Abstract
Hepatocellular carcinoma (HCC), the major form of primary liver cancer, is one of the most deadly human cancers. The pathogenesis of HCC is frequently linked with continuous hepatocyte death, inflammatory cell infiltration and compensatory liver regeneration. Understanding the molecular signaling pathways driving or mediating these processes during liver tumorigenesis is important for the identification of novel therapeutic targets for this dreadful disease. The classical IKKβ-dependent NF-κB signaling pathway has been shown to promote hepatocyte survival in both developing and adult livers. In addition, it also plays a crucial role in liver inflammatory responses by controlling the expression of an array of growth factors and cytokines. One of these cytokines is IL-6, which is best known for its role in the liver acute phase response. IL-6 exerts many of its functions via activation of STAT3, a transcription factor found to be important for HCC development. This review will focus on recent studies on the roles of NF-κB and STAT3 in liver cancer. Interactions between the two pathways and their potential as therapeutic targets will also be discussed.
Keywords: NF-κB, STAT3, signaling transduction, inflammation, carcinogenesis, liver cancer, HCC
Introduction
Nearly 25 years ago, Dvorak recognized that the composition of the tumor stroma is very similar to that of granulation tissue of healing skin wounds. He therefore suggests that tumors are wounds that do not heal 1. Careful examination of the many phases of wound healing and tumorigenesis reveals even more extensive similarities between these two processes 2. Importantly, the human body mounts inflammatory responses in both situations aiming to clear dead cells and restore the tissue integrity 2. However, unlike the normal wound healing process that is tightly regulated both in extent and in duration, the inflammatory response during cancer development is not self-limited.
It is estimated that about 15% of human cancers are associated with chronic infections and inflammation 3. The best examples of inflammation- and infection-associated cancers include colon cancer and inflammatory bowel diseases, gastric cancer and chronic Helicobacter pylori infection 4, and hepatocellular carcinoma (HCC) following chronic hepatitis virus infection 5. Persistent infections and inflammation in these organs lead to continuous cell death and long-lasting local infiltration of inflammatory cells 3. Even those cancers, whose development is not associated with pre-existing infection or inflammation, are accompanied by massive inflammatory cell recruitment into the tumor, a phenomenon which led Virchow to his original suggestion that inflammation and cancer are linked 6. This inflammatory response is likely caused by necrotic cell death in the core of rapidly growing tumor mass due to lack of oxygen and nutrients. Continuous cell death and inflammatory cell infiltration during cancer development are accompanied with production of a great number of cytokines, chemokines and growth factors, favoring increased cellular proliferation 3. In addition, reactive oxygen and nitrogen species generated by both oncogene-expressing cells and inflammatory cells could cause oxidative damage to host DNA, resulting in activation of oncogenes and/or inactivation of tumor suppressor genes and various epigenetic changes that favor tumor progression. Therefore, etiologies that influence either cell survival or ensuing inflammatory responses are likely to have an impact on the course of tumor development.
HCC, which is refractory to nearly all currently available anti-cancer therapies, is the third leading cause of cancer-related deaths worldwide 7. HCC frequently develops in patients who are chronically infected with one of two hepatitis viruses, HBV or HCV 8, 9. Chronic HBV/HCV infection in the liver results in hepatocyte death and inflammatory cell infiltration. Virus-infected hepatocytes are killed by host immune cells as well as by intrinsic cytopathic effects of either HBV or HCV 10, 11. Continuing hepatocyte death triggers long-lasting compensatory liver repair and regeneration and eventually leads to severe liver fibrosis or cirrhosis. Although the mechanisms underlying chronic HBV/HCV infection-induced HCC development are not fully elucidated due to the absence of suitable mouse systems, cycles of hepatocyte death, inflammatory cell infiltration and compensatory regeneration/proliferation in the infected liver are thought to play a crucial role 12.
Multiple signaling pathways are involved in this injury-inflammation-regeneration response and in human HCC development. IKKβ-dependent classical NF-κB signaling, a regulator of cell survival, immunity and inflammation, is one of the more important pathways that is activated during liver injury and inflammation and has been studied quite extensively in mouse models of liver carcinogenesis. STAT3 is another transcriptional factor involved in immune responses, inflammation and tumorigenesis, and was found to be critical for compensatory liver regeneration and chemically-induced HCC development. This review will focus on recent findings regarding the roles of NF-κB and STAT3 signaling in liver injury, inflammation and cancer. Interestingly, the two transcription factors and their activation pathways do not act in isolation and are engaged in extensive crosstalk, which will also be discussed in this review.
IKK/NF-κB signaling pathway in HCC development
NF-κB, a collection of dimeric transcription factors, first identified based on their interaction with the immunoglobulin light-chain enhancer in B cells 13, are present in all cells 14. Seven distinct NF-κB proteins can form a variety of dimers, not all of which are active. These proteins include: NF-κB1 (p105 and p50), NF-κB2 (p100 and p52), RelA (p65), RelB and c-Rel. In non-stimulated cells, most NF-κB dimers are retained in the cytoplasm by binding to inhibitory IκB proteins, except for the dimers formed by p105 and p100, which are inactive and contain intrinsic IκB-like-moieties. In response to proinflammatory stimuli, such as tumor necrosis factor (TNF) or interleukin 1β (IL-1β), the IκB kinase (IKK) complex, composed of the IKKα and IKKβ catalytic subunits and the IKKγ regulatory subunit is activated, resulting in IκB phosphorylation and eventual ubiquitin-mediated degradation, leading to the nuclear entry of freed NF-κB dimmers 15. Of the two catalytic subunits, IKKβ is the one which is most critical for IκB degradation, forming the core of what is known as the classical NF-κB activation pathway. By contrast, IKKα is required for the inducible processing of the inactive p100 protein to its active derivative p52, thus forming the core of the so called alternative NF-κB pathway 15, 16.
A link between NF-κB and cancer first became evident with the cloning of RelA and the realization of its close kinship with the viral oncoprotein v-Rel 17. The view was further supported by observations of activated NF-κB in many human cancers 18. In addition, the Bcl-3 oncogene, activated by chromosomal translocation in B-cell chronic lymphocytic leukemia, was identified as a member of the IκB family 19, 20. More recently, mutations in upstream components of the IKK-NF-κB signaling system were identified in multiple myeloma and are thought to lead to cell autonomous activation of NF-κB, thereby enhancing cell survival and proliferation 21, 22. However, extensive search failed to identify NF-κB-activating mutations in most other cancers and most likely cancer-associated constitutive NF-κB activities are the result of exposure to pro-inflammatory stimuli in the tumor microenvironment.
Hepatocyte IKK-dependent NF-κB signaling suppresses liver cancer development by promoting hepatocyte survival
A key role of NF-κB in liver homeostasis was first revealed by studying RelA/p65 deficient mice, which suffer embryonic lethality with extensive liver apoptosis and degeneration 23. This liver apoptosis is induced by TNF and backcrossing of p65 knockout mice with TNF- or TNF receptor 1 (TNFR1)-deficient mice prevents liver damage and the lethal phenotype 23, 24, 25. Later on, IKKβ 26, 27 and IKKγ 28, 29 knockout mice were found to exhibit very similar phenotypes. These genetic studies clearly demonstrate an anti-apoptotic role for IKK-dependent NF-κB signaling in hepatocytes, mainly during early liver development.
The role of IKK-dependent classical NF-κB signaling in adult mouse liver physiology, however, is more complex. Mice with hepatocytes-specific ablation of IKKβ (Alb-Cre/IkkβF/F or IkkβΔhep mice) develop normally and their livers are not even sensitive to administration of LPS, a strong TNF inducer 30, 31. However, careful analysis suggests that residual hepatocyte IKK activity (presumably from IKKα) in IkkβΔhep mice may be sufficient for TNF-induced NF-κB activation, which is completely blocked by an additional ablation of IKKα (Ikkα/IkkβΔhep mice) 30. These results suggest that IKKα and IKKβ in adult hepatocytes may have somewhat redundant functions in suppressing apoptosis and necrosis. Indeed, unlike IkkβΔhep mice, Ikkα/IkkβΔhep mice or mice deficient of the regulatory component IKKγ in hepatocytes (IkkγΔhep mice) suffer from extensive hepatocyte death and liver failure upon TNF-inducing challenges 30, 32. Furthermore, IkkγΔhep or Ikkα/IkkβΔhep mice exhibit spontaneous liver damage, which is not seen in IkkβΔhep mice 31, 32, 33. Like IkkβΔhep mice, mice deleted of RelA in hepatocytes (RelAΔhep mice) are also healthy unless challenged and exposed to TNF. Based on available evidence, it is safe to conclude that the IKK/NF-κB pathway is important for hepatocyte survival and maintenance of liver homeostasis in response to various environmental challenges that can induce the production of TNF and other hepatotoxic cytokines.
The activated IKK/NF-κB pathway may play a tumor-promoting role by protecting tumor cells from death or enhancing their proliferation. This hypothesis was first tested in a mouse model of azoxymethane (AOM)+dextrane sulfate sodium (DSS)-induced colitis-associated cancer (CAC). Conditional disruption of the Ikkβ gene in intestinal epithelial cells (IEC) resulted in increased apoptotic elimination of AOM-induced premalignant cells and greatly reduced the development of colonic adenomas 34. However, strikingly different results were obtained in the diethylnitrosamine (DEN)-induced mouse HCC model. DEN is a pro-carcinogen that, upon metabolic activation in zone 3 hepatocytes, forms bulky DNA adducts 35. Upon subsequent cell proliferation, some of these DNA adducts are fixed into permanent genetic alterations that may cause activation of oncogenes, such as β-catenin (He and Karin, unpublished results). A single dose of DEN given to two-week-old mice is sufficient to induce HCC in 100% of male mice. However, when DEN is given to male mice that are older than 4 weeks of age, it is no longer effective in HCC induction on its own and requires assistance from other tumor promoters, such as phenobarbitol. This age-dependent difference in carcinogenic efficacy is not likely to be due to altered metabolic activation of DEN 36, 37. The main reason that DEN is not a complete carcinogen in mice that are more than 4 weeks old is the nearly complete absence of proliferating hepatocytes 38. Thus, any agent that induces hepatocyte proliferation should function as a tumor promoter. Indeed, partial hepatectomy after DEN administration results in effective hepatocarcinogenesis in older mice 38. It was found that liver-specific disruption of IKKβ greatly enhances DEN-induced hepatocyte death relative to wild-type mice 39. Although this may enhance the elimination of DEN-damaged hepatocytes, it should be noted that enhanced hepatocyte death also results in enhanced compensatory proliferation. Consequently, IkkβΔhep mice are 3-4 fold more susceptible to DEN-induced HCC development than wild-type mice 39. An even more striking effect on HCC development is seen upon the conditional deletion of hepatocyte IKKγ/NEMO 33. In this case, IkkγΔhep mice exhibit spontaneous liver damage and sequentially develop hepatosteatosis, hepatitis, liver fibrosis, and HCC without any known exposure to a carcinogen 33.
Multiple mechanisms were proposed to explain the pro-survival function of the IKK/NF-κB pathway, which can either enhance tumor development (as it does in the colon) or attenuate tumor development (as it does in the liver) 40. In the liver a critical pro-survival mechanism involves NF-κB's ability to maintain anti-oxidant defenses by controlling the expression of several key reactive oxygen species (ROS)-scavenging proteins 41, 42. Mice that lack IKKβ exhibit extensive ROS accumulation in their livers shortly after injection of DEN, whose metabolism in zone 3 hepatocytes results in ROS production 39. Increased ROS accumulation is also seen in livers of unchallenged IkkγΔhep mice 33. ROS accumulation in the liver can be prevented by dietary administration of the potent anti-oxidant butylated hydroxyanisole (BHA). Indeed, liver damage, compensatory proliferation and hepatocarcinogenesis in both IkkβΔhep and IkkγΔhep mutant mice are reversed by BHA consumption 33, 39. Excessive ROS accumulation promotes cell death through various mechanisms, including prolonged JNK activation 41. In support of this view, increased JNK phosphorylation and kinase activity are observed in livers of IkkγΔhep mice and DEN-challenged IkkβΔhep mice 33, 39. Importantly, reduced hepatocyte death, less compensatory proliferation and suppressed hepatocarcinogenesis were observed upon crossing of IkkβΔhep mice to Jnk1−/− mice 43. Therefore, the IKK/NF-κB pathway maintains hepatocyte survival by preventing ROS accumulation and excessive JNK activation, thereby reducing liver damage, proliferation and cancer development (Figure 1).
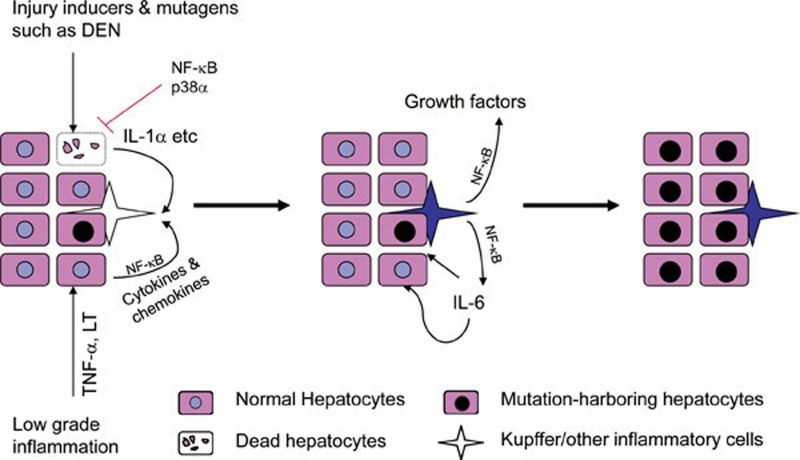
Figure 1.
Roles of NF-κB signaling in hepatocarcinogenesis. In the injury-promoted DEN hepatocarcinogenesis model, Kupffer cells are activated by IL-1α released from dying hepatocytes. Hepatocyte NF-κB (and p38α) inhibits this process by promoting hepatocyte survival. In low-grade, chronic, inflammation-promoted HCC models, hepatocytes with activated NF-κB produce cytokines and chemokines which activate Kupffer cells and recruit and activate other inflammatory cells and thereby maintain an inflammatory microenvironment. In both models, activated Kupffer cells produce cytokines and growth factors, such as IL-6, that are essential for the expansion of mutated hepatocytes and subsequent HCC development. Production of such cytokines by Kupffer cells is NF-κB dependent.
Hepatocyte IKK/NF-κB promotes HCC development by maintaining liver inflammatory responses
In sharp contrast to the tumor-suppressing role of hepatocyte IKK/NF-κB signaling in the mouse models described above, in other HCC models the NF-κB pathway was found to promote tumor development. The first example came from the elegant work of Pikarsky and colleagues 44. They employed Mdr2−/− mice, which spontaneously develop cholangitis due to defective cholesterol phospholipid secretion in the bile 45. These mice developed low-grade chronic liver inflammation that eventually results in the development of HCC. It was found that NF-κB was activated in Mdr2−/− hepatocytes, although the initial stimulus leading to NF-κB activation has not been fully identified. NF-κB activation promotes low amounts of TNF production and paracrine TNF signaling maintains NF-κB activation in Mdr2−/− hepatocytes. Correspondingly, treatment of Mdr2−/− mice with a neutralizing TNF antibody inhibits NF-κB activation in hepatocytes and decreases expression of NF-κB-dependent anti-apoptotic genes 44. The authors examined the tumorigenic function of hepatocyte NF-κB by expressing a nondegradable form of IκBα from a doxycycline-regulated liver-specific promoter and found that inhibition of NF-κB activation retarded and reduced HCC development in Mdr2−/− mice 44. A similar tumor-promoting role for hepatocyte NF-κB was observed in transgenic mice that express lymphotoxin (LT)α:β heterotrimers in hepatocytes 46. LTα:β transgenic mice develop liver inflammation, evidenced by chronic penetration of T, B and dendritic cells into their livers and elevated production of cytokines such as IL-1β, IFNγ and IL-6 46. Chronic liver inflammation is accompanied by increased hepatocyte proliferation that eventually leads to appearance of HCC in old mice. Crossing of LTα:β transgenic mice with IkkβΔhep mice prevented liver inflammation and reduced HCC development, suggesting that in this case IKKβ activation in hepatocytes is tumor promoting because it is required to sustain the chronic inflammatory response initiated by LTα:β expression 46.
Notably in both Mdr2−/− and LTαβ-transgenic mice, HCC development depends on chronic low grade inflammation and no liver injury has been observed either prior to or subsequent to NF-κB inhibition 44, 46. Thus in these models, in contrast to the injury-driven IkkβΔhep+DEN and IkkγΔhep models, the main function of NF-κB in hepatocytes appears to be the production of cytokines that maintain the inflammatory microenvironment in which these tumors develop (Figure 1).
IKK/NF-κB in liver myeloid cells promotes liver cancer development through IL-6 and liver inflammatory responses
Different environmental challenges and stimuli are sensed by resident myeloid cells (Kupffer cells in liver), which initiate an inflammatory response aimed to remove the insults and repair the injured tissue. Activated Kupffer cells produce a panel of inflammatory cytokines and growth factors in an IKK/NF-κB-dependent manner. In the DEN model, where hepatocyte IKK/NF-κB signaling was found to inhibit HCC development, activation of IKKβ/NF-κB in Kupffer cells promotes tumor development 39. Deletion of IKKβ in liver myeloid cells in addition to hepatocytes diminished the production of pro-inflammatory cytokines, such as IL-6 and TNF, reduced liver compensatory proliferation and strongly inhibited DEN-induced HCC development 39. Deletion of IKKβ in Kupffer cells was also found to inhibit the metastatic growth of Lewis lung carcinoma cells in liver 47. The mechanism by which DEN administration leads to IKK/NF-κB activation in Kupffer cells was found to depend on the release of IL-1α by necrotic hepatocytes which activates an MyD88-dependent signaling pathway upon binding to IL-1 receptor (IL-1R) on Kupffer cells. Inhibition of IL-1R signaling or ablation of MyD88 was found to attenuate DEN-induced HCC development 48.
One of the most important NF-κB-dependent cytokines that is produced by activated Kupffer cells is IL-6. Interestingly, DEN-treated female mice which unlike male mice are resistant to DEN-induced HCC development, produce less IL-6 than similarly treated male mice 49. IL-6 is a major STAT3 activator in liver and male mice lacking IL-6 exhibit reduced DEN-induced STAT3 activation and are as protected from HCC development as wild-type female 49. These results suggest that the striking male preference in HCC development in both human and mice may be due to differential IL-6 production 8, 49. Whereas IL-6 ablation abolishes the male bias in DEN-induced HCC development, ovariectomy enhances IL-6 production and augments HCC induction in female mice 49. It is likely that gender-specific differences in IL-6 expression also affect the incidence of human HCC, as serum IL-6 is higher after menopause 50, 51 and postmenopausal women display higher HCC incidence than premenopausal women 8. Moreover, expression of IL-6 is elevated in both liver cirrhosis and HCC 52, 53 and was recently found to correlate with rapid progression from viral hepatitis to HCC 54, 55. Precise mechanisms by which elevated IL-6 promotes HCC development are not known, but some of IL-6 functions are likely mediated by activation of STAT3.
STAT3 in liver cancer
STAT3 signaling is turned on in human HCC
STAT3 was first identified and cloned from mouse liver cDNA library in the study of IL-6 signaling 56, 57. STAT3 belongs to the signal transducer and activator of transcription (STAT) family. Like its relatives, STAT3 is inactive in nonstimulated cells, but is rapidly activated by various cytokines and growth factors, such as IL-6 and EGF family members, as well as hepatocyte growth factor (HGF) 58, 59. STAT3 activation requires phosphorylation of a critical tyrosine residue (Tyr705), which mediates its dimerization that is a prerequisite for nucleus entry and DNA binding 60. The phosphorylation of STAT3 at Tyr705 is most commonly mediated by Janus kinases (JAKs), especially JAK2, but its activity is also subject to fine tuning by other mechanisms, including serine (Ser727) phosphorylation 61 and reversible acetylation 62. Activation of STAT3 also turns on strong negative feedback loops involving SHP phosphatases and suppressor of cytokine signaling 3 (SOCS3) 63. These feedback mechanisms dampen STAT3 activity and ensure that cytokine-induced STAT3 activation is a transient event in normal cells. However, in cancer cells STAT3 is often found to be constitutively activated 64.
We have examined a large number of human HCC specimens and detected phosphorylated (i.e. activated) STAT3 in approximately 60% of them, with STAT3-positive tumors being more aggressive 65. These findings are consistent with those of other studies in which STAT3 was found to be activated in the majority of HCCs with poor prognosis and not in surrounding non-tumor tissue or in normal liver 66. However, the events that lead to STAT3 activation in human HCC are not known. Interestingly, activating mutations in the gene encoding the gp130 signaling subunit of IL-6 receptor family members were identified in benign hepatic adenomas 67. When combined with a β-catenin activating mutation, these mutations, which cause STAT3 activation, lead to HCC development 67. Nevertheless, STAT3-activating mutations are rare in human cancers. Most likely, as discussed above for NF-κB, STAT3 in cancer cells is activated by cytokines and growth factors that are produced within the tumor microenvironment. Indeed, the expression of IL-6, one of the major STAT3-activating cytokines, is elevated in human liver diseases and HCC 52, 53. In addition, many HCC risk factors, including HCV infection and hepatosteatosis, cause oxidative stress 68, 69, 70 and just like JNK, STAT3 can also be activated in response to ROS accumulation 65. As discussed below, NF-κB-induced expression of anti-oxidants prevents inadvertent activation of STAT3 by ROS accumulation, but it needs to be determined whether NF-κB activity is down-regulated during human hepatocarcinogenesis to allow STAT3 activation. Nevertheless, the majority of STAT3-positive HCCs do not exhibit NF-κB activation and most NF-κB positive HCCs do not show activated STAT3 65. However, the main cause of STAT3 activation in human HCC could simply be the elevated expression of IL-6 and related cytokines, such as IL-11 and IL-22.
STAT3 promotes HCC development in mouse models
Germ line ablation of Stat3 results in early embryonic lethality 71. In fact, loss of STAT3 is lethal even to embryonic stem cells 72, 73, underscoring a critical role for STAT3 in cell growth and/or survival. To overcome these problems, a number of tissue-specific Stat3 knockout mouse strains were generated to allow STAT3 deletion in differentiated cells 74. Using such conditional STAT3 knockout mice, it has been shown that STAT3 is required for tumorigenesis in mouse skin 75, intestine 76, 77 and liver 65. Such results left little doubt that STAT3 is a critical oncogenic transcription factor and an attractive target for cancer therapy 78.
We used hepatocyte-specific STAT3 deficient mice (Stat3Δhep) to examine the role of STAT3 in DEN-induced liver tumorigenesis. Stat3Δhep mice were found to exhibit more than a 6-fold reduction in HCC load relative to Stat3F/F mice 65. Furthermore, tumors in Stat3Δhep mice were smaller, suggesting that STAT3 may play a role in HCC cell proliferation and/or survival. We derived cell lines from DEN-induced HCCs (dih cells) of Stat3F/F mice. Deletion of STAT3 in cultured Stat3F/F dih cells, accomplished by infecting the cells with a Cre-expressing adenovirus, resulted in cell death, suggesting that activated STAT3 is required for the survival of HCC cells. Although dih cells that are completely STAT3-deficient cannot survive, cells with a partial reduction of STAT3 expression, accomplished by shRNA transduction are viable, but exhibit a senescent phenotype and fail to form subcutaneous tumors upon transplantation 65.
Interestingly, dependence on STAT3 for survival is also seen in anaplastic large cell lymphomas that spontaneously appear in NPM-ALK transgenic mice, which invariably show STAT3 activation 79. The lymphoma cells rapidly die when depleted of STAT3 in vitro 79. Given this strict dependence on STAT3 for survival, it is puzzling to find that a few tumors can still develop in the complete absence of STAT3 in both the DEN-induced HCC model and in NPM-ALK transgenic mice 65, 79. It is plausible that an alternative pathway can be activated in STAT3-null tumors but this pathway is hardly active in the presence of STAT3 78.
STAT3 as a therapeutic target in human HCC
As compelling data continue to accumulate STAT3 has become an attractive molecule target for the treatment and prevention of human malignancies. While safety is a primary concern, given the embryonic lethality of STAT3-null mice, with the use of STAT3 inhibitors, tissue-specific Stat3 ablation experiments indicate that STAT3 is not required for the survival of differentiated cells. These results provide supportive evidence that it may be safe to target STAT3 for human cancer therapy.
Different types of STAT3 inhibitors were designed to either directly target STAT3 by inhibiting its dimerization, DNA binding, or nuclear entry or through the targeting of upstream components in the STAT3 activation pathway 80, 81. S3I-201 is a direct STAT3 inhibitor that blocks both STAT3 dimerization and DNA-binding and transcriptional activities 82. Treatment of tumor xenografts derived from a human breast cancer cell line with constitutive STAT3 activity with S3I-201 resulted in inhibition of tumor growth 82. The therapeutic effect of S3I-201 on xenografts of the human HCC cell line Huh-7 was also examined and it was found that at a dose of 5 mg/kg given every other day, S3I-201 inhibited STAT3 tyrosine phosphorylation and tumor growth 83. Another widely used STAT3 inhibitor is AG490 which blocks activation of STAT3 by inhibiting the upstream kinase JAK2 84. We have tested the effect of S3I-201 and AG490 on the in vivo tumorigenic growth of dih cells and found effective inhibition of STAT3 activity and tumor growth 65. The higher the level of STAT3 in a tumor cell line, the more susceptible it is to STAT3 inhibition 65.
Despite the testing of a number of different STAT3 inhibitors, their overall anti-tumor effects have not been overly impressive 80. One explanation is that most of currently available STAT3 inhibitors target the conventional STAT3 pathway, i.e. STAT3 tyrosine phosphorylation, dimerization and DNA binding. This pathway, however, may not be the only mechanism through which STAT3 promotes tumorigenesis. For example, forced expression of a nonphosphorylatable STAT3 variant can mimic some STAT3-dependent functions in tumorigenesis 85. To address this possibility, STAT3 ablation via systemic administration of a validated antisense oligonucleotide was recently tested in mouse tumor models 79, 86. The Stat3 antisense oligonucleotide significantly reduced STAT3 protein amounts and inhibited cell proliferation and tumorigenic growth of several human HCC cell lines transplanted into mice 86. A similar anti-tumor effect of Stat3 antisense oligonucleotides was shown in a mouse lymphoma model 79. Effective inhibition of tumorigenic growth of many different types of cancer cells transplanted into mice was observed upon treatment with AZD1480, a highly specific JAK2 inhibitor 87.
Crosstalk between IKK/NF-κB and STAT3 in liver cancer
NF-κB and STAT3 each control the expression of a large number of downstream genes that control cell proliferation, survival, stress responses and immune functions. Some of the target genes for NF-κB and STAT3 overlap and in addition, the two transcription factors are engaged in both positive and negative crosstalk 88, 89, 90. In mouse DEN model, DEN-induced hepatocyte death results in release of IL-1α which activates NF-κB signaling in Kupffer cells, which produce a panel of cytokines and growth factors, including IL-6 39. IL-6 released by Kupffer cells activates STAT3 in hepatocytes and STAT3-activated genes are critical for compensatory hepatocyte proliferation and liver tumorigenesis 49, 65. However, more recently we found that the two transcription factors are also engaged in negative crosstalk within HCC cells 65. NF-κB activation results in increased expression of proteins, such as ferritin heavy chain and superoxide dismutase 2 that have an anti-oxidant function that prevents excessive ROS accumulation 41, 42. Inactivation of IKKβ in HCC cells or hepatocytes favors the accumulation of ROS which oxidize the catalytic cysteine of various protein tyrosine phosphatases (PTPs) 41, including SHP1 and SHP2, the phosphatases that dephosphorylate STAT3 and JAK2 91. Oxidation of SHP1 and SHP2 results in loss of their catalytic activity and accumulation of phosphorylated and activated JAK2 and STAT3, which stimulate the proliferation and tumorigenic growth of NF-κB-deficient HCC 65. Treatment of mice bearing IKKβ-deficient tumors with an anti-oxidant (BHA) restores SHP1/2 activity, reduces JAK2 and STAT3 phosphorylation and inhibits tumor growth. More recently, the loss of IKKβ in neutrophils was also found to result in activation of STAT3, which enhances the survival and proliferation of NF-κB-deficient neutrophils 92.
Not only NF-κB can affect STAT3 activity, STAT3 was also found to contribute to NF-κB activation. Activated STAT3 in cancer cells is able to bind RelA/p65 in the nucleus and this results in reversible acetylation of RelA/p65 by the STAT3-recruited acetyltransferase p300 93. Acetylation of RelA/p65 prolongs its nuclear retention 94. Therefore, it was suggested that activated STAT3 may account for constitutive activation of NF-κB in some human cancers. This mechanism, however, does not seem to operate in most human HCCs as the majority of tumors with activated STAT3 do not show NF-κB activation 65.
Concluding remarks
Although the etiology of human HCC is well established, its molecular pathogenesis is poorly understood. As a consequence, mechanism-based therapies for HCC are rare and being refractory to conventional anti-cancer drugs, HCC remains to be one of the deadliest human cancers with a 5 year survival rate of less than 10 percent 95. The studies discussed above suggest that NF-κB and STAT3 are likely to play important roles in liver inflammatory responses and maintenance of homeostasis and also make critical contributions to HCC development and progression. Although the mechanisms responsible for NF-κB and STAT3 activation in human HCC are not fully understood, a role for NF-κB-regulated expression of the STAT3-activating cytokine IL-6 has recently emerged both in viral hepatitis and in hepatosteatosis 96. Both the pathways that control IL-6 expression and those that control its ability to activate STAT3 offer interesting opportunities to therapeutic intervention as well as prevention.
A variety of animal models were used to study the roles of NF-κB, STAT3 and other signaling pathways in HCC development. However, due to the inability of human hepatitis viruses to infect mice or rats, a rodent model for virally-induced hepatocarcinogenesis is still not available. In addition, most of our mechanistic understanding of NF-κB and STAT3 in HCC comes from studies using cell type-specific knockout mice. NF-κB or STAT3 in these mice are ablated only in certain cell types and remain intact and fully functional in most other cells. Thus, the results obtained may not precisely predict the effect of pharmaceutical inhibitors that interfere with the activity of these transcription factors in all cells. The successful translation of the knowledge gained about NF-κB and STAT3 in HCC will depend on suitable solutions to these potential problems and appropriate human studies that will validate the promising results obtained in mice.
References
- Dvorak HF. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med. 1986;315:1650–1659. doi: 10.1056/NEJM198612253152606. [DOI] [PubMed] [Google Scholar]
- Schafer M, Werner S. Cancer as an overhealing wound: an old hypothesis revisited. Nat Rev Mol Cell Biol. 2008;9:628–638. doi: 10.1038/nrm2455. [DOI] [PubMed] [Google Scholar]
- Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst PB, Gold BD. The disease spectrum of Helicobacter pylori: the immunopathogenesis of gastroduodenal ulcer and gastric cancer. Annu Rev Microbiol. 2000;54:615–640. doi: 10.1146/annurev.micro.54.1.615. [DOI] [PubMed] [Google Scholar]
- Seeff LB. Introduction: The burden of hepatocellular carcinoma. Gastroenterology. 2004;127:S1–S4. doi: 10.1053/j.gastro.2004.09.010. [DOI] [PubMed] [Google Scholar]
- Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow. Lancet. 2001;357:539–545. doi: 10.1016/S0140-6736(00)04046-0. [DOI] [PubMed] [Google Scholar]
- Parkin DM, Bray FI, Devesa SS. Cancer burden in the year 2000. The global picture. Eur J Cancer. 2001;37 Suppl 8:S4–66. doi: 10.1016/s0959-8049(01)00267-2. [DOI] [PubMed] [Google Scholar]
- Bosch FX, Ribes J, Diaz M, Cleries R. Primary liver cancer: worldwide incidence and trends. Gastroenterology. 2004;127:S5–S16. doi: 10.1053/j.gastro.2004.09.011. [DOI] [PubMed] [Google Scholar]
- Tong MJ, el-Farra NS, Reikes AR, Co RL. Clinical outcomes after transfusion-associated hepatitis C. N Engl J Med. 1995;332:1463–1466. doi: 10.1056/NEJM199506013322202. [DOI] [PubMed] [Google Scholar]
- Nakamoto Y, Kaneko S. Mechanisms of viral hepatitis induced liver injury. Curr Mol Med. 2003;3:537–544. doi: 10.2174/1566524033479591. [DOI] [PubMed] [Google Scholar]
- Herzer K, Sprinzl MF, Galle PR. Hepatitis viruses: live and let die. Liver Int. 2007;27:293–301. doi: 10.1111/j.1478-3231.2006.01422.x. [DOI] [PubMed] [Google Scholar]
- Block TM, Mehta AS, Fimmel CJ, Jordan R. Molecular viral oncology of hepatocellular carcinoma. Oncogene. 2003;22:5093–5107. doi: 10.1038/sj.onc.1206557. [DOI] [PubMed] [Google Scholar]
- Sen R, Baltimore D. Multiple nuclear factors interact with the immunoglobulin enhancer sequences. Cell. 1986;46:705–716. [PubMed] [Google Scholar]
- Barnes PJ, Karin M. Nuclear factor-κB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med. 1997;336:1066–1071. doi: 10.1056/NEJM199704103361506. [DOI] [PubMed] [Google Scholar]
- Ghosh S, Karin M.Missing pieces in the NF-κB puzzle Cell 2002109Suppl:S81–S96. [DOI] [PubMed] [Google Scholar]
- Vallabhapurapu S, Karin M. Regulation and function of NF-κB transcription factors in the immune system. Annu Rev Immunol. 2009;27:693–733. doi: 10.1146/annurev.immunol.021908.132641. [DOI] [PubMed] [Google Scholar]
- Gilmore TD. The Re1/NF-κB/I κB signal transduction pathway and cancer. Cancer Treat Res. 2003;115:241–265. [PubMed] [Google Scholar]
- Karin M, Cao Y, Greten FR, Li ZW. NF-κB in cancer: from innocent bystander to major culprit. Nat Rev Cancer. 2002;2:301–310. doi: 10.1038/nrc780. [DOI] [PubMed] [Google Scholar]
- Franzoso G, Bours V, Park S, Tomita-Yamaguchi M, Kelly K, Siebenlist U. The candidate oncoprotein Bcl-3 is an antagonist of p50/NF-κB-mediated inhibition. Nature. 1992;359:339–342. doi: 10.1038/359339a0. [DOI] [PubMed] [Google Scholar]
- Bours V, Franzoso G, Azarenko V, et al. The oncoprotein Bcl-3 directly transactivates through κB motifs via association with DNA-binding p50B homodimers. Cell. 1993;72:729–739. doi: 10.1016/0092-8674(93)90401-b. [DOI] [PubMed] [Google Scholar]
- Annunziata CM, Davis RE, Demchenko Y, et al. Frequent engagement of the classical and alternative NF-κB pathways by diverse genetic abnormalities in multiple myeloma. Cancer Cell. 2007;12:115–130. doi: 10.1016/j.ccr.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keats JJ, Fonseca R, Chesi M, et al. Promiscuous mutations activate the noncanonical NF-κB pathway in multiple myeloma. Cancer Cell. 2007;12:131–144. doi: 10.1016/j.ccr.2007.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beg AA, Sha WC, Bronson RT, Ghosh S, Baltimore D. Embryonic lethality and liver degeneration in mice lacking the RelA component of NF-κB. Nature. 1995;376:167–170. doi: 10.1038/376167a0. [DOI] [PubMed] [Google Scholar]
- Doi TS, Marino MW, Takahashi T, et al. Absence of tumor necrosis factor rescues RelA-deficient mice from embryonic lethality. Proc Natl Acad Sci USA. 1999;96:2994–2999. doi: 10.1073/pnas.96.6.2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfeld ME, Prichard L, Shiojiri N, Fausto N. Prevention of hepatic apoptosis and embryonic lethality in RelA/TNFR-1 double knockout mice. Am J Pathol. 2000;156:997–1007. doi: 10.1016/S0002-9440(10)64967-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Van Antwerp D, Mercurio F, Lee KF, Verma IM. Severe liver degeneration in mice lacking the IκB kinase 2 gene. Science. 1999;284:321–325. doi: 10.1126/science.284.5412.321. [DOI] [PubMed] [Google Scholar]
- Tanaka M, Fuentes ME, Yamaguchi K, et al. Embryonic lethality, liver degeneration, and impaired NF-κB activation in IKK-β-deficient mice. Immunity. 1999;10:421–429. doi: 10.1016/s1074-7613(00)80042-4. [DOI] [PubMed] [Google Scholar]
- Rudolph D, Yeh WC, Wakeham A, et al. Severe liver degeneration and lack of NF-κB activation in NEMO/IKKgamma-deficient mice. Genes Dev. 2000;14:854–862. [PMC free article] [PubMed] [Google Scholar]
- Makris C, Godfrey VL, Krahn-Senftleben G, et al. Female mice heterozygous for IKK γ/NEMO deficiencies develop a dermatopathy similar to the human X-linked disorder incontinentia pigmenti. Mol Cell. 2000;5:969–979. doi: 10.1016/s1097-2765(00)80262-2. [DOI] [PubMed] [Google Scholar]
- Luedde T, Assmus U, Wustefeld T, et al. Deletion of IKK2 in hepatocytes does not sensitize these cells to TNF-induced apoptosis but protects from ischemia/reperfusion injury. J Clin Invest. 2005;115:849–859. doi: 10.1172/JCI23493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda S, Chang L, Li ZW, Luo JL, Leffert H, Karin M. IKKβ is required for prevention of apoptosis mediated by cell-bound but not by circulating TNFα. Immunity. 2003;19:725–737. doi: 10.1016/s1074-7613(03)00301-7. [DOI] [PubMed] [Google Scholar]
- Luedde T, Heinrichsdorff J, de Lorenzi R, De Vos R, Roskams T, Pasparakis M. IKK1 and IKK2 cooperate to maintain bile duct integrity in the liver. Proc Natl Acad Sci USA. 2008;105:9733–9738. doi: 10.1073/pnas.0800198105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luedde T, Beraza N, Kotsikoris V, et al. Deletion of NEMO/IKKγ in liver parenchymal cells causes steatohepatitis and hepatocellular carcinoma. Cancer Cell. 2007;11:119–132. doi: 10.1016/j.ccr.2006.12.016. [DOI] [PubMed] [Google Scholar]
- Greten FR, Eckmann L, Greten TF, et al. IKKβ links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell. 2004;118:285–296. doi: 10.1016/j.cell.2004.07.013. [DOI] [PubMed] [Google Scholar]
- Verna L, Whysner J, Williams GM. N-nitrosodiethylamine mechanistic data and risk assessment: bioactivation, DNA-adduct formation, mutagenicity, and tumor initiation. Pharmacol Ther. 1996;71:57–81. doi: 10.1016/0163-7258(96)00062-9. [DOI] [PubMed] [Google Scholar]
- Lai DY, Arcos JC. Minireview: dialkylnitrosamine bioactivation and carcinogenesis. Life Sci. 1980;27:2149–2165. doi: 10.1016/0024-3205(80)90379-3. [DOI] [PubMed] [Google Scholar]
- Magee PN, Barnes JM. Carcinogenic nitroso compounds. Adv Cancer Res. 1967;10:163–246. doi: 10.1016/s0065-230x(08)60079-2. [DOI] [PubMed] [Google Scholar]
- Fausto N. Mouse liver tumorigenesis: models, mechanisms, and relevance to human disease. Semin Liver Dis. 1999;19:243–252. doi: 10.1055/s-2007-1007114. [DOI] [PubMed] [Google Scholar]
- Maeda S, Kamata H, Luo JL, Leffert H, Karin M. IKKbeta couples hepatocyte death to cytokine-driven compensatory proliferation that promotes chemical hepatocarcinogenesis. Cell. 2005;121:977–990. doi: 10.1016/j.cell.2005.04.014. [DOI] [PubMed] [Google Scholar]
- Luo JL, Kamata H, Karin M. IKK/NF-κB signaling: balancing life and death--a new approach to cancer therapy. J Clin Invest. 2005;115:2625–2632. doi: 10.1172/JCI26322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamata H, Honda S, Maeda S, Chang L, Hirata H, Karin M. Reactive oxygen species promote TNFα-induced death and sustained JNK activation by inhibiting MAP kinase phosphatases. Cell. 2005;120:649–661. doi: 10.1016/j.cell.2004.12.041. [DOI] [PubMed] [Google Scholar]
- Pham CG, Bubici C, Zazzeroni F, et al. Ferritin heavy chain upregulation by NF-κB inhibits TNFalpha-induced apoptosis by suppressing reactive oxygen species. Cell. 2004;119:529–542. doi: 10.1016/j.cell.2004.10.017. [DOI] [PubMed] [Google Scholar]
- Sakurai T, Maeda S, Chang L, Karin M. Loss of hepatic NF-κB activity enhances chemical hepatocarcinogenesis through sustained c-Jun N-terminal kinase 1 activation. Proc Natl Acad Sci USA. 2006;103:10544–10551. doi: 10.1073/pnas.0603499103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pikarsky E, Porat RM, Stein I, et al. NF-κB functions as a tumour promoter in inflammation-associated cancer. Nature. 2004;431:461–466. doi: 10.1038/nature02924. [DOI] [PubMed] [Google Scholar]
- Mauad TH, van Nieuwkerk CM, Dingemans KP, et al. Mice with homozygous disruption of the mdr2 P-glycoprotein gene. A novel animal model for studies of nonsuppurative inflammatory cholangitis and hepatocarcinogenesis. Am J Pathol. 1994;145:1237–1245. [PMC free article] [PubMed] [Google Scholar]
- Haybaeck J, Zeller N, Wolf MJ, et al. A lymphotoxin-driven pathway to hepatocellular carcinoma. Cancer Cell. 2009;16:295–308. doi: 10.1016/j.ccr.2009.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda S, Hikiba Y, Sakamoto K, et al. IκB kinasebeta/nuclear factor-κB activation controls the development of liver metastasis by way of interleukin-6 expression. Hepatology. 2009;50:1851–1860. doi: 10.1002/hep.23199. [DOI] [PubMed] [Google Scholar]
- Sakurai T, He G, Matsuzawa A, et al. Hepatocyte necrosis induced by oxidative stress and IL-1 α release mediate carcinogen-induced compensatory proliferation and liver tumorigenesis. Cancer Cell. 2008;14:156–165. doi: 10.1016/j.ccr.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naugler WE, Sakurai T, Kim S, et al. Gender disparity in liver cancer due to sex differences in MyD88-dependent IL-6 production. Science. 2007;317:121–124. doi: 10.1126/science.1140485. [DOI] [PubMed] [Google Scholar]
- Jilka RL, Hangoc G, Girasole G, et al. Increased osteoclast development after estrogen loss: mediation by interleukin-6. Science. 1992;257:88–91. doi: 10.1126/science.1621100. [DOI] [PubMed] [Google Scholar]
- Ershler WB, Keller ET. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annu Rev Med. 2000;51:245–270. doi: 10.1146/annurev.med.51.1.245. [DOI] [PubMed] [Google Scholar]
- Tilg H, Wilmer A, Vogel W, et al. Serum levels of cytokines in chronic liver diseases. Gastroenterology. 1992;103:264–274. doi: 10.1016/0016-5085(92)91122-k. [DOI] [PubMed] [Google Scholar]
- Trikha M, Corringham R, Klein B, Rossi JF. Targeted anti-interleukin-6 monoclonal antibody therapy for cancer: a review of the rationale and clinical evidence. Clin Cancer Res. 2003;9:4653–4665. [PMC free article] [PubMed] [Google Scholar]
- Nakagawa H, Maeda S, Yoshida H, et al. Serum IL-6 levels and the risk for hepatocarcinogenesis in chronic hepatitis C patients: an analysis based on gender differences. Int J Cancer. 2009;125:2264–2269. doi: 10.1002/ijc.24720. [DOI] [PubMed] [Google Scholar]
- Wong VW, Yu J, Cheng AS, et al. High serum interleukin-6 level predicts future hepatocellular carcinoma development in patients with chronic hepatitis B. Int J Cancer. 2009;124:2766–2770. doi: 10.1002/ijc.24281. [DOI] [PubMed] [Google Scholar]
- Wegenka UM, Buschmann J, Lutticken C, Heinrich PC, Horn F. Acute-phase response factor, a nuclear factor binding to acute-phase response elements, is rapidly activated by interleukin-6 at the posttranslational level. Mol Cell Biol. 1993;13:276–288. doi: 10.1128/mcb.13.1.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong Z, Wen Z, Darnell JE Jr. Stat3: a STAT family member activated by tyrosine phosphorylation in response to epidermal growth factor and interleukin-6. Science. 1994;264:95–98. doi: 10.1126/science.8140422. [DOI] [PubMed] [Google Scholar]
- Takeda K, Akira S. STAT family of transcription factors in cytokine-mediated biological responses. Cytokine Growth Factor Rev. 2000;11:199–207. doi: 10.1016/s1359-6101(00)00005-8. [DOI] [PubMed] [Google Scholar]
- Hirano T, Ishihara K, Hibi M. Roles of STAT3 in mediating the cell growth, differentiation and survival signals relayed through the IL-6 family of cytokine receptors. Oncogene. 2000;19:2548–2556. doi: 10.1038/sj.onc.1203551. [DOI] [PubMed] [Google Scholar]
- Yoshimura A, Naka T, Kubo M. SOCS proteins, cytokine signalling and immune regulation. Nat Rev Immunol. 2007;7:454–465. doi: 10.1038/nri2093. [DOI] [PubMed] [Google Scholar]
- Wen Z, Zhong Z, Darnell JE Jr. Maximal activation of transcription by Stat1 and Stat3 requires both tyrosine and serine phosphorylation. Cell. 1995;82:241–250. doi: 10.1016/0092-8674(95)90311-9. [DOI] [PubMed] [Google Scholar]
- Yuan ZL, Guan YJ, Chatterjee D, Chin YE. Stat3 dimerization regulated by reversible acetylation of a single lysine residue. Science. 2005;307:269–273. doi: 10.1126/science.1105166. [DOI] [PubMed] [Google Scholar]
- Kubo M, Hanada T, Yoshimura A. Suppressors of cytokine signaling and immunity. Nat Immunol. 2003;4:1169–1176. doi: 10.1038/ni1012. [DOI] [PubMed] [Google Scholar]
- Al Zaid Siddiquee K, Turkson J. STAT3 as a target for inducing apoptosis in solid and hematological tumors. Cell Res. 2008;18:254–267. doi: 10.1038/cr.2008.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He G, Yu GY, Temkin V, et al. Hepatocyte IKKβ/NF-κB inhibits tumor promotion and progression by preventing oxidative stress-driven STAT3 activation. Cancer Cell. 2010;17:286–297. doi: 10.1016/j.ccr.2009.12.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvisi DF, Ladu S, Gorden A, et al. Ubiquitous activation of Ras and Jak/Stat pathways in human HCC. Gastroenterology. 2006;130:1117–1128. doi: 10.1053/j.gastro.2006.01.006. [DOI] [PubMed] [Google Scholar]
- Rebouissou S, Amessou M, Couchy G, et al. Frequent in-frame somatic deletions activate gp130 in inflammatory hepatocellular tumours. Nature. 2009;457:200–204. doi: 10.1038/nature07475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–2576. doi: 10.1053/j.gastro.2007.04.061. [DOI] [PubMed] [Google Scholar]
- Parekh S, Anania FA. Abnormal lipid and glucose metabolism in obesity: implications for nonalcoholic fatty liver disease. Gastroenterology. 2007;132:2191–2207. doi: 10.1053/j.gastro.2007.03.055. [DOI] [PubMed] [Google Scholar]
- Wang T, Weinman SA. Causes and consequences of mitochondrial reactive oxygen species generation in hepatitis C. J Gastroenterol Hepatol. 2006;21 Suppl 3:S34–S37. doi: 10.1111/j.1440-1746.2006.04591.x. [DOI] [PubMed] [Google Scholar]
- Takeda K, Noguchi K, Shi W, et al. Targeted disruption of the mouse Stat3 gene leads to early embryonic lethality. Proc Natl Acad Sci USA. 1997;94:3801–3804. doi: 10.1073/pnas.94.8.3801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raz R, Lee CK, Cannizzaro LA, d'Eustachio P, Levy DE. Essential role of STAT3 for embryonic stem cell pluripotency. Proc Natl Acad Sci USA. 1999;96:2846–2851. doi: 10.1073/pnas.96.6.2846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuda T, Nakamura T, Nakao K, et al. STAT3 activation is sufficient to maintain an undifferentiated state of mouse embryonic stem cells. EMBO J. 1999;18:4261–4269. doi: 10.1093/emboj/18.15.4261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DE, Lee CK. What does Stat3 do. J Clin Invest. 2002;109:1143–1148. doi: 10.1172/JCI15650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan KS, Sano S, Kiguchi K, et al. Disruption of Stat3 reveals a critical role in both the initiation and the promotion stages of epithelial carcinogenesis. J Clin Invest. 2004;114:720–728. doi: 10.1172/JCI21032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollrath J, Phesse TJ, von Burstin VA, et al. gp130-mediated Stat3 activation in enterocytes regulates cell survival and cell-cycle progression during colitis-associated tumorigenesis. Cancer Cell. 2009;15:91–102. doi: 10.1016/j.ccr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Grivennikov S, Karin E, Terzic J, et al. IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell. 2009;15:103–113. doi: 10.1016/j.ccr.2009.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inghirami G, Chiarle R, Simmons WJ, Piva R, Schlessinger K, Levy DE. New and old functions of STAT3: a pivotal target for individualized treatment of cancer. Cell Cycle. 2005;4:1131–1133. doi: 10.4161/cc.4.9.1985. [DOI] [PubMed] [Google Scholar]
- Chiarle R, Simmons WJ, Cai H, et al. Stat3 is required for ALK-mediated lymphomagenesis and provides a possible therapeutic target. Nat Med. 2005;11:623–629. doi: 10.1038/nm1249. [DOI] [PubMed] [Google Scholar]
- Yue P, Turkson J. Targeting STAT3 in cancer: how successful are we. Expert Opin Investig Drugs. 2009;18:45–56. doi: 10.1517/13543780802565791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher S, Drewry JA, Shahani VM, Page BD, Gunning PT. Molecular disruption of oncogenic signal transducer and activator of transcription 3 (STAT3) protein. Biochem Cell Biol. 2009;87:825–833. doi: 10.1139/o09-044. [DOI] [PubMed] [Google Scholar]
- Siddiquee K, Zhang S, Guida WC, et al. Selective chemical probe inhibitor of Stat3, identified through structure-based virtual screening, induces antitumor activity. Proc Natl Acad Sci USA. 2007;104:7391–7396. doi: 10.1073/pnas.0609757104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L, Amin R, Gallicano GI, et al. The STAT3 inhibitor NSC 74859 is effective in hepatocellular cancers with disrupted TGF-β signaling. Oncogene. 2009;28:961–972. doi: 10.1038/onc.2008.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meydan N, Grunberger T, Dadi H, et al. Inhibition of acute lymphoblastic leukaemia by a Jak-2 inhibitor. Nature. 1996;379:645–648. doi: 10.1038/379645a0. [DOI] [PubMed] [Google Scholar]
- Yang J, Chatterjee-Kishore M, Staugaitis SM, et al. Novel roles of unphosphorylated STAT3 in oncogenesis and transcriptional regulation. Cancer Res. 2005;65:939–947. [PubMed] [Google Scholar]
- Li WC, Ye SL, Sun RX, et al. Inhibition of growth and metastasis of human hepatocellular carcinoma by antisense oligonucleotide targeting signal transducer and activator of transcription 3. Clin Cancer Res. 2006;12:7140–7148. doi: 10.1158/1078-0432.CCR-06-0484. [DOI] [PubMed] [Google Scholar]
- Hedvat M, Huszar D, Herrmann A, et al. The JAK2 inhibitor AZD1480 potently blocks Stat3 signaling and oncogenesis in solid tumors. Cancer Cell. 2009;16:487–497. doi: 10.1016/j.ccr.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grivennikov SI, Karin M. Dangerous liaisons: STAT3 and NF-κB collaboration and crosstalk in cancer. Cytokine Growth Factor Rev. 2010;21:11–19. doi: 10.1016/j.cytogfr.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson GP, Nozell SE, Benveniste ET. NF-κB and STAT3 signaling in glioma: targets for future therapies. Expert Rev Neurother. 2010;10:575–586. doi: 10.1586/ern.10.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollrath J, Greten FR. IKK/NF-κB and STAT3 pathways: central signalling hubs in inflammation-mediated tumour promotion and metastasis. EMBO Rep. 2009;10:1314–1319. doi: 10.1038/embor.2009.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentino L, Pierre J. JAK/STAT signal transduction: regulators and implication in hematological malignancies. Biochem Pharmacol. 2006;71:713–721. doi: 10.1016/j.bcp.2005.12.017. [DOI] [PubMed] [Google Scholar]
- Hsu L-C, Enzler T, Seita J, et al. IL-1β-driven neutrophilia preserves antibacterial defense in the absence of the kinase IKKβ Nat Immunol 2010in press. [DOI] [PMC free article] [PubMed]
- Lee H, Herrmann A, Deng JH, et al. Persistently activated Stat3 maintains constitutive NF-κB activity in tumors. Cancer Cell. 2009;15:283–293. doi: 10.1016/j.ccr.2009.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Fischle W, Verdin E, Greene WC. Duration of nuclear NF-κB action regulated by reversible acetylation. Science. 2001;293:1653–1657. doi: 10.1126/science.1062374. [DOI] [PubMed] [Google Scholar]
- Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–1236. doi: 10.1002/hep.20933. [DOI] [PubMed] [Google Scholar]
- Park EJ, Lee JH, Yu GY, et al. Dietary and genetic obesity promote liver inflammation and tumorigenesis by enhancing IL-6 and TNF expression. Cell. 2010;140:197–208. doi: 10.1016/j.cell.2009.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]