Abstract
Background:
Metabolic syndrome refers to a constellation of conditions that increases a person’s risk of diabetes and cardiovascular disease. We describe the prevalence of metabolic syndrome and its components in relation to sociodemographic factors in the Canadian adult population.
Methods:
We used data from cycle 1 of the Canadian Health Measures Survey, a cross-sectional survey of a representative sample of the population. We included data for respondents aged 18 years and older for whom fasting blood samples were available; pregnant women were excluded. We calculated weighted estimates of the prevalence of metabolic syndrome and its components in relation to age, sex, education level and income.
Results:
The estimated prevalence of metabolic syndrome was 19.1%. Age was the strongest predictor of the syndrome: 17.0% of participants 18–39 years old had metabolic syndrome, as compared with 39.0% of those 70–79 years. Abdominal obesity was the most common component of the syndrome (35.0%) and was more prevalent among women than among men (40.0% v. 29.1%; p = 0.013). Men were more likely than women to have an elevated fasting glucose level (18.9% v. 13.6%; p = 0.025) and hypertriglyceridemia (29.0% v. 20.0%; p = 0.012). The prevalence of metabolic syndrome was higher among people in households with lower education and income levels.
Interpretation:
About one in five Canadian adults had metabolic syndrome. People at increased risk were those in households with lower education and income levels. The burden of abdominal obesity, low HDL (high-density lipoprotein) cholesterol and hypertriglyceridemia among young people was especially of concern, because the risk of cardiovascular disease increases with age.
Chronic disease contributes significantly to morbidity and mortality in the Canadian population.1 As such, the economic costs are substantial. Metabolic syndrome refers to a constellation of conditions that approximately doubles a person’s risk of cardiovascular disease, independently of other risk factors.2–5 The cause of metabolic syndrome has not been fully elucidated; a summary of the current proposed mechanisms is discussed elsewhere.6
Several sets of criteria have been established for the detection of metabolic syndrome, many of which have been continually updated.6–8 The set of criteria most commonly used in the past was published in the third report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III criteria).9 Recently, the International Diabetes Federation, the American Heart Association, the National Heart, Lung, and Blood Institute, and other organizations collaborated to release a unified set of criteria.10
The Canadian Health Measures Survey, conducted in 2007–2009, was the first cross-sectional survey of a representative sample of Canadians that collected biological samples since the Canadian Heart Health Surveys about 20 years ago.11 We used data from the Canadian Health Measures Survey to describe the prevalence of metabolic syndrome and its components by age, sex, education level and income adequacy in a sample of the Canadian adult population. Because different studies have used various criteria in the past to define metabolic syndrome, and because there is continuing controversy as to the appropriate criteria, we calculated the prevalence according to several types of criteria to better facilitate comparison to findings from past and future studies.
Methods
Study population
We included data from cycle 1 (2007–2009) of the Canadian Health Measures Survey. Procedures and methods for data collection for the survey have been described previously.12,13 In brief, this survey, conducted by Statistics Canada, was completed by a representative sample covering about 96.3% of the Canadian population aged 6–79 years. People living on reserves or in institutions, full-time members of the Armed Forces and people living in remote areas were excluded. Statistics Canada provided weights for each participant that corresponded to the number of people represented by that person in the Canadian population. In brief, participant weights were calculated by multiplying the weight for the collection site by the selection weights for household, and adjusted for nonresponse. The weights for collection site and households were based on the 2006 census. The household weights were then converted to individual weights and further adjusted for nonresponse. Additional details about the sampling and estimations are described elsewhere.14
For our analysis, we selected survey respondents aged 18 years and older regardless of their history of chronic diseases or medication use. We excluded pregnant women. We included data only for participants from whom fasting blood samples were taken, because the criteria for metabolic syndrome require measurements of fasting glucose and plasma triglycerides. As part of the national survey, fasting blood samples were collected from randomly selected participants, who constituted 46.6% of the total adult sample excluding pregnant women. Statistics Canada provided separate weights for this group to ensure appropriate representativeness at the population level; these weights were adjusted for nonresponse.
The ethics approval process for the Canadian Health Measures Survey has been described previously, and all participants gave their informed consent.15 Ethical approval for this project was obtained from the University of Manitoba Health Research Ethics Board and Statistics Canada.
Criteria for metabolic syndrome
We report the prevalence of metabolic syndrome using the original criteria for the syndrome (the Adult Treatment Panel III criteria9). According to these criteria, metabolic syndrome is present if three or more of the following criteria are met: abdominal obesity (waist circumference > 102 cm for men and > 88 cm for women); elevated plasma triglyceride level (≥ 1.7 mmol/L); decreased high-density lipoprotein (HDL) cholesterol level (< 1.03 mmol/L for men and < 1.30 mmol/L for women); elevated blood pressure (≥ 130/85 mm Hg); or elevated fasting glucose level (≥ 6.1 mmol/L). We used this set of criteria to facilitate comparisons with findings from previous studies.
We also report the prevalence of metabolic syndrome using the most recent unified criteria,10 which are identical to the Adult Treatment Panel III criteria except for abdominal obesity (waist circumference ≥ 102 cm for men and ≥ 88 cm for women) and elevated fasting glucose level (≥ 5.6 mmol/L). As recommended by the developers of the unified criteria, we also report prevalence of the syndrome using lower thresholds for waist circumference (≥ 94 cm for men and ≥ 80 cm for women).10 The reason for reporting prevalence using these two sets of cut-offs for waist circumference is because of the limited evidence supporting either cut-off.
Participants who reported taking medication to control blood pressure were considered positive for meeting the elevated blood pressure criterion because biological markers would not accurately reflect risk. Those who had a previous diagnosis of type 2 diabetes were considered to have impaired glucose tolerance. This previous diagnosis was used as a surrogate marker, because data regarding use of diabetes medication may have incorrectly identified people with type 1 diabetes as having impaired glucose tolerance. Data on use of lipid-lowering medications were not available.
Demographic variables
We grouped participants by age as follows: 18–29, 30–39, 40–49, 50–59, 60–69 and 70 years or older. If low cell numbers were present, we merged age groups to meet confidentiality requirements set by Statistics Canada. Education level, determined on the basis of the highest level achieved in the household, was classified into four categories: less than secondary school graduation, secondary school graduation, some postsecondary education and postsecondary graduation. Income adequacy, as defined by Statistics Canada on the basis of total household income and the number of individuals in the household,16 was classified into four categories: lowest income group, lower–middle income group, upper–middle income group and highest income group.
Statistical analysis
Statistical analysis was conducted using SPSS version 18 for data manipulation and weighted analysis (without bootstrapping). We used SUDAAN version 10.0.1 for prevalence estimates and analysis with bootstrapping as per Statistics Canada recommendations. Participants who did not have complete data for all components of the metabolic syndrome were included only in analyses conducted to provide prevalence estimates for individual components. We used the χ2 test to determine differences in prevalence by age group, education level and income level. Binary logistic regression was used to determine predictors of metabolic syndrome. Data presented, including percentages and standard errors, were generated using weighting and bootstrapping. Significance was set at a p value of less than 0.05.
Results
About 1800 participants (rounded to the nearest 10 as per Statistics Canada confidentiality requirements) were included in our study, representing about 24 473 500 Canadians. Missing data for individual components of metabolic syndrome resulted in less than 1% of the sample being excluded for prevalence estimates of metabolic syndrome.
Table 1 shows the estimated prevalence of metabolic syndrome in the Canadian adult population according to the Adult Treatment Panel III criteria, and the unified criteria with standard and low thresholds for abdominal obesity. All results relating to metabolic syndrome are reported hereafter according to the unified criteria.
Table 1:
Weighted estimates of the prevalence of metabolic syndrome among Canadian adults, according to different criteria
| Criteria* | Estimated prevalence, weighted, % (SE) | ||
|---|---|---|---|
| Toal | Men | Women | |
| Adult Treatment Panel III criteria9 | 17.7 (1.6) | 15.9 (1.8) | 19.5 (2.0) |
| Unified criteria10 with high thresholds for waist circumference† | 19.1 (1.7) | 17.8 (2.0) | 20.5 (2.1) |
| Unified criteria10 with low thresholds for waist circumference‡ | 23.2 (1.3) | 23.4 (1.7) | 22.9 (1.8) |
Note: SE = standard error.
See Methods for definitions of criteria.
Threshold set at ≥ 102 cm for men and ≥ 88 cm for women.
Threshold set at ≥ 94 cm for men and ≥ 80 cm for women.
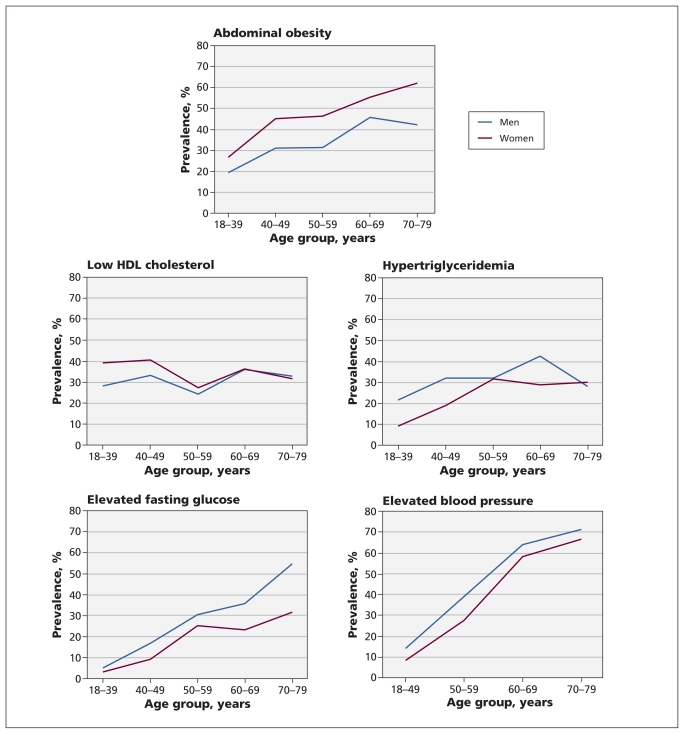
The estimated prevalence was 19.1% overall. The prevalence was higher among women than among men (20.5% v. 17.8%), but this difference was not significant (p = 0.28). Abdominal obesity was the most common component of the syndrome, with 35.0% of the population meeting this criterion (Table 2); it was more prevalent among women than among men (40.0% v. 29.1%; p = 0.013). The prevalence of high blood pressure and low HDL cholesterol did not differ significantly between men and women (Table 2). When the data were stratified by age and sex (Figure 1), we observed that 26.6% of young women (aged 18–39 years) had abdominal obesity and 39.4% had low HDL cholesterol. Among young men, 21.6% had hypertriglyceridemia.
Table 2:
Weighted estimates of the prevalence of metabolic syndrome and its components identified according to the unified criteria, by age, sex and income
| Characteristic | Estimated prevalence, weighted, % (SE) | |||||
|---|---|---|---|---|---|---|
| Metabolic syndrome* | Elevated blood pressure | Elevated fasting glucose | Low HDL cholesterol | Hypertriglyceridemia | Abdominal obesity (high threshold*) | |
| Overall | 19.1 (1.7) | 24.3 (1.5) | 16.2 (1.0) | 33.6 (2.7) | 24.5 (2.2) | 35.0 (2.2) |
| Age group, yr | ||||||
| 18–39‡ | 17.0 (1.4) | 4.9 (1.1) | 4.4 (0.7) | 34.0 (3.7) | 15.6 (2.5) | 23.1 (2.2) |
| 40–49 | 17.5 (3.4) | 22.1 (3.1) | 13.3 (3.2) | 36.7 (3.5) | 26.4 (4.0) | 37.3 (3.8) |
| 50–59 | 27.3 (3.2) | 30.0 (5.0) | 27.8 (3.6) | 26.5 (5.1) | 32.3 (5.3) | 40.5 (4.7) |
| 60–69 | 39.7 (4.3) | 59.2 (2.9) | 29.4 (2.7) | 36.4 (3.7) | 35.6 (2.4) | 51.0 (3.0) |
| 70–79 | 39.0 (5.0) | 64.5 (3.5) | 42.9 (7.1) | 32.4 (5.0) | 29.4 (2.7) | 52.7 (4.2) |
| p value† | < 0.001 | < 0.001 | < 0.001 | 0.45 | 0.001 | < 0.001 |
| Sex | ||||||
| Male | 17.8 (2.0) | 25.5 (2.1) | 18.9 (1.4) | 30.3 (2.1) | 29.0 (3.2) | 29.1 (2.1) |
| Female | 20.5 (2.1) | 23.1 (2.0) | 13.6 (1.4) | 36.8 (4.1) | 20.0 (2.1) | 40.0 (3.7) |
| p value† | 0.28 | 0.39 | 0.025 | 0.12 | 0.012 | 0.013 |
| Education level | ||||||
| Less than secondary school graduation | 40.1 (7.5) | 44.5 (5.6) | 43.5 (6.9) | 37.9 (8.5) | 35.2 (6.3) | 63.8 (7.7) |
| Secondary school graduation | 34.3 (4.5) | 34.5 (5.8) | 25.8 (5.8) | 37.7 (4.2) | 34.3 (5.3) | 49.5 (4.8) |
| Some postsecondary | 9.4 (2.4) | 22.2 (4.5) | 6.1 (1.6) | 31.0 (7.0) | 11.9 (3.8) | 35.9 (6.0) |
| Postsecondary graduation | 15.2 (1.6) | 20.9 (1.5) | 14.1 (0.9) | 32.4 (3.2) | 23.0 (2.5) | 30.0 (2.0) |
| p value† | 0.002 | < 0.001 | 0.001 | 0.58 | 0.015 | 0.003 |
| Income level | ||||||
| Lowest income | 21.3 (6.2) | 25.0 (6.4) | 21.0 (6.4) | 42.6 (6.8) | 19.7 (4.1) | 36.7 (7.4) |
| Lower–middle income | 31.6 (5.4) | 31.8 (4.1) | 24.0 (3.6) | 49.6 (5.8) | 27.5 (5.4) | 46.2 (5.5) |
| Upper–middle income | 20.5 (2.8) | 28.4 (2.1) | 16.4 (1.7) | 33.0 (3.3) | 25.6 (3.4) | 34.5 (2.8) |
| Highest income | 15.2 (1.6) | 18.4 (1.8) | 13.7 (1.7) | 30.5 (2.9) | 24.2 (2.2) | 33.4 (3.2) |
| p value† | 0.0498 | 0.017 | 0.16 | 0.034 | 0.74 | 0.11 |
Note: HDL = high-density lipoprotein, SE = standard error.
According to the unified criteria with high thresholds for waist circumference (≥ 102 cm for men and ≥ 88 cm for women).10
χ2 test.
The age groups 18–29 and 30–39 years were merged to meet privacy standards set by Statistics Canada.
Figure 1:
Weighted estimates of the prevalence of the components of metabolic syndrome (defined according to recent unified criteria10) by age and sex. Abdominal obesity = waist circumference ≥ 102 cm for men and ≥ 88 cm for women. Low level of high-density lipoprotein (HDL) cholesterol = < 1.03 mmol/L for men and < 1.30 mmol/L for women. Hypertriglyceridemia = plasma triglyceride level ≥ 1.7 mmol/L. Elevated fasting glucose level = ≥ 5.6 mmol/L. Elevated blood pressure = ≥ 130/85 mm Hg. For blood pressure, the two youngest groups were collapsed to 18–49 years owing to low prevalence, which compromised confidentiality.
The distribution of prevalence estimates by number of components of metabolic syndrome is summarized in Table 3. Low HDL cholesterol was the most common component that was found on its own, such that 36.1% of those with only one component had low HDL cholesterol (data not shown). When looking at the distribution of the different combinations of components of metabolic syndrome, we observed that impaired glucose tolerance without the presence of any of the other four components occurred in only 15.8% of people with impaired glucose tolerance. Of that 15.8%, the majority were men.
Table 3:
Weighted estimates of the prevalence by number of components of metabolic syndrome identified according to the unified criteria, by age, sex, education level and income
| Characteristic | No. of components identified; estimated prevalence, weighted, % (SE) | p value* | ||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 or 5 | ||
| Overall | 33.3 (2.9) | 28.7 (1.5) | 18.8 (1.3) | 11.7 (1.3) | 7.4 (1.1) | |
| Sex | 0.06 | |||||
| Male | 33.1 (2.6) | 28.0 (2.1) | 21.1 (1.5) | 10.5 (1.5) | 7.3 (1.0) | |
| Female | 33.6 (3.8) | 29.4 (1.7) | 16.5 (1.7) | 13.0 (1.8) | 7.5 (1.6) | |
| Age group, yr | < 0.001 | |||||
| 18–39 | 47.8 (4.8) | 30.6 (3.8) | 15.0 (2.3) | 5.3 (1.2) | 1.2 (0.3) | |
| 40–49 | 30.1 (4.6) | 30.1 (2.7) | 22.3 (4.4) | 11.5 (2.3) | 6.0 (2.6) | |
| 50–59 | 30.2 (6.3) | 26.1 (3.6) | 16.4 (3.4) | 16.0 (1.8) | 11.3 (2.8) | |
| 60–69 | 11.2 (2.0) | 26.8 (2.8) | 22.3 (4.0) | 22.5 (3.8) | 17.2 (2.2) | |
| 70–79 | 10.4 (2.7) | 22.6 (3.9) | 28.1 (2.1) | 18.7 (3.7) | 20.3 (3.9) | |
| Education level† | < 0.001 | |||||
| Less than secondary school graduation | 28.0 (6.4) | 28.0 (6.4) | 40.1 (7.5) | |||
| Secondary school graduation | 50.0 (3.2) | 15.7 (3.5) | 34.3 (4.5) | |||
| Some postsecondary | 67.1 (7.6) | 23.5 (6.8) | 9.4 (2.4) | |||
| Postsecondary graduation | 66.3 (1.9) | 18.5 (1.1) | 15.2 (1.6) | |||
| Income level | 0.010 | |||||
| Lowest income | 36.9 (6.4) | 22.3 (8.3) | 19.5 (6.4) | 7.5 (1.9) | 13.8 (5.5) | |
| Lower–middle income | 21.5 (5.3) | 27.7 (3.0) | 19.2 (4.7) | 18.7 (4.5) | 12.9 (3.8) | |
| Upper–middle income | 30.9 (4.9) | 30.9 (3.9) | 17.7 (2.2) | 13.3 (2.4) | 7.2 (1.3) | |
| Highest income | 36.8 (3.3) | 28.0 (1.8) | 20.0 (1.4) | 9.6 (1.2) | 5.5 (1.6) | |
Note: SE = standard error.
χ2 test.
Those with 0 or 1 component were grouped, as were those with 3 or more components, in keeping with Statistics Canada’s confidentiality requirements.
The most common combination of components among participants who met three of the criteria for metabolic syndrome were abdominal obesity, low HDL cholesterol and hypertriglyceridemia (30.4% of those meeting three criteria). Among participants with four criteria, the most common combination was high blood pressure, abdominal obesity, low HDL cholesterol and hypertriglyceridemia (one-third of those with four criteria).
Education and income level were both significant predictors of metabolic syndrome independent of age and sex: higher levels of education and income were associated with a lower prevalence of metabolic syndrome (Table 4). However, neither education nor income had a linear relation with metabolic syndrome. Income level was not a significant predictor when education was included in the model, probably because education and income level were multicolinear. Sex was not significantly associated with metabolic syndrome, and neither sex-stratified analysis nor interactions between sex and education or income levels revealed any differential patterns between the sexes.
Table 4:
Predictors of metabolic syndrome identified according to the unified criteria, as per binary logistic regression analysis*
| Variable | OR (95% CI) |
|---|---|
| Income level | |
| Lowest income | 0.68 (0.33–1.38) |
| Lower middle income | 1.00 (ref) |
| Upper middle income | 0.49 (0.26–0.93) |
| Highest income | 0.40 (0.21–0.78) |
| Education | |
| Less than secondary school graduation | 0.89 (0.39–2.04) |
| Secondary school graduation | 1.00 (ref) |
| Some postsecondary | 0.30 (0.13–0.70) |
| Postsecondary graduation | 0.45 (0.25–0.81) |
Note: CI = confidence interval, OR = odds ratio.
Two separate models are presented, both adjusted by age and sex.
Interpretation
Using the current unified criteria,10 we found that the prevalence of metabolic syndrome in the Canadian adult population was 19.1%. Although sex-related differences in prevalence were not significant for the syndrome overall, they were significant for the components of impaired glucose tolerance, hypertriglyceridemia and abdominal obesity. In general, there was a significantly higher prevalence of metabolic syndrome and increased number of components associated with lower income level and lower level of household education.
The public health implications of these results are substantial. Greater efforts are needed to address poor lifestyle habits, particularly among younger adults and those of low socioeconomic status. Clinically, these results reiterate the importance of screening for other cardiovascular risk factors among those who meet any of the criteria for metabolic syndrome, but especially among those with impaired glucose tolerance, because it is rarely observed alone. Having health care professionals focus only on impaired glucose tolerance would result in missing a substantial proportion of individuals at risk.
The prevalence of metabolic syndrome reported in our study based on the unified criteria is lower than the prevalence reported in the American adult population 20 years and older included in the National Health and Nutrition Examination Survey (NHANES) III (1988–1994) and the NHANES 1999–2000 survey using the revised Adult Treatment Panel III criteria, which are comparable to the unified criteria.17 The age-adjusted prevalence in the American adult population was 32.3% in 1999–2000, as compared with 19.1% among Canadians in the present sample. A portion of the difference in prevalence between the two populations may be accounted for by the exclusion of people 18–19 years old in the NHANES data, because this age group has low rates of risk factors for chronic diseases.
The Canadian Heart Health Survey, which was conducted from 1986 to 1992 and used an adapted version of the Adult Treatment Panel III criteria, reported a prevalence of 14.4% among Canadians 18–64 years old.11 It is difficult to compare the prevalence to that in the current study and determine whether it has increased because the Canadian Heart Health Survey used body mass index instead of waist circumference, and diabetes diagnosis instead of fasting glucose levels. Nevertheless, the prevalence appears to have increased, particularly in the younger groups. In 1986–1992, 8.7% of men and 4.6% of women aged 18–34 years had metabolic syndrome, as compared with 17.0% overall among those 18–39 years old in the present study. In Australia, 19.5% and 17.2% of men and women more than 24 years old had metabolic syndrome according to the Adult Treatment Panel III criteria.6 Although the Canadian rates of metabolic syndrome are high at 19.1%, the rates are no worse than those in Australia and are lower than those in the United States. Minor differences in the criteria used to identify metabolic syndrome may influence estimates and complicate comparisons.
In another American study based on NHANES data (2003–2006), differences between women and men in the prevalence of the components of metabolic syndrome were similar to those seen in the current study. In the US study, 60.7% of women and 44.8% of men had abdominal obesity,18 as compared with 40.0% of women and 29.1% of men in the Canadian study. Higher rates of abdominal obesity among women in other populations have been previously reported.19,20 Also, in the 2003–2006 US study, 26.5% of women and 35.6% of men had hypertriglyceridemia,18 as compared with 20.0% of women and 29.0% of men in the current study. Neither the NHANES studies nor the current study showed significant differences in the overall prevalence of metabolic syndrome between sexes.17,18
The burden of abdominal obesity, low HDL cholesterol and hypertriglyceridemia among young people in our study is especially of concern, because the risk of cardiovascular disease increases with age. These results are cause for intervention and public health measures to reduce the burden of risk for chronic diseases among young adults. Each component of metabolic syndrome is responsive to lifestyle changes. A French study found that adherence to nutritional guidelines was inversely and significantly associated with HDL cholesterol and overall risk of metabolic syndrome among people 18–49 years old.21
In the current study, the prevalence of metabolic syndrome was higher among participants with lower levels of household education and lower income adequacy. Socioeconomic status has long been known to predict higher rates of many chronic diseases.22 A recent Australian study reported a worse metabolic profile among women than among men in relation to socioeconomic profile, which indicates that low socioeconomic status may affect women’s health to a greater extent.23 This sex-related difference was also noted in the American population.24 We did not, however, observe a sex-related difference in metabolic syndrome in relation to either income adequacy or education level in our study. Similar to our findings, the relation of individual components of metabolic syndrome to income and education was not linear in the Australian sample.23 This is an interesting pattern and contradictory to the linear relation of socioeconomic status and cardiovascular-related outcomes observed by others.22,24,25
Limitations
Our study has several limitations. First, we did not apply ethnic-specific cut-offs to the criteria for metabolic syndrome, as has been suggested in previous research.26,27 There is currently no consensus on the use of ethnic-specific cut-offs for waist circumference.10 Also, the sample was not large enough to determine ethnic patterns of metabolic syndrome, and Aboriginal people living on reserve were excluded from the sample.
Second, the sample we used for analysis was smaller than the overall survey sample, because we could include data only for participants from whom fasting blood samples were taken. However, separate weights for this group were provided by Statistics Canada to account for the smaller sample.
Conclusion
We found that about one in five Canadian adults had metabolic syndrome. People at increased risk were those in households with lower education and income levels. The burden of abdominal obesity, low HDL cholesterol and hypertriglyceridemia among young people is of concern, especially because the risk of cardiovascular disease increases with age. Public health initiatives to improve dietary habits and physical activity are needed to address these health issues.
The prevalence data from our study can be used as benchmarks for comparison with findings from smaller population-specific studies and to track risk factors for chronic diseases over time. Public health efforts to address these important risk factors for diabetes and cardiovascular disease in populations of low socioeconomic status are imperative. For health care professionals, our findings reiterate the importance of screening for other risk factors among patients in whom any component of metabolic syndrome is identified.
Acknowledgements
The authors acknowledge the Manitoba Research Data Centre for providing facilities and equipment to conduct the research.
Natalie Riediger is supported by a Canadian Institutes of Health Research Frederick Banting and Charles Best Canada Graduate Scholarship as well as top-up scholarship funding from the Faculty of Medicine and Department of Community Health Sciences at the University of Manitoba.
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Natalie Riediger conducted the analysis and interpretation of the data and prepared the manuscript. Ian Clara assisted in the analysis of data and revised the article for intellectual content. Both of the authors approved the final version of the manuscript submitted for publication.
Funding: There was no funding for this study.
References
- 1.Denton FT, Spencer BG. Chronic health conditions: changing prevalence in an aging population and some implications for the delivery of health care services. Can J Aging 2010;29:11–21 [DOI] [PubMed] [Google Scholar]
- 2.Haffner SM, Valdez RA, Hazuda HP, et al. Prospective analysis of the insulin-resistance syndrome (syndrome X). Diabetes 1992;41:715–22 [DOI] [PubMed] [Google Scholar]
- 3.Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001;24:683–9 [DOI] [PubMed] [Google Scholar]
- 4.McNeill AM, Rosamond WD, Girman CJ, et al. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care 2005;28:385–90 [DOI] [PubMed] [Google Scholar]
- 5.Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002;288:2709–16 [DOI] [PubMed] [Google Scholar]
- 6.Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome — a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med 2006;23:469–80 [DOI] [PubMed] [Google Scholar]
- 7.Grundy SM, Brewer BH, Cleeman JI, et al. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on Scientific Issues related to definition. Circulation 2004;109:433–8 [DOI] [PubMed] [Google Scholar]
- 8.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/Nation Heart, Lung, and Blood Institute scientific statement. Curr Opin Cardiol 2006;21:1–6 [DOI] [PubMed] [Google Scholar]
- 9.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–421 [PubMed] [Google Scholar]
- 10.Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome. A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120:1640–5 [DOI] [PubMed] [Google Scholar]
- 11.Brien SE, Katzmarzyk PT. Physical activity and the metabolic syndrome in Canada. Appl Physiol Nutr Metab 2006;31:40–7 [DOI] [PubMed] [Google Scholar]
- 12.Bryan SN, St-Denis M, Wojtas D. Canadian Health Measures Survey: clinic operations and logistics. Health Rep 2007;18 (Suppl):53–70 [PubMed] [Google Scholar]
- 13.Tremblay M, Wolfson M, Gorber SC. Canadian Health Measures Survey: rationale, background and overview. Health Rep 2007;18(Suppl):7–20 [PubMed] [Google Scholar]
- 14.Giroux S. Canadian Health Measures Survey: sampling strategy overview. Health Rep 2007;18(Suppl):31–36 [PubMed] [Google Scholar]
- 15.Day B, Langlois R, Temblay M, et al. Canadian Health Measures Survey: ethical, legal and social issues. Health Rep 2007; 18(Suppl):37–52 [PubMed] [Google Scholar]
- 16.Canadian Health Measures Survey cycle 1 data dictionary. Ottawa (ON): Statistics Canada; 2010 [Google Scholar]
- 17.Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among U.S. adults. Diabetes Care 2004; 27:2444–9 [DOI] [PubMed] [Google Scholar]
- 18.Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Natl Health Stat Repors 2009;13:1–7 [PubMed] [Google Scholar]
- 19.Esteghamati A, Meysamie A, Khalilzadeh O, et al. Third national surveillance of risk factors of non-communicable diseases (SuRFNCD-2007) in Iran: methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC Public Health 2009;9;167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erem C, Hacihasanoglu A, Deger O, et al. Prevalence of metabolic syndrome and associated risk factors among Turkish adults: Trabzon MetS study. Endocrine 2008;33:9–20 [DOI] [PubMed] [Google Scholar]
- 21.Julia C, Vernay M, Salanave B, et al. Nutrition patterns and metabolic syndrome: a need for action in young adults (French Nutrition and Health Survey — ENNS, 2006–2007). Prev Med 2010;51:488–93 [DOI] [PubMed] [Google Scholar]
- 22.Marmot MG, Shipley MJ, Rose G. Inequalities in death: Specific explanations of a general pattern? Lancet 1984;1:1003–6 [DOI] [PubMed] [Google Scholar]
- 23.Kavanagh A, Bentley RJ, Turrell G, et al. Socioeconomic position, gender, health behaviours and biomarkers of cardiovascular disease and diabetes. Soc Sci Med 2010;71:1150–60 [DOI] [PubMed] [Google Scholar]
- 24.Loucks EB, Rehkopf DH, Thurston RC, et al. Socioeconomic disparities in metabolic syndrome differ by gender: evidence from NHANES III. Ann Epidemiol 2007;17:19–26 [DOI] [PubMed] [Google Scholar]
- 25.Albert MA, Glynn RJ, Buring J, et al. Impact of traditional and novel risk factors on the relationship between socioeconomic status and incident cardiovascular events. Circulation 2006;114: 2619–26 [DOI] [PubMed] [Google Scholar]
- 26.Chateau-Degat M, Dewailly E, Poirier P, et al. Comparison of diagnostic criteria of the metabolic syndrome in 3 ethnic groups of Canada. Metabolism 2008;57:1526–32 [DOI] [PubMed] [Google Scholar]
- 27.He M, Li ETS, Harris S, et al. Canadian global village reality: Anthropometric surrogate cutoffs and metabolic abnormalities among Canadians of East Asian, South Asian, and European descent. Can Fam Physician 2010;56:e174–82 [PMC free article] [PubMed] [Google Scholar]