Abstract
We studied the efficacy of prophylactic plate fixation technique and a modified harvest of the osteocutaneous radial forearm free flap (OCRFFF) to minimize the incidence of postoperative donor radius pathological fracture. We retrospectively studied of the first 70 consecutive patients undergoing OCRFFF harvest by the University of Kansas Head and Neck Microvascular Reconstruction Team. Mean follow-up was 13 months. One of two patients undergoing OCRFFF harvest without prophylactic fixation developed a pathological radius fracture. The 68 subsequent OCRFFF patients underwent prophylactic fixation of the donor radius, and none developed a symptomatic radius fracture. Five of 68 patients did have a radiographically visible fracture requiring no intervention. The plate fixation technique was further modified to exclude monocortical screws in the radius bone donor defect (subsequent 39 patients), without any further fractures detected. One patient required forearm hardware removal for an attritional extensor tendon tear. The described modified OCRFFF harvest and prophylactic plate fixation technique may eliminate postoperative pathological fracture of the donor radius. Donor morbidity is similar to that of the fasciocutaneous radial forearm free flap , affording safe use of OCRFFF in head and neck reconstruction.
Keywords: Free flap, radius bone, reconstructive surgery
Ideal reconstruction in the oral cavity after extirpative surgery continues to be a formidable challenge. Any alteration in the soft tissue and bony characteristics of the native oral cavity can have both significant cosmetic and functional ramifications. Microvascular reconstruction of such defects has been shown to be a cost-effective technique to improve postoperative function.1 The radial forearm fasciocutaneous free flap (RFFF) has become a “workhorse” flap in the head and neck for soft tissue reconstructions.1,2,3 Although the RFFF is most commonly harvested as a fasciocutaneous flap, perforators to the radius allow it to be developed as an osteocutaneous radial forearm free flap (OCRFFF). A combination of a large skin paddle to line the palatal mucosal surface, a small volume of the soft tissue, and a moderate vascularized bone stock are the requirements that are fulfilled very well by a reconstruction with an OCRFFF. Ideal reconstruction alternatives to the composite defect have been elusive, and frequently, the soft tissue or bony reconstruction components must take precedence. Some authors have advocated the double free flap reconstruction, using the best tissue available for each component—sensate RFFF for soft tissue reconstruction and an osseous free flap for mandibular reconstruction.4,5 This approach has obvious disadvantages of increased resource utilization (operative time and cost) and two separate donor sites, with associated morbidity. A radial forearm free flap is an ideal solution to the most problematic aspect of choosing the flap for reconstruction of a complex head and neck defect: a need for a long, 10- to 13-cm pedicle to span the distance between the midface and cervical vessels. Using an OCRFFF eliminates the need for vein grafts, which shortens operative time and improves the success of the reconstruction. Despite this, its use as an osteocutaneous free flap was abandoned early on. Two issues have been largely to blame for limiting surgeons' consideration of the OCRFFF as an option for single-stage reconstruction of composite defects in the head and neck: the inadequacy of available bone and the potential for morbidity, most notably pathological fracture.6,7
INDICATIONS AND CONTRAINDICATIONS
We describe a modified harvest technique for the OCRFFF that employs prophylactic internal fixation of the donor radius. The evolution of this technique has resulted in a safe OCRFFF harvest, with donor site morbidity similar to that observed with the widely used RFFF.
General contraindications to microvascular free tissue transfer also apply to the OCRFFF procedure. Physical signs and symptoms of poor peripheral digit perfusion or healing contraindicate harvest of the radial artery pedicle. An incomplete palmar arch precludes radial artery pedicle harvest because inadequate blood supply to the lateral digits results when only the ulnar artery perfuses the hand. Radial artery thrombosis or compromise is also apparent on a preoperative Allen test. We evaluate equivocal Allen tests with objective Doppler photoplethysmography. This test can confirm adequate ulnar artery perfusion to the hand, which then allows safe harvest of the radial artery and use of the OCRFFF. If ulnar perfusion is inadequate, an alternate flap must be used.
Previous surgery or trauma to the proposed donor arm must be closely investigated, especially by means of radiography, to ensure normal and intact vascular and musculoskeletal anatomy. A similar workup applies to obvious congenital deformities.
When bony defects larger than ~10 cm are anticipated, reconstruction may require more bone than is safely available using the OCRFFF procedure, depending somewhat on the patient's stature.
SUBJECTS AND METHODS
A retrospective review of medical charts was completed for the first 70 consecutive patients undergoing OCRFFF reconstruction by the Head and Neck Microvascular Reconstruction Team at the University of Kansas Medical Center. Surgeries were performed between September 1994 and August 2000.
Preoperative Assessment
After it has been determined that the OCRFFF is the most appropriate reconstruction of the anticipated or known composite defect, the patient is assessed preoperatively for harvest safety. A history of peripheral vascular disease, diabetes, poor or slow wound healing, or coagulopathy is important to know prior to consideration for any RFFF harvest. In addition, history of osteoporosis or forearm trauma or surgery may influence the decision to use the OCRFFF. The dominant hand side as well as the patient's occupation and recreational activities may also influence the surgeon's reconstructive decision. OCRFFF may not be an appropriate choice if the patient desires dental rehabilitation with osseointegrated implants postoperatively, as the bone stock usually is not sufficient for support.
On exam, a standard subjective Allen's test and objective Allen's test (Doppler plethysmography) are performed on both forearms to predict adequate thenar perfusion after harvest.8 The hand and forearm are inspected for scars and signs of previous trauma or healing difficulties. Forearm plain films may be necessary if a bony deformity is encountered or suspected.
OCRFFF Harvest
The fasciocutaneous paddle, lateral intermuscular septum, and radial artery pedicle are harvested as described previously, with three specific modifications.9 First, the skin paddle is slightly proximally (2 cm proximal to the wrist crease) and ulnar biased to assist with skin coverage of the radius fixation hardware (Fig. 1). Because of this ulnar biasing, the cephalic vein and lateral antebrachial cutaneous nerve are frequently too radial for inclusion in the harvest. We have not had problems harvesting a significant fasciocutaneous paddle extending dorsally on the ulnar side of the forearm. Second, the brachioradialis tendon is carefully and widely undermined and retracted radially. Finally, the perforators within the lateral intermuscular septum extending from the radial artery pedicle to the periosteum of the radius must be preserved. We prefer harvest under tourniquet control.
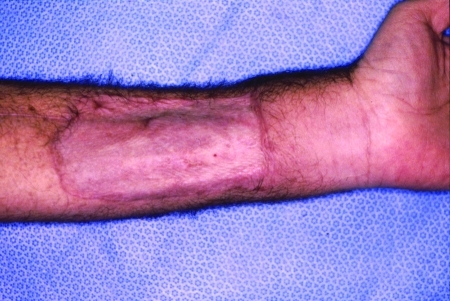
Figure 1.
Healed osteocutaneous radial forearm free flap donor site. The proximal bias of the skin paddle from the wrist crease is at least 2 cm, and the ulnar bias allows skin coverage of radius and plate hardware.
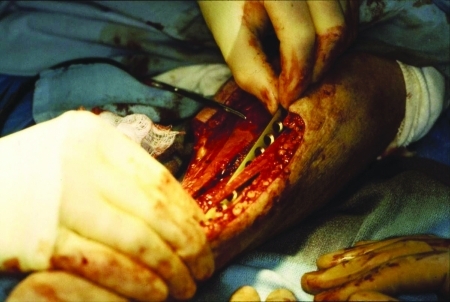
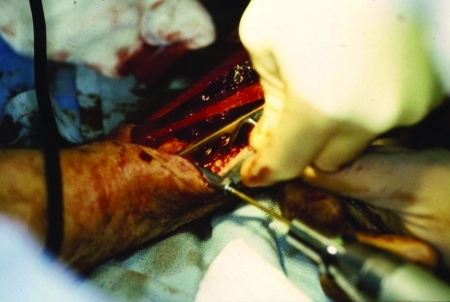
The flexor digitorum superficialis is then released from the radius and retracted ulnarly to visualize the flexor pollicis longus (FPL). The FPL and periosteum are longitudinally split over the midline of the volar surface of the radius using a No. 15 scalpel. This midline is determined by palpation of the radius thickness, remembering that the radius diameter enlarges distally. This is performed on the ulnar side of the lateral intermuscular septum and pedicle. The required length of bone is the marked with a surgical pen. The vascularized radius bone graft is generally harvested between the pronator teres (PT) and brachioradialis tendon insertions. The distal osteotomy must be made at least 2.5 cm proximal to the radius styloid process to allow at least two screws to be inserted during internal fixation. Proximally, the bone can be harvested even beyond the PT insertion; however, the PT tendon requires reinsertion to the remaining radius bone and/or fixation plate. The proximal and distal osteotomies are marked by sharply incising the periosteum in a beveled fashion, such that the resulting bony defect is slightly beveled concavely. A fine-blade oscillating saw is utilized to make the longitudinal radius cut through its midportion (Fig. 2). Copious antibiotic-containing saline irrigation is used. This cut is placed to allow harvest of ~50% of the radius thickness. The cut is usually started proximally at the base of the anticipated beveled proximal osteotomy and moves distally. Because of the curvature of the radius and increased radius circumference distally, this minimizes the incidence of harvesting too much of the radial circumference proximally. A thin metal ruler is then inserted in the longitudinal cuts to act as a backstop during the proximal and distal beveled osteotomies (Fig. 3). The periosteum is then incised dorsally with a scalpel, completing the bone graft harvest. The tourniquet is released, and the OCRFFF is then left to perfuse on its pedicle until transfer of the flap to the recipient site. The distal pedicle is first clamped and hand perfusion is again confirmed prior to actual pedicle sacrifice (intraoperative Allen's test). Silk ties and/or medium hemoclips are used during pedicle sacrifice (Fig. 4).
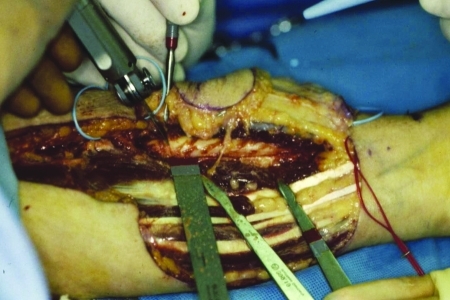
Figure 2.
The horizontal osteotomy is started proximally, using an oscillating saw. Approximately 50% of the thickness of the bone is harvested.
Figure 3.
Inserting a metal ruler in the proximal and distal ends of the longitudinal cut helps prevent overcutting and creates bevel-shaped osteotomies.
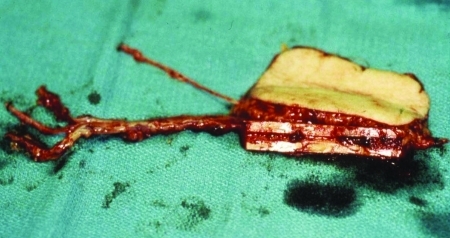
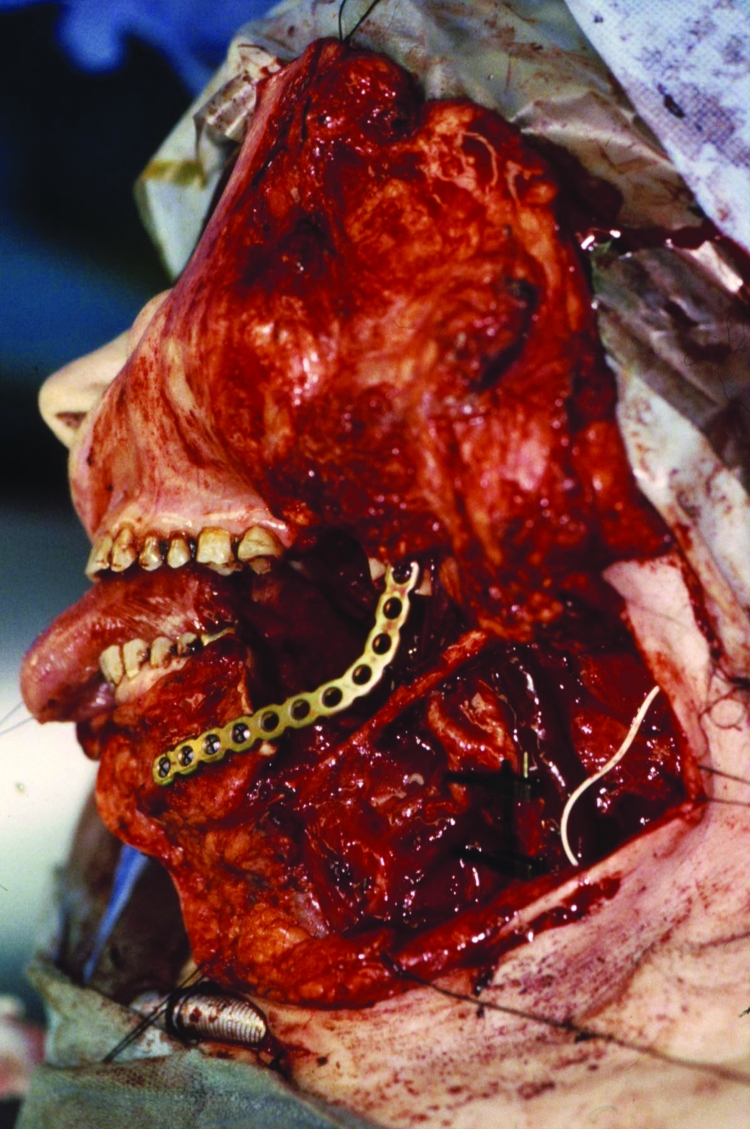
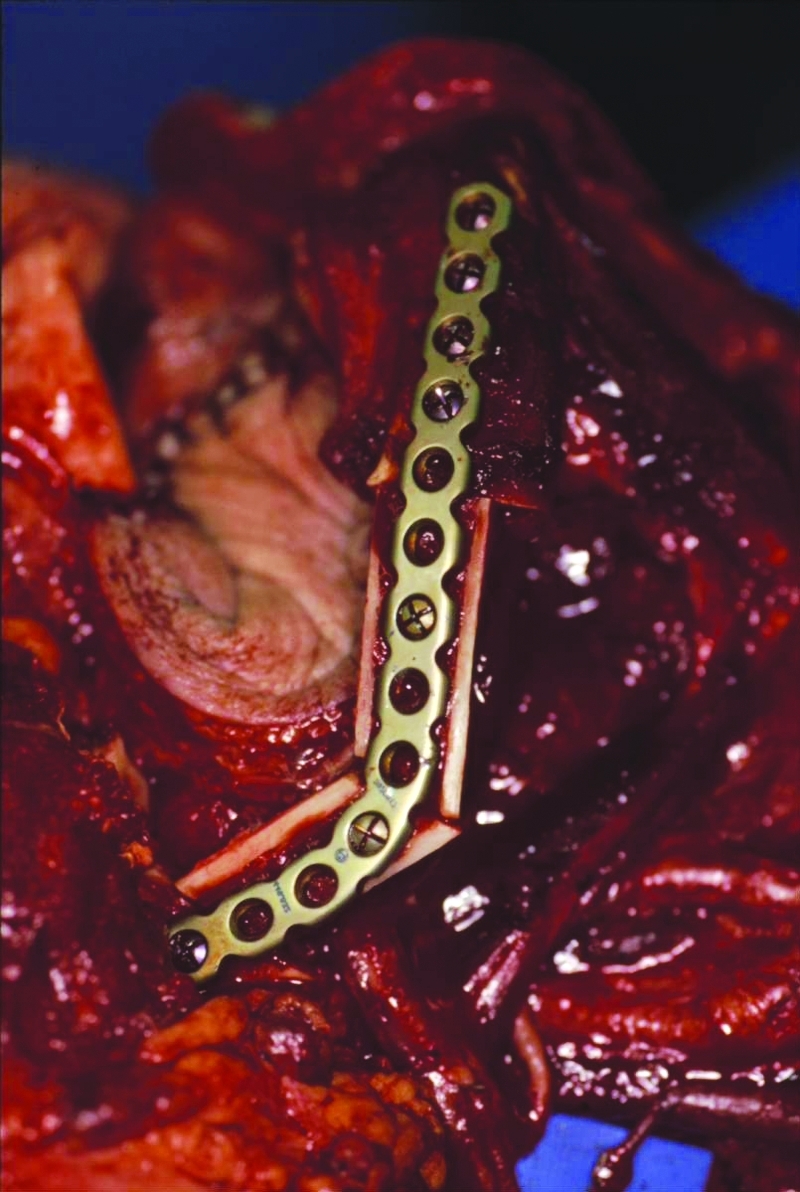
Figure 4.
Osteocutaneous radial forearm free flap appearance immediately after harvest. Note a long vascular pedicle and the attached bone segment.
Prophylactic Internal Fixation of Donor Radius and Wound Closure
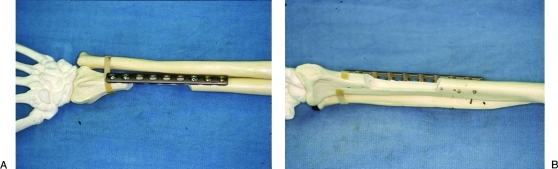
Prophylactic internal fixation can be performed with or without reinflating the arm tourniquet. The dorsal radius is exposed proximally and distally. An appropriately sized 3.5 low-contact dynamic compression plate (AO Synthes, Davos, Switzerland) is positioned over the radius and bent to the contour of the bone (Fig. 5). Usually 8- to 14-hole plates are required depending on the length of the harvested radius graft. Distally, the radial wrist extensors (abductor pollicis longus, extensor pollicis brevis, extensor carpi radialis longus, and extensor carpi radialis brevis) are retracted radially and at least two standard bicortical screws are placed (Fig. 6). Proximally, the supinator is visualized, and with long bone harvests, this muscle is subperiosteally elevated and the plate placed beneath it. Care is taken to protect the posterior interosseous nerve, a branch of the deep radial nerve, which pierce the supinator. At least two, and usually three, bicortical screws are placed proximally (Fig. 7A). No screws are placed in the defect cavity to avoid the risk of additional stress risers (Fig. 7B).10
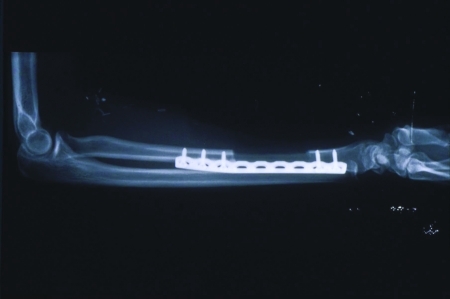
Figure 5.
A 3.5 low-contact dynamic compression plate is used for prophylactic internal fixation of the donor radius. It is positioned over the radial side of the bone and bent to its contour as needed.
Figure 6.
Two bicortical screws are placed distally after retracting the radial wrist extensors (abductor pollicis longus, extensor pollicis brevis, extensor carpi radialis longus, extensor carpi radialis brevis).
Figure 7.
Model of donor radius defect and prophylactic internal fixation technique. (A) From the volar view, the beveling at the osteotomy edges is demonstrated. Note how the plate only partially overlaps the bony defect. (B) The dorsal view shows the two and three bicortical screws placed distally and proximally, respectively. No monocortical screws are placed within the defect.
The arm is then closed as for a fasciocutaneous forearm flap using a meshed split-thickness skin graft with three modifications. First, the PT tendon is reinserted onto the remaining radius or fixation plate as necessary. Second, the FPL remnant is sutured over the radius defect and plate. Finally, the flexor digitorum superficialis can usually be brought over the flexor carpi radialis tendon to the radial skin edge. This provides a second muscular layer over the bony donor site (Fig. 8), and helps the skin graft take on the flexor carpi radialis tendon (Fig. 9). The donor site is covered with Xeroform gauze (Sherwood Medical, St. Louis, MO), cotton balls, and a gauze wrap. A rigid plaster ulnar-gutter splint is then applied and wrapped with an elastic bandage.
Figure 8.
Two muscle layers are reapproximated over the plate to ensure its coverage.
Figure 9.
Split-thickness skin graft in place at the osteocutaneous radial forearm free flap donor site completing the closure.
Postoperative Management
The donor arm is elevated in the air with a pillowcase sling hanging from an IV pole for the first 48 hours and then kept elevated on a pillow. The donor arm is monitored at the same schedule as the microvascular flap. The arm splint is taken down at 5 to 7 days postoperatively, and the donor site is dressed with a fresh Xeroform and cotton wrap dressing for protection during healing. The arm sutures and/or staples are removed at ~10 days postoperatively. The patient is encouraged to perform normal movements with the donor arm after splint removal.
RESULTS
Of the first 70 consecutive patients undergoing head and neck reconstruction with the OCRFFF, 40 patients (57%) were male and 30 (43%) were female with ages ranging from 16 to 89 with a mean age of 62 years.
Sixty-nine (98%) of patients underwent OCRFFF reconstruction immediately after cancer extirpative surgery, and only 1 (2%) patient underwent OCRFFF for secondary reconstruction. The nondominant arm was chosen as the donor site in most cases, with only 6 (9%) patients requiring dominant arm harvests due to unsuitable vascular supply to their nondominant hands. The radial artery was reconstructed with a saphenous vein graft in only one patient for concerns of inadequate ulnar flow to the hand restoring adequate flow to the hand without sequelae. The first two OCRFFF harvests were treated postoperatively with a period of immobilization without donor radius plating. The subsequent 68 OCRFFF patients underwent prophylactic internal fixation after radius bone harvest. The first 29 OCRFFF undergoing internal fixation also had intermittent monocortical screws placed within the bone graft defect (Fig. 10). This practice was believed to yield stress risers at these screw sites, and this step was abandoned in subsequent patients. The current technique is as described in Subjects and Methods. In all cases, ~50% of the radius circumference was harvested, and lengths ranged from 5.5 to 12 cm (mean: 7.8 ± 0.2 standard error of the mean). Fasciocutaneous skin paddle size ranged from 12 cm2 to 126 cm2 with a mean of 72 cm2 ( ± 3.3 standard error of the mean). Only one patient underwent primary closure of the skin paddle donor site, and the remainder underwent skin grafting as described previously. Average tourniquet time was 89 minutes (60–129 minutes range).
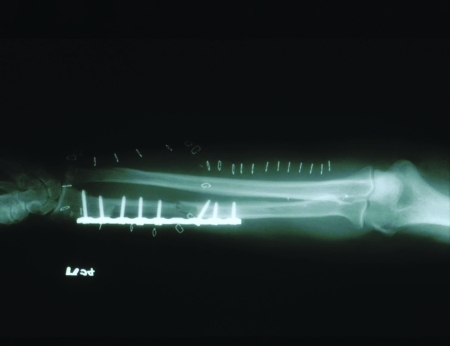
Figure 10.
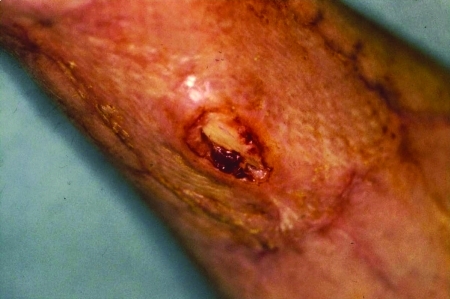
Old technique of placing monocortical screws within the bone defect, abandoned after 29 patients due to higher risk of radial bone fractures.
Mean follow-up was 13.2 months, with a range of 0 to 45 months. The most common donor site complication was flexor carpi radialis tendon exposure (Fig. 11; 46% patients), with only one requiring subsequent operative intervention without sequelae. There have been no patients with hardware loosening or exposure at the donor site. One patient attritionally ruptured her extensor pollicis longus tendon on the distal end of the fixation plate. This was thought to be due to the plate being placed too ulnarly. She required operative tendon transfer repair and removal of the 12-hole fixation plate at 5 months after reconstruction. Postoperative donor site fracture occurred in one of the first two patients (50%) who did not undergo prophylactic internal fixation of the radius. There have been no clinically significant donor radius fractures in any of the remaining 68 patients. No patients have required prolonged immobilization, bone grafting, or revision internal fixation. There were 5 (7%) radiographically discovered fractures discovered in the postoperative period on routine forearm X-rays in the plated patients (Fig. 12). Each of these patients had the older technique of intermittent monocortical screw placement in the donor defect, prompting the modified technique. There have been no further fractures in the subsequent 39 OCRFFF patients.
Figure 11.
Tendon exposure site at flexor carpi radialis: it healed with local wound care for 3 weeks.
Figure 12.
Radiographically detected, asymptomatic donor radius fracture that required no intervention. Note that the fracture occurred at the site of a monocortical screw placed within the bony defect (old technique).
Postoperative function using this harvest technique has been extensively described previously.10 Despite most donor arms being the nondominant arms, both strength and range-of-motion parameters all measured 84% or better compared with the unoperated arms. Follow-up radiographs have shown significant reconstitution and remodeling of the radius bone by 5 months after surgery, without any evidence of osteopenia or hardware loosening.
DISCUSSION
Since its introduction in 1981 by Yang et al, the RFFF has become a “workhorse” flap in head and neck reconstruction.11 Its increasing popularity has mainly stemmed from its superior soft tissue characteristics. It offers large amounts of thin pliable skin that conforms well to the native contours for the recipient site (Fig. 13), is relatively easy to harvest concurrently with the extirpative procedure, has a long vascular pedicle with large-caliber vessels, has predictable innervation for reestablishing local sensation, and has minimal donor site morbidity. The RFFF was also described early on as an osteocutaneous flap (OCRFFF) with harvest of a vascularized portion of the radius bone.12 Despite this significantly broadened applicability of the OCRFFF, its widespread acceptance as an option for single-stage reconstruction of composite defects in the head and neck has been limited by two issues.
Figure 13.
Well-healed thin osteocutaneous radial forearm free flap skin paddle reconstructing the left tonsillar fossa soft palate and retromolar trigone mucosa.
First, the amount of the radius bone grafts available is limited in length and caliber. The length of bone safely harvested without significant forearm dysfunction is limited by the attachments of the PT muscle proximally and brachioradialis muscle distally. This exact length depends on the patient's stature. Our longest bone graft was 12 cm, less than that typically available from the fibular osteocutaneous free flap.13 However, this has been adequate for reconstruction of segmental mandibular defects that are less than the hemimandible in size (Fig. 14). In addition, the thickness of the bone graft is limited to 50% of the radius circumference. We have found this adequate to retain monocortical screws for stabilization to the lingual surface of a locking reconstruction plate (Fig. 15). Unfortunately, this thickness is still inadequate to support osseointegrated dental implants.14 Dental implantation is generally not covered by third-party payers or Medicare at this time and is not an option for many of our head and neck cancer patients who have limited resources. We have been successful in the placement of tissue-borne prosthesis and the reestablishment of mastication.
Figure 14.
Lateral segmental mandibulectomy (4 to 6 cm) for oral cancer resection is the type of the defect that lends itself particularly well to reconstruction by osteocutaneous radial forearm free flap.
Figure 15.
Two osteocutaneous radial forearm free flap bone fragments in place, after one wedge-shaped subperiosteal osteotomy is performed on the radius bone graft.
The second and more worrisome issue is that of donor site morbidity following OCRFFF harvest. Early published series demonstrated donor radius fracture rates ranging up to 67%.6 In 1999, Thoma et al reported a 15% fracture incidence in 60 consecutive patients over a 11-year period.15 Many of these arms were prophylactically immobilized, and fractures were treated with a variety of methods ranging from prolonged immobilization to vascularized bone graft reconstructions.
To strengthen the radius, a logical option was prophylactic internal fixation. At our institution, initial studies of prophylactic plate fixation in matched pairs of fresh human radii revealed that the plated bones were 64% and 70% as strong as intact bones to bending and torsional forces, respectively.16 As described by Werle et al, our clinical experience has confirmed these laboratory results, with arm function measuring 84% or better than the unoperated arm and the absence of any clinically significant or symptomatic radius fractures.10 The five radiographically detectable fractures were all thought to be due to the placement of monocortical screws within the donor bone defect, a practice abandoned in the subsequent 39 consecutive patients (Fig. 16). There have been no further fractures detected using the technique described above. Only one patient required removal of her forearm hardware secondary to an attritional extensor tendon tear on the distal end of a fixation plate placed too ulnarly. Essentially, donor site morbidity after OCRFFF using this technique has been limited to that observed routinely during harvest of the common fasciocutaneous RFFF.
Figure 16.
Current technique of proper prophylactic plating of the donor radius arm. Note that the plate is placed partially over the defect and partially over the remaining radius bone, with two bicortical screws placed distally, three bicortical screws placed proximally, and no screws placed in the defect cavity.
CONCLUSION
The OCRFFF offers high-quality soft tissue and adequate bone for many uses in head and neck reconstruction. The modified OCRFFF harvest and prophylactic internal fixation technique may eliminate the problem of postoperative pathological fracture of the donor radius without any additional morbidity.
References
- Tsue T T, Desyatnikova S S, Deleyiannis F WB, et al. Comparison of cost and function in reconstruction of the posterior oral cavity and oropharynx. Free vs pedicled soft tissue transfer. Arch Otolaryngol Head Neck Surg. 1997;123:731–737. doi: 10.1001/archotol.1997.01900070075012. [DOI] [PubMed] [Google Scholar]
- Soutar D S, McGregor I A. The radial forearm flap in intraoral reconstruction: the experience of 60 consecutive cases. Plast Reconstr Surg. 1986;78:1–8. doi: 10.1097/00006534-198607000-00001. [DOI] [PubMed] [Google Scholar]
- Vaughan E D. The radial forearm free flap in orofacial reconstruction. Personal experience in 120 consecutive cases. J Craniomaxillofac Surg. 1990;18:2–7. doi: 10.1016/s1010-5182(05)80596-7. [DOI] [PubMed] [Google Scholar]
- Urken M L, Weinberg H, Vickery C, et al. The combined sensate radical forearm and iliac crest free flaps for reconstruction of significant glossectomy-mandibulectomy defects. Laryngoscope. 1992;102:543–558. doi: 10.1288/00005537-199205000-00014. [DOI] [PubMed] [Google Scholar]
- Nakatsuka T, Harii K, Yamada A, Ueda K, Ebihara S. Dual free flap transfer using forearm flap for mandibular reconstruction. Head Neck. 1992;14:452–458. doi: 10.1002/hed.2880140605. [DOI] [PubMed] [Google Scholar]
- Matthews R N, Fatah F, Davies D M, Eyre J, Hodge R A, Walsh-Waring G P. Experience with the radial forearm flap in 14 cases. Scand J Plast Reconstr Surg. 1984;18:303–310. doi: 10.3109/02844318409052855. [DOI] [PubMed] [Google Scholar]
- Timmons M J, Missotten F E, Poole M D, Davies D M. Complications of radial forearm flap donor sites. Br J Plast Surg. 1986;39:176–178. doi: 10.1016/0007-1226(86)90078-0. [DOI] [PubMed] [Google Scholar]
- Nuckols D A, Tsue T T, Toby E B, Girod D A. Preoperative evaluation of the radial forearm free flap patient with the objective Allen's test. Otolaryngol Head Neck Surg. 2000;123:553–557. doi: 10.1067/mhn.2000.110728. [DOI] [PubMed] [Google Scholar]
- Urken M L. Radial forearm. In: Urken M L, Cheney M L, Sullivan M J, Biller H F, editors. Atlas of Regional and Free Flaps for Head and Neck Reconstruction. New York: Raven Press; 1995. pp. 149–168. [Google Scholar]
- Werle A H, Tsue T T, Toby E B, Girod D A. Osteocutaneous radial forearm free flap: its use without significant donor site morbidity. Otolaryngol Head Neck Surg. 2000;123:711–717. doi: 10.1067/mhn.2000.110865. [DOI] [PubMed] [Google Scholar]
- Yang G, Chen B, Gao Y, et al. Forearm free skin flap transplantation. Natl Med J China. 1981;61:139. [Google Scholar]
- Soutar D S, Scheker L R, Tanner N SB, McGregor I A. The radial forearm flap: a versatile method for intra-oral reconstruction. Br J Plast Surg. 1983;36:1–8. doi: 10.1016/0007-1226(83)90002-4. [DOI] [PubMed] [Google Scholar]
- Hidalgo D A. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg. 1989;84:71–79. [PubMed] [Google Scholar]
- Moscoso J F, Keller J, Genden E, et al. Vascularized bone flaps in oromandibular reconstruction. A comparative anatomic study of bone stock from various donor sites to assess suitability for enosseous dental implants. Arch Otolaryngol Head Neck Surg. 1994;120:36–43. doi: 10.1001/archotol.1994.01880250032004. [DOI] [PubMed] [Google Scholar]
- Thoma A, Khadaroo R, Grigenas O, et al. Oromandibular reconstruction with the radial-forearm osteocutaneous flap: experience with 60 consecutive cases. Plast Reconstr Surg. 1999;104:368–378. discussion 379–380. doi: 10.1097/00006534-199908000-00007. [DOI] [PubMed] [Google Scholar]
- Edmonds J L, Bowers K W, Toby E B, Jayaraman G, Girod D A. Torsional strength of the radius after osteofasciocutaneous free flap harvest with and without primary bone plating. Otolaryngol Head Neck Surg. 2000;123:400–408. doi: 10.1067/mhn.2000.109474. [DOI] [PubMed] [Google Scholar]