Abstract
Frontal sinus and supraorbital rim fractures are common in facial trauma patients. Coronal incision is the standard approach for surgical management of these injuries. Nevertheless, with this incision, complications can occur as wide scars and alopecia. Because surgical repair of fronto-orbital fractures is often indicated for aesthetic reasons, surgical incision might be an “aesthetic incision.” So we have adopted the pretrichial incision, already used in brow-lift and foreheadplasty but never described in craniomaxillofacial trauma surgery. Nineteen upper-third facial trauma patients were treated: five cases were approached via an existing laceration, four cases via a coronal incision, and 10 cases via a unilateral zigzag pretrichial incision. To assess the postsurgical scar, the Patient and Observer Scar Assessment Scale was used and the scar's width was measured. In all cases, a wide surgical field was obtained to perform correct fracture reduction. Unlike straight or stealth coronal incisions, with pretrichial incision no wide scar or alopecia was registered. We think that pretrichial incision is an aesthetically reasonable alternative to the standard coronal approach for craniomaxillofacial trauma patients.
Keywords: Pretrichial hairline incision, coronal incision, frontal sinus fracture, surgical facial approach, facial trauma
Fractures of the frontal sinus and orbit are relatively common in facial trauma patients (5 to 15% of all maxillofacial trauma) and are associated with high-velocity injuries such as motor vehicle accidents, assaults, and sporting events.1 Generally, they occur in adults between 20 and 40 years of age and can result in significant ophthalmologic and cosmetic morbidity.2 The coronal incision is the standard approach in craniomaxillofacial surgery, first used in the treatment of congenital craniofacial deformity and in neurosurgical procedures. As management of craniomaxillofacial fractures evolved with increased indications for wide exposure of the operative field, rigid internal fixation, and primary bone grafting, this approach became more frequent. However, in numerous patients, complications due to this approach, such as anesthesia or paresthesia of the scalp, wide and irregular incision scars, temporary or permanent alopecia, were indicated as unavoidable.3 To decrease this morbidity, some authors modified the straight-line coronal incision using other incisions such as the “stealth incision,” or, in older patients with deep forehead creases, the mid-forehead and “gull wing” incisions.4,5 However, the same complications were described. We are convinced that one of the most important considerations in craniomaxillofacial surgery must be the postoperative appearance of the final scar, which will undoubtedly have social implications. Because surgical reduction of the facial upper-third fractures is often indicated to reestablish an aesthetic facial contour, we think that the surgeon must constantly strive to produce the most aesthetically pleasing incision to create the best surgical scar.
Therefore, the surgical incision must be an aesthetic incision. Keeping this concept in mind, together with the principle of facial aesthetic units, we used the pretrichial incision, already well described by Marten in aesthetic surgery, to successfully perform surgical repair of facial upper-third fractures.6,7 Doing online bibliographical researches, no study was found about the use of the pretrichial incision in craniofacial trauma surgery. So we can say that our work first describes this incision in trauma surgery.
PATIENT AND METHODS
Nineteen patients with facial upper-third fractures were admitted to our department from January 2005 to November 2008. All patients were males, between 13 and 52 years of age, and the etiologies of the fractures were motor vehicle collisions in 12 cases, sport accidents in four cases, and assaults in three cases. Isolated frontal sinus anterior table fracture occurred in eight cases; frontal sinus anterior table fracture associated with orbital roof fracture occurred in eight cases. In three remaining cases, the frontal sinus fracture was associated with other facial fractures (i.e., naso-orbital fractures and Le Fort II fracture). In the last three cases, there was also nasofrontal drainage system involvement along with dural lacerations. All patients required semiacute surgical treatment of the fractures. Five cases were approached via an existing laceration. Fourteen required a surgical incision. A coronal flap was used in the first four cases (a straight incision in one case and a stealth incision in three cases), and a unilateral pretrichial incision was used to approach the 10 consecutive cases. In three cases approached by pretrichial incision, a combined neurosurgical-maxillofacial team was necessary. In one case, we required the use of cranial bone grafts to reconstruct the frontal sinus anterior wall: from a unilateral pretrichial incision, we harvested such grafts easily. To assess the postsurgical scar, the Patient and Observer Scar Assessment Scale was used, and the scar's width was measured.8 Two maxillofacial residents and one medical student, blinded to each other's assessment, scored all scars. Two exhaustive cases with facial upper-third fractures successfully treated by using the unilateral pretrichial incision are described as follows.
A 22-year-old man was referred to our department for a craniofacial trauma caused by a sport accident. The patient presented a visible and palpable frontal bone depression, periorbital ecchymosis, and eyelid ptosis (Fig. 1). A computed tomography (CT) scan showed displaced frontal sinus anterior table fracture associated with orbital roof fracture with intact nasofrontal drainage system (Fig. 2). The fractures were treated through a unilateral zigzag pretrichial incision exposing a wide surgical field allowing open reduction and internal rigid fixation (Fig. 3). A postoperative CT scan showed a good restored bone contour (Fig. 4). Surgical incision healed without complications (Fig. 5), and after 20 months of follow-up, scar is quasi invisible (Fig. 6).
Figure 1.
Preoperative frontal view of the patient affected by left frontal sinus anterior table fracture associated with orbital roof fracture (left). Preoperative oblique view of the same patient (right).
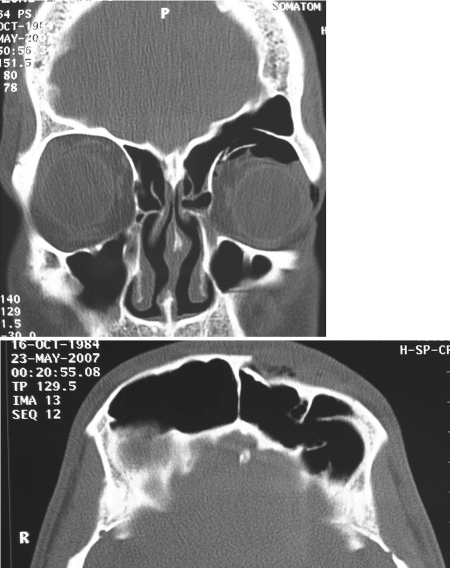
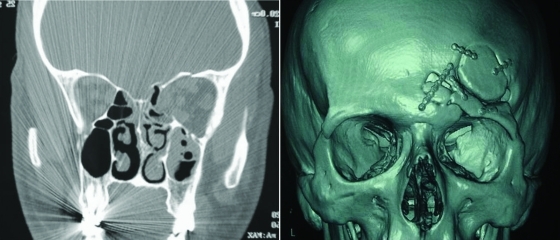
Figure 2.
Preoperative coronal and axial computed tomography images.
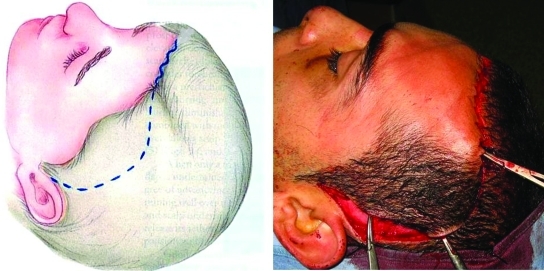
Figure 3.
Preoperative design for pretrichial incision (left). Wide surgical field and proper reduction and fixation of anterior frontal sinus wall fracture (right).
Figure 4.
Postoperative coronal and axial computed tomography images.
Figure 5.
Progressive phases of scar healing.
Figure 6.
Excellent aesthetic result after 20 months of follow-up.
A 30-year-old man with male pattern baldness was referred to our department for a craniomaxillofacial trauma caused by a motorcycle accident. He presented left periorbital ecchymosis and edema, subconjunctival hemorrhage, eyelid ptosis, eyelid lacerations, enophthalmos, and pain during eye movements, along with diplopia (Fig. 7). A CT scan showed displaced fracture of left frontal sinus anterior wall, nondisplaced fractures of frontal sinus posterior wall, and blowout fractures of the inferior, medial, and superior left orbital walls with dural laceration, needing combined neurosurgical and maxillofacial repairs (Fig. 8). With a left unilateral zigzag pretrichial incision, we were able to widely expose the frontal sinus anterior wall fracture. Through a craniotomy, performed by a neurosurgeon, the damaged left orbital roof was reduced. The frontal sinus was then obliterated with abdominal fat and stabilized with microplates and screws (Fig. 9). Finally, inferior and medial orbital walls were reconstructed with polyethylene implants (Medpor, Strykez Corporation, Newnan, Georgia) using a Lynch incision and a transconjunctival incision. A postoperative CT scan confirmed a correct surgical reduction (Fig. 10). The pretrichial incision healed without aesthetic complications (Fig. 11) and after 30 months of follow-up, the scar is insignificant (Fig. 12).
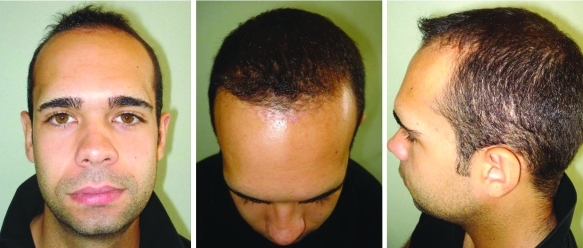
Figure 7.
Preoperative oblique view (left). Close-up view of preoperative frontal hairline in a male pattern baldness (right).
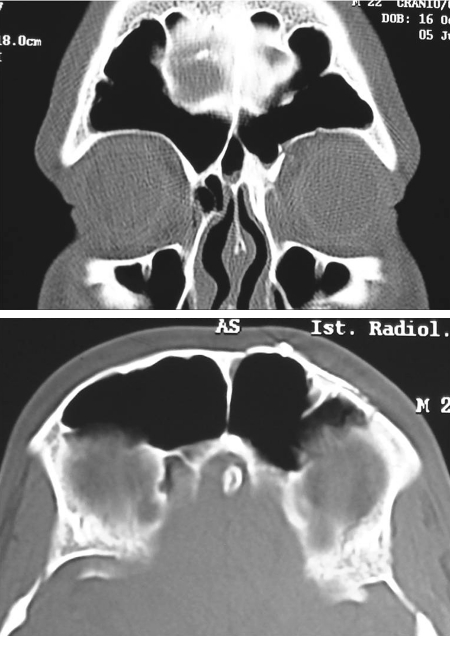
Figure 8.
Preoperative coronal and axial computed tomography images.
Figure 9.
Surgical pretrichial incision (above, left). Surgical field after frontal craniotomy: reduction and fixation of the orbital roof with suture Vicryl (Ethicon Inc., Johnson and Johnson, Somerville, NJ) 3.0 (above, right). Obliteration of the frontal sinus with abdominal fat (below, left). Repositioning of the frontal cranial flap after reduction and fixation of the fractures of the frontal sinus anterior wall and folding of the orbital roof with a galeal flap (below, right).
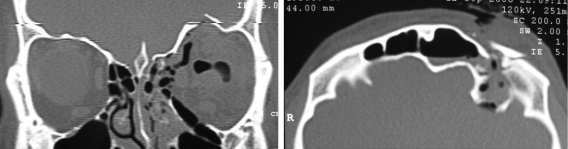
Figure 10.
Case 8. Postoperative coronal and 3-D computed tomography images.
Figure 11.
Case 8. Progressive phases of scar healing.
Figure 12.
Case 8. Excellent aesthetic result after 30 months of follow-up.
Surgical Technique
The site for pretrichial incision is usually marked after sedation but before local anesthetic is injected. Hair shaving is not performed. The incision begins laterally as a preauricular incision and continues along the temporal scalp as a hemicoronal incision. In proximity of the superior temporal fusion line of the skull, it turns forward along the frontal hairline following a zigzag pattern just within the most anterior portion of the hairline and ending just beyond the midline (Fig. 13). This zigzag incision is also used in case of male pattern baldness: in fact, the frontal hairline, representing the upper boundary of the forehead unit and lying between the forehead and the scalp, is always visible, because the cutaneous texture and color of forehead and scalp are very different from each other. The incision is performed with a No. 15 scalpel perpendicular to the hair follicles. Keeping in mind that hair follicles in the temporal area are oriented in a posterior and inferior direction but in the frontal hairline are oriented in an anterior and inferior direction, the scalpel slant must be changed: 30 to 45 degrees forward slant in the temporal area and 30 to 45 degrees backward slant in the frontal area9 (Fig. 14). The forehead flap is then harvested, and the frontal branch of the facial nerve is protected as usual.10 After a wide exposure of the operative field, careful hemostasis with electrocautery is performed, avoiding injuries to hair follicles. Raney clips can be used for hemostasis depending on surgeon preference. After correct reduction and fixation of the fracture, a suction drainage is positioned. Tension-free suture of the prehairline incision line is accomplished with a layered closure by using 5–0 nylon in a simple interrupted manner as for the skin. A double relaxation suture of the galea or the temporoparietal fascia with nonabsorbable suture followed by a superficial skin closure with stapler suture or 4–0 nylon epidermal suture is performed in the temporal area, where alopecia or scar widening is more severe and frequent.11 Suction drainage is usually removed after 3 days and superficial skin suture after 10 days.
Figure 13.
Plan for pretrichial incision.
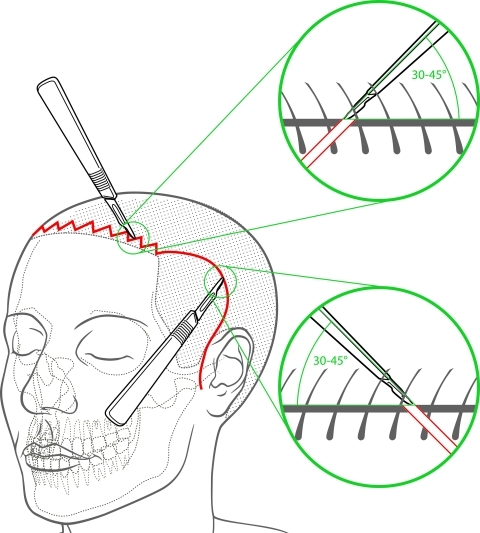
Figure 14.
To make surgical incision perpendicular to the hair follicles, the scalpel is slanted 30 to 45 degrees forward in the frontal area and 30 to 34 degrees backward in the temporal area.
RESULTS
With the unilateral zigzag pretrichial incision, we got a greater exposure of the frontal prominence, the supraorbital rim, the glabellar area, and the malar eminence, usually obtained with a standard coronal incision. Compared with the coronal incision, operative time increased slightly (a few minutes) and the operative blood loss was similar.
Excellent aesthetic results with regard to a good restored bone profile and to a quasi-invisible scar were recorded in all 10 patients undergoing the pretrichial incision, even in three patients with male pattern baldness. A high level of the patient satisfaction and an excellent observer's overall opinion were obtained.
DISCUSSION
The isolated frontal sinus anterior table fractures and supraorbital rim fractures or other associated facial lesions are associated with high-energy craniomaxillofacial trauma, and they generally occur in young adults between 20 and 40 years of age, representing the cohort of working and socially active people in whom cosmetic morbidity can cause a significant handicap.1,2 Consequently, surgical reduction of facial upper-third fractures is often indicated to correct aesthetic defects arising from an altered bone profile in young patients. However, the price these patients pay in the location and appearance of the incision line is great. Patients having thinning hair or who keep their hair very short or shaved would often prefer a small depression in the lower forehead to a 10-inch coronal scar across the top of the head. Facial upper-third fractures are approached, where possible, through an existing laceration, but if there are no lacerations, or a wider surgical field is necessary, or neurosurgical time is mandatory, the problem of the best surgical approach becomes urgent. Hemicoronal incision gives poor exposure and frequently has to be extended toward the upper forehead to provide exposure of relevant anatomy. Coronal incision is the standard approach in craniofacial traumatic surgery, but this straight-line incision often leaves a very noticeable scar.3 To decrease morbidity, Munro and Fearon changed the straight-line coronal incision in a zigzag coronal incision, which they called a “stealth incision.”5 This incision appeared immediately less visible compared with the conventional coronal one especially if the patient had long hair. However, complications like wide scars or alopecia, caused by these two standard incisions, can often result in an iatrogenic deformity more severe than the injury itself. Because surgical treatment of facial upper-third fractures must also answer to strict aesthetic demands, we are convinced that a surgical incision must be an “aesthetic incision.” Considering this, along with the principle of facial aesthetic units, we have chosen to adopt the zigzag unilateral pretrichial incision.6,7 This incision, resulting in a concealed scar along the frontal hairline, was performed for the first time as an access for frontal rhytidectomy with wonderful aesthetic results, but so far has never been described in craniofacial trauma surgery. The frontal arm of pretrichial incision must be made as a random zigzag line following hairline undulations (Fig. 15). This results in a more natural transition from forehead skin to scalp, thus avoiding a “wig appearance.” Moreover, a zigzag incision produces both an extensible and mobile scar because minimal tension is distributed in an irregular manner.6,7
Figure 15.
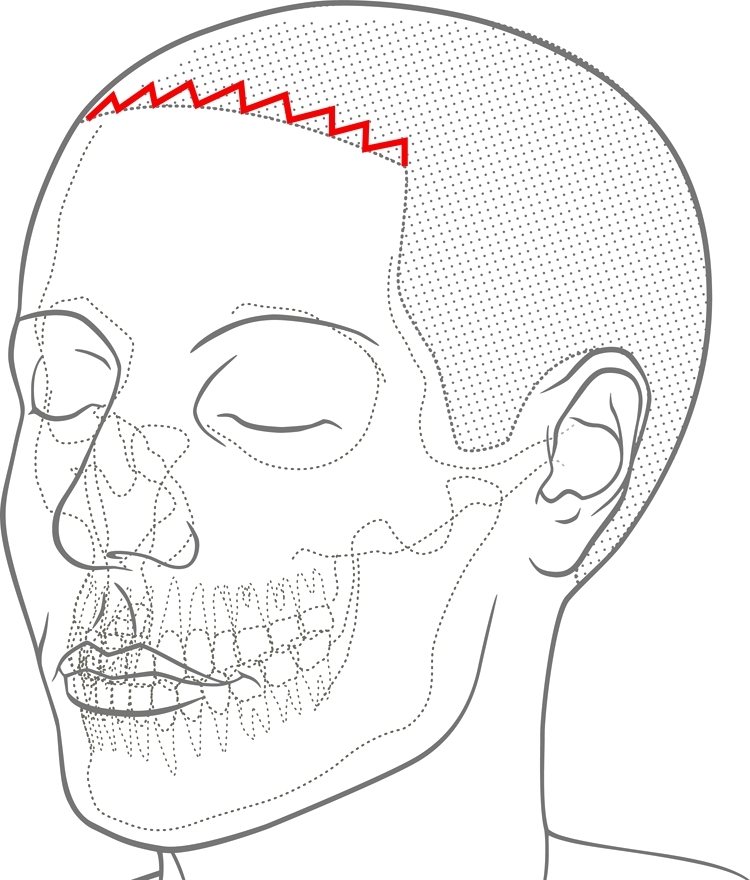
The frontal arm of the pretrichial incision must be made as a random zigzag line just within the fine hair along the hair line, following its natural undulations.
Hair follicle orientation observation is of major importance before incisions are performed. As Camirand and Doucet demonstrated, during forehead-lifts, anterior hairline scars can be improved by making hairline incisions perpendicular to the hair follicles rather than parallel to them, because the incisions perpendicular to hair follicles cut them and are able to produce hair growth through and in front of the scar, with a more aesthetic and natural postoperative result compared with the parallel incision.12 To preserve deep papillae and the deep part of the follicles, the incision is performed with a scalpel slanted between 30 and 45 degrees to the surface of the scalp and perpendicular to the hair follicles, keeping in mind that hair follicles have different orientation and direction of growth.6,7,12 Usually, in the temporal area, they are oriented in a posterior and inferior direction, and in the frontal hairline, they are oriented in an anterior and inferior direction.9 For this reason, passing from the temporal to the frontal area, the scalpel slant is changed: 30 to 45 degrees forward slant in the temporal area and 30 to 45 degrees backward slant in the frontal area. Another advantage is that, if a straight-line coronal incision is used, some type of marker should be placed along the incision to assist with symmetric closure of the scalp.
Indeed, a correct suture of skin margins of the entire wound has become easier to perform thanks to the microzigzag incisions in all our patients. Bearing in mind facial aesthetic units, and aware of the good aesthetic results obtained in hairy patients, we also used the pretrichial incision in three patients with a male pattern baldness. The hairline represents the upper boundary of the forehead unit and lies between the forehead and the scalp. It is always visible, also in patients with male pattern baldness or fine sparse hair, because the cutaneous texture and color of forehead and scalp are very different from each other. So, by hiding the incision along the hairline, the natural border of forehead unit, the final scar is less visible even in these patients, because it is perceived as normal facial topography. In all those cases where the unilateral zigzag pretrichial incision was used, correct reduction and fixation of all the frontal fractures were performed by means of only one unilateral incision. We gain a greater exposure of the frontal prominence, the supraorbital rim, the glabellar area, and the malar eminence, usually obtained with a standard coronal incision, because we lower the pivot point of the forehead flap thanks to the frontal hairline arm and the preauricular arm of the unilateral pretrichial incision.
Wonderful cosmetic results with a quasi-invisible scar were obtained and high level of the patient overall satisfaction was registered. For these reasons, we think that the zigzag unilateral pretrichial incision is an aesthetically possible alternative to the standard coronal approach for craniomaxillofacial trauma patients.
References
- Strong E B. Frontal sinus fractures: current concepts. Craniomaxillofac Trauma Reconstruction. 2009;2:161–175. doi: 10.1055/s-0029-1234020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell R B, Dierks E J, Brar P, Potter J K, Potter B E. A protocol for the management of frontal sinus fractures emphasizing sinus preservation. J Oral Maxillofac Surg. 2007;65:825–839. doi: 10.1016/j.joms.2006.05.058. [DOI] [PubMed] [Google Scholar]
- Shepherd D E, Ward-Booth R P, Moos K F. The morbidity of bicoronal flaps in maxillofacial surgery. Br J Oral Maxillofac Surg. 1985;23:1–8. doi: 10.1016/0266-4356(85)90072-5. [DOI] [PubMed] [Google Scholar]
- Cheney M L, Gliklich R, Li K K, Topf P, Montgomery W. Midforehead incision: an approach to the frontal sinus and upper face. J Craniofac Surg. 1995;6:408–411. [PubMed] [Google Scholar]
- Munro I R, Fearon J A. The coronal incision revisited. Plast Reconstr Surg. 1994;93:185–187. doi: 10.1097/00006534-199401000-00031. [DOI] [PubMed] [Google Scholar]
- Marten T J. Hairline lowering during foreheadplasty. Plast Reconstr Surg. 1999;103:224–236. doi: 10.1097/00006534-199901000-00037. [DOI] [PubMed] [Google Scholar]
- Marten T. Open foreheadplasty. In: Knize D M, editor. The Forehead and the Temporal Fossa: Anatomy and Technique. Lippincott, Philadelphia, PA: Williams & Wilkins; 2001. pp. 154–187. [Google Scholar]
- de Kar A L van, Corion L UM, Smeulders M JC, Draaijers L J, der Horst C MAM van, Zuijlen P PM van. Reliable and feasible evaluation of linear scars by the Patient and Observer Scar Assessment Scale. Plast Reconstr Surg. 2005;116:514–522. doi: 10.1097/01.prs.0000172982.43599.d6. [DOI] [PubMed] [Google Scholar]
- Mowlavi A, Majzoub R K, Cooney D S, Wilhelmi B J, Guyuron B. Follicular anatomy of the anterior temporal hairline and implications for rhytidectomy. Plast Reconstr Surg. 2007;119:1891–1895. discussion 1896. doi: 10.1097/01.prs.0000259191.59277.7a. [DOI] [PubMed] [Google Scholar]
- Al-Kayat A, Bramley P. A modified pre-auricular approach to the temporomandibular joint and malar arch. Br J Oral Surg. 1979–80;17:91–103. doi: 10.1016/s0007-117x(79)80036-0. [DOI] [PubMed] [Google Scholar]
- Burm J S, Oh S J. Prevention and treatment of wide scar and alopecia in the scalp: wedge excision and double relaxation suture. Plast Reconstr Surg. 1999;103:1143–1149. doi: 10.1097/00006534-199904040-00007. [DOI] [PubMed] [Google Scholar]
- Camirand A, Doucet J. A comparison between parallel hairline incisions and perpendicular incisions when performing a face lift. Plast Reconstr Surg. 1997;99:10–15. doi: 10.1097/00006534-199701000-00002. [DOI] [PubMed] [Google Scholar]