Abstract
Cell/tissue biopreservation has broad public health and socio-economic impact affecting millions of lives. Cryopreservation technologies provide an efficient way to preserve cells and tissues targeting the clinic for applications including reproductive medicine and organ transplantation. Among these technologies, vitrification has displayed significant improvement in post-thaw cell viability and function by eliminating harmful effects of ice crystal formation compared to the traditional slow freezing methods. However, high cryoprotectant agent concentrations are required, which induces toxicity and osmotic stress to cells and tissues. It has been shown that vitrification using small sample volumes (i.e., <1 μl) significantly increases cooling rates and hence reduces the required cryoprotectant agent levels. Recently, emerging nano- and micro-scale technologies have shown potential to manipulate picoliter to nanoliter sample sizes. Therefore, the synergistic integration of nanoscale technologies with cryogenics has the potential to improve biopreservation methods.
Keywords: cryopreservation, cryoprotectant agents, droplet vitrification, minimum volume vitrification
Biopreservation refers to extended conservation of cellular life at ultra-low temperatures to store cells and tissues. Cryopreservation has extensive applications in modern medicine, including human fertility preservation [1–4], conservation and transport of cells/tissues for transplantation [5] and storage of cells for tissue regeneration and cell therapy [6–8]. There have been significant efforts to develop cryopreservation techniques and to optimize cryopreservation protocols for various cell and tissue types, such as embryos [9], hepatocytes [10], stem cells [11] and blood vessels [12,13].
During cryopreservation, cells/tissues undergo cooling to sub-zero temperatures at which biological activity is slowed down or completely stopped. At the end of the cryopreservation process, biopreserved cells are thawed, and ideally resume biological activity. During the cryopreservation process, cryoprotectant agents (CPAs) are needed to protect cells from cryoinjury by decreasing the temperature at which intracellular ice formation occurs. CPAs act as osmotic buffers [14–16] and prevent harmful critical electrolyte concentration gradients [17,18]. Moreover, CPAs stabilize cell membranes and maintain macromolecules in their native form [19,20]. Some examples of widely used CPAs include Dimethylsulphoxide (DMSO), 1,2-propanediol (PROH) and ethylene glycol (EG) [21,22], sucrose, trehalose and mannitol.
Slow freezing and vitrification are currently available methods in laboratories and clinics [23]. Slow freezing is an established technique pioneered in the early 1970s, which cryopreserves biological samples at controlled freezing rates to avoid intracellular ice formation and minimizes structural damage to the cell membrane [24] and cytoskeleton [25]. CPAs are used at relatively low concentrations (e.g., 1.5 M) [21] in slow freezing, which has become a standard method for cell and tissue cryopreservation [26–29]. However, cells undergoing slow freezing processes still suffer injury, due to the formation of ice crystals, extreme hyperosmolarity and dehydration [30].
As an alternative cryopreservation method, vitrification offers improved outcomes [23,31–34] by preventing the formation of ice crystals and the increase in ionic strength of unfrozen concentrated solutions [35,36]. Vitrification refers to conversion of the liquid phase directly into a glass-like solid. Vitrification techniques require higher CPA concentrations (e.g., 6–8 M) and higher cooling rates (e.g., −1500°C/min) compared with slow freezing methods. Rapid cooling rates can be achieved by immersing cells/tissues directly into liquid nitrogen (−196°C) or liquid nitrogen vapor (−160°C). High CPA levels used in vitrification lower the freezing point and increase the medium viscosity. However, it is known that these high CPA levels can cause osmotic shock and toxicity to cells resulting in alterations in the cytoskeleton [37–39], spindle disassembly and chromosome dispersal [40].
Minimum sample volume (<1 μl) methods have been developed to reduce the adverse effects of high CPA concentrations needed for vitrification. These methods have been effective to increase the cooling rates and reduce the required CPA levels. These approaches include open pulled straws (OPS) [41], glass capillaries [42], electron microscopy grids (EMGs) [43,44], Cryoloop™ [45], Cryotop [46], gel loading tip [47,48] and droplet-based vitrification [10,49–51]. Even though cryobiological efficacy of minimum volume vitrification methods has been demonstrated, these methods are operationally demanding and require high technical skills limiting their widespread utilization. Recent advances in nano- and micro-scale technologies allow the manipulation of nanoliter sample volumes. Examples include microfluidics for CPA loading/unloading to minimize osmotic shock [52], quartz capillary microchannels as vitrification carriers to increase cooling rates [11,53], and ejector-based droplet generation systems for vitrification of cells at high throughput [10,49,51,54,55]. There are other droplet generation methods including acoustics [51], inkjet [56] and microfluidics [57].
Nano- and micro-scale technologies have already demonstrated the potential to transform modern medicine with alternative approaches in diagnostics, surgical and therapeutic practices [58–61]. These technologies, when applied to biopreservation, could enable the widespread use of minimum volume vitrification approaches in the biopreservation realm. In this article, we describe the existing vitrification-based cryo-preservation approaches with an emphasis on minimum volume droplet-based methods. We highlight the potential applications of these technologies in biopreservation of cells, tissues and tissue-engineered constructs.
Vitrification
The vitrification phenomenon was first described and investigated back in the 1890s [62]. Application of vitrification for cryopreservation with structurally ceased state was not recognized until 1937 by Luyet [63,64]. In vitrification, as the glass transition temperature is reached during cooling, the elevated viscosity of the glass-like solid conserves the natural disorder of molecules existing in liquid and stops all chemical reactions that require molecular diffusion, leading to metabolic inactivity and stability over time [65,66]. Thus, cells/tissues survive the cooling process without significant damage resulting from ice-crystal formation.
Vitrification usually requires addition of high levels of CPAs (permeable and/or nonpermeable) (i.e., 6–8 M) prior to cooling. The use of nonpermeable CPAs, such as sugars (e.g., sucrose and trehalose) and polymers (e.g., polyvinylpyrrolidone and polyvinyl alcohol), can reduce the required permeable CPA concentration and enhance the glass transition process [67–69]. Another strategy is to use stepwise loading of CPAs, in which a pretreatment step with lower concentrations can be employed to minimize the osmotic shock and toxicity [23].
An increase in cooling rate facilitates cells to pass through the phase transition temperature rapidly, thereby decreasing cryoinjury to the cell membrane [70]. In addition, an increase in cooling and warming rates leads to vitrification at lower CPA concentrations, thus alleviating the detrimental toxic and osmotic effects to the cells [71]. To address these challenges, vitrification carrier systems have been developed to increase cooling and warming rates by using minimum volume approaches. However, most minimum volume vitrification systems have low throughput, which fits well with the cryopreservation of reproductive cells (i.e., oocytes) that are collected in small quantities during the clinical process. However, throughput becomes a limitation for vitrification of cells/tissues with larger process volumes, such as whole blood, blood components and stem cells.
Carrier-based vitrification systems
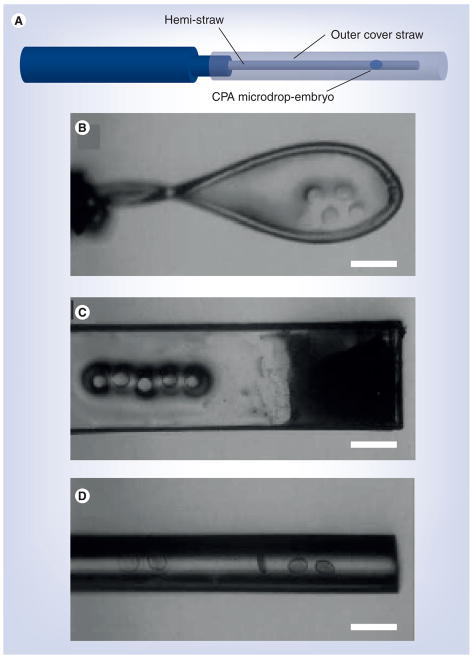
A variety of carrier systems have been developed for vitrification using minimum sample volumes (Table 1) [67,72,73]. Conventional plastic straw is one of the initial vitrification carriers used for cryopreservation of embryos [9], which provides a cooling rate of 2500°C/min and a warming rate of 1300°C/min. However, since this carrier system encompasses a large sample volume (i.e., 45 μl) [74], it is hard to achieve an ultra rapid cooling rate, and high CPA concentrations are required to realize vitrification. To reduce the vitrification sample volume, several other methods have been developed; such as OPS (~1 μl) [41] and hemi-straw systems (~0.3 μl) (Figure 1a) [75]. Using these systems, cryoinjury was reduced as the cooling and warming rates (OPS: 16,700 and 13,900°C/min; hemi-straw: >20,000°C/min) were higher than conventional straws.
Table 1.
Summary of vitrification carrier systems.
| Vitrification carrier | Sample volume/size | Cooling rate (°C/min) | Warming rate (°C/min) | Clinically in use | Ref. |
|---|---|---|---|---|---|
| Conventional straw | 0.25 ml | 2500 | 1300 | Yes | [9] |
| Open pulled straw | ~1 μl | 16,700 | 13,900 | No | [41] |
| Hemi-straw | ~0.3 μl | >20,000 | N/A | No | [75,162] |
| Electron microscopy grid | <1 μl | 150,000 | 150,000 | [43–44] | |
| Cryoloop | 0.7–1.0 mm (inner diameter) | 700,000 | N/A | Yes | [45] |
| Cryotop | <0.1 μl | 23,000 | 42,000 | No | [46] |
| Cryotip | N/A | 12,000 | 24,000 | No | [85] |
| Gel loading tip | 0.6–0.7 μl | No | [47–48] | ||
| Quartz microcapillary | ~3 mm (inner diameter) | 250,000 | N/A | No | [11,53,78] |
| Minimum drop size | 0.1–0.5 μl | 130,000 | N/A | No | [54,99–101] |
| Ejector-based droplet | ~ 1 nl | N/A | N/A | No | [10,49,51,102–104] |
Figure 1. Minimum volume vitrification carriers.
(A) Hemi-straw, which was inserted into a 0.5 ml straw for storage, (B) Cryoloop [48], (C) Cryotop [48] and (D) gel loading tip [48]. Scale bar = 400 μm.
(B–D) Reproduced with permission from [48] © (2011) Elsevier.
Glass capillaries were proposed as a vitrification carrier, offering controllable cooling and warming rates using different diameters. For example, capillaries of 440 μm–2 mm in diameter could provide cooling rates of 12,000–2000°C/min and warming rates of 62,000 to 5000°C/min, respectively [42]. The capillary approach has been applied for cryopreservation of bovine oocytes [42] and embryos [76]. This method resulted in comparable hatching rates compared with those using the OPS technique (glass capillary: 19%; OPS: 27%; control: 80%), suggesting no critical difference in the cooling/warming rates relative to OPS. Closed pulled straws have been developed to avoid potential cross-contamination from direct contact with liquid nitrogen. Improved survival (79%) and spindle morphology conservation [77] have been shown with this method compared with OPS (63%) for the vitrification of mouse oocytes.
Quartz microcapillaries have been recently utilized for vitrification [11,53,78] given that higher heat transfer rates (cooling rate of 250,000°C/min) can be achieved compared to glass and plastic capillaries. In this approach, thin-wall quartz micro capillary (outer diameter: 0.2 mm; wall thickness: 0.01 mm) has led to ultrafast cooling rates of up to 250,000°C/mm [11]. Therefore, this method lowered the CPA levels needed for vitrification. Accordingly, quartz microcapillaries have recently proved to be superior in terms of cell survival (murine embryonic stem cells [11] and mouse oocytes [79]) compared to conventional straws, OPS and EMGs.
Electron microscopy grid was developed to vitrify samples with a volume less than 1 μl, with theoretical cooling and warming rates of approximately 150,000°C/min [43,44]. This system has been used for vitrification of bovine blastocysts [80] and showed similar embryo survival rates compared with nonvitrified blastocysts and an increased hatching rate (68%) compared with plastic straw vitrification (53%). A simplified EMG method has been used for mouse oocytes with survival and fertilization rates of 90.0% and 56.7%, respectively [81].
Cryoloop is one of the most clinically employed approaches to vitrify embryos and oocytes, which has demonstrated increased cell survivability compared to straw-based approaches after thawing [45]. In this approach, the carrier consists of a small nylon loop (0.7–1.0 mm in diameter) mounted on a stainless steel pipe inserted into the lid of a cryovial (Figure 1b). The sample is first placed on the Cryoloop, which has a thin layer of CPA film. The loop is then sealed in a cryovial, which is subsequently filled with liquid nitrogen. Since the sample volume is limited to the loop size, cooling rates as high as 700,000°C/min can be achieved due to the absence of a solid support and the minimum sample volume (<1 μl) that is used [46,82].
Cryotop is a recently developed vitrification approach, which uses a polypropylene strip attached to a holder accompanied with a protective cap (Figure 1C). In this method, sample (<0.1 μl) is loaded with a glass capillary on top of the film strip. Then, the solution is removed, leaving behind a thin layer sufficient to cover the cells to be cryopreserved. The minimum sample volume used for this approach enhances the cooling rate up to 23,000°C/min, and warming rate up to 42,100°C/min [46]. Consequently, the Cryotop method has demonstrated higher efficiency for bovine oocyte vitrification compared to plastic straws and OPS with improved fertilization and blastocyst development, and with higher percentage of typical spindle and chromosome morphology [83,84]. On the other hand, Cryotip constitutes a narrow capillary that can be heat-sealed at both ends after cell loading to provide a closed system. Although lower cooling and warming rates (12,000 and 24,000°C/min, respectively) were reported with this system compared with the Cryotop method, survival of human blastocysts, pregnancy and delivery rates following vitrification did not display a significant difference [85].
In the gel loading tip method, the vitrification solution volume is controlled by the pipette tip size (typically 0.6–0.7 μl) (Figure 1D) [47,48]. Using this vitrification method, the cleavage rate of bovine embryos and rabbit zygotes were lower than the rates achieved by the Cryotop technique [48]. This difference can be attributed to high CPA concentrations and the inferior cooling rates offered by the gel loading tip approach.
Limitations of carrier-based vitrification approaches
Carrier-based minimum volume vitrification systems described here have successfully improved the survivability and functionality of cells undergoing cryopreservation compared with conventional plastic straw systems. However, a major challenge associated with these systems is the need for manual handling, skilled technicians, hence, leading to a low throughput process. Nano- and micro-scale droplet-vitrification offers a carrier-free approach, which involves generation of cell encapsulating CPA droplets followed by direct injection into liquid nitrogen [10]. Since no vitrification carrier or container is needed in this approach, higher cooling and warming rates can be achieved through direct contact with liquid nitrogen. More importantly, recent advances in nano- and micro-droplet generation and ejection technologies allowed effective vitrification of droplets in a continuous manner, which can potentially attain throughput levels required for most biopreservation applications, such as blood cryopreservation [86]. Recent developments in carrier-free, droplet-based vitrification methods are discussed in the next section.
Carrier-free, droplet-based vitrification approaches
Droplet-based vitrification involves loading of samples with vitrification solution, followed by deposition of the solution cell suspension in the form of microdroplets into liquid nitrogen [10,49,52]. Alternatively, droplets are deposited onto a surface with high thermal conductivity (e.g., aluminum), followed by rapid immersion into liquid nitrogen. The main advantage of this technique is the potential to achieve higher cooling and warming rates due to lower heat capacity of a microdroplet at the absence of a bulky carrier. Carrier-free techniques reduce the likelihood of ice crystal formation and reduces the CPA concentrations [49]. Encouraging results have been achieved by droplet-based vitrification techniques with various plant species [87,88]. The promising outcomes achieved with this technology in plant biopreservation have paved the way for applications with mammalian cells, such as oocyte and embryo crypreservation [46,50,89,90].
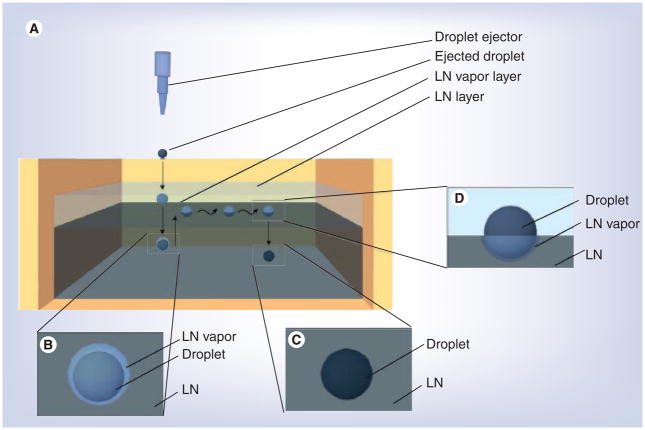
Landa et al. has employed this technique for cryopreservation of mouse embryos [46,89]. In this study, after pre-equilibration in medium with 10% glycerol, embryos in 5–20 μl volume droplets were directly immersed into liquid nitrogen. High survivability (greater than 90%) and developmental potential was demonstrated with eight-cell embryos frozen in microdroplets, in which greater than 83% of embryos developed to blastocysts and more than 73% of embryos underwent implantation after 48 and 96 h of in vitro culture [89]. However, in this study, introducing a droplet (5–20 μl) directly into liquid nitrogen led to the suspension and hovering of the droplet on the surface surrounded by liquid nitrogen vapor blanket (Figure 2), which is known as the Leidenfrost phenomenon [49]. The vapor blanket becomes the bottleneck for effective heat transfer. Despite this drawback, carrier-free vitrification systems can still provide higher heat transfer rates than carrier-based systems, if smaller size droplets are used. Papis [50] and Dhali [90] utilized a similar direct droplet immersion method with reduced vitrification volume (i.e., 6 μl) for bovine oocyte and mouse zygote vitrification, and higher cleavage and blastocyst rates were observed compared with those droplet vitrification methods that used larger droplets. The enhancement in cryopreservation outcomes could be attributed to the increased cooling rates achieved with smaller droplets.
Figure 2. Generation of droplets and levitation of droplets on top of liquid nitrogen.
(A) Experimental setup and the behavior of droplets over time. (B) Droplet swimming in the liquid nitrogen. The droplet in darker color is surrounded by the liquid nitrogen vapor as shown in the schematic drawing. (C) Droplet sunk in the liquid nitrogen. (D) Droplet floating on top of liquid nitrogen.
Reproduced with permission from [49].
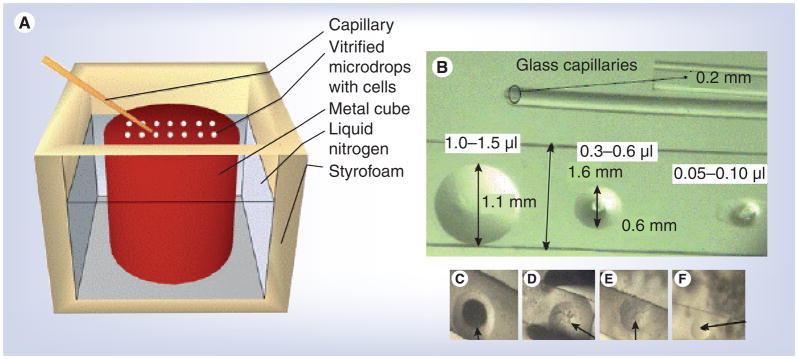
Solid surface vitrification (SSV) [91] method vitrifies droplets without direct contact with liquid nitrogen. In this approach, cells/tissues in a small droplet of CPA solution are placed with pipettes or glass capillaries onto a metal surface (e.g., aluminum foil) cooled by liquid nitrogen or liquid nitrogen vapor (Figure 3a). SSV has been utilized for cryopreservation of in vitro-matured oocytes derived from cattle [92], goat [93] and pig [94,95] by encapsulating 5–10 oocytes in a 1–2 μl droplet of the vitrification solution. However, these studies displayed low rates of developmental competence of vitrified oocytes after activation [92] or IVF [94,96]. In addition, the cleavage rate of vitrified oocytes was reduced (14%) compared with noncryopreserved oocytes (46%), suggesting that damage still existed even though the plasma membrane integrity of the vitrified oocytes was maintained. The decreased developmental competence could be attributed to compromised spindle and/or chromosome configuration caused by vitrification as suggested in previous reports [96,97]. This potential cryoinjury could be resulting from inefficient heat transfer within a relatively bulky droplet that contains 5–10 oocytes. The heat transfer efficiency can be improved by reducing the droplet volume through encapsulating a single oocyte.
Figure 3. Droplet vitrification.
(A) The solid surface vitrification device. A metal cube covered with aluminum foil was partially submerged into liquid nitrogen. Microdroplets of vitrification solution containing the oocytes were dropped onto the cold upper surface of the metal cube and are instantaneously vitrified. (B) The modified minimum drop size technique. Droplets of various sizes were placed on glass cover slips using capillaries. (C–F) Droplets generated by MDS technique during vitrification with (C) ice crystals, (D & E) with fractures, and (F) without crystallization and fractures using CPA concentration reduced by 50% of those used in (C).
Reproduced with permission from [54] © (2010) Elsevier.
Minimizing the volume of vitrification solution containing cells/tissues not only offers the obvious benefit of increasing both cooling and warming rates, but also decreases the likelihood of ice crystal nucleation/formation [98]. Although there is no clear definition of what volume can be defined as ‘minimum’ for vitrification, it usually refers to a volume around, or less than, 1 μl [46]. Based on this principle, Arav et al. [99–101] developed the minimum drop size (MDS) technique, in which nanoliter (0.1–0.5 μl) volumes of vitrification solution was used. The MDS technique has been successfully used to vitrify porcine [99,100] and bovine [101] oocytes, and bovine and sheep embryos [54]. The MDS method was recently modified by depositing 0.1–0.5 μl droplets on glass coverslips followed by immersion into liquid nitrogen or nitrogen slush (Figure 3b). This technique was shown to maximize the cooling rates up to 130,000°C/min, allowing up to a 50% reduction in CPA concentrations compared with conventional vitrification protocols (Figure 3C–3F) [54].
Improved cryopreservation outcomes have been demonstrated with droplet-vitrification methods for oocyte and embryo cryopreservation compared to slow freezing and conventional straw-based vitrification methods with increased survivability and function. However, the labor- and time-intensive procedures often limit the throughput for cell vitrification. In addition, the limited control over the droplet size prevents a uniform size distribution among the generated droplets, which causes inconsistencies in droplet vitrification. Thus, application of the technologies listed above to vitrify cells in a bulk processing volume, such as red blood cells (RBCs), stem cells and hepatocytes, has not been practical.
Recently, Demirci et al. demonstrated ejection-based droplet-vitrification, with which a single to few cells could be encapsulated in reduced droplet volumes (1.5–500 nl) with a negligible reduction in cell viability [10,51]. This droplet generation and ejection technology has been demonstrated to generate droplets at high-throughput with rates up to 1000 droplets per second [10,49,51,102–104]. Moreover, there are other droplet generation technologies that offer extremely small droplet volumes (<1 nl) based on acoustic ejection [51,105–107], which has the capability to generate smaller droplets than the methods described above. Smaller droplets could allow the vitrification to occur at even higher cooling and warming rates than the MDS technique, while using significantly reduced CPA concentrations (~1.5 M), and hence minimizing the osmotic and mechanical stress to cells. It was also experimentally demonstrated that there is a relationship between droplet size and CPA concentrations, suggesting that small droplets vitrify at lower CPA concentrations [10]. With this method, droplets maintain their spherical shape when ejected and dropped into liquid nitrogen. This may provide even cooling of droplets from surface to center compared to other droplet-vitrification approaches discussed above, such as solid surface vitrification, in which hemispheres were generated instead of spheres. Various mammalian cell types (AML-12 hepatocytes, NIH-3T3 fibroblasts, HL-1 cardiomyocytes, mouse embryonic stem cells and RAJI cells) were ejected using droplets with high viability (>89%) after recovery [10,49].
Although most of the minimum volume vitrification approaches were initially designed for cryopreservation of reproductive cells (e.g., embryos and oocytes), advances in biomedical sciences and regenerative medicine will broaden the applications of vitrification technologies to find broad applications, such as preserving high quality cell/tissue sources for transplantation and cell therapy, and extending shelf-life of tissue engineered constructs for tissue regeneration. For future clinical applications, the ejection systems are sterilized and operated in sterile hoods [108,109]. Furthermore, sterile liquid nitrogen can be used to avoid potential contamination [110]. Sterilization of liquid nitrogen has been shown by methods using sterile polytetrafluoroethylene (PTFE) cartridge filteration [111] or ultraviolet (UV) radiation [112].
Applications of vitrification in cryopreservation of cells & tissues
The procedures used to cryopreserve cells or tissues depend on several factors, including cell size, cytoplasm volume and types of cells in the population. Most mammalian cells can be cryopreserved by using the slow-freezing method with a cooling rate of approximately −1°C/min and rapid warming, which results in more than 90% retained cell viability. However, there is a challenge to cryopreserve cells that have a large cytoplasm (e.g., oocytes) due to the harmful effects of intracellular ice crystal formation. There are also challenges associated with cryopreservation of tissues with mixed cell populations of varying sizes, since the optimal freezing procedure for each cell type is different. Thus, cryopreservation methods preserving the utmost cell viability after recovery are desired. As discussed earlier, vitrification has presented great potential to address the particular challenges listed above since it has demonstrated improved viability after both freezing and thawing compared with other methods (Table 2).
Table 2.
Vitrification methods for cell and tissue cryopreservation.
| Cells/tissues | Challenges for cryopreservation | Commonly used vitrification methods | Survival/viability | Limitations | Ref. |
|---|---|---|---|---|---|
| Corneal grafts | Endothelium damage (intracellular freezing at high cooling rates, solution effect injury at low cooling rates) | Nonpermeating CPAs, Teflon-coated bag as vitrification carrier | <10% | CPA toxicity, devitrification during heating process | [163–165] |
| Human embryonic stem cells | Sensitive to CPA, requires extremely critical timing and high degree of skill | OPS (1–20 μl), Glass straw (20–130 μl) | >75% | Time consuming, labor intensive | [12,144] |
| Adult stem cells | Loss of undifferentiated state and viability | OPS | >80% | Time consuming, labor intensive | [12,140,144] |
| Tissue engineered constructs | CPA needs to permeate entire TEC to prevent ice formation | Glass vial | 95% | Organs are too large to be vitrified | [12–13] |
| Chondrocytes/cartilage | CPA concentration required to prevent ice formation | Glass vial | Chondrocytes: 93% Cartilage: 85% |
High thermal processing required to be rapid enough | [12,161] |
| Tissue engineered blood vessels | Stiffening of biomaterials during freezing | CPA concentration >50% (v/v) | 50% | Viability loss during warming | [12–13] |
| Oocytes/zygotes/cleaved embryos | Extremely sensitive to CPAs | OPS, Cryoloops, Cryotop, 0.25 ml straw, EM copper grid, solid surface | Zygotes: 90% survival, 82% cleavage, 30% blastocyst | Hardening of the zona, misalignment of chromosomes | [67,113] |
| Sperm | Sensitive to osmotic shock, large volume | Multi-thermal gradient | 50% decrease in motility | Large sample volume, optimal cooling rate needed | [54,67] |
| Ovarian tissue | Large sample size | Straws or grids | Pyknosis, vacularization, cell swelling detected | Hard to preserve large samples, must be cut into pieces, crystallization during cooling | [67,166] |
CPA: Cryoprotectant agent; EM: Electron microscopy; OPS: Open pulled straws; TEC: Tissue engineered constructs.
Vitrification of reproductive cells
Cryopreservation remains a practical option to preserve and extend human fertility in modern clinical practice [113,114]. Embryo cryopreservation has become a routine procedure in IVF clinics [115]. Patients who might have ethical or religious concerns on embryo freezing potentially consider cryopreservation of oocytes as a viable option. This technology is particularly valuable for cancer patients, offering an opportunity to preserve fertility before chemotherapy or radiation treatment. However, oocytes cryopreserved using slow freezing or traditional vitrification methods have not led to birth rates that are acceptably high for clinical applications after implantation in vivo (<5%) [116,117]. This is mostly due to irreversible damage to oocytes, such as zona hardening and misalignment of the chromosomes [113]. The distinct advantages of vitrification have led to wide investigation for fertility preservation, especially as a possible means to increase oocyte survival, pregnancy and birth rates.
Vitrification of oocytes
Vitrification of bovine, mouse and human oocytes have been studied using various vitrification carrier systems [74,77,118]. Vajta et al. used the OPS method for the vitrification of bovine oocytes, and reported that 50% of the vitrified oocytes cleaved and 25% of them developed into blastocysts after IVF, with pregnancies achieved following transfer at both oocyte and blastocyst stages [41]. Similar survival rates were observed when EMG and Cryoloop approaches were used. However the cleavage rate (EMG: 30%, Cryoloop: 26 vs fresh oocytes: 50–70%) and blastocyst development (EMG: 15 vs fresh oocytes: 40%) after IVF were significantly reduced [44,119]. Morato et al. compared Cryotop to OPS for vitrification of bovine oocytes, and showed that Cryotop was superior to OPS approach yielding higher cleavage (46 vs 32%) and blastocyst rates (5 vs no blastocyst), with uncompromised spindle and chromosome configurations (60 vs 38%) [84]. Higher survival rates and improved conservation of spindle morphology have been achieved with mouse oocytes by using close pulled straws (79 and 93%) rather than conventional straws (77 and 79%), microscopy grids (39 and 95%) and OPS (63 and 89%) [77]. When vitrifying mouse oocytes using electron microscopy grids, significant reduction in hatching rates (39 vs 85% for fresh oocytes) was observed [81]. The Cryoloop approach proved successful in vitrification of mouse oocytes, showing comparable survival, fertilization and blastocyst development rates, intact spindles and similar chromosome morphology to fresh oocytes [120,121]. When quartz microcapillaries were used to vitrify mouse oocytes, similar survival, fertilization and blastocyst development rates to fresh oocytes were observed. However, with this method, when blastocyts derived from vitrified oocytes were transferred to surrogate mothers, lower birth rates were observed (19%) compared with those obtained from fresh oocytes (23%) [79].
In the case of human oocytes, when the OPS method was used for vitrification, high survival and fertilization rates (68.6 and 71.7%) were achieved. However, pregnancy (15.3%) and birth (4.6%) rates were still relatively low [122]. Cryoloop and hemi-straw systems were also tested for vitrification of human oocytes [123], and similar survival rates were observed with these two approaches (81 vs 85%, respectively). Another study [124] using the Cryoloop for vitrification of human oocytes reported similar results with moderate fertilization rate (72%), low pregnancy rates (5–6%), and reduced rates of normal meiotic spindles and chromosomes [125]. On the other hand, encouraging results have been reported with the use of the Cryotop method for human oocyte vitrification, with higher survival (90–99%), fertilization (81–93%) and pregnancy (32–41%) [46,83,113,126] rates. However, there is still need for improvement to achieve higher success rates.
Vitrification of embryos
Early-stage embryos
Vitrification of bovine early-stage embryos was demonstrated using 0.25 ml conventional straws with post-thaw cleavage rates less than 5% [127]. By contrast, higher survival rates and better conservation of normal cell morphology were achieved when OPS (88%) and close pulled straws (85%) were used [128]. For human early-stage embryo vitrification, the hemi-straw method resulted in comparable survival rates with higher development potential than Cryoloop (38 vs 29%) [123]. However, higher survival (85%) and pregnancy (44%) rates were observed in a separate study, which also utilized Cryoloop for vitrification of human embryos leading to births [129]. Successful results were also demonstrated with the Cryotop method for vitrification of early-stage human embryos, with higher levels of survival (100%), cleavage (93%) and blastocyst (52%) rates compared with the results obtained with other approaches detailed above [46].
Blastocysts
Both OPS and EMGs have been used for vitrification of bovine blastocysts. Using OPS, pregnancies were achieved following blastocyst transfer, although low survival rate was observed [41]. When EMGs were used for vitrification of bovine blastocysts, no significant difference was observed in survival rates between vitrified and nonvitrified blastocysts. However, survival rate was reduced 48 h after the vitrification procedure compared with nonvitrified cells (73 vs 84%) [80].
Higher survival rate (82%) was achieved with vitrification of mouse blastocysts using OPS compared with conventional plastic straw method (69%) [130], which can be attributed to reduced vitrification volume of OPS. On the other hand, closed pulled straws showed higher pregnancy and birth rates (70 and 45%) compared with the OPS (20 and 8%) and conventional straws (10 and 5%) obtained after transferring vitrified expanded blastocysts to the uterus of a pseudo pregnant mouse [131]. The Cryoloop approach also resulted in high implantation (80%) and fetal development (55%) rates of vitrified mouse blastocysts after being transferred to pseudopregnant recipients, which were comparable to those observed with nonvitrified cells [45].
A number of approaches have been used for vitrification of human blastocysts, including EMGs, hemi-straw, Cryoloop and Cryotop. EMGs yielded high survival (83–90%), hatching (49%), implantation (29%) and pregnancy rates (34–48%) [132,133], which were comparable to those obtained using Cryoloop [45,134–137] and Cryotop [46,138] (90 and 53% for survival and pregnancy rates, respectively). The results obtained using the hemi-straw method resulted in lower survival, hatching (19%), implantation (13%) and pregnancy (19%) rates compared with other approaches described above [75].
Vitrification of oocytes and embryos using various minimum volume carriers all showed improvements compared with conventional straws. However, it should be noted that the results achieved with these methods are highly dependent on the skills of the embryologist, and hence comparisons between different studies have to take this as a consideration for future biopreservation technologies. The variations due to manual processes could potentially be eliminated, if automated systems are applied. It should also be noted that the efficiencies of these methods depend on the species and developmental stages of embryos in preservation.
Vitrification of stem cells
Regenerative medicine has shown potential to repair or replace tissue/organ function lost due to disease, damage or congenital defects [139]. The strategies presently under development include transplantation of stem cells, manipulation of a patient’s own stem cells, and the use of scaffold materials that provide biochemical signals to stimulate stem cells to start differentiation. Therefore, it is crucial to be able to preserve stem cells for future regenerative therapies.
Biopreservation of stem cell lines is often challenging due to the difficulty in conservation of undifferentiated phenotypes through cycles of cell division. Hence, it is hard to provide persistent and qualified cell sources for clinical use [140]. Cryopreservation provides an affordable, fast, and efficient solution for stem cell banking for both research and clinical use. Vitrification has been successfully used to preserve various types of stem cells, such as embryonic stem cells [141], mesenchymal stem cells [142] and hemopoietic stem cells [143]. Current vitrification protocols for stem cells consist of stepwise addition of vitrification solution to minimize osmotic shock, in which a small volume of the CPA solution and cells are immersed directly into liquid nitrogen. Upon warming, a series of stepwise dilutions is sufficient to completely remove the vitrification solution. After vitrification, cell viability in higher than 80% was achieved [144]. On the other hand, cryopreservation of stem cells using slow freezing resulted in a survival rate of only 10% [140].
Both Cryotip and quartz microcapillaries have been tested for the vitrification of mouse embryonic stem cells. When Cryotip approach was used, more than 99% of the cells survived after warming [145]. By using the quartz micro-capillary approach, murine embryonic stem cells were successfully cryopreserved without compromising their undifferentiated phenotype expression postvitrification [11]. OPS approach was used to vitrify human embryonic stem cells derived from the inner cell mass of human blastocysts [146,147]. The achieved cell attachment postwarming was comparable to those of nonvitrified stem cells, although a small percentage of nonspecific differentiation was observed (24%). However, the pluripotency of stem cells was retained after warming [147]. The efficiency of other vitrification approaches for human embryonic stem cell preservation needs further investigation.
Vitrification approaches used for stem cell cryopreservation discussed above are time consuming and require a high level of skill to prevent cell loss. In addition, given the large number of cells to be preserved, a high throughput approach is needed. Therefore, the ejector-based carrier-free droplet-vitrification technique described above could be a suitable candidate technology for stem cell vitrification with its high-throughput processing capability and the use of lower CPA concentrations with small droplet size.
Vitrification of tissue engineered constructs
Tissue engineering technologies have the potential to develop regenerative therapies for currently incurable diseases and untreatable conditions, such as diabetes, heart disease, renal failure, osteoporosis and spinal cord injuries [148–153]. The ability to cryogenically preserve tissue engineered constructs (TECs) would be indispensable for successfully transferring replacement tissues from the laboratory setting to the clinic. This would allow distributing cell-based products to patients on a demand basis by increasing the shelf life of the products.
With the recent developments in cryogenic science, cryopreservation of tissues and TECs for extended periods of time has become achievable. The tissues that have been found incompatible with freezing protocols are generally highly vascularized due to endothelium damage. So far, animal intestines and ovaries have been successfully recovered from the cryopreservation process, showing function after transplantation. The primary issue with tissue and TEC cryopreservation is preventing ice crystal formation and maintaining the integrity and mechanical properties of both the cells and extracellular matrix (ECM) during cooling and thawing steps. In addition, dehydration that occurs during the freezing process results in a stiffer tissue due to increased crosslinking between collagen fibers [140]. Thus, slow freezing is not optimal for cryopreservation of tissues or TECs due to the difficulties in preserving the structural stability of biomaterials and regenerative tissue integrity during liquid-ice phase transition. Vitrification appears to be a more promising modality for TEC cryopreservation, since it can maintain tissue integrity by preventing ice crystal formation [140].
Vitrification of various TECs, such as tissue engineered (TE) bones (TEBs) [154], TE pancreatic substitutes (TEPS) [155,156], and TE blood vessels (TEBVs) [157], have shown encouraging results. Song et al. demonstrated the vitrification of TEPS using DMSO and 1,2-propanediol, showing comparable results with the nonfrozen control [156]. In the case of TE cartilage cryopreservation, chondrocytes showed survival rates of up to 93% after vitrification [158]. Similarly, vitrification of rabbit cartilage has resulted in high viability (>80%) after thawing [159]. In addition, improved cryopreservation outcomes were observed by vitrification of native vascular tissues compared to those by slow freezing [160,161]. More than 80% of the maximum contractions were maintained in vitrified vessels with similar responses to drug stimulation, while less than 30%, were retained in frozen vessels [160]. In a separate study, a vitrification solution consisting of DMSO, propylene glycol and formamide was used for a collagen-based TEBVs, and negligible ice formation was observed. By contrast, extensive ice formation was observed in frozen specimens using the slow freezing method. Thus, vitrification seems to be an appropriate approach for TEBV cryopreservation. However, a similar reduction in viability was observed in both frozen and vitrified constructs (38 vs 39%) compared with fresh samples (63%) [140].
Compared with slow freezing, enhanced outcomes have been shown for TEC cryopreservation using vitrification. However, challenges still exist with current existing approaches. For instance, it is not practical to achieve ultra-rapid vitrification using minimum volume approaches given the large TEC size, and high CPA concentrations have to be used for vitrification to occur. Moreover, it is important to ensure that vitrification solution is present throughout the construct and cells. Additionally, toxicity and cellular osmotic shock of high levels of CPAs is another challenge for TEC vitrification, so it is necessary to minimize CPA concentrations to reduce damage to cells. Furthermore, optimizing protocols for CPA removal is also vital to avoid devitrification since construct viability has been found to decrease during the warming process [13].
Conclusion & future perspective
In this article, we presented the minimum volume vitrification approaches and their applications in medicine. Minimum volume vitrification approaches reduce CPA concentrations required for vitrification since they can attain increased cooling and warming rates. Hence, this process enables reduced toxicity and osmotic shock to cells and tissues that undergo cryopreservation processes. Among these methods, droplet-vitrification offers further potential advantages, allowing vitrification at even higher cooling rates using smaller droplet sizes. However, challenges still remain, such as throughput limitations and demand for skilled operators. Therefore, future research efforts need to focus on improving current vitrification approaches by developing novel vitrification systems that can minimize both the dependence on skilled operators as well as variations due to manual handling process steps. Emerging nano- and micro-scale technologies enable sample manipulation in small scales. The successful integration of these technologies with the current know-how in cryobiology has the potential to address these needs by offering automation and high throughput operation in biopreservation, leading to an increase in successful clinical biopreservation outcomes.
Executive summary.
Existing and emerging applications of vitrification include cryopreservation of reproductive cells, stem cells, blood and tissue engineered constructs.
Vitrification displays significant improvement in post-thaw cell viability and function compared with the traditional slow freezing methods by eliminating ice crystal formation.
Vitrification using minimum sample volume enables increased cooling and warming rates and the utilization of lower cryoprotectant agent concentrations, thus reducing toxicity and osmotic shock to cells/tissues.
Minimum volume vitrification systems are divided into two categories: carrier-based and carrier-free (droplet-based vitrification) systems.
Droplet-based vitrification offers potential advantages over carrier-based vitrification methods, allowing vitrification at even higher cooling rates using smaller sample sizes.
Emerging nano- and micro-scale technologies have the potential to improve throughput limitations and reduce skill dependence of the current vitrification systems by enabling sample manipulation in a small scale.
Footnotes
For reprint orders, please contact: reprints@futuremedicine.com
Financial & competing interests disclosure
P Catalano would like to thank the Fulbright Scholar Program for partially supporting his postdoctoral fellowship in Bio-Acoustic-MEMS in Medicine (BAMM) Laboratory, Center for Bioengineering, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA. This work was supported by NIH R21 HL095960. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Bibliography
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- 1▪▪.Tao T, Zhang W, Del Valle A. Human oocyte cryopreservation. Curr Opin Obstet Gynecol. 2009;21(3):247–252. doi: 10.1097/GCO.0b013e328329c2d2. Summarizes the clinical breakthroughs in human oocyte cryopreservation and emphasizes on the role of vitrification methods. [DOI] [PubMed] [Google Scholar]
- 2.Dunn L, Fox KR. Techniques for fertility preservation in patients with breast cancer. Curr Opin Obstet Gynecol. 2009;21(1):68–73. doi: 10.1097/GCO.0b013e32831e13b9. [DOI] [PubMed] [Google Scholar]
- 3.Tulandi T, Huang JY, Tan SL. Preservation of female fertility: an essential progress. Obstet Gynecol. 2008;112(5):1160–1172. doi: 10.1097/AOG.0b013e31818bba31. [DOI] [PubMed] [Google Scholar]
- 4.Krausz C, Forti G. Sperm cryopreservation in male infertility due to genetic disorders. Cell Tissue Bank. 2006;7(2):105–112. doi: 10.1007/s10561-005-1967-9. [DOI] [PubMed] [Google Scholar]
- 5.Ishine N, Rubinsky B, Lee CY. Transplantation of mammalian livers following freezing: vascular damage and functional recovery. Cryobiology. 2000;40(1):84–89. doi: 10.1006/cryo.1999.2225. [DOI] [PubMed] [Google Scholar]
- 6.Schneider RK, Neuss S, Knuchel R, Perez-Bouza A. Mesenchymal stem cells for bone tissue engineering. Pathologe. 2010;31(Suppl 2):138–146. doi: 10.1007/s00292-010-1329-7. [DOI] [PubMed] [Google Scholar]
- 7.Watt SM, Austin E, Armitage S. Cryopreservation of hematopoietic stem/progenitor cells for therapeutic use. Methods Mol Biol. 2007;368:237–259. doi: 10.1007/978-1-59745-362-2_17. [DOI] [PubMed] [Google Scholar]
- 8.Dieckmann C, Renner R, Milkova L, Simon JC. Regenerative medicine in dermatology: biomaterials, tissue engineering, stem cells, gene transfer and beyond. Exp Dermatol. 2010;19(8):697–706. doi: 10.1111/j.1600-0625.2010.01087.x. [DOI] [PubMed] [Google Scholar]
- 9▪.Rall WF, Fahy GM. Ice-free cryopreservation of mouse embryos at −196 degrees C by vitrification. Nature. 1985;313(6003):573–575. doi: 10.1038/313573a0. Vitrification for the first time was employed for embryo cryopreservation. [DOI] [PubMed] [Google Scholar]
- 10▪▪.Demirci U, Montesano G. Cell encapsulating droplet vitrification. Lab Chip. 2007;7(11):1428–1433. doi: 10.1039/b705809h. Highlights for the first time that droplet vitrification can be achieved at high throughput. [DOI] [PubMed] [Google Scholar]
- 11.He X, Park EY, Fowler A, Yarmush ML, Toner M. Vitrification by ultra-fast cooling at a low concentration of cryoprotectants in a quartz micro-capillary: a study using murine embryonic stem cells. Cryobiology. 2008;56(3):223–232. doi: 10.1016/j.cryobiol.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hunt CJ, Timmons PM. Cryopreservation of human embryonic stem cell lines. Methods Mol Biol. 2007;368:261–270. doi: 10.1007/978-1-59745-362-2_18. [DOI] [PubMed] [Google Scholar]
- 13.Brockbank KGM, Walsh JR, Song YC, Taylor MJ, editors. Vitrification: Preservation of Cellular Implants. Marcel Dekker; NY, USA: 2003. [Google Scholar]
- 14.Somero GN. Protons, osmolytes, fitness of internal milieu for protein function. Am J Physiol. 1986;251(2 Pt 2):R197–213. doi: 10.1152/ajpregu.1986.251.2.R197. [DOI] [PubMed] [Google Scholar]
- 15.Singer MA, Lindquist S. Thermotolerance in Saccharomyces cerevisiae: the Yin and Yang of trehalose. Trends Biotechnol. 1998;16(11):460–468. doi: 10.1016/s0167-7799(98)01251-7. [DOI] [PubMed] [Google Scholar]
- 16.Wright DL, Eroglu A, Toner M, Toth TL. Use of sugars in cryopreserving human oocytes. Reprod Biomed Online. 2004;9(2):179–186. doi: 10.1016/s1472-6483(10)62127-x. [DOI] [PubMed] [Google Scholar]
- 17.Mazur P. Freezing of living cells: mechanisms and implications. Am J Physiol. 1984;247(3 Pt 1):C125–142. doi: 10.1152/ajpcell.1984.247.3.C125. [DOI] [PubMed] [Google Scholar]
- 18.Meryman HT. Cryoprotective agents. Cryobiology. 1971;8(2):173–183. doi: 10.1016/0011-2240(71)90024-1. [DOI] [PubMed] [Google Scholar]
- 19.Crowe JH, Crowe LM, Carpenter JF, et al. Interactions of sugars with membranes. Biochim Biophys Acta. 1988;947(2):367–384. doi: 10.1016/0304-4157(88)90015-9. [DOI] [PubMed] [Google Scholar]
- 20.Anchordoguy TJ, Rudolph AS, Carpenter JF, Crowe JH. Modes of interaction of cryoprotectants with membrane phospholipids during freezing. Cryobiology. 1987;24(4):324–331. doi: 10.1016/0011-2240(87)90036-8. [DOI] [PubMed] [Google Scholar]
- 21.Tao T, Del Valle A. Human oocyte and ovarian tissue cryopreservation and its application. J Assist Reprod Genet. 2008;25(7):287–296. doi: 10.1007/s10815-008-9236-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Picton HM, Kim SS, Gosden RG. Cryopreservation of gonadal tissue and cells. Br Med Bull. 2000;56(3):603–615. doi: 10.1258/0007142001903418. [DOI] [PubMed] [Google Scholar]
- 23.Chen SU, Yang YS. Slow freezing or vitrification of oocytes: their effects on survival and meiotic spindles, the time schedule for clinical practice. Taiwan J Obstet Gynecol. 2009;48(1):15–22. doi: 10.1016/S1028-4559(09)60030-9. [DOI] [PubMed] [Google Scholar]
- 24.Desrosiers P, Legare C, Leclerc P, Sullivan R. Membranous and structural damage that occur during cryopreservation of human sperm may be time-related events. Fertil Steril. 2006;85(6):1744–1752. doi: 10.1016/j.fertnstert.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 25.Fabbri R, Porcu E, Marsella T, Rocchetta G, Venturoli S, Flamigni C. Human oocyte cryopreservation: new perspectives regarding oocyte survival. Hum Reprod. 2001;16(3):411–416. doi: 10.1093/humrep/16.3.411. [DOI] [PubMed] [Google Scholar]
- 26.Boldt J, Tidswell N, Sayers A, Kilani R, Cline D. Human oocyte cryopreservation: 5-year experience with a sodium-depleted slow freezing method. Reprod Biomed Online. 2006;13(1):96–100. doi: 10.1016/s1472-6483(10)62021-4. [DOI] [PubMed] [Google Scholar]
- 27.Chen SU, Lien YR, Chen HF, Chang LJ, Tsai YY, Yang YS. Observational clinical follow-up of oocyte cryopreservation using a slow-freezing method with 1,2-propanediol plus sucrose followed by ICSI. Hum Reprod. 2005;20(7):1975–1980. doi: 10.1093/humrep/deh884. [DOI] [PubMed] [Google Scholar]
- 28.Ware CB, Nelson AM, Blau CA. Controlled-rate freezing of human ES cells. Biotechniques. 2005;38(6):879–880. 882–873. doi: 10.2144/05386ST01. [DOI] [PubMed] [Google Scholar]
- 29.Chi HJ, Koo JJ, Kim MY, Joo JY, Chang SS, Chung KS. Cryopreservation of human embryos using ethylene glycol in controlled slow freezing. Hum Reprod. 2002;17(8):2146–2151. doi: 10.1093/humrep/17.8.2146. [DOI] [PubMed] [Google Scholar]
- 30.Gratwohl A. Thomas’ hematopoietic cell transplantation. Eur J Haematol. 2010;84(1):95. doi: 10.1111/j.1600-0609.2009.01360.x. [DOI] [PubMed] [Google Scholar]
- 31.Vajta G, Nagy ZP. Are programmable freezers still needed in the embryo laboratory? Review on vitrification. Reprod Biomed Online. 2006;12(6):779–796. doi: 10.1016/s1472-6483(10)61091-7. [DOI] [PubMed] [Google Scholar]
- 32.Keskintepe L, Sher G, Machnicka A, et al. Vitrification of human embryos subjected to blastomere biopsy for pre-implantation genetic screening produces higher survival and pregnancy rates than slow freezing. J Assist Reprod Genet. 2009;26(11–12):629–635. doi: 10.1007/s10815-009-9369-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stehlik E, Stehlik J, Katayama KP, et al. Vitrification demonstrates significant improvement versus slow freezing of human blastocysts. Reprod Biomed Online. 2005;11(1):53–57. doi: 10.1016/s1472-6483(10)61298-9. [DOI] [PubMed] [Google Scholar]
- 34.Fadini R, Brambillasca F, Renzini MM, et al. Human oocyte cryopreservation: comparison between slow and ultrarapid methods. Reprod Biomed Online. 2009;19(2):171–180. doi: 10.1016/s1472-6483(10)60069-7. [DOI] [PubMed] [Google Scholar]
- 35.Fahy GM, MacFarlane DR, Angell CA, Meryman HT. Vitrification as an approach to cryopreservation. Cryobiology. 1984;21(4):407–426. doi: 10.1016/0011-2240(84)90079-8. [DOI] [PubMed] [Google Scholar]
- 36.Rayos AA, Takahashi Y, Hishinuma M, Kanagawa H. Quick freezing of unfertilized mouse oocytes using ethylene glycol with sucrose or trehalose. J Reprod Fertil. 1994;100(1):123–129. doi: 10.1530/jrf.0.1000123. [DOI] [PubMed] [Google Scholar]
- 37.Vincent C, Johnson MH. Cooling, cryoprotectants, the cytoskeleton of the mammalian oocyte. Oxf Rev Reprod Biol. 1992;14:73–100. [PubMed] [Google Scholar]
- 38.Vincent C, Garnier V, Heyman Y, Renard JP. Solvent effects on cytoskeletal organization and in-vivo survival after freezing of rabbit oocytes. J Reprod Fertil. 1989;87(2):809–820. doi: 10.1530/jrf.0.0870809. [DOI] [PubMed] [Google Scholar]
- 39.Joly C, Bchini O, Boulekbache H, Testart J, Maro B. Effects of 1,2-propanediol on the cytoskeletal organization of the mouse oocyte. Hum Reprod. 1992;7(3):374–378. doi: 10.1093/oxfordjournals.humrep.a137654. [DOI] [PubMed] [Google Scholar]
- 40.Saunders KM, Parks JE. Effects of cryopreservation procedures on the cytology and fertilization rate of in vitro-matured bovine oocytes. Biol Reprod. 1999;61(1):178–187. doi: 10.1095/biolreprod61.1.178. [DOI] [PubMed] [Google Scholar]
- 41.Vajta G, Holm P, Kuwayama M, et al. Open pulled straw (OPS) vitrification: a new way to reduce cryoinjuries of bovine ova and embryos. Mol Reprod Dev. 1998;51(1):53–58. doi: 10.1002/(SICI)1098-2795(199809)51:1<53::AID-MRD6>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 42.Hochi S, Akiyama M, Minagawa G, Kimura K, Hanada A. Effects of cooling and warming rates during vitrification on fertilization of in vitro-matured bovine oocytes. Cryobiology. 2001;42(1):69–73. doi: 10.1006/cryo.2001.2298. [DOI] [PubMed] [Google Scholar]
- 43.Steponkus PL, Myers SP, Lynch DV, et al. Cryopreservation of Drosophila melanogaster embryos. Nature. 1990;345(6271):170–172. doi: 10.1038/345170a0. [DOI] [PubMed] [Google Scholar]
- 44.Martino A, Songsasen N, Leibo SP. Development into blastocysts of bovine oocytes cryopreserved by ultra-rapid cooling. Biol Reprod. 1996;54(5):1059–1069. doi: 10.1095/biolreprod54.5.1059. [DOI] [PubMed] [Google Scholar]
- 45▪▪.Lane M, Schoolcraft WB, Gardner DK. Vitrification of mouse and human blastocysts using a novel Cryoloop container-less technique. Fertil Steril. 1999;72(6):1073–1078. doi: 10.1016/s0015-0282(99)00418-5. Cryoloop was used successfully for the first time in cryopreservation of both mouse and human embryos. [DOI] [PubMed] [Google Scholar]
- 46.Kuwayama M. Highly efficient vitrification for cryopreservation of human oocytes and embryos: the Cryotop method. Theriogenology. 2007;67(1):73–80. doi: 10.1016/j.theriogenology.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 47.Tominaga K. Cryopreservation and sexing of in vivo- and in vitro-produced bovine embryos for their practical use. J Reprod Dev. 2004;50(1):29–38. doi: 10.1262/jrd.50.29. [DOI] [PubMed] [Google Scholar]
- 48.Hochi S, Terao T, Kamei M, Kato M, Hirabayashi M, Hirao M. Successful vitrification of pronuclear-stage rabbit zygotes by minimum volume cooling procedure. Theriogenology. 2004;61(2–3):267–275. doi: 10.1016/s0093-691x(03)00232-2. [DOI] [PubMed] [Google Scholar]
- 49▪▪.Song YS, Adler D, Xu F, et al. Vitrification and levitation of a liquid droplet on liquid nitrogen. Proc Natl Acad Sci USA. 2010;107(10):4596–4600. doi: 10.1073/pnas.0914059107. Theoretically demonstrates the simultaneous occurrence of levitation of droplets on liquid nitrogen (Leidenfrost phenomenon) during vitrification. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Papis K, Shimizu M, Izaike Y. Factors affecting the survivability of bovine oocytes vitrified in droplets. Theriogenology. 2000;54(5):651–658. doi: 10.1016/S0093-691X(00)00380-0. [DOI] [PubMed] [Google Scholar]
- 51.Demirci U, Montesano G. Single cell epitaxy by acoustic picolitre droplets. Lab Chip. 2007;7(9):1139–1145. doi: 10.1039/b704965j. [DOI] [PubMed] [Google Scholar]
- 52.Song YS, Moon S, Hulli L, Hasan SK, Kayaalp E, Demirci U. Microfluidics for cryopreservation. Lab Chip. 2009;9(13):1874–1881. doi: 10.1039/b823062e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Risco R, Elmoazzen H, Doughty M, He X, Toner M. Thermal performance of quartz capillaries for vitrification. Cryobiology. 2007;55(3):222–229. doi: 10.1016/j.cryobiol.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 54.Arav A, Yavin S, Zeron Y, Natan D, Dekel I, Gacitua H. New trends in gamete’s cryopreservation. Mol Cell Endocrinol. 2002;187(1–2):77–81. doi: 10.1016/s0303-7207(01)00700-6. [DOI] [PubMed] [Google Scholar]
- 55.Samot J, Sangjun M, Shao L, et al. Blood banking in living droplets. PLoS ONE. 2011;6(3):e17530. doi: 10.1371/journal.pone.0017530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Merrin J, Leibler S, Chuang JS. Printing multistrain bacterial patterns with a piezoelectric inkjet printer. PloS ONE. 2007;2(7):7. doi: 10.1371/journal.pone.0000663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abate AR, Hung T, Mary P, Agresti JJ, Weitz DA. High-throughput injection with microfluidics using picoinjectors. Proc Natl Acad Sci USA. 2010;107(45):19163–19166. doi: 10.1073/pnas.1006888107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Emerich DF, Thanos CG. Nanotechnology and medicine. Expert Opin Biol Ther. 2003;3(4):655–663. doi: 10.1517/14712598.3.4.655. [DOI] [PubMed] [Google Scholar]
- 59.Wilkinson JM. Nanotechnology applications in medicine. Med Device Technol. 2003;14(5):29–31. [PubMed] [Google Scholar]
- 60.Polla DL, Erdman AG, Robbins WP, et al. Microdevices in medicine. Annu Rev Biomed Eng. 2000;2:551–576. doi: 10.1146/annurev.bioeng.2.1.551. [DOI] [PubMed] [Google Scholar]
- 61.Angeli E, Buzio R, Firpo G, et al. Nanotechnology applications in medicine. Tumori. 2008;94(2):206–215. doi: 10.1177/030089160809400213. [DOI] [PubMed] [Google Scholar]
- 62.Tammann G. Ueber die abhangkeit der Zahl der Kernr, welche sich in verschiedenen underkuhlten flussigkeiten bilden, von der temperatur. Z Phys Chem. 1898;25:39. [Google Scholar]
- 63.Luyet BJ. The vitrification of organic colloids and of protoplasm. Biodynamica. 1937;1:14. [Google Scholar]
- 64.Luyet BJ, Gehenio PM, editors. Life and Death at Low Temperatures. Biodynamica; Normandy, MI, USA: 1940. [Google Scholar]
- 65▪.Wowk B. Thermodynamic aspects of vitrification. Cryobiology. 2010;60(1):11–22. doi: 10.1016/j.cryobiol.2009.05.007. Describes thermodynamic behavior during vitrification process. [DOI] [PubMed] [Google Scholar]
- 66.Leopold AC, editor. Membranes, Metabolism, Dry Organisms. Cornell University Press; Ithaca, NY, USA: 1986. [Google Scholar]
- 67.Liebermann J, Nawroth F, Isachenko V, Isachenko E, Rahimi G, Tucker MJ. Potential importance of vitrification in reproductive medicine. Biol Reprod. 2002;67(6):1671–1680. doi: 10.1095/biolreprod.102.006833. [DOI] [PubMed] [Google Scholar]
- 68.Chen SU, Yang YS. Vitrification of oocytes: various procedures. In: Tucker MJ, Liebermann J, editors. Vitrification in Assisted Reproduction: A User’s Manual and Troubleshooting Guide. Informa Healthcare; London, UK: 2007. pp. 129–144. [Google Scholar]
- 69.Wang HY, Lu SS, Lun ZR. Glass transition behavior of the vitrification solutions containing propanediol, dimethyl sulfoxide and polyvinyl alcohol. Cryobiology. 2009;58(1):115–117. doi: 10.1016/j.cryobiol.2008.10.131. [DOI] [PubMed] [Google Scholar]
- 70.Ghetler Y, Yavin S, Shalgi R, Arav A. The effect of chilling on membrane lipid phase transition in human oocytes and zygotes. Hum Reprod. 2005;20(12):3385–3389. doi: 10.1093/humrep/dei236. [DOI] [PubMed] [Google Scholar]
- 71.Katkov II, Isachenko V, Isachenko E. Vitrification in small quenched volumes with a minimal amount of, or without vitrificants: basic biophysics and thermodynamics. In: Tucker MJ, Liebermann J, editors. Vitrification in Assisted Reproduction: A User’s Manual and Trouble-shooting Guide. Informa Healthcare; London, UK: 2007. pp. 21–32. [Google Scholar]
- 72.Wusteman MC, Pegg DE, Robinson MP, Wang LH, Fitch P. Vitrification media: toxicity, permeability, dielectric properties. Cryobiology. 2002;44(1):24–37. doi: 10.1016/S0011-2240(02)00002-0. [DOI] [PubMed] [Google Scholar]
- 73.Kattera S, Chen C. Cryopreservation of embryos by vitrification: current development. Int Surg. 2006;91(5 Suppl):S55–62. [PubMed] [Google Scholar]
- 74.Chen SU, Lien YR, Chen HF, Chao KH, Ho HN, Yang YS. Open pulled straws for vitrification of mature mouse oocytes preserve patterns of meiotic spindles and chromosomes better than conventional straws. Hum Reprod. 2000;15(12):2598–2603. doi: 10.1093/humrep/15.12.2598. [DOI] [PubMed] [Google Scholar]
- 75.Vanderzwalmen P, Bertin G, Debauche C, et al. Vitrification of human blastocysts with the Hemi-Straw carrier: application of assisted hatching after thawing. Hum Reprod. 2003;18(7):1504–1511. doi: 10.1093/humrep/deg298. [DOI] [PubMed] [Google Scholar]
- 76.Rios GL, Mucci NC, Kaiser GG, Alberio RH. Effect of container, vitrification volume and warming solution on cryosurvival of in vitro-produced bovine embryos. Anim Reprod Sci. 2010;118(1):19–24. doi: 10.1016/j.anireprosci.2009.06.015. [DOI] [PubMed] [Google Scholar]
- 77.Chen SU, Lien YR, Cheng YY, Chen HF, Ho HN, Yang YS. Vitrification of mouse oocytes using closed pulled straws (CPS) achieves a high survival and preserves good patterns of meiotic spindles, compared with conventional straws, open pulled straws (OPS) and grids. Hum Reprod. 2001;16(11):2350–2356. doi: 10.1093/humrep/16.11.2350. [DOI] [PubMed] [Google Scholar]
- 78.Arav A, Zeron Y, Ocheretny A. new device and method for vitrification increases the cooling rate and allows successful cryopreservation of bovine oocytes. Theriogenology. 2000;53:2. [Google Scholar]
- 79.Lee HJ, Elmoazzen H, Wright D, et al. Ultra-rapid vitrification of mouse oocytes in low cryoprotectant concentrations. Reprod Biomed Online. 2010;20(2):201–208. doi: 10.1016/j.rbmo.2009.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Park SP, Kim EY, Kim DI, et al. Simple, efficient and successful vitrification of bovine blastocysts using electron microscope grids. Hum Reprod. 1999;14(11):2838–2843. doi: 10.1093/humrep/14.11.2838. [DOI] [PubMed] [Google Scholar]
- 81.Kim SH, Ku SY, Sung KC, et al. Simplified EM grid vitrification is a convenient and efficient method for mouse mature oocyte cryopreservation. Yonsei Med J. 2006;47(3):399–404. doi: 10.3349/ymj.2006.47.3.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Isachenko E, Isachenko V, Katkov II, Dessole S, Nawroth F. Vitrification of mammalian spermatozoa in the absence of cryoprotectants: from past practical difficulties to present success. Reprod Biomed Online. 2003;6(2):191–200. doi: 10.1016/s1472-6483(10)61710-5. [DOI] [PubMed] [Google Scholar]
- 83.Kuwayama M, Vajta G, Kato O, Leibo SP. Highly efficient vitrification method for cryopreservation of human oocytes. Reprod Biomed Online. 2005;11(3):300–308. doi: 10.1016/s1472-6483(10)60837-1. [DOI] [PubMed] [Google Scholar]
- 84.Morato R, Izquierdo D, Paramio MT, Mogas T. Cryotops versus open-pulled straws (OPS) as carriers for the cryopreservation of bovine oocytes: effects on spindle and chromosome configuration and embryo development. Cryobiology. 2008;57(2):137–141. doi: 10.1016/j.cryobiol.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 85.Kuwayama M, Vajta G, Ieda S, Kato O. Comparison of open and closed methods for vitrification of human embryos and the elimination of potential contamination. Reprod Biomed Online. 2005;11(5):608–614. doi: 10.1016/s1472-6483(10)61169-8. [DOI] [PubMed] [Google Scholar]
- 86.Scott KL, Lecak J, Acker JP. Biopreservation of red blood cells: past, present, future. Transf Med Rev. 2005;19(2):127–142. doi: 10.1016/j.tmrv.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 87.Kim HH, Lee JK, Yoon JW, et al. Cryopreservation of garlic bulbil primordia by the droplet-vitrification procedure. Cryo Lett. 2006;27(3):143–153. [PubMed] [Google Scholar]
- 88.Gallard A, Panis B, Dorion N, Swennen R, Grapin A. Cryopreservation of Pelargonium apices by droplet-vitrification. Cryo Lett. 2008;29(3):243–251. [PubMed] [Google Scholar]
- 89.Landa V, Tepla O. Cryopreservation of mouse 8-cell embryos in microdrops. Folia Biol (Praha) 1990;36(3–4):153–158. [PubMed] [Google Scholar]
- 90.Dhali A, Anchamparuthy VM, Butler SP, Pearson RE, Mullarky IK, Gwazdauskas FC. Gene expression and development of mouse zygotes following droplet vitrification. Theriogenology. 2007;68(9):1292–1298. doi: 10.1016/j.theriogenology.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 91.Bagis H, Sagirkaya H, Mercan HO, Dinnyes A. Vitrification of pronuclear-stage mouse embryos on solid surface (SSV) versus in cryotube: comparison of the effect of equilibration time and different sugars in the vitrification solution. Mol Reprod Dev. 2004;67(2):186–192. doi: 10.1002/mrd.10388. [DOI] [PubMed] [Google Scholar]
- 92.Dinnyes A, Dai Y, Jiang S, Yang X. High developmental rates of vitrified bovine oocytes following parthenogenetic activation, in vitro fertilization, somatic cell nuclear transfer. Biol Reprod. 2000;63(2):513–518. doi: 10.1095/biolreprod63.2.513. [DOI] [PubMed] [Google Scholar]
- 93.Begin I, Bhatia B, Baldassarre H, Dinnyes A, Keefer CL. Cryopreservation of goat oocytes and in vivo derived 2- to 4-cell embryos using the Cryoloop (CLV) and solid-surface vitrification (SSV) methods. Theriogenology. 2003;59(8):1839–1850. doi: 10.1016/s0093-691x(02)01257-8. [DOI] [PubMed] [Google Scholar]
- 94.Gupta MK, Uhm SJ, Lee HT. Cryopreservation of immature and in vitro matured porcine oocytes by solid surface vitrification. Theriogenology. 2007;67(2):238–248. doi: 10.1016/j.theriogenology.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 95.Somfai T, Ozawa M, Noguchi J, et al. Developmental competence of in vitro-fertilized porcine oocytes after in vitro maturation and solid surface vitrification: effect of cryopreservation on oocyte antioxidative system and cell cycle stage. Cryobiology. 2007;55(2):115–126. doi: 10.1016/j.cryobiol.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 96.Rojas C, Palomo MJ, Albarracin JL, Mogas T. Vitrification of immature and in vitro matured pig oocytes: study of distribution of chromosomes, microtubules, actin microfilaments. Cryobiology. 2004;49(3):211–220. doi: 10.1016/j.cryobiol.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 97.Shi LY, Jin HF, Kim JG, et al. Ultra-structural changes and developmental potential of porcine oocytes following vitrification. Anim Reprod Sci. 2007;100(1–2):128–140. doi: 10.1016/j.anireprosci.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 98.Rall WF. Factors affecting the survival of mouse embryos cryopreserved by vitrification. Cryobiology. 1987;24(5):387–402. doi: 10.1016/0011-2240(87)90042-3. [DOI] [PubMed] [Google Scholar]
- 99.Arav A, Shehu D, Mattioli M. Osmotic and cytotoxic study of vitrification of immature bovine oocytes. J Reprod Fertil. 1993;99(2):353–358. doi: 10.1530/jrf.0.0990353. [DOI] [PubMed] [Google Scholar]
- 100.Arav A, Rubinsky B, Fletcher G, Seren E. Cryogenic protection of oocytes with antifreeze proteins. Mol Reprod Dev. 1993;36(4):488–493. doi: 10.1002/mrd.1080360413. [DOI] [PubMed] [Google Scholar]
- 101.Arav A, Zeron Y. Vitrification of bovine oocytes using modified minimum drop size technique (MDS) is effected by the composition and concentration of the vitrification solution and by the cooling conditions. Theriogenology. 1997;47:2. [Google Scholar]
- 102.Tasoglu S, Kaynak G, Szeri AJ, Demirci U, Muradoglu M. Impact of a compound droplet on a flat surface: a model for single cell epitaxy. Phys Fluids. 1994;22(8):082103. doi: 10.1063/1.3475527. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Xu F, Moon SJ, Emre AE, et al. A droplet-based building block approach for bladder smooth muscle cell (SMC) proliferation. Biofabrication. 2010;2(1):014105. doi: 10.1088/1758-5082/2/1/014105. [DOI] [PubMed] [Google Scholar]
- 104.Xu F, Moon S, Zhang X, Shao L, Song YS, Demirci U. Multi-scale heat and mass transfer modelling of cell and tissue cryopreservation. Philos Transact A Math Phys Eng Sci. 2010;368(1912):561–583. doi: 10.1098/rsta.2009.0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Demirci U, Yaralioglu GG, Haeggstrom E, Khuri-Yakub BT. Femtoliter to picoliter droplet generation for organic polymer deposition using single reservoir ejector arrays. IEEE Trans Semiconduct Manuf. 2005;18(4):709–715. [Google Scholar]
- 106.Demirci U, Yaralioglu GG, Haeggstrom E, et al. Acoustically actuated flextensional SixNy and single-crystal silicon 2-D micromachined ejector arrays. IEEE Trans Semiconduct Manuf. 2004;17(4):517–524. [Google Scholar]
- 107.Demirci U. Acoustic picoliter droplets for emerging applications in semiconductor industry and biotechnology. J Microelectromech Syst. 2006;15(4):957–966. [Google Scholar]
- 108.Bac BH, Song Y, Moon Y, Kim MH, Kang IM. Effective utilization of incinerated municipal solid waste incineration ash: zeolitic material synthesis and silica extraction. Waste Manag Res. 2010;28(8):714–722. doi: 10.1177/0734242X09360056. [DOI] [PubMed] [Google Scholar]
- 109.Audi L, Fernandez-Cancio M, Carrascosa A, et al. Novel (60%) and recurrent (40%) androgen receptor gene mutations in a series of 59 patients with a 46, XY disorder of sex development. J Clin Endocrinol Metab. 2010;95(4):1876–1888. doi: 10.1210/jc.2009-2146. [DOI] [PubMed] [Google Scholar]
- 110.Bielanski A, Vajta G. Risk of contamination of germplasm during cryopreservation and cryobanking in IVF units. Hum Reprod. 2009;24(10):2457–2467. doi: 10.1093/humrep/dep117. [DOI] [PubMed] [Google Scholar]
- 111.McBurnie LD, Bardo B. Validation of sterile filtration of liquid nitrogen. Pharm Technol N Am. 2002;26:9. [Google Scholar]
- 112.Parmegiani L, Cognigni GE, Filicori M. Ultra-violet sterilization of liquid nitrogen prior to vitrification. Hum Reprod. 2009;24(11):2969. doi: 10.1093/humrep/dep329. [DOI] [PubMed] [Google Scholar]
- 113.Lucena E, Bernal DP, Lucena C, Rojas A, Moran A, Lucena A. Successful ongoing pregnancies after vitrification of oocytes. Fertil Steril. 2006;85(1):108–111. doi: 10.1016/j.fertnstert.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 114.Agca Y. Cryopreservation of oocyte and ovarian tissue. ILAR J. 2000;41(4):207–220. doi: 10.1093/ilar.41.4.207. [DOI] [PubMed] [Google Scholar]
- 115.Mandelbaum J, Belaisch-Allart J, Junca AM, et al. Cryopreservation in human assisted reproduction is now routine for embryos but remains a research procedure for oocytes. Hum Reprod. 1998;13(Suppl 3):161–174. doi: 10.1093/humrep/13.suppl_3.161. discussion 175–167. [DOI] [PubMed] [Google Scholar]
- 116.Saragusty J, Arav A. Current progress in oocyte and embryo cryopreservation by slow freezing and vitrification. Reproduction. 2010;141(1):1–19. doi: 10.1530/REP-10-0236. [DOI] [PubMed] [Google Scholar]
- 117.Oktay K, Cil AP, Bang H. Efficiency of oocyte cryopreservation: a meta-analysis. Fertil Steril. 2006;86(1):70–80. doi: 10.1016/j.fertnstert.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 118.Pornwiroon S, Kunathikom S, Makemaharn O, Huanaraj R. Vitrification of mouse oocyte using open pulled straws compared with needles. J Med Assoc Thai. 2006;89(12):2015–2020. [PubMed] [Google Scholar]
- 119.Mavrides A, Morroll D. Cryopreservation of bovine oocytes: is Cryoloop vitrification the future to preserving the female gamete? Reprod Nutr Dev. 2002;42(1):73–80. doi: 10.1051/rnd:20020008. [DOI] [PubMed] [Google Scholar]
- 120.Sun HX, Hu YL, Chen LJ, Zhang NY, Xu ZP. Influence of two different vitrification cryopreservation methods on spindles of mouse oocytes. Zhonghua Nan Ke Xue. 2006;12(12):1076–1079. 1083. [PubMed] [Google Scholar]
- 121.Wang Z, Sun Z, Chen Y, He F. A modified Cryoloop vitrification protocol in the cryopreservation of mature mouse oocytes. Zygote. 2009;17(3):217–224. doi: 10.1017/S0967199409005309. [DOI] [PubMed] [Google Scholar]
- 122.Kuleshova L, Gianaroli L, Magli C, Ferraretti A, Trounson A. Birth following vitrification of a small number of human oocytes: case report. Hum Reprod. 1999;14(12):3077–3079. doi: 10.1093/humrep/14.12.3077. [DOI] [PubMed] [Google Scholar]
- 123.Liebermann J, Tucker MJ. Effect of carrier system on the yield of human oocytes and embryos as assessed by survival and developmental potential after vitrification. Reproduction. 2002;124(4):483–489. doi: 10.1530/rep.0.1240483. [DOI] [PubMed] [Google Scholar]
- 124.Chen ZJ, Li Y, Hu JM, Li M. Successful clinical pregnancy of cryopreserved human oocytes after vitrification. Zhonghua Yi Xue Za Zhi. 2006;86(29):2037–2040. [PubMed] [Google Scholar]
- 125.Li YF, He QH, Zhang HW, et al. Cryopreservation by Cryoloop damages human immature oocytes. Zhonghua Nan Ke Xue. 2008;14(6):498–502. [PubMed] [Google Scholar]
- 126.Antinori M, Licata E, Dani G, Cerusico F, Versaci C, Antinori S. Cryotop vitrification of human oocytes results in high survival rate and healthy deliveries. Reprod Biomed Online. 2007;14(1):72–79. doi: 10.1016/s1472-6483(10)60766-3. [DOI] [PubMed] [Google Scholar]
- 127.Campos-Chillon LF, Suh TK, Barcelo-Fimbres M, et al. Vitrification of early-stage bovine and equine embryos. Theriogenology. 2009;71(2):349–354. doi: 10.1016/j.theriogenology.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 128.Yu XL, Deng W, Liu FJ, et al. Closed pulled straw vitrification of in vitro-produced and in vivo-produced bovine embryos. Theriogenology. 2010;73(4):474–479. doi: 10.1016/j.theriogenology.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 129.Desai N, Blackmon H, Szeptycki J, Goldfarb J. Cryoloop vitrification of human day 3 cleavage-stage embryos: post-vitrification development, pregnancy outcomes and live births. Reprod Biomed Online. 2007;14(2):208–213. doi: 10.1016/s1472-6483(10)60789-4. [DOI] [PubMed] [Google Scholar]
- 130.Zhu L, Lou C, Huang MZ, Li H, Xing FQ. Vitrification of mouse blastocysts using two kinds of straw systems. Di Yi Jun Yi Da Xue Xue Bao. 2003;23(9):992–995. [PubMed] [Google Scholar]
- 131.Saki G, Rahim F, Moradi L. The study of developmental capacity of vitrified mouse blastocysts in different straws after transfer to mouse pseudo pregnant. Pak J Biol Sci. 2008;11(14):1809–1814. doi: 10.3923/pjbs.2008.1809.1814. [DOI] [PubMed] [Google Scholar]
- 132.Son WY, Yoon SH, Yoon HJ, Lee SM, Lim JH. Pregnancy outcome following transfer of human blastocysts vitrified on electron microscopy grids after induced collapse of the blastocoele. Hum Reprod. 2003;18(1):137–139. doi: 10.1093/humrep/deg029. [DOI] [PubMed] [Google Scholar]
- 133.Cho HJ, Son WY, Yoon SH, Lee SW, Lim JH. An improved protocol for dilution of cryoprotectants from vitrified human blastocysts. Hum Reprod. 2002;17(9):2419–2422. doi: 10.1093/humrep/17.9.2419. [DOI] [PubMed] [Google Scholar]
- 134.Mukaida T, Nakamura S, Tomiyama T, Wada S, Kasai M, Takahashi K. Successful birth after transfer of vitrified human blastocysts with use of a Cryoloop containerless technique. Fertil Steril. 2001;76(3):618–620. doi: 10.1016/s0015-0282(01)01968-9. [DOI] [PubMed] [Google Scholar]
- 135.Brockbank KGM, Walsh JR, Song YC, Taylor MJ. Vitrification: preservation of cellular implants. In: Ashammakhi N, Ferretti P, editors. Topics in Tissue Engineering. Vol. 26. University of Oulu; Finland: 2003. [Google Scholar]
- 136.Mukaida T, Nakamura S, Tomiyama T, et al. Vitrification of human blastocysts using Cryoloops: clinical outcome of 223 cycles. Hum Reprod. 2003;18(2):384–391. doi: 10.1093/humrep/deg047. [DOI] [PubMed] [Google Scholar]
- 137.Mukaida T, Takahashi K, Kasai M. Blastocyst cryopreservation: ultrarapid vitrification using Cryoloop technique. Reprod Biomed Online. 2003;6(2):221–225. doi: 10.1016/s1472-6483(10)61713-0. [DOI] [PubMed] [Google Scholar]
- 138.Hiraoka K, Kinutani M, Kinutani K. Blastocoele collapse by micropipetting prior to vitrification gives excellent survival and pregnancy outcomes for human day 5 and 6 expanded blastocysts. Hum Reprod. 2004;19(12):2884–2888. doi: 10.1093/humrep/deh504. [DOI] [PubMed] [Google Scholar]
- 139.Toh WS, Lee EH, Cao T. Potential of human embryonic stem cells in cartilage tissue engineering and regenerative medicine. Stem Cell Rev. 2011;7(3):544–559. doi: 10.1007/s12015-010-9222-6. [DOI] [PubMed] [Google Scholar]
- 140.Kuleshova LL, Gouk SS, Hutmacher DW. Vitrification as a prospect for cryopreservation of tissue-engineered constructs. Biomaterials. 2007;28(9):1585–1596. doi: 10.1016/j.biomaterials.2006.11.047. [DOI] [PubMed] [Google Scholar]
- 141.Amps KJ, Jones M, Baker D, Moore HD. In situ cryopreservation of human embryonic stem cells in gas-permeable membrane culture cassettes for high post-thaw yield and good manufacturing practice. Cryobiology. 2010;60(3):344–350. doi: 10.1016/j.cryobiol.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 142.Grein TA, Freimark D, Weber C, Hudel K, Wallrapp C, Czermak P. Alternatives to dimethylsulfoxide for serum-free cryopreservation of human mesenchymal stem cells. Int J Artif Organs. 2010;33(6):370–380. [PubMed] [Google Scholar]
- 143.Berz D, McCormack EM, Winer ES, Colvin GA, Quesenberry PJ. Cryopreservation of hematopoietic stem cells. Am J Hematol. 2007;82(6):463–472. doi: 10.1002/ajh.20707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Zhang D, Efendic S, Brismar K, Gu HF. Effects of MCF2L2, ADIPOQ and SOX2 genetic polymorphisms on the development of nephropathy in Type 1 diabetes mellitus. BMC Med Genet. 2010;11(1):116. doi: 10.1186/1471-2350-11-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kader A, Agarwal A, Sharma R, Falcone T. Vitrification of isolated mice blastomeres using a closed loading device. Reprod Biol Endocrinol. 2009;7:17. doi: 10.1186/1477-7827-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Li Y, Tan JC, Li LS. Comparison of three methods for cryopreservation of human embryonic stem cells. Fertil Steril. 2010;93(3):999–1005. doi: 10.1016/j.fertnstert.2008.10.052. [DOI] [PubMed] [Google Scholar]
- 147.Reubinoff BE, Pera MF, Vajta G, Trounson AO. Effective cryopreservation of human embryonic stem cells by the open pulled straw vitrification method. Hum Reprod. 2001;16(10):2187–2194. doi: 10.1093/humrep/16.10.2187. [DOI] [PubMed] [Google Scholar]
- 148.Giraldo JA, Weaver JD, Stabler CL. Tissue engineering approaches to enhancing clinical islet transplantation through tissue engineering strategies. J Diabetes Sci Technol. 2010;4(5):1238–1247. doi: 10.1177/193229681000400525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tedder ME, Simionescu A, Chen J, Liao J, Simionescu DT. Assembly and testing of stem cell-seeded layered collagen constructs for heart valve tissue engineering. Tissue Eng Part A. 2010;17(1–2):25–36. doi: 10.1089/ten.tea.2010.0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zhang X, Reagan MR, Kaplan DL. Electrospun silk biomaterial scaffolds for regenerative medicine. Adv Drug Deliv Rev. 2009;61(12):988–1006. doi: 10.1016/j.addr.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zhang X, Wang X, Keshav V, Johanas JT, Leisk GG, Kaplan DL. Dynamic culture conditions to generate silk-based tissue-engineered vascular grafts. Biomaterials. 2009;30(19):3213–3223. doi: 10.1016/j.biomaterials.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhang X, Baughman CB, Kaplan DL. In vitro evaluation of electrospun silk fibroin scaffolds for vascular cell growth. Biomaterials. 2008;29(14):2217–2227. doi: 10.1016/j.biomaterials.2008.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Geckil H, Xu F, Zhang XH, Moon S, Demirci U. Engineering hydrogels as extracellular matrix mimics. Nanomedicine (Lond) 2010;5(3):469–484. doi: 10.2217/nnm.10.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Liu BL, McGrath J. Vitrification solutions for the cryopreservation of tissue-engineered bone. Cell Preserv Technol. 2004;2(2):11. [Google Scholar]
- 155.Mukherjee N, Chen Z, Sambanis A, Song Y. Effects of cryopreservation on cell viability and insulin secretion in a model tissue-engineered pancreatic substitute (TEPS) Cell Transplant. 2005;14(7):449–456. doi: 10.3727/000000005783982882. [DOI] [PubMed] [Google Scholar]
- 156.Song YC, Chen ZZ, Mukherjee N, et al. Vitrification of tissue engineered pancreatic substitute. Transplant Proc. 2005;37(1):253–255. doi: 10.1016/j.transproceed.2004.11.027. [DOI] [PubMed] [Google Scholar]
- 157.Dahl SL, Chen Z, Solan AK, Brockbank KG, Niklason LE, Song YC. Feasibility of vitrification as a storage method for tissue-engineered blood vessels. Tissue Eng. 2006;12(2):291–300. doi: 10.1089/ten.2006.12.291. [DOI] [PubMed] [Google Scholar]
- 158.Smith AU. Cartilage. In: Karow AM Jr, Abouna GJM, Humphries AL Jr, editors. Organ Preservation for Transplantation. Little Brown; Boston, MA, USA: 1974. pp. 214–227. [Google Scholar]
- 159.Song YC, An YH, Kang QK, et al. Vitreous preservation of articular cartilage grafts. J Invest Surg. 2004;17(2):65–70. doi: 10.1080/08941930490422438. [DOI] [PubMed] [Google Scholar]
- 160.Song YC, Khirabadi BS, Lightfoot F, Brockbank KG, Taylor MJ. Vitreous cryopreservation maintains the function of vascular grafts. Nat Biotechnol. 2000;18(3):296–299. doi: 10.1038/73737. [DOI] [PubMed] [Google Scholar]
- 161.Elder E, Chen Z, Ensley A, Nerem R, Brockbank K, Song Y. Enhanced tissue strength in cryopreserved, collagen-based blood vessel constructs. Transplant Proc. 2005;37(10):4625–4629. doi: 10.1016/j.transproceed.2005.10.033. [DOI] [PubMed] [Google Scholar]
- 162.Chian RC, Quinn P, editors. Fertility Cryopreservation. University Press Cambridge; Cambridge, UK: 2010. [Google Scholar]
- 163.Armitage WJ. Cryopreservation for corneal storage. Dev Ophthalmol. 2009;43:63–69. doi: 10.1159/000223839. [DOI] [PubMed] [Google Scholar]
- 164.Meltendorf C, Hincha DK, Hoffmann F. Vitrification of posterior corneal lamellae. Cryobiology. 2002;44(2):170–178. doi: 10.1016/s0011-2240(02)00022-6. [DOI] [PubMed] [Google Scholar]
- 165.Armitage WJ, Rich SJ. Vitrification of organized tissues. Cryobiology. 1990;27(5):483–491. doi: 10.1016/0011-2240(90)90037-5. [DOI] [PubMed] [Google Scholar]
- 166.Shaw JM, Oranratnachai A, Trounson AO. Fundamental cryobiology of mammalian oocytes and ovarian tissue. Theriogenology. 2000;53(1):59–72. doi: 10.1016/s0093-691x(99)00240-x. [DOI] [PubMed] [Google Scholar]