Abstract
Radiofrequency (RF) ablation has been increasingly utilized as a minimally invasive treatment for primary and metastatic liver tumors, as well as tumors in the kidneys, bones, and adrenal glands. The development of high-current RF ablation has subsequently led to an increased risk of thermal skin injuries at the grounding pad site. The incidence of skin burns in recent studies ranges from 0.1–3.2% for severe skin burns (second-/third-degree), and from 5–33% for first-degree burns.1–3
Keywords: Colorectal cancer, radiofrequency ablation, complications
CASE REPORT
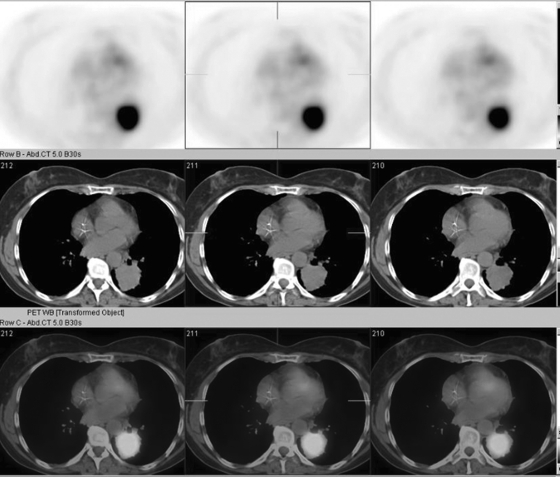
A 58-year-old woman with metastatic colorectal cancer was found to have a growing metastatic lung mass. Positron emission tomography–computed tomography (PET–CT) demonstrated a large hypermetabolic left lower lobe mass (Fig. 1). Upon review of various therapeutic options, the decision was made to proceed with percutaneous RF ablation.
Figure 1.
Positron emission tomography–computed tomography (PET–CT) demonstrates a hypermetabolic mass within the left lower lobe.
Percutaneous RF ablation was performed under CT guidance and conscious sedation (Fig. 2). The treatment was performed with a standard protocol using a cool-tip RF ablation system (Valley Laboratory, Covidien, Mansfield, MA). Grounding pads were placed and appropriately positioned on the anterior aspect of both thighs with the long axis perpendicular to the RF ablation electrode. The total pad surface area was 480 cm2. A cluster electrode was centered within the lung mass. Three ablation cycles covering different portions of the tumor, each lasting 12 minutes, were performed. The grounding pads were firmly and correctly applied to the patient's skin throughout the procedure and were adherent to the skin after electrode removal.
Figure 2.
Axial prone noncontrast computed tomography demonstrates appropriate electrode positioning within the mass.
There were no intraprocedural or immediate postprocedural complications, and the patient tolerated the procedure well. While in recovery in the Interventional Radiology (IR) holding area, the patient complained of pain on her anterior right thigh. On physical exam, there was a large, flaccid bulla with surrounding pink inflammation at the leading edge of previously placed grounding pads. The bulla was immediately covered with silver sulfadiazine ointment (Fig. 3). The wound management team was consulted for in-house care and subsequent outpatient management.
Figure 3.
Large flaccid bulla with surrounding pink inflammation and topical silver sulfadiazine ointment at day 1.
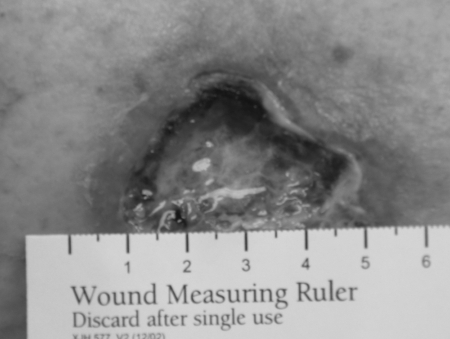
Over the following months, the bulla progressed to a large, 4-cm ulceration extending to the subcutaneous tissue (Figs. 4 and 5). Delayed postburn blistering and full-thickness ulceration were indicative of a third-degree burn. The patient underwent debridement of loose tissue and application of daily silver sulfadiazine ointment and nonadhesive dressings. Skin grafting was not indicated. The ulceration took over 9 months to heal completely, ultimately with significant scar formation.
Figure 4.
Superficial erosions with adherent denuded epidermis and hemorrhagic crust at day 60.
Figure 5.
Full thickness ulceration with pink undermined borders and visible subcutaneous tissue at the base on day 90.
DISCUSSION
RF ablation has proven to be safe and effective for the treatment of malignant tumors in various patients who are nonsurgical candidates. Thermal injuries at the grounding pad site have been increasingly reported with the use of higher current and more powerful systems. The incidence of skin burns in recent studies ranges from 0.1–3.2% for severe skin burns (second-/third-degree) and from 5–33% for first-degree burns.1,2,3 In this case, the grounding pads were appropriately applied, as per equipment protocol, with full-skin contact throughout the procedure. Although extensive discussion took place with the vendor, no definitive conclusion as to the etiology of the burn was obtained.
Monopolar RF systems use grounding pads to complete the RF circuit. The same amount of energy is deposited at the tip of the electrode as the skin pads. The much larger surface area of the grounding pads is used to disperse the large heat loads. Published guidelines in 2000 by Goldberg et al4 have limited the incidence of the more severe, second- and third-degree burns. The guidelines recommend using sufficiently large surface area foil grounding pads oriented to maximize the leading edge of the grounding pad. Placement of the pads is equally as important. The leading edge is the area of maximum power concentration, which led to the recommendation that the side of the pad with the biggest edge should face the active electrode.
RF ablation procedures are frequently performed under general anesthesia; therefore, the diagnosis of skin pad burns is often delayed until after the procedure when grounding pads are removed and the patient complains of pain, or obvious epidermal changes are noted on physical exam. At this point, cutaneous injury and damage is irreversible. One possible method for the prevention of skin burns is to use a dispersive electrode that measures underlying skin temperature throughout the procedure to prevent severe thermal injury while still reversible.5,6 Dissipation of heat from the skin occurs primarily by conduction of heat away from the site through blood, as well as by convection of heat into the surrounding tissues. Patients with decreased peripheral circulation due to peripheral vascular disease, or hypothermia-induced vasoconstriction, are at a theoretical increased risk of RF ablation grounding pad-related skin burns.
Treatment of grounding pad skin burns requires long-term follow-up in a wound care or dermatologic clinic, usually on the order for several months to years. Length of treatment and time to heal depend both on the size and depth of injury, as well as comorbid patient conditions affecting wound healing, such as peripheral vascular disease, diabetes mellitus, and immunosuppression. The morbidity and mortality associated with severe thermal injuries are primarily related to superinfection with both bacterial and fungal organisms. Topical silver sulfadiazine and debridement of loose tissue can help minimize the risk of superinfection. Deep second- and third-degree burns that are slow to heal may require autologous or allogenic epidermal grafts. Unfortunately, any thermal injury extending beyond the epidermis (superficial/deep second- and third-degree) will involve the cutaneous appendages and ultimately result in scar formation.7
The existing grounding pad technology and design is a limiting factor for further increases in RF power. Multiple methods to reduce skin heating, including increasing the surface area of the grounding pads, increasing the number of pads, and using sequential activation of the pads,8 have been reported with good results.
With respect to skin pad burns, there is increased morbidity and time needed to heal in patients with underlying medical diseases, such as immunosuppression, diabetes, peripheral vascular disease, as well as venous stasis. This patient demographic accounts for a large proportion of patients undergoing RF ablation. Fortunately, our patient had none of the above comorbidities, and healed well without further complication or need for a skin graft.
In conclusion, the increasing utilization of RF ablation to treat various nonsurgical tumors has led to clinical demand for more powerful and efficient systems, which has increased the risk of skin burns at the grounding pad site. Although the reported incidence of severe third-degree burns is low, these are significant complications with associated morbidity, mortality, and need for long-term follow-up and wound care. As illustrated in our case report, even when all appropriate guidelines and protocols are followed, there is still a risk of skin burn at the grounding pad site, which raises the possibility of pad malfunction. Further work needs to be done to eliminate this unnecessary complication.
References
- Mulier S, Mulier P, Ni Y, et al. Complications of radiofrequency coagulation of liver tumours. Br J Surg. 2002;89(10):1206–1222. doi: 10.1046/j.1365-2168.2002.02168.x. [DOI] [PubMed] [Google Scholar]
- Rhim H. Complications of radiofrequency ablation in hepatocellular carcinoma. Abdom Imaging. 2005;30(4):409–418. doi: 10.1007/s00261-004-0255-7. [DOI] [PubMed] [Google Scholar]
- Steinke K, Gananadha S, King J, Zhao J, Morris D L. Dispersive pad site burns with modern radiofrequency ablation equipment. Surg Laparosc Endosc Percutan Tech. 2003;13(6):366–371. doi: 10.1097/00129689-200312000-00003. [DOI] [PubMed] [Google Scholar]
- Goldberg S N, Solbiati L, Halpern E F, Gazelle G S. Variables affecting proper system grounding for radiofrequency ablation in an animal model. J Vasc Interv Radiol. 2000;11(8):1069–1075. doi: 10.1016/s1051-0443(07)61341-4. [DOI] [PubMed] [Google Scholar]
- Thiagalingam A, Pouliopoulos J M, Barry M A, et al. A thermochromic dispersive electrode can measure the underlying skin temperature and prevent burns during radiofrequency ablation. J Cardiovasc Electrophysiol. 2005;16(7):781–788. doi: 10.1111/j.1540-8167.2005.40747.x. [DOI] [PubMed] [Google Scholar]
- Berber E, Flesher N L, Siperstein A E. Initial clinical evaluation of the RITA 5-centimeter radiofrequency thermal ablation catheter in the treatment of liver tumours. Cancer J Sci Am. 2000;6:319–329. [Google Scholar]
- James W D, Berger T G, Elston D M. Andrews' Diseases of the Skin, Clinical Dermatology. 10th ed. Philadelphia: Saunders; 2000. [Google Scholar]
- Schutt D J, Swindle M M, Bastarrika G A, Haemmerich D. Sequential activation of ground pads reduces skin heating during radiofrequency ablation: initial in vivo porcine results. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:4287–4290. doi: 10.1109/IEMBS.2009.5332714. [DOI] [PMC free article] [PubMed] [Google Scholar]