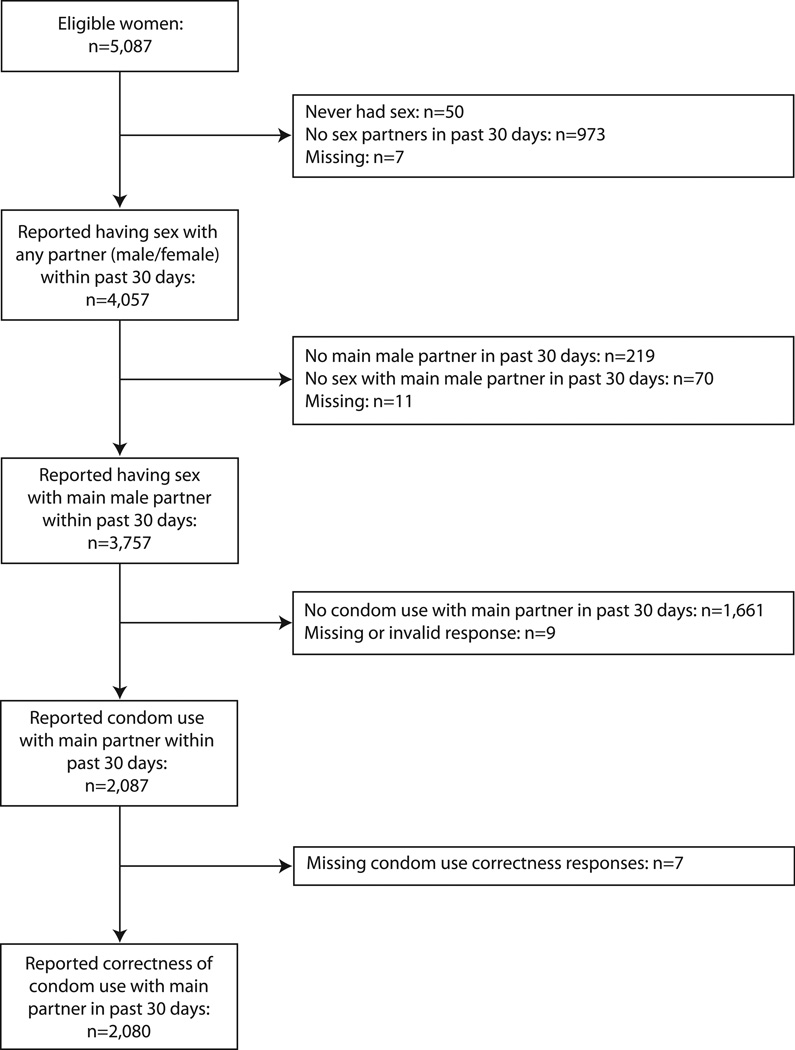
Among the first 5,087 women enrolled in CHOICE, 3,757 reported having sex with a main male partner. Of these women, 2,087 (56%) reported at least one instance of condom use with their main partner within the past 30 days (Figure 1). However, only 59% (n=1,240) of these women reported consistent condom use. The demographic and behavioral characteristics of consistent versus inconsistent condom users are shown in Table 1. In univariate analyses, marital status and education were significantly associated with an increased number of unprotected acts during the past 30 days. Separated, divorced, or widowed women were more likely to report a greater number of unprotected acts compared to single or never married women (RR=1.7, 95% CI 1.1, 2.5), and women with some college education reported a 50% greater number of unprotected acts compared to women with a college or graduate degree (RR=1.5, 95% CI 1.2, 2.0).
Figure 1.
Flow diagram of the numbers of study participants included in each data analysis step.
Table 1.
Demographic and behavioral correlates of inconsistent condom use among sexually active women enrolled in the Contraceptive CHOICE Project who reported any condom use within the past 30 days.
| Condom Use | Risk for Number of Unprotected Actsa | |||||
|---|---|---|---|---|---|---|
| Consistent | Inconsistent | Crude | Adjusted | |||
| n=1240 | n=847 | Relative Risk | 95% CI | Relative Risk | 95% CI | |
| Demographic Characteristics | ||||||
| Race | ||||||
| African American | 45.6 | 49.0 | 0.90 | 0.73, 1.11 | 1.26 | 1.04, 1.53 |
| White | 47.2 | 42.0 | Referent | -- | Referent | - |
| Other | 7.2 | 9.0 | 1.24 | 0.88, 1.76 | 1.30 | 0.93, 1.82 |
| Ethnicity | ||||||
| Hispanic | 4.7 | 5.4 | 1.17 | 0.77, 1.78 | ||
| Non-Hispanic | 95.3 | 94.6 | Referent | -- | ||
| Age (years) | ||||||
| <21 | 26.0 | 22.4 | Referent | -- | -- | -- |
| 21–25 | 39.5 | 41.9 | 1.03 | 0.81, 1.38 | 0.93 | 0.72, 1.21 |
| >25 | 34.5 | 35.7 | 1.08 | 0.83, 1.42 | 0.87 | 0.66, 1.16 |
| Marital status | ||||||
| Single/never married | 64.6 | 59.7 | Referent | -- | -- | -- |
| Married/living with a partner | 30.9 | 33.1 | 1.10 | 0.89, 1.36 | 0.96 | 0.75, 1.21 |
| Separated/divorced/widowed | 4.5 | 7.2 | 1.65 | 1.11, 2.45 | 1.02 | 0.68, 1.51 |
| Education level | ||||||
| ≤ High school | 32.5 | 36.2 | 1.14 | 0.86 1.52 | 1.08 | 0.81, 143 |
| Some college | 43.1 | 44.4 | 1.51 | 1.15, 1.98 | 1.19 | 0.91, 1.55 |
| College degree/graduate degree | 24.4 | 19.4 | Referent | -- | -- | -- |
| Trouble paying for basic necessities in the past 12 months or currently receives public assistance | ||||||
| No | 47.3 | 41.1 | Referent | -- | ||
| Yes | 52.7 | 58.9 | 1.12 | 0.92, 1.37 | ||
| Behavioral Characteristics | ||||||
| Lifetime sexual partners | ||||||
| 1–4 | 44.5 | 35.5 | Referent | -- | Referent | -- |
| 5–9 | 31.1 | 31.0 | 1.47 | 1.17, 1.86 | 1.21 | 0.97, 1.50 |
| ≥10 | 24.4 | 33.5 | 2.04 | 1.61, 2.57 | 1.58 | 1.24, 2.02 |
| Age at first intercourse (years) | ||||||
| <14 | 7.3 | 8.0 | 2.06 | 1.32, 3.20 | 1.70 | 1.15, 2.52 |
| 14–18 | 75.7 | 79.6 | 1.61 | 1.23, 2.12 | 1.36 | 1.06, 1.75 |
| ≥19 | 17.0 | 12.4 | Referent | -- | Referent | -- |
| Duration of sexual relationship with partner | ||||||
| 0–3 months | 23.4 | 19.2 | Referent | -- | Referent | -- |
| 4–6 months | 10.6 | 13.5 | 1.72 | 1.23, 2.40 | 1.33 | 1.00, 1.76 |
| 7–12 months | 10.7 | 11.3 | 1.50 | 1.04, 2.17 | 1.26 | 0.90, 1.77 |
| >1 year | 55.3 | 56.0 | 1.13 | 0.86, 1.48 | 1.23 | 0.93, 1.63 |
| Perceived STI risk with partner in next 3 months | ||||||
| Not at all likely | 83.0 | 83.2 | Referent | -- | ||
| More than not at all likely | 17.0 | 16.8 | 0.90 | 0.67, 1.22 | ||
| Number of sex acts in the past 30 days | ||||||
| 1–9 | 73.6 | 49.6 | Referent | -- | Referent | -- |
| ≥10 | 26.4 | 50.4 | 7.92 | 6.83, 9.18 | 6.97 | 5.95, 8.17 |
| Perceived control over condom use | ||||||
| Partner has more say | 3.2 | 3.3 | 1.23 | 0.74, 2.07 | 1.16 | 0.73, 1.85 |
| Equal say | 54.0 | 42.8 | Referent | -- | Referent | -- |
| You have more say | 40.9 | 52.6 | 1.30 | 1.06, 1.60 | 1.11 | 0.91, 1.35 |
| Don’t talk about it | 1.9 | 1.3 | 1.08 | 0.50, 2.34 | 0.88 | 0.45, 1.74 |
| Condom use self-efficacy | ||||||
| 1st quartile (Lowest; 5–14) | 5.6 | 21.6 | 4.46 | 3.40, 6.34 | 2.50 | 1.81, 3.47 |
| 2nd quartile (15–19) | 20.3 | 34.8 | 2.17 | 1.59, 2.95 | 1.59 | 1.16, 2.17 |
| 3rd quartile (20–23) | 34.7 | 25.3 | 1.23 | 0.88, 1.72 | 1.17 | 0.84, 1.63 |
| 4th quartile (Highest; 24–25) | 39.4 | 18.3 | Referent | -- | Referent | -- |
| Perceived partner willingness to use condoms | ||||||
| Extremely willing | 76.6 | 49.5 | Referent | -- | Referent | -- |
| Not extremely willing | 23.4 | 50.5 | 2.20 | 1.81, 2.68 | 1.47 | 1.20, 1.80 |
| Reason for condom use with partner | ||||||
| Prevent only pregnancy or only STI | 34.4 | 48.7 | 1.66 | 1.35, 2.03 | 1.29 | 1.07, 1.56 |
| Both | 65.6 | 51.3 | Referent | -- | Referent | -- |
| Incorrect condom use | ||||||
| No | 68.3 | 56.7 | Referent | -- | Referent | -- |
| Yes | 31.7 | 43.3 | 1.57 | 1.29, 1.92 | 1.07 | 0.89, 1.29 |
| Concurrent contraceptive use | ||||||
| No | 83.2 | 77.2 | Referent | -- | Referent | -- |
| Yes | 16.8 | 22.8 | 1.30 | 1.04, 1.63 | 1.20 | 0.97, 1.48 |
| Positive for STI at baselineb | ||||||
| No | 93.5 | 93.5 | Referent | -- | ||
| Yes | 6.5 | 6.5 | 1.06 | 0.75, 1.52 | ||
Poisson regression used to estimate the risk of number of unprotected sex acts (count) across independent variable categories
Participant tested positive for Chlamydia trachomatis, Neisseria gonorrhoeae, or Trichomonas vaginalis at baseline enrollment
Of the behavioral characteristics significantly associated with a greater number of unprotected acts, women who reported 10 or more lifetime sexual partners (RR=2.0, 95% CI 1.6, 2.6), younger age at first intercourse (RR=2.1, 95% CI 1.3, 3.2), 10 or more acts of intercourse in the past 30 days (RR=7.9, 95% CI 6.8, 9.2), decreased condom use self-efficacy (RR=4.5, 95% CI 3.4, 6.3), and less partner willingness to use condoms (RR=2.2, 95% CI 1.8, 2.7) reported at least twice the number of unprotected acts than women who did not report these behaviors. Screening positive for an STI at baseline was not significantly associated with the risk of a greater number of unprotected acts during the past 30 days.
Table 1 also presents the results of our multivariable analysis. We included race, age, and the 12 statistically significant variables from univariate analysis in our final model. Importantly, women who engaged in 10 or more sex acts within the past 30 days reported nearly seven times the number of unprotected acts compared to women who reported less than 10 acts (RRadj=7.0, 95% CI 6.0, 8.2). Women in the lowest (RRadj=2.5, 95% CI 1.8, 3.5) and second lowest (RRadj=1.6, 95% CI 1.2, 2.2) quartiles for condom use self-efficacy reported 2.5 and 1.6 times the number of unprotected acts compared to women who reported high condom use self-efficacy (uppermost 4th quartile).
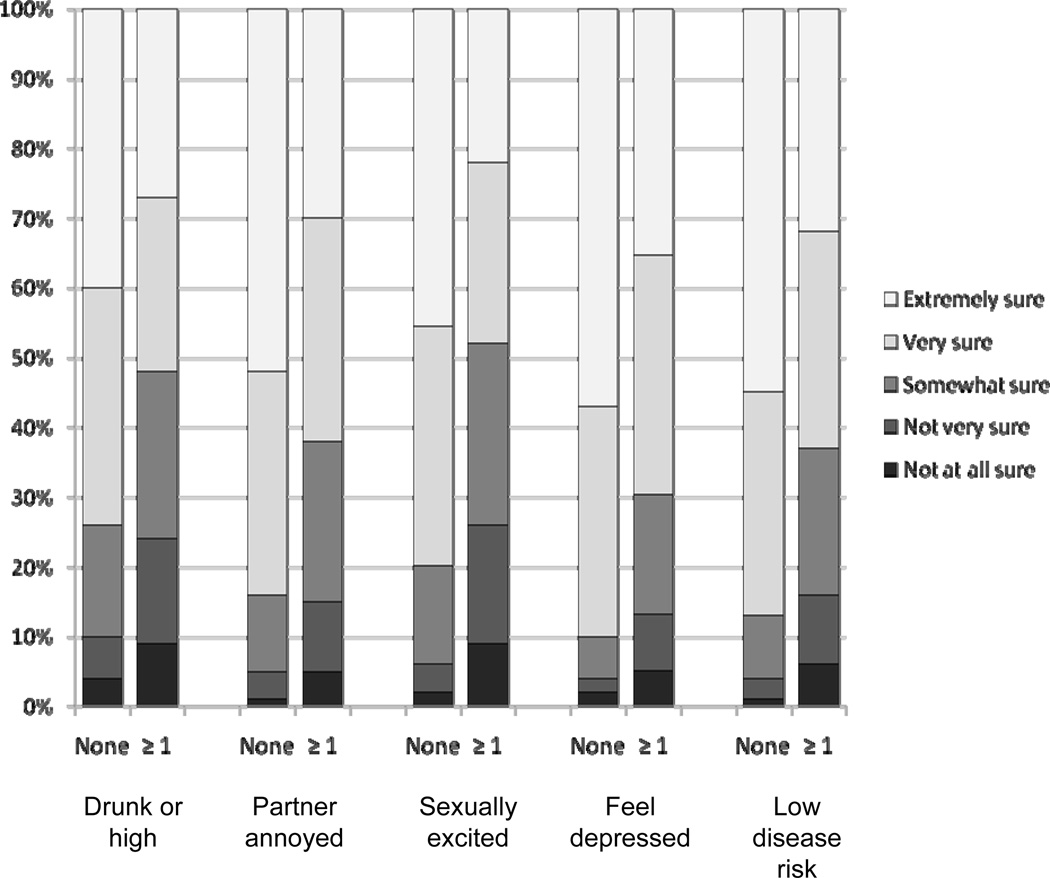
Two out of every three participants reported they were “very sure” or “extremely sure” they would use a condom in each of the five condom use self-efficacy scenarios (Figure 2). Women who reported reduced confidence (e.g., “not at all sure”, “not very sure”, or “somewhat sure”) were more likely to report at least one act of unprotected intercourse compared to women who were “very” or “extremely sure”. Specifically, in unadjusted analyses women who reported reduced confidence were significantly more likely to report unprotected intercourse than protected intercourse when they were a little drunk or high (RR=2.7, 95% CI 2.2, 3.2), their partner was annoyed by using condoms (RR=1.7, 95% CI 1.6, 1.9), sexually excited (RR=2.2, 95% CI 1.9, 2.4), depressed (RR=1.9, 95% CI 1.8, 2.1), and perceived their disease risk to be low (RR=2.0, 95% CI 1.8, 2.2).
Figure 2.
Condom self-efficacy (5-point Likert scale) reported for each of the five scenarios by unprotected sexual acts during the past 30 days (none or ≥ 1).
Among the 2,087 women who reported condom use with a main partner in the past 30 days, data regarding correct condom use were available for 2,080 women; 36% (n=757) reported using condoms incorrectly. Incorrect condom use was reported by 43% of inconsistent condom users and 32% of consistent condom users. Overall, 2,080 women reported 14,193 acts of condom use during the past 30 days; the rate of breakage or slippage was 4.5% (n=634), the rate of flipping the condom over for re-use was 1.6% (n=228), and the rate of genital contact before or after condom use was 14.1% (n=2001). Condom breakage or slippage was reported by 17% (n=355) of women, flipping the condom over for re-use was reported by 5% (n=95), and genital contact before or after condom use was reported by 22% (n=455) of women.
Table 2 presents the demographic and behavioral characteristics of correct and incorrect condom users. Women 21–25 years (RR=1.2, 95% CI 1.0, 1.4) or separated, widowed, or divorced (RR=1.3, 95% CI 1.0, 1.6) were more likely to report incorrect condom use. Compared with correct condom users, incorrect users perceived themselves to be at greater risk for future STIs with their main partners (RR=1.2, 95% CI 1.0, 1.4), participated in a greater number of sex acts in the past 30 days (RR=1.6, 95% CI 1.5, 1.8), had lower condom use self-efficacy (RR=1.5, 95% CI 1.2, 1.7), perceived their main partners to be less willing to use condoms (RR=1.2, 95% CI 1.1, 1.3), and more often used condoms inconsistently (RR=1.4, 95% CI 1.2, 1.5). On multivariable analysis (Table 2), women who perceived themselves to be at higher risk for STIs in the next 3 months (RRadj=1.2, 95% CI 1.1, 1.4), engaged in 10 or more sex acts in the past 30 days (RRadj=1.5, 95% CI 1.4, 1.7) or who used condoms inconsistently (RRadj=1.2, 95% CI 1.0, 1.3) were significantly more likely to use condoms incorrectly after adjusting for age, race, marital status, condom use self-efficacy, and perceived partner willingness to use condoms.
Table 2.
Demographic and behavioral correlates of reporting one or more condom problems during condom use among sexually active women enrolled in the Contraceptive CHOICE Project who reported any condom use within the past 30 days.
| Condom Use | Risk for Any Incorrect Condom Usea | |||||
|---|---|---|---|---|---|---|
| Correct | Incorrect | Crude | Adjusted | |||
| n=1323 | n=757 | Relative Risk | 95% CI | Relative Risk | 95% CI | |
| Demographic Characteristics | ||||||
| Race | ||||||
| African American | 48.2 | 44.9 | 0.90 | 0.80, 1.01 | 0.95 | 0.84, 1.08 |
| White | 43.4 | 47.8 | Referent | -- | Referent | -- |
| other | 8.4 | 7.3 | 0.86 | 0.68, 1.08 | 0.81 | 0.64, 1.01 |
| Ethnicity | ||||||
| Hispanic | 4.5 | 5.9 | 1.20 | 0.96, 1.51 | ||
| Non-Hispanic | 95.5 | 94.1 | Referent | -- | ||
| Age (years) | ||||||
| <21 | 25.7 | 22.6 | Referent | -- | -- | -- |
| 21–25 | 38.6 | 43.7 | 1.17 | 1.01, 1.36 | 1.11 | 0.96, 1.30 |
| >25 | 35.7 | 33.7 | 1.05 | 0.90, 1.23 | 0.97 | 0.82, 1.15 |
| Marital status | ||||||
| Single/never married | 62.9 | 62.3 | Referent | -- | -- | -- |
| Married/living with a partner | 32.4 | 30.7 | 0.97 | 0.86, 1.10 | 0.98 | 0.86, 1.12 |
| Separated/divorced/widowed | 4.7 | 7.0 | 1.27 | 1.03, 1.57 | 1.19 | 0.92, 1.50 |
| Education level | ||||||
| ≤ High school | 34.7 | 32.9 | 0.99 | 0.84, 1.16 | ||
| Some college | 42.7 | 45.1 | 1.05 | 0.91, 1.22 | ||
| College degree/graduate degree | 22.6 | 22.0 | Referent | -- | ||
| Trouble paying for basic necessities in the past 12 months or currently receives public assistance | ||||||
| No | 45.9 | 42.8 | Referent | -- | ||
| Yes | 54.1 | 57.2 | 1.08 | 0.97, 1.22 | ||
| Behavioral Characteristics | ||||||
| Lifetime sexual partners | ||||||
| 1–4 | 41.7 | 39.2 | Referent | -- | Referent | -- |
| 5–9 | 31.8 | 29.8 | 1.00 | 0.87, 1.15 | 0.92 | 0.80, 1.07 |
| ≥10 | 26.5 | 31.0 | 1.15 | 1.00, 1.13 | 1.04 | 0.90, 1.20 |
| Age at first intercourse (years) | ||||||
| <14 | 7.9 | 7.0 | 0.87 | 0.67, 1.13 | ||
| 14–18 | 77.5 | 77.0 | 0.94 | 0.81, 1.10 | ||
| ≥19 | 14.6 | 16.0 | Referent | -- | ||
| Duration of sexual relationship with partner | ||||||
| 0–3 months | 20.8 | 23.2 | Referent | -- | ||
| 4–6 months | 11.5 | 12.3 | 0.97 | 0.80, 1.19 | ||
| 7–12 months | 10.5 | 11.9 | 1.00 | 0.82, 1.22 | ||
| >1 year | 57.2 | 52.6 | 0.88 | 0.77, 1.02 | ||
| Perceived STI risk with partner in next 3 months | ||||||
| Not at all likely | 84.5 | 80.7 | Referent | -- | Referent | -- |
| More than not at all likely | 15.5 | 19.3 | 1.18 | 1.02, 1.36 | 1.24 | 1.08, 1.42 |
| Number of sex acts in the past 30 days | ||||||
| 1–9 | 70.5 | 52.2 | Referent | -- | Referent | -- |
| ≥10 | 29.5 | 47.8 | 1.62 | 1.45, 1.81 | 1.52 | 1.35, 1.71 |
| Perceived control over condom use | ||||||
| Partner has more say | 3.2 | 3.3 | 1.04 | 0.76, 1.44 | ||
| Equal say | 50.0 | 48.5 | Referent | -- | ||
| You have more say | 44.8 | 47.1 | 1.05 | 0.94, 1.18 | ||
| Don’t talk about it | 2.0 | 1.1 | 0.66 | 0.36, 1.21 | ||
| Condom use self-efficacy | ||||||
| 1st quartile (Lowest; 5–14) | 9.7 | 16.3 | 1.46 | 1.24, 1.73 | 1.19 | 0.99, 1.43 |
| 2nd quartile (15–19) | 25.9 | 26.6 | 1.10 | 0.94, 1.29 | 0.97 | 0.83, 1.15 |
| 3rd quartile (20–23) | 32.2 | 28.9 | 1.02 | 0.87, 1.19 | 0.98 | 0.84, 1.15 |
| 4th quartile (Highest; 24–25) | 32.2 | 28.2 | Referent | -- | Referent | -- |
| Perceived partner willingness to use condoms | ||||||
| Extremely willing | 67.7 | 61.7 | Referent | -- | Referent | -- |
| Not extremely willing | 32.3 | 38.3 | 1.18 | 1.05, 1.32 | 1.09 | 0.96, 1.24 |
| Reason for condom use with partner | ||||||
| Prevent only pregnancy or only STI | 39.5 | 41.1 | 1.04 | 0.93, 1.17 | ||
| Both | 60.5 | 58.9 | Referent | -- | ||
| Consistency of condom use during past 30 days | ||||||
| Used condoms “every time” | 63.7 | 51.7 | Referent | -- | Referent | -- |
| Used condoms “less than every time” | 36.3 | 48.3 | 1.37 | 1.22, 1.53 | 1.15 | 1.02, 1.31 |
| Concurrent contraceptive use | ||||||
| No | 80.2 | 81.8 | Referent | -- | ||
| Yes | 19.8 | 18.2 | 0.94 | 0.81, 1.09 | ||
| Positive for STI at baselineb | ||||||
| No | 92.7 | 94.7 | Referent | -- | ||
| Yes | 7.3 | 5.3 | 0.80 | 0.61, 1.04 | ||
Poisson regression with robust error variance used to estimate the risk of any condom problems (binary outcome) across independent variable categories
Participant tested positive for Chlamydia trachomatis, Neisseria gonorrhoeae, or Trichomonas vaginalis at baseline enrollment
DISCUSSION
In our analysis, we identified the demographic and behavioral correlates of inconsistent and incorrect condom use among a cohort of sexually active, condom-using women at high risk for both STIs and unintended pregnancies. The number of unprotected sexual acts was most strongly predicted by a greater number of sex acts in the past 30 days, higher perception of partner willingness to use condoms, condom use self-efficacy, and young age at first intercourse. The finding that women who engaged in a greater number of sex acts reported greater unprotected acts is similar to other published studies [18, 20]. For women who have sex frequently, condom use may be particularly burdensome and decidedly more challenging than simply forgoing condom use.
Additionally, women’s perceptions of their partners’ willingness to use condoms predict their actual condom use behavior; women are less likely to use condoms consistently if they perceive their partners to be reluctant to use condoms [25–27]. Negotiating condom use may be more difficult if women perceive their partners to be less willing to use condoms or if they have more frequent sex. Interestingly, however, evidence suggests that women actually underestimate their partners’ desires to use condoms [27], indicating the need for more partner dialogue about condom use. Discussions about condom use among women and their partners may encourage them to use condoms more consistently.
We also observed a strong association between condom use self-efficacy and inconsistent condom use—women with lower self-efficacy to use condoms were more than twice as likely to report a greater number of unprotected acts compared to women with high condom use self-efficacy. Our finding is consistent with the results from Project PROTECT, which observed a 1.6 increased odds of unprotected intercourse among young women with low condom use self-efficacy [18]. Similarly, another study reported condom use self-efficacy accounted for 64% of the variance in condom use, with higher self-efficacy correlated with more consistent condom use [21]. A third of women in our study reported reduced self-efficacy in all five scenarios. We found that within each scenario, reduced self-efficacy was associated with a much greater risk of unprotected sex; an important finding that may provide possible opportunities for targeted education.
In this cohort of CHOICE women, incorrect condom use was reported by 36% of women with similar rates of breakage or slippage (4.5%), flipping the condom over for re-use (1.6%), or penile-genital contact prior to use (14.1%) as recently reported in a randomized clinical trial of condom users [14, 28]. Incorrect use was most strongly correlated with the number of sex acts in the past 30 days, the consistency of condom use, and one’s perceived risk for future STIs. Women who reported more than 10 sex acts in the past 30 days were 50% more likely to use condoms incorrectly or experience a condom problem, suggesting that there is increased risk of error with each act of condom use. Consistent with previous studies [16, 29], incorrect condom users were also more likely to be inconsistent condom users, perhaps because these couples are less practiced at using condoms.
Although we categorized condom breakage and slippage as incorrect condom use in our analysis, we recognize that these problems are more likely due to the properties of the condom rather than the characteristics of the user. To investigate the possibility that cases of condom breakage and slippage are different from other cases of incorrect use (i.e., genital contact before or after condom use and flipping a condom over for re-use), we performed a separate analysis for correct condom use after excluding women who reported condom breakage or slippage as the only condom problem they encountered (12%, n=243). Similar to the results from our previous analysis, frequent sex acts (RRadj=1.5, 95% CI 1.3, 1.8) and inconsistent condom use (RRadj=1.4, 95% CI 1.2, 1.7) remained significantly associated with incorrect condom use after adjusting for variables that were significant in univariate analysis. Unexpectedly, however, incorrect condom use was no longer associated with a higher perceived risk for future STIs. Perhaps because condom breakage and slippage are obvious condom use problems, women who experienced these problems can better appreciate that they are at higher risk for future STIs.
There are a number of strengths to this study. Our analysis was performed using data from a large sample of diverse women, who are at high risk for both STIs and unintended pregnancies. We explored a wide range of demographic and behavioral characteristics associated with condom use in the literature, and explored both consistent and correct condom use. However, we acknowledge several limitations to this analysis. Although diverse, women in our analysis were enrolled in a cohort study investigating the satisfaction and continuation rates of contraception, did not wish to become pregnant for one year, and were willing to try a new contraceptive method. Therefore, our study population might differ from the general population of women, potentially reducing the generalizability of our results. Additionally, our data were obtained via self-report, which by nature is prone to information bias. However, we minimized the extent of bias by administering quantitative, standardized surveys by trained personnel. Finally, we did not observe an association between baseline STI and inconsistent or incorrect condom use. Our condom use variables were limited to behavior during the 30 days prior to STI testing, while pre-existing cases could have occurred prior to that period. Furthermore, we did not assess the STI-infection status of the male partner which has been shown to be important when evaluating condom effectiveness for prevalent gonorrhea and chlamydia infections [30].
In summary, consistent condom use among sexually active women is most strongly influenced by the frequency of sex, women’s self-efficacy to use condoms, and perceptions about partner willingness to use condoms. Correct condom use is most strongly associated with the frequency of sex, the consistency of condom use, and women’s perceptions about their risk for future STIs. Interventions to improve consistent and correct condom use should promote skills for condom negotiation, encourage regular partner communication and discussions about condom use, and emphasize the importance of condoms for STI prevention rather than exclusively as contraception. This may improve women’s self-efficacy and abilities to successfully negotiate and implement condom use with their partners. However, because condoms are frequently used inconsistently or incorrectly, it is equally important to counsel women on other methods of STI prevention, including prudent partner selection, frequent self and partner STI screening, and sexual abstinence when practical.
Acknowledgements
This research was supported in part by a Midcareer Investigator Award in Women’s Health Research (K24 HD01298), Award Number K12HD001459 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Clinical and Translational Science Awards (UL1RR024992, TL1 RR024995), and by Grant Number KL2RR024994 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Cates W, Jr, Steiner MJ. Dual protection against unintended pregnancy and sexually transmitted infections: what is the best contraceptive approach? Sex Transm Dis. 2002 Mar;29(3):168–174. doi: 10.1097/00007435-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2008. Atlanta, GA: U.S. Department of Health and Human Services; 2009. Nov, [Google Scholar]
- 3.HIV prevalence estimates--United States, 2006. MMWR Morb Mortal Wkly Rep. 2008 Oct 3;57(39):1073–1076. [PubMed] [Google Scholar]
- 4.Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ. 2004 Jun;82(6):454–461. [PMC free article] [PubMed] [Google Scholar]
- 5.Shlay JC, McClung MW, Patnaik JL, et al. Comparison of sexually transmitted disease prevalence by reported level of condom use among patients attending an urban sexually transmitted disease clinic. Sex Transm Dis. 2004 Mar;31(3):154–160. doi: 10.1097/01.olq.0000114338.60980.12. [DOI] [PubMed] [Google Scholar]
- 6.Warner L, Stone KM, Macaluso M, et al. Condom use and risk of gonorrhea and Chlamydia: a systematic review of design and measurement factors assessed in epidemiologic studies. Sex Transm Dis. 2006 Jan;33(1):36–51. doi: 10.1097/01.olq.0000187908.42622.fd. [DOI] [PubMed] [Google Scholar]
- 7.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States 1994 and 2001. Perspect Sex Reprod Health. 2006 Jun;38(2):90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 8.Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspect. 1998 Jan–Feb;30(1):24–29. 46. [PubMed] [Google Scholar]
- 9.Guttmacher Institute. State Facts About Abortion. New York: 2006. [cited October 15, 2010]. Available from: http://www.guttmacher.org/pubs/sfaa/new_york.html. [Google Scholar]
- 10.Choice of contraceptives. Treat Guidel Med Lett. 2007 Dec;5(64):101–108. [PubMed] [Google Scholar]
- 11.Jones RK, Darroch JE, Henshaw SK. Contraceptive use among U.S. women having abortions in 2000–2001. Perspect Sex Reprod Health. 2002 Nov–Dec;34(6):294–303. [PubMed] [Google Scholar]
- 12.Chandra A, Martinez GM, Mosher WD, et al. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat. 2005 Dec;23(25):1–160. [PubMed] [Google Scholar]
- 13.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance - United States, 2009. MMWR Surveill Summ. 2010 Jun 4;59(5):1–142. [PubMed] [Google Scholar]
- 14.Duerr A, Gallo MF, Warner L, et al. Assessing Male Condom Failure and Incorrect Use. Sex Transm Dis. 2011 Jan 27;38(12) doi: 10.1097/OLQ.0b013e3182096b62. [DOI] [PubMed] [Google Scholar]
- 15.Shrier LA, Walls C, Lops C, et al. Correlates of Incorrect Condom Use among Depressed Young Women: An Event-level Analysis. J Pediatr Adolesc Gynecol. 2010 May;19 doi: 10.1016/j.jpag.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Warner L, Newman DR, Kamb ML, et al. Problems with condom use among patients attending sexually transmitted disease clinics: prevalence, predictors, and relation to incident gonorrhea and chlamydia. Am J Epidemiol. 2008 Feb 1;167(3):341–349. doi: 10.1093/aje/kwm300. [DOI] [PubMed] [Google Scholar]
- 17.Crosby R, Sanders S, Yarber WL, et al. Condom-use errors and problems: a neglected aspect of studies assessing condom effectiveness. Am J Prev Med. 2003 May;24(4):367–370. doi: 10.1016/s0749-3797(03)00015-1. [DOI] [PubMed] [Google Scholar]
- 18.Peipert JF, Lapane KL, Allsworth JE, et al. Women at risk for sexually transmitted diseases: correlates of intercourse without barrier contraception. Am J Obstet Gynecol. 2007 Nov;197(5):e471–e478. doi: 10.1016/j.ajog.2007.03.032. 474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Posner SF, Pulley LV, Artz L, et al. Psychosocial factors associated with self-reported male condom use among women attending public health clinics. Sex Transm Dis. 2001 Jul;28(7):387–393. doi: 10.1097/00007435-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Wiemann CM, Chacko MR, Kozinetz CA, et al. Correlates of consistent condom use with main-new and main-old sexual partners. J Adolesc Health. 2009 Sep;45(3):296–299. doi: 10.1016/j.jadohealth.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 21.Lindberg CE. Knowledge, self-efficacy, coping, and condom use among urban women. J Assoc Nurses AIDS Care. 2000 Sep–Oct;11(5):80–90. doi: 10.1016/S1055-3290(06)60387-7. [DOI] [PubMed] [Google Scholar]
- 22.Secura GM, Allsworth JE, Madden T, et al. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010 Aug;203(2):e111–e117. doi: 10.1016/j.ajog.2010.04.017. 115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Redding CA, Rossi JS. Testing a model of situational self-efficacy for safer sex among college students: Stage of change and gender-based differences. Psychol Health. 1999;14(3):467–486. [Google Scholar]
- 24.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998 Nov 18;280(19):1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 25.Bralock A, Koniak-Griffin D. What do sexually active adolescent females say about relationship issues? J Pediatr Nurs. 2009 Apr;24(2):131–140. doi: 10.1016/j.pedn.2008.02.036. [DOI] [PubMed] [Google Scholar]
- 26.Brown LK, DiClemente R, Crosby R, et al. Condom use among high-risk adolescents: anticipation of partner disapproval and less pleasure associated with not using condoms. Public Health Rep. 2008 Sep–Oct;123(5):601–607. doi: 10.1177/003335490812300510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Edwards GL, Barber BL. Women may underestimate their partners' desires to use condoms: possible implications for behaviour. J Sex Res. 2010 Jan;47(1):59–65. doi: 10.1080/00224490902867863. [DOI] [PubMed] [Google Scholar]
- 28.Macaluso M, Blackwell R, Jamieson DJ, et al. Efficacy of the male latex condom and of the female polyurethane condom as barriers to semen during intercourse: a randomized clinical trial. Am J Epidemiol. 2007 Jul 1;166(1):88–96. doi: 10.1093/aje/kwm046. [DOI] [PubMed] [Google Scholar]
- 29.Macaluso M, Kelaghan J, Artz L, et al. Mechanical failure of the latex condom in a cohort of women at high STD risk. Sex Transm Dis. 1999 Sep;26(8):450–458. doi: 10.1097/00007435-199909000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Warner L, Newman DR, Austin HD, et al. Condom effectiveness for reducing transmission of gonorrhea and chlamydia: the importance of assessing partner infection status. Am J Epidemiol. 2004 Feb 1;159(3):242–251. doi: 10.1093/aje/kwh044. [DOI] [PubMed] [Google Scholar]