Abstract
This study exploited the unique opportunity to compare estimates of electronic health record (EHR) and specific health information technology (HIT) use for clinical activities by office-based physicians using data from two contemporaneous, nationally representative physician surveys: the 2008 National Ambulatory Medical Care Survey (NAMCS) and the 2008 Health Tracking Physician Survey (HTPS). Survey respondents included 4,117 physicians from the HTPS and 1,187 physicians from the NAMCS. We compared the survey designs and national estimates of EHR and specific HIT use for clinical activities in the two surveys and conducted multivariate analyses examining physician and practice characteristics associated with the adoption of “basic” or “fully functional” systems. The surveys asked nearly identical questions on EHR use.
Questions on specific HIT use for clinical activities overlapped but with differences. National estimates of all-EHR use were similar (HTPS 24.31 percent, 95 percent confidence interval [CI]: 22.99–25.69 percent vs. NAMCS 27.24 percent, 95 percent CI: 23.53–31.29 percent), but partial EHR use (i.e., part paper and part electronic) was higher in the HTPS than in the NAMCS (23.93 percent, 95 percent CI: 22.61–25.30 percent vs. 18.40 percent, 95 percent CI: 15.62–21.54 percent in the NAMCS). Both surveys reported low use of “fully functional” systems (HTPS 7.84 percent, 95 percent CI: 7.03–8.73 percent vs. NAMCS 4.56 percent, 95 percent CI 3.09–6.68 percent), but the use of “basic” systems was much higher in the HTPS than in the NAMCS (22.29 percent vs. 11.16 percent). Using multivariate analyses, we found common physician or practice characteristics in the two surveys, although the magnitude of the estimated effects differed. In conclusion, use of a “fully functional” EHR system by office-based physicians was low in both surveys. It may be a daunting task for physicians, particularly those in small practices, to adopt and achieve “meaningful use” in the next two years.
Key words: health information technology, electronic health records, physician survey
Introduction
Health information technology (HIT) is “the application of information processing involving both computer hardware and software that deals with the storage, retrieval, sharing, and use of health care information, data, and knowledge for communication and decision making.”1 HIT such as electronic health records (EHRs, also called electronic medical records) has the potential to improve the quality and safety of care received by patients.2–4 However, the adoption of EHRs, particularly those that meet the criteria of a fully functional system, has been slow among office-based physicians.5 To encourage adoption, the Health Information Technology for Economic and Clinical Health (HITECH) Act was passed in 2009, authorizing up to $27 billion in total funding to support widespread adoption of EHRs by physicians and hospitals through incentive payments from Medicare and Medicaid programs.6
Two large, nationally representative public-use physician surveys have been used to track adoption of EHRs among physicians. One is the National Ambulatory Medical Care Survey (NAMCS), conducted annually by the Centers for Disease Control and Prevention (CDC). Since 2005, the public-use data files have included information on HIT use (including EHRs) in physicians' offices. The latest available for public use is the 2008 survey. The other survey is the Community Tracking Study (CTS) Physician Survey, conducted by the Center for Studying Health System Change and sponsored by the Robert Wood Johnson Foundation. The CTS physician surveys have been conducted in 1996–1997, 1998–1999, 2000–2001, 2004–2005, and 2008. Information on HIT use was included since the 2004–2005 survey. The 2008 survey, renamed the Health Tracking Physician Survey (HTPS) because of survey design changes, contains information on HIT use (including EHRs), which provides a unique opportunity for comparison with the NAMCS. The HTPS surveyed more than four times as many physicians as the 2008 NAMCS and thus can provide more precise estimates.
This study exploits the unique opportunity to estimate the use of HIT by office-based physicians using data from the two contemporaneous, nationally representative physician surveys: the 2008 NAMCS and 2008 HTPS. To the best of our knowledge, these are the only two such surveys that are conducted periodically and available for public use. The NAMCS and HTPS have considerable overlap in information regarding HIT use, but there are important differences in sampling schemes and survey items regarding HIT use for clinical activities. While recent studies have examined the NAMCS data and others used CTS physician surveys, no studies have compared data from both.7–14
This comparison presents a unique opportunity to examine the robustness in national estimates of HIT adoption. Moreover, although similar information on HIT use was collected in the two surveys, the questions often differed in wording and the order in which they were asked. Any inconsistency in responses to similar survey questions may reveal useful implications for future survey design to generate consistent results and better track HIT adoption nationally. In addition, estimates from 2008, which preceded the passage of the HITECH Act, will provide useful baseline information that can facilitate comparisons with future progress under the multiyear incentive program to effectively monitor the diffusion of EHRs.
Data
This section discusses the NAMCS and HTPS data and draws attention to similarities and differences in survey designs and information on EHR and specific HIT use for clinical activities.
Survey Designs
Table 1 compares the designs of the two surveys.15, 16 The major differences lie in their sample frames and sampling strategies.
Table 1.
Comparison of Survey Designs
| 2008 Health Tracking Physician Survey | 2008 National Ambulatory Medical Care Survey | |
|---|---|---|
| Field time | February–October 2008 | 2008 |
| Sample frame | •AMA master file |
|
|
||
|
||
| Inclusion criteria | Office-based and hospital-based physicians who provide direct patient care for at least 20 hours per week | Office-based and CHC-based physicians principally engaged in direct patient care activities |
| Exclusion criteria |
|
|
|
|
|
|
||
|
||
| Weighted response rate | 61.9% | 59.6% |
| Mode of survey | Self-administered mail survey | One initial telephone interview and two in-person interviews |
| Sample design | Stratified probability sampling | Multistaged probability sampling |
| Geographic areas represented | 50 states and District of Columbia | 50 states and District of Columbia |
| Total sample | 4,720 | 1,187 |
Sources: Centers for Disease Control and Prevention. 2008 National Ambulatory Care Survey Micro-Data File Documentation. Available at http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm (accessed April 5, 2011); Strouse, Richard, et al. HSC 2008 Health Tracking Physician Survey Methodology Report (Technical Publication No. 77). Center for Studying Health System Change, September 2009. Available at http://www.hschange.org (accessed April 5, 2011).
The 2008 NAMCS utilized two concurrent sample frames and sampling processes. The “traditional” sample frame was derived from the American Medical Association (AMA) and American Osteopathic Association (AOA) master files. Physicians were sampled utilizing a complicated multistage probability design that involved probability samples of primary sampling units (PSU) and physicians within the PSUs stratified by specialties. To increase representation of physicians at community health centers (CHC), a separate sample frame of CHC providers was developed based on information from the Health Resources and Services Administration's Bureau of Primary Health Care and the Indian Health Service. To ensure that CHC providers were included only once, those selected through the “traditional” process were excluded. The initial survey was conducted by telephone followed by two in-person interviews. The final sample included 1,187 physicians who responded and saw patients during the assigned week. The weighted response rate was 59.6 percent based on the number of full participants only.17
The 2008 HTPS employed a much simpler design. The sample frame was derived from the AMA master file only. Although the AOA master file was not used, the AMA master file contains the majority of osteopathic physicians in the AOA master file.18 Previous CTS physician surveys that sampled from both files found that only 0.5 percent of sampled physicians were listed in the AOA master file but omitted from the AMA master file.19 The survey utilized a classical stratified design with proportional allocation. Physicians were first stratified by 10 geographic regions, within which further stratification by primary care physicians and specialists was performed. The survey was self-administered by mail; 4,720 physicians were eligible and completed the survey with a weighted response rate of 61.9 percent.20
Both surveys are nationally representative of non-federally-employed physicians who provide direct patient care in the 50 states and the District of Columbia. The NAMCS focused on office-based physicians. To be comparable, we excluded 603 hospital-based physicians from the HTPS. The final samples for this study included 4,117 physicians from the 2008 HTPS and 1,187 physicians from the 2008 NAMCS. Both surveys developed sampling weights that adjust for nonresponses to generate nationally representative estimates.21, 22 Table 2 compares demographic and practice characteristics of physicians included in the final samples. Overall, the characteristics of physicians and their practices are similar between the two surveys. Although demographic characteristics are not available in the public-use NAMCS data, the newly released 2008 NAMCS summary tables showed similar gender and racial/ethnic compositions as in the HTPS.23 Similarly, although geographic information and metropolitan statistical area (MSA) status are not included in the public-use HTPS data, this information reported elsewhere is similar to that in the NAMCS.24
Table 2.
Physician and Practice Characteristics
| 2008 Health Tracking Physician Survey (HTPS) (n = 4,117) |
2008 National Ambulatory Medical Care Survey (NAMCS) (n = 1,187) |
|||||
|---|---|---|---|---|---|---|
| n | % | Weighted % | n | % | Weighted % | |
| Specialty | ||||||
| Internal medicine/general or family practice | 1,335 | 32.43 | 32.85 | 360 | 30.33 | 33.76 |
| Pediatrics | 384 | 9.33 | 8.05 | 115 | 9.69 | 10.49 |
| OB/GYN | 289 | 7.02 | 7.17 | 76 | 6.40 | 8.50 |
| Psychiatry | 259 | 6.29 | 6.56 | 69 | 5.81 | 5.63 |
| Other medical specialty | 1,017 | 24.70 | 25.32 | 265 | 22.33 | 20.70 |
| Other surgery specialty | 833 | 20.23 | 20.05 | 302 | 25.44 | 20.92 |
| Practice type | ||||||
| Solo/two physicians† | 1,566 | 38.04 | 37.80 | 360 | 30.33 | 32.32 |
| HMO or other prepaid practice‡,¥ | 161 | 3.91 | 4.06 | 26 | 2.19 | 2.44 |
| Community health center | n.a. | 131 | 11.04 | 3.06 | ||
| Other practice type | 2,390 | 58.05 | 58.14 | 670 | 56.44 | 62.18 |
| Revenue from Medicare | ||||||
| 50% or less | 3,417 | 83.00 | 82.91 | 982 | 82.73 | 80.06 |
| More than 50% | 700 | 17.00 | 17.09 | 144 | 12.13 | 14.34 |
| Missing | n.a. | 61 | 5.14 | 5.60 | ||
| Revenue from Medicaid | ||||||
| 50% or less | 3,867 | 93.93 | 94.04 | 1,054 | 88.79 | 90.08 |
| More than 50% | 250 | 6.07 | 5.96 | 70 | 5.90 | 4.10 |
| Missing | n.a. | 63 | 5.31 | 5.82 | ||
| Number of managed care contracts | ||||||
| None | 476 | 11.56 | 11.74 | 125 | 10.53 | 10.60 |
| 1 or more | 3,641 | 88.44 | 88.26 | 1,027 | 86.52 | 86.53 |
| Missing | n.a. | 35 | 2.95 | 2.87 | ||
| Gender | ||||||
| Male | 3,061 | 74.35 | 73.42 | n.a. | ||
| Female | 1,056 | 25.65 | 26.58 | n.a. | ||
| Race/ethnicity | ||||||
| Non-Hispanic White | 3,015 | 73.23 | 72.12 | n.a. | ||
| Hispanic | 224 | 5.44 | 5.44 | n.a. | ||
| Non-Hispanic Black | 135 | 3.28 | 3.39 | n.a. | ||
| Asian or Pacific Islander | 593 | 14.40 | 15.38 | n.a. | ||
| Other | 150 | 3.64 | 3.67 | n.a. | ||
| Year started practice | ||||||
| 1975 or earlier | 422 | 10.25 | 8.92 | n.a. | ||
| 1976–1990 | 1,663 | 40.39 | 40.22 | n.a. | ||
| 1991–2000 | 1,335 | 32.43 | 33.43 | n.a. | ||
| 2001 or later | 697 | 16.93 | 17.43 | n.a. | ||
| Geographic region | ||||||
| West | n.a. | 285 | 24.01 | 22.95 | ||
| Northeast | n.a. | 249 | 20.98 | 21.81 | ||
| Midwest | n.a. | 256 | 21.57 | 20.90 | ||
| South | n.a. | 397 | 33.45 | 34.34 | ||
| Non-MSA | n.a. | 109 | 9.18 | 9.41 | ||
Note: HMO: health maintenance organization; MSA: metropolitan statistical area.
In the NAMCS, only solo practice was included.
In the HTPS, only HMO setting was asked.
Weighted estimate from the NAMCS was based on fewer than 30 unweighted observations.
Electronic Health Records
In the two surveys, questions regarding EHR use were nearly identical. For example, in the HTPS, the physicians were asked, “Does your main practice use electronic medical records?” The choices were “Yes, all electronic;” “Yes, part electronic and part paper;” “No, all paper;” and “Don't know.” An EHR was defined as a “computer-based patient medical record.”25 In the NAMCS, physicians were asked, “Does your practice use electronic medical records (not including billing records)?”26 The same choices were provided, but no definition of an EHR was given in the physician induction interview form. For the purpose of this study, answers of “Don't know” were considered as having no EHRs.
Specific Health Information Technology Use for Clinical Activities
In addition to the use of EHRs in general, both surveys asked about the specific use of HIT for multiple clinical activities. These questions were asked independent of the question regarding EHR use in both surveys. In the HTPS, physicians were asked to think about the “use of computers and other forms of [HIT], including hand-held computers, in diagnosing or treating patients for a list of clinical activities.”27 For each activity where HIT was available, the physician was asked whether he or she personally used the technology. In the NAMCS, physicians were asked whether a “computerized system” was used in his or her practice to perform a list of clinical activities and whether the feature was turned off (i.e., not being used).28 For the purpose of this study, only those who had HIT available for a certain clinical activity and used it were counted.
Table 3 compares the list of clinical activities using HIT reported in the two surveys.29, 30 Although considerable overlap exists in the clinical activities included, there are significant differences. Both surveys asked about electronic prescribing, transmitting, and drug-interaction information. However, in the NAMCS, the latter two questions were asked only of those reporting availability of electronic prescribing, whereas in the HTPS, these questions were asked regardless of the use of HIT for writing prescriptions electronically. Although both surveys asked about HIT for patient information, only one general question regarding patient notes, problem lists, or medication lists was asked in the HTPS, but separate questions were asked in the NAMCS, some of which were conditional on the availability of other features. Both surveys also asked questions regarding electronic ordering of lab tests, and viewing lab results and images. The HTPS asked one general question regarding viewing results from laboratory and radiology tests. In contrast, the NAMCS asked separate questions regarding viewing lab results and images with a follow-up question confirming if images were sent electronically. Questions regarding formulary checking, electronic exchange of clinical information with other providers, and reminders to physicians and patients regarding preventive care and follow-up visits were asked only in the HTPS. On the other hand, questions regarding information on patient demographics and public reporting capacity were asked only in the NAMCS.
Table 3.
Survey Items for Health Information Technology Use in Physicians' Offices
| 2008 Health Tracking Physician Survey | 2008 National Ambulatory Medical Care Survey | ||||||
|---|---|---|---|---|---|---|---|
| Survey Item | All EHR | Partial EHR | No EHR | Survey Item | All EHR | Partial EHR | No EHR |
| Does your main practice use electronic medical records? | 24.31 | 23.93 | 51.76 | Does your practice use electronic medical records (not including billing)? | 27.24 | 18.40 | 54.37 |
| Is information technology available in YOUR PRACTICE for the following activities? (used sometimes or routinely) | Does your practice have a computerized system for the following? (not turned off) | ||||||
| Patient Information | |||||||
| Patient demographic information | 98.06 | 92.89 | 67.12 | ||||
| Demographic information including patient problem list | 68.90 | 47.43 | 10.20 | ||||
| Access to patient notes, medication lists, or problem lists | 97.32 | 81.63 | 19.39 | Clinical notes | 92.25 | 61.53 | 12.29 |
| Notes including medical history and follow-up notes | 82.44 | 53.24 | 9.04 | ||||
| Order-Entry Management | |||||||
| Write prescriptions | 86.88 | 45.01 | 11.34 | Orders for prescription | 84.73 | 49.97 | 10.25 |
| Transmitting prescriptions electronically to pharmacy | 69.09 | 32.56 | 12.92 | ||||
| Write and transmit prescriptions electronically to pharmacy (Constructed) | 68.03 | 28.83 | 8.44 | Prescription sent electronically to pharmacy if order prescriptions using computerized system | 54.07 | 28.91 | 6.12 |
| Order laboratory, radiology, or other diagnostic tests | 85.57 | 61.25 | 27.65 | Orders for tests | 71.34 | 36.92 | 11.80 |
| Test orders sent electronically | 43.37 | 18.74 | 6.56 | ||||
| Results Management | |||||||
| View results of laboratory, radiology, or other diagnostic test | 95.40 | 84.59 | 55.25 | Viewing laboratory results | 84.55 | 61.85 | 33.50 |
| Viewing imaging results | 71.74 | 53.77 | 28.94 | ||||
| Images electronically returned | 37.54 | 24.10 | 11.00 | ||||
| Exchange clinical data and images with other physicians | 75.59 | 52.69 | 18.84 | ||||
| Exchange clinical data and images with hospitals and laboratories | 68.09 | 49.46 | 23.26 | ||||
| Decision Support | |||||||
| Obtain information on potential patient drug interactions with other drugs, allergies, and/or patient conditions | 88.51 | 74.96 | 51.55 | ||||
| Obtain drug interaction information if electronically ordering prescriptions (Constructed) | 80.56 | 39.39 | 9.85 | Warning of drug interactions or contraindications provided if electronically ordering prescriptions | 64.24 | 39.04 | 6.90 |
| Obtain information about treatment alternatives or recommended guidelines | 90.24 | 86.19 | 70.45 | Out-of-range test levels highlighted | 65.52 | 45.00 | 25.85 |
| Obtain up-to-date decision support for diagnostic and treatment recommendations based on data about your patients and practice guideline | 77.18 | 68.64 | 50.87 | Reminders regarding guideline-based interventions or screening tests | 64.81 | 35.25 | 13.39 |
| Generate reminders for clinicians about preventive services | 56.37 | 29.46 | 15.16 | ||||
| Generate reminders for clinicians about other needed patient follow-up | 58.66 | 31.83 | 16.27 | ||||
| Generate reminders to patients about preventive services | 44.80 | 25.55 | 18.36 | ||||
| Communicate about clinical issues with patients by e-mail | 35.19 | 23.06 | 11.95 | ||||
| Obtain information on formularies | 59.83 | 47.17 | 29.44 | ||||
| Access information on patient's preferred language | 31.29 | 16.38 | 5.37 | ||||
| Public Health Reporting | |||||||
| Public health reporting | 32.14 | 14.90 | 8.48 | ||||
| Notifiable diseases sent electronically | 14.40 | 4.87 | 2.92 | ||||
Basic and Fully Functional Systems
Previous literature demonstrated the importance of distinguishing the use of an EHR system that can only perform limited functionalities from the use of systems that are fully functional.31 We adopted the terminology of “basic” and “fully functional” systems used in previous studies.32, 33 The definition of a fully functional system was derived from the Institute of Medicine's framework that defines possible functions of an EHR and was developed via consensus of an expert panel using a modified Delphi process.34, 35 A “basic” system has only the “minimum set of functions that would merit the use of the term ‘electronic health record’” determined by the expert panel.36 Table 4 listed the survey items used to define those systems. Since the NAMCS used nearly identical HIT items as in the study by DesRoches et al. (with the exception of the information on electronic list of medications taken by patients, which is not available from the 2008 NAMCS), the adoption was direct.37 For the HTPS, we adapted the definitions to the extent possible with items available in the survey. The most important difference was that more decision support features available in the HTPS were used to define a “fully functional” system (see Table 4). An EHR system that did not meet the criteria of a “basic” system was not considered a “true” EHR system. Based on these definitions, we classified physicians into three groups based on the functionality of their EHR systems: “fully functional,” “basic,” or “other.” The “other” category included both those reporting no EHRs and those with EHRs that did not meet the criteria of a “basic” system. Since questions regarding HIT use were asked independent of questions on EHRs, following previous studies, if a physician reported use of an EHR system, we assumed the reported HIT use was as part of the EHR system.38, 39
Table 4.
Operational Definitions of Basic and Fully Functional Electronic Health Record Systems
| 2008 Health Tracking Physician Survey | 2008 National Ambulatory Medical Care | ||||
|---|---|---|---|---|---|
| Survey Item | Basic System | Fully Function al System | Survey Item | Basic System | Fully Function al System |
| Is information technology available in YOUR PRACTICE for the following activities? | Does your practice have a computerized system for the following? | ||||
| Patient Information | |||||
| Patient demographic information | X | X | |||
| Demographic information including patient problem list | X | X | |||
| Access to patient notes, medication lists, or problem lists | X | X | Clinical notes | X | X |
| Notes including medical history and follow-up notes | X | ||||
| Order-Entry Management | |||||
| Write prescriptions | X | X | Orders for prescription | X | X |
| Transmitting prescriptions to pharmacy | X | Prescription sent electronically to pharmacy | X | ||
| Order laboratory, radiology, or other diagnostic tests | X | Orders for tests | X | ||
| Test orders sent electronically | X | ||||
| Results Management | |||||
| View results of laboratory, radiology, or other diagnostic test | X | X | Viewing laboratory results | X | X |
| Exchange clinical data and images with other physicians | X | Viewing imaging results | X | X | |
| Exchange clinical data and images with hospitals and laboratories | X | Images electronically returned | X | ||
| Decision Support | |||||
| Obtain information on potential patient drug interactions with other drugs, allergies, and/or patient conditions | X | Warning of drug interactions or contraindications provided | X | ||
| Obtain information about treatment alternatives or recommended guidelines | X | Out-of-range test levels highlighted | X | ||
| Obtain up-to-date decision support for diagnostic and treatment recommendations based on data about your patients and practice guideline | X | Reminders regarding guideline-based interventions or screening tests | X | ||
| Generate reminders for clinicians about preventive services | X | ||||
| Generate reminders for clinicians about other needed patient follow-up | X | ||||
| Adoption level; % of Physicians(95% CI) | 22.29 (21.01–23.63) | 7.84 (7.03–8.73) | Adoption level: % of Physicians(95% CI) | 11.16 (9.04–13.69) | 4.56 (3.09–6.68) |
Data Analysis
We calculated nationally representative estimates using weights provided in each survey. In the NAMCS, standard errors (SEs) and 95 percent confidence intervals (CIs) were estimated using the ultimate cluster design variables provided in the public-use data, which have been shown to generate reliable estimates.40 No design variables are available in the public-use HTPS to account for the survey design. However, the HTPS employed a simple design that is very close to a simple random sampling (SRS).41 According to the in-house test conducted by the HTPS, the mean and median design effects (deff) of 88 means and proportions using both the total sample and specialty subgroups were both equal to 1.02.42 Deff is “the ratio of the sampling variance given the actual survey design over the variance assuming SRS”; a deff of 1.02 means that the actual sampling variance was 2 percent larger than that if SRS was employed.43 Following the HTPS suggestion, we inflated the SEs estimated assuming SRS by 1.5 percent (equivalent to a 3 percent inflation of the sample variance); 95 percent CIs were estimated using the adjusted SEs.44
We also compared the physician and practice characteristics associated with the adoption of a “fully functional,” “basic,” or “other” system using multivariate regressions. Since “fully functional” systems were a subset of “basic” systems, we applied ordered logistic regression models.45 Physician and practice characteristics included in the regressions were those found in previous literature to be associated with adoption of EHRs.46–48 To the extent possible, we included variables that could be consistently defined in both surveys. The “full” models included both common variables and those available only in one survey. The “reduced” models included only common variables. However, because the NAMCS oversampled CHC providers, we retained the indicator for CHCs as well as those for missing values in the “reduced” model using the NAMCS data. For comparison between surveys, we reported marginal effects (dy/dx) at the weighted means of the independent variables. Regressions using the NAMCS data were estimated using “SVY” commands in Stata 9.2 to account for its complex survey design. For regressions using the HTPS data, since the public-use data file lacks sample design variables, we estimated the models using pseudo-maximum likelihood estimation with Huber-White robust standard errors and weighted using sampling weights that adjust for nonresponses.
All analyses were conducted using SAS 9.2 and Stata 9.2. For comparisons of estimates between surveys, nonoverlapping 95 percent CIs were regarded as statistically significant differences.
Human Subject Protection
This study used only public-use data and institutional review was not required.
Results
Table 3 compares the EHR use and specific HIT applications for various clinical activities among office-based physicians using the two surveys. There was no significant difference in the estimated proportions of physicians using all EHRs (HTPS: 24.31 percent, 95 percent CI: 22.99–25.69 percent vs. NAMCS: 27.24 percent, 95 percent CI: 23.53–31.29 percent). However, a higher proportion of physicians using partial EHRs was reported in the HTPS than in the NAMCS (23.93 percent, 95 percent CI: 22.61–25.30 percent vs. 18.40 percent, 95 percent CI: 15.62–21.54 percent). Although items were available in both surveys regarding HIT use for patient information, order-entry management, results management, and decision support, the specific items used in those domains were different and not very comparable. The closest item was for electronically writing/ordering prescriptions, and the proportions of physicians reporting using HIT for this activity were very close in the two surveys for overall use (HTPS: 37.76 percent, 95 percent CI: 36.25–39.30 percent vs. NAMCS: 37.84 percent, 95 percent CI: 34.35–41.47 percent) and by all-EHR, partial-EHR, and no-EHR users. For other items that were comparable (e.g., ordering tests, making clinical notes, electronically submitting prescriptions to a pharmacy, viewing test results), the HTPS generally estimated higher use than the NAMCS.
We further classified an EHR system as a “basic” or a “fully functional” system. Both surveys estimated low use of “fully functional” systems (HTPS: 7.84 percent, 95 percent CI: 7.03–8.73 percent vs. NAMCS: 4.56 percent, 95 percent CI: 3.09–6.68 percent). However, reported use of “basic” systems was much higher in the HTPS than in the NAMCS (22.29 percent vs. 11.16 percent) (see Table 4). Table 5 and Table 6 report marginal effects from the multivariate analyses. Although the magnitudes of the marginal effects were different, the directions of the effects were generally consistent across the two surveys. Controlling for other physician and practice characteristics, both surveys found that small practices (solo or two physicians), physicians in psychiatry or surgical specialties, and those receiving more than 50 percent of revenues from Medicare were significantly less likely to use a “basic” or a “fully functional” system. On the other hand, physicians in HMOs or other prepaid managed care practices were more likely to use a “basic” system. Using the HTPS, differences across gender, race/ethnicity, and years in practice were also found. Using the NAMCS, physicians in the western region had the highest use of EHR systems.
Table 5.
Use of a Basic Electronic Health Record System
| 2008 Health Tracking Physician Survey (HTPS) |
2008 National Ambulatory Medical Care Survey (NAMCS) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Full Model Marg. Eff. | Reduced Model Marg. Eff. | Full Model Marg. Eff. | Reduced Model Marg. Eff. | |||||
| Specialty | ||||||||
| Internal medicine/general or family practice | [R] | [R] | [R] | [R] | ||||
| Pediatrics | −7.75% | *** | −8.20% | *** | −0.11% | 0.01% | ||
| OB/GYN | −4.93% | ** | −4.98% | ** | −3.91% | −4.07% | * | |
| Psychiatry | −14.23% | *** | −14.35% | *** | −6.08% | *** | −6.03% | *** |
| Other medical specialty | −3.77% | *** | −3.56% | *** | 0.02% | 0.04% | ||
| Other surgery specialty | −9.39% | *** | −8.70% | *** | −4.60% | ** | −4.55% | ** |
| Practice type | ||||||||
| Solo/two physicians† | −15.34% | *** | −16.25% | *** | −5.80% | *** | −5.57% | *** |
| HMO or other prepaid practice‡,¥ | 20.23% | *** | 19.94% | *** | 14.91% | ** | 18.87% | *** |
| Community health center | n.a. | −0.56% | 0.24% | |||||
| Other practice type | [R] | [R] | [R] | [R] | ||||
| Revenue from Medicare | ||||||||
| 50% or less | [R] | [R] | [R] | [R] | ||||
| More than 50% | −5.98% | *** | −6.36% | *** | −6.66% | *** | −6.63% | *** |
| Missing | n.a | n.a | 12.87% | 10.87% | ||||
| Revenue from Medicaid | ||||||||
| 50% or less | [R] | [R] | [R] | [R] | ||||
| More than 50% | −1.71% | −1.43% | −6.12% | *** | −5.97% | ** | ||
| Missing | n.a | n.a | −5.21% | −4.72% | ||||
| Number of managed care contracts | ||||||||
| None | −2.31% | −2.78% | * | −7.54% | *** | −7.43% | *** | |
| 1 or more | [R] | [R] | [R] | [R] | ||||
| Missing | n.a | n.a | −3.82% | −3.49% | ||||
| Female | −2.57% | ** | n.a | |||||
| Race/ethnicity | ||||||||
| Non-Hispanic White | [R] | n.a | ||||||
| Hispanic | −0.76% | n.a | ||||||
| Non-Hispanic Black | −1.44% | n.a | ||||||
| Asian | −2.76% | * | n.a | |||||
| Other | −5.18% | * | n.a | |||||
| Year started practice | ||||||||
| 1975 or earlier | −14.66% | *** | n.a | |||||
| 1976–1990 | −7.70% | *** | n.a | |||||
| 1991–2000 | −4.40% | *** | n.a | |||||
| 2001 or later | [R] | n.a | ||||||
| Geographic region | ||||||||
| West | n.a. | [R] | ||||||
| Northeast | n.a. | −1.10% | ||||||
| Midwest | n.a. | −3.97% | ** | |||||
| South | n.a. | −3.20% | * | |||||
| Non-MSA | n.a. | 1.14% | ||||||
Note: HMO: health maintenance organization; MSA: metropolitan statistical area.
In the NAMCS, only solo practice was included.
In the HTPS, only HMO-setting was asked.
Estimate from the NAMCS was based on fewer than 30 unweighted observations.
p < .01
p < .05
p < .10
Table 6.
Use of a Fully Functional Electronic Health Record System
| 2008 Health Tracking Physician Survey (HTPS) |
2008 National Ambulatory Medical Care Survey (NAMCS) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Full Model Marg. Eff. | Reduced Model Marg. Eff. | Full Model Marg. Eff. | Reduced Model Marg. Eff. | |||||
| Specialty | ||||||||
| Internal medicine/general or family practice | [R] | [R] | [R] | [R] | ||||
| Pediatrics | −2.35% | *** | −2.56% | *** | −0.05% | 0.00% | ||
| OB/GYN | −1.55% | *** | −1.62% | *** | −1.47% | −1.55% | ||
| Psychiatry | −3.97% | *** | −4.14% | *** | −2.22% | ** | −2.23% | ** |
| Other medical specialty | −1.24% | *** | −1.21% | *** | 0.01% | 0.02% | ||
| Other surgery specialty | −2.92% | *** | −2.81% | *** | −1.75% | ** | −1.76% | ** |
| Practice type | ||||||||
| Solo/two physicians† | −5.12% | *** | −5.64% | *** | −2.25% | *** | −2.19% | *** |
| HMO or other prepaid | ||||||||
| practice‡,¥ | 37.51% | *** | 36.61% | *** | 8.00% | * | 11.70% | ** |
| Community health center | n.a. | −0.22% | 0.10% | |||||
| Other practice type | [R] | [R] | [R] | [R] | ||||
| Revenue from Medicare | ||||||||
| 50% or less | [R] | [R] | [R] | [R] | ||||
| More than 50% | −1.90% | *** | −2.08% | *** | −2.47% | *** | −2.50% | *** |
| Missing | n.a. | n.a. | 6.46% | 5.30% | ||||
| Revenue from Medicaid | ||||||||
| 50% or less | [R] | [R] | [R] | [R] | ||||
| More than 50% | −0.56% | −0.49% | −2.22% | *** | −2.20% | ** | ||
| Missing | n.a. | n.a. | −1.92% | −1.78% | ||||
| Number of managed care | ||||||||
| contracts | ||||||||
| None | −0.76% | −0.94% | * | −2.76% | *** | −2.75% | *** | |
| 1 or more | [R] | [R] | [R] | [R] | ||||
| Missing | n.a. | n.a. | −1.42% | −1.32% | ||||
| Female | −0.86% | ** | n.a. | |||||
| Race/ethnicity | ||||||||
| Non-Hispanic White | [R] | n.a. | ||||||
| Hispanic | −0.26% | n.a. | ||||||
| Non-Hispanic Black | −0.48% | n.a. | ||||||
| Asian | −0.91% | * | n.a. | |||||
| Other | −1.61% | ** | n.a. | |||||
| Year started practice | ||||||||
| 1975 or earlier | −4.13% | *** | n.a. | |||||
| 1976–1990 | −2.58% | *** | n.a. | |||||
| 1991–2000 | −1.46% | *** | n.a. | |||||
| 2001 or later | [R] | n.a. | ||||||
| Geographic region | ||||||||
| West | n.a. | [R] | ||||||
| Northeast | n.a. | −0.43% | ||||||
| Midwest | n.a. | −1.52% | * | |||||
| South | n.a. | −1.25% | ||||||
| Non-MSA | n.a. | 0.46% | ||||||
Note: HMO: health maintenance organization; MSA: metropolitan statistical area.
In the NAMCS, only solo practice was included.
In the HTPS, only HMO setting was asked.
Estimate from NAMCS was based on 30 or fewer unweighted observations.
p < .01
p < .05
p < .10
Discussion
We compared two contemporaneous physician surveys on EHR use and specific HIT applications for clinical activities. To the best of our knowledge, these are the only two nationally representative and public-use physician surveys that contain information on HIT use. Therefore, this study provided a rare opportunity to compare and cross-validate the national estimates of HIT adoption. The HTPS, which contains more than four times as many physicians as the NAMCS, is relatively less known to researchers. Thus, this study also provided an introduction of this source for tracking HIT use among physicians.
We found consistent estimates of all-EHR use between the surveys; however, estimates of partial-EHR use varied significantly despite the nearly identical questions on EHR use in the two surveys. One possible explanation was the uncertainty regarding what constitutes an EHR. A brief definition of an EHR was provided in the HTPS survey instrument, but not in the NAMCS. The observed difference may reflect this additional clarification. On the other hand, the NAMCS was conducted through one telephone and two in-person interviews. Such live encounters could allow double-checking of information provided by the respondents, which may also affect the responses. Despite these differences, in both surveys the physicians using all EHRs reported higher use of HIT for all clinical activities included in the surveys than those using only partial or no EHRs. This finding may suggest that EHRs with those clinical functionalities integrated into the system may be easier to use than stand-alone systems to perform these clinical activities. Alternatively, because the time since adoption is unknown, this finding could also reflect early adopters' growing comfort with these systems over time and their willingness to apply EHRs more broadly.
Comparison of the two contemporaneous surveys also demonstrated the difficulties in obtaining precise information through surveys and the importance of follow-up questions. For instance, in the HTPS, when respondents were asked a single question regarding HIT use for accessing patient notes, problem lists, or medication lists, 97.3 percent of physicians using all EHRs reported HIT use for this clinical activity. This estimate was comparable to the reported general use of a computerized system for clinical notes in the NAMCS (92.3 percent of physicians using all EHRs). However, when additional follow-up questions were asked in the NAMCS regarding access to specific information such as patient problem lists, medical history, and follow-up notes, the prevalence of use was much lower, especially for problem lists. Only 63.4 percent of all-EHR users in the NAMCS were using a computerized system that included all of the above-mentioned information: problem lists, clinical notes, medical history, and follow-up notes.
Although accessing patient information or test results using HIT implies electronically storing this information, it could not be determined from either survey how the information was stored. If only scanned copies of patient notes or test results were included, the information may be less helpful as this format prevents the information from being searched and used by decision support tools to aid clinical decision making. This was particularly likely among those using only partial EHRs (i.e., still using part paper records). While national surveys provide an important opportunity to track the adoption of EHRs and other HIT for clinical activities at a national level, details regarding the specific systems adopted and their implementation were often lacking. However, EHR systems can vary considerably from practice to practice. Without such details, it is hard to gauge the actual use or effectiveness of these systems.
Electronic exchange of clinical data among providers is a core objective of Stage 1 “meaningful use” of EHRs for incentive payments in 2011–2012.49 According to the HTPS, about 40 percent reported use of HIT for such exchange. The prevalence was even higher among physicians using all EHRs (75.6 percent for exchange with other physicians and 68.1 percent for exchange with hospitals or laboratories). Although whether an EHR system had such capacity could not be ascertained in this survey, the fact that higher availability and use among all-EHR users suggests that EHRs may enable easier exchange of data. However, at least at the time of these surveys, few EHR systems can communicate directly with each other; such electronic exchange between providers or with hospitals and laboratories may be limited to sending scanned copies unless the exchange is within a closed health system. As demonstrated by the NAMCS, when asked if a computerized system was used for viewing images, 71.7 percent of physicians using all EHRs reported such HIT application. However, when asked if images were actually sent electronically, the number dropped to 37.5 percent, suggesting that manual scanning of images may be needed at many of those practices.
Both surveys found that physicians in small practices (solo or two physicians) were significantly less likely to use a “basic” or a “fully functional” system. This finding is consistent with other studies.50, 51 Approximately 3 percent of physicians in small practices were estimated by both surveys to be using “fully functional” systems in 2008. With such a low rate of use in 2008, to implement an EHR system that will meet the “meaningful use” requirements in 2011–2012, physicians in small practices may face significantly more challenges both financially and technologically than larger practices. Moreover, in both surveys, a higher proportion of physicians in small practices received more than 50 percent of revenue from Medicare, and physicians receiving more than 50 percent of their revenue from Medicare were found to be less likely to adopt a “basic” or a “fully functional” system. Such a combination indicates an even more troublesome prospect for physicians in small practices; if adoption and “meaningful use” cannot be established by the end of the five-year incentive period, they will face further reduction in revenue because of their higher dependence on Medicare payments.52
Providers in psychiatry were also significantly less likely to use a “basic” or a “fully functional” system compared to primary care physicians. Mental health providers are generally more concerned about ensuring the confidentiality of patient information—especially mental health information—in EHRs.53 This likely reflects the “long-standing conventions concerning confidentiality in the mental health field”; in addition, various “federal laws and regulations that govern the treatment and release of certain information regarding mental health and alcohol and other drug abuse” add to the challenge of adopting EHRs in mental health practices.54
Use of “basic” or “fully functional” systems was also lower among physicians in surgical specialties. This disparity likely reflected the concern that the existing systems and requirements for their meaningful use generally are “geared toward primary care medical practices, which can limit the utility of EHRs for specialty surgical practice,” as voiced in the recently released position statement on EHRs by the American Academy of Orthopaedic Surgeons (AAOS).55 While recognizing the potential benefits of improving patient safety and quality of care, the AAOS urges the recognition of the “differences in needs and uses of EHR by disparate medical specialties, especially the differences between surgical specialties and primary care specialties.”56 Since the actual use of EHRs rather than the general access to them were examined in this study, the lower reported use among surgeons may also represent the delegation of use to other staff members at their practices.57
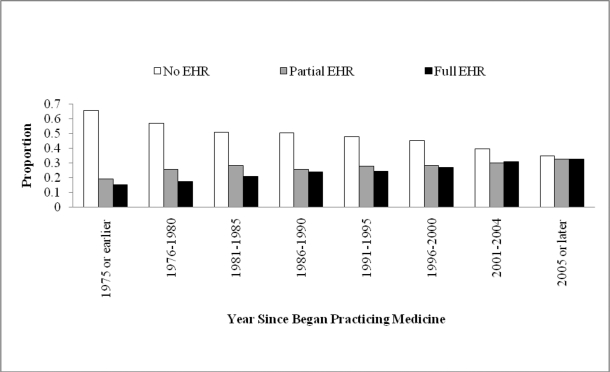
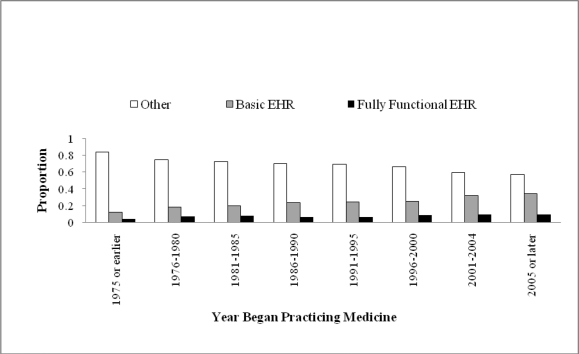
Use of both “basic” and “fully functional” systems was inversely related to the number of years in practice (see Figure 1 and Figure 2), which is consistent with previous studies.58, 59 The effect persists even after controlling for other physician characteristics using multivariate analyses. Older physicians who have been in practice for a longer time may have less experience and comfort with HIT or information technology use in general than younger physicians. Such age difference in HIT adoption by physicians was also reported in some previous studies but not in others.60–62 Nonetheless, this age difference in HIT use will likely disappear over time with better education and as the older physicians retire from practices.63
Figure 1.
Electronic Health Record Adoption by Year Since Began Practicing Medicine: 2008 Health Tracking Physician Survey (No EHR, Partial EHR, Full EHR)
Figure 2.
Electronic Health Record Adoption by Year Since Began Practicing Medicine: 2008 Health Tracking Physician Survey (Other, Basic EHR, Fully Functional EHR)
Using the 2008 HTPS, we found that female physicians were less likely to use “basic” or “fully functional” systems than male physicians. Previous literature has shown mixed results regarding gender differences in HIT adoption.64–67 Many of these studies were limited either to one specialty or to a few states, suggesting possible variations across geographic regions or by physician specialties in the relationship between gender and HIT adoption.68–70 Although we have controlled for large geographic regions and several physician specialty groups in the multivariate analyses, there may be residual variations not captured by the categories that we examined in the regression analyses. A previous national study of physicians failed to find a gender difference in adoption of EHRs.71 Future studies are needed to further explore this issue and determine if there are gender-specific barriers to HIT use by physicians.
Compared with non-Hispanic whites, physicians in the “other” race/ethnicity group had a significantly lower use of “fully functional” systems (p < .05). This “other” group was a residual category capturing all other non-Hispanic racial/ethnic minorities excluding non-Hispanic blacks and Asians (or Pacific Islanders) but including those reporting mixed race. Unfortunately, the 2008 public-use HTPS does not have information to further divide this group. Future studies that oversample physicians in these minority groups are needed to determine which subgroup(s) may be at a disadvantage in HIT use. This finding is contrary to a previous national study that found insignificant race/ethnicity differences.72 However, our study included nearly three times as many physicians in the “other” category than the previous study (150 from the 2008 HTPS vs. 35 in the previous study), which may partially explain the difference in findings.73 Moreover, physicians who serve disproportionately Hispanic patient populations may be at a disadvantage in adopting comprehensive EHRs.74
Limitations
Several limitations of this study should be discussed. As alluded to in the previous discussion, the information on EHR or specific HIT use for clinical activities was not detailed in both surveys to determine the actual implementation and effectiveness of these systems. This lack of detail, however, is a common limitation of large national surveys. To define “basic” and “fully functional” systems, we assumed that the reported HIT use was part of the EHR system. However, this could not be ascertained in either survey and likely resulted in overestimation of the prevalence of these systems particularly among users of partial EHRs (i.e., part paper and part electronic).
Many practices use practice management software for administrative and financial matters that may include functionalities such as patient demographic characteristics, but the surveys lack information on use of such HIT in the offices. Also, because of the differences in survey items used for HIT use, the definitions of a “fully functional” system were not directly comparable between the two surveys. Additionally, although we attempted to define the physician or practice characteristics as similarly as possible in the two surveys, discrepancies remained because of data availability, which may have led to differential estimates. Nonetheless, generally consistent findings were found despite these differences.
Also, this study used data from 2008, which is the latest year with public-use files available from both surveys. With the passage of the HITECH Act in 2009 and the release of final rules for Stage 1 “meaningful use” in July 2010, many changes likely have taken place since then. The preliminary findings from the 2010 NAMCS (not yet available for public use) by the CDC found that 50.7 percent of physicians reported use of EHRs in 2010, but only one-fifth of them (or 10 percent of the total of physicians) were using “fully functional” systems based on the same definition as in this study, suggesting only small (absolute) improvement since 2008.75 Estimates from this study provide useful baseline information to facilitate comparisons with future development under the multiyear incentive program to monitor diffusion of EHRs over time.
Conclusion
This study exploited a unique opportunity to compare the estimates of the EHR adoption and specific HIT use for clinical activities in physician offices using data from two contemporaneous, nationally representative physician surveys. To the extent that the results from the two surveys were consistent, they lent credibility to the estimated results. While nearly half of physicians reported use of some EHRs in their practices, only 4.6–7.8 percent of office-based physicians had systems that met the criteria of a “fully functional” system in 2008. The definition of a “fully functional” system used in this study was far less stringent than that required for Stage 1 “meaningful use” of EHRs to receive the incentive payments in 2011 and 2012.76 Given that the latest estimates showed only a small (absolute) increase in the use of “fully functional” systems in 2010 (10.1 percent), it may be a daunting task for physicians, particularly those in small practices, to adopt EHRs and achieve “meaningful use” in the next two years.77 On the other hand, 51 percent of physicians were already using partial or full EHRs by 2010, and half of them reported systems that met the criteria of a “basic” system, suggesting that either expanding existing systems or adopting new systems that qualify for “meaningful use” may be less challenging among those providers than the low adoption rate of “fully functional” systems suggested.78 According to the Office of the National Coordinator for Health Information Technology (ONC) Web site, 41 percent of office-based physicians are planning to achieve meaningful use of EHRs and apply for incentive payments and 32.4 percent plan to apply this year, which indicates a more promising overall prospective.
The year 2011 is the first of the five-year incentive payment period. It is still too early to know the impact of the incentive payments on the diffusion of EHRs among physicians. However, lessons can be learned from the recent experience in England with the implementation and adoption of nationwide EHRs, which revealed many unexpected macro-, meso-, and microlevel challenges.79 England took a “top-down” approach with “government driven, national implementations of standardized, commercial software applications.”80 The implementation has been significantly delayed despite the continued enthusiasm among providers. One of the major complaints was the inflexibility of the standardized software to meet local needs. Unlike England, the United States is taking a “bottom-up” approach without nationwide standardization of systems but is requiring the systems to have necessary clinical and public-reporting capacities. Although this approach may alleviate some of the tension experienced in England, the core and menu requirements specified by the final rules of Stage 1 “meaningful use” for incentive payments further restrict the local choices. While local organizations may have the freedom to choose their systems under this approach, this freedom likely will create more difficulties down the road in achieving interoperability across systems. Experiences in England demonstrated that even with nationwide standardized systems, interoperability remains a great challenge.81, 82 Along with interoperability comes the question of how to achieve the optimal balance between protecting patient confidentiality and supporting patient care.
Acknowledgments
Special thanks to Paul O. Gubbins, PharmD, for editing this manuscript. Any errors that remain are ours.
Notes
- 1.U.S. Department of Health and Human Services, Office of the National Coordinator for Health Information Technology. “Glossary of Selected Terms Related to Health IT.” Available at http://healthit.hhs.gov/portal/server.pt/community/health_it_hhs_gov__glossary/1256 (accessed May 30, 2011).
- 2.Amarasingham Ruban, et al. “Clinical Information Technologies and Inpatient Outcomes: A Multiple Hospital Study.”. Archives of Internal Medicine. 2009;169(no. 2):108–14. doi: 10.1001/archinternmed.2008.520. [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal David, et al. Health Information Technology in the United States: The Information Base for Progress. Princeton, NJ: Robert Wood Johnson Foundation; 2006. [Google Scholar]
- 4.Chaudhry Basit, et al. “Systematic Review: Impact of Health Information Technology on Quality, Efficiency, and Costs of Medical Care.”. Annals of Internal Medicine. 2006;144(no. 10):E12–E22. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 5.Hsiao, Chun-Ju, et al. “Electronic Medical Record/Electronic Health Record Systems of Office-based Physicians: United States, 2009 and Preliminary 2010 State Estimates.” National Center for Health Statistics (NCHS) Health E-stat, December 2010. Available at http://www.cdc.gov/nchs/data/hestat/emr_ehr_09/emr_ehr_09.htm [PubMed]
- 6.Blumenthal David, Tavenner Marilyn. “The ‘Meaningful Use’ Regulation for Electronic Health Records.”. New England Journal of Medicine. 2010;363(no. 6):501–4. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 7.Romano Max J, Stafford Randall S. “Electronic Health Records and Clinical Decision Support Systems: Impact on National Ambulatory Care Quality.”. Archives of Internal Medicine. 2011;171(no. 10):897–903. doi: 10.1001/archinternmed.2010.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Chenghui, West-Strum Donna. “Patient Panel of Underserved Populations and Adoption of Electronic Medical Record Systems by Office-based Physicians.”. Health Services Research. 2010;45(no. 4):963–84. doi: 10.1111/j.1475-6773.2010.01113.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keyhani Salomeh, et al. “Electronic Health Record Components and the Quality of Care.”. Medical Care. 2008;46(no. 12):1267–72. doi: 10.1097/MLR.0b013e31817e18ae. [DOI] [PubMed] [Google Scholar]
- 10.Linder Jeffery A, et al. “Electronic Health Record Use and the Quality of Ambulatory Care in the United States.”. Archives of Internal Medicine. 2007;167(no. 13):1400–1405. doi: 10.1001/archinte.167.13.1400. [DOI] [PubMed] [Google Scholar]
- 11.Hing Esther S, et al. “Electronic Medical Record Use by Office-based Physicians and Their Practices: United States, 2006.”. Advance Data. 2007;(no. 393):1–7. [PubMed] [Google Scholar]
- 12.Elder Keith T, et al. “Health Information Technology and Physician Career Satisfaction.”. Perspectives in Health Information Management. Summer 2010:1–18. [PMC free article] [PubMed] [Google Scholar]
- 13.Grossman, Joy M. Even When Physicians Adopt E-Prescribing, Use of Advanced Features Lags (Issue Brief No. 133). Center for Studying Health System Change, July 2010. [PubMed]
- 14.Pagán Jose J, et al. “Which Physicians Have Access to Electronic Prescribing and Which Ones End Up Using It?”. Health Policy. 2009;89(no. 3):288–94. doi: 10.1016/j.healthpol.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. 2008 National Ambulatory Care Survey Micro-Data File Documentation Available at http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm (accessed April 5, 2011).
- 16.Strouse, Richard, et al. HSC 2008 Health Tracking Physician Survey Methodology Report (Technical Publication No. 77). Center for Studying Health System Change, September 2009. Available at http://www.hschange.org (accessed April 5, 2011).
- 17.Centers for Disease Control and Prevention. 2008 National Ambulatory Care Survey Micro-Data File Documentation Available at http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm (accessed April 5, 2011).
- 18.Centers for Disease Control and Prevention. 2008 National Ambulatory Care Survey Micro-Data File Documentation Available at http://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm (accessed April 5, 2011).
- 19.Strouse, Richard, et al. HSC 2008 Health Tracking Physician Survey Methodology Report (Technical Publication No. 77).
- 20.Strouse, Richard, et al. HSC 2008 Health Tracking Physician Survey Methodology Report (Technical Publication No. 77).
- 21.Centers for Disease Control and Prevention. 2008 National Ambulatory Care Survey Micro-Data File Documentation
- 22.Strouse, Richard, et al. HSC 2008 Health Tracking Physician Survey Methodology Report (Technical Publication No. 77).
- 23.Centers for Disease Control and Prevention. National Ambulatory Medical Care Survey: 2008 Summary Tables Available at http://www.cdc.gov/nchs/ahcd/web_tables.htm (accessed April 5, 2011).
- 24.Boukus, Ellyn, et al. A Snapshot of U.S. Physicians: Key Findings from the 2008 Health Tracking Physician Survey (Data Bulletin No. 35). Center for Studying Health System Change, September 2009. [PubMed]
- 25.Center for Study Health System Change. 2008 HSC Health Tracking Physician Survey Public Use File: User's Guide Available at http://www.icpsr.umich.edu (accessed April 5, 2011).
- 26.Centers for Disease Control and Prevention. 2008 National Ambulatory Care Survey Micro-Data File Documentation
- 27.Center for Study Health System Change. 2008 HSC Health Tracking Physician Survey Public Use File: User's Guide
- 28.Centers for Disease Control and Prevention. 2008 National Ambulatory Care Survey Micro-Data File Documentation
- 29.Centers for Disease Control and Prevention. 2008 National Ambulatory Care Survey Micro-Data File Documentation
- 30.Center for Study Health System Change. 2008 HSC Health Tracking Physician Survey Public Use File: User's Guide
- 31.Li, Chenghui, Donna West-Strum. “Patient Panel of Underserved Populations and Adoption of Electronic Medical Record Systems by Office-based Physicians.” [DOI] [PMC free article] [PubMed]
- 32.Hsiao Chun-Ju, et al. “Electronic Medical Record/Electronic Health Record Systems of Office-based Physicians: United States, 2009 and Preliminary 2010 State Estimates.” [PubMed]
- 33.DesRoches Catherine M, et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.”. New England Journal of Medicine. 2008;359(no. 1):50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- 34.DesRoches Catherine M, et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.”. New England Journal of Medicine. 2008;359(no. 1):50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- 35.International Organization for Standardization. Electronic Health Record Definition, Scope, and Context, 2nd draft (ISO/TC 215 Technical Report). Geneva: International Organization for Standardization, August 2003.
- 36.DesRoches, Catherine M., et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.” [DOI] [PubMed]
- 37.DesRoches, Catherine M., et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.” [DOI] [PubMed]
- 38.Hsiao, Chun-Ju, et al. “Electronic Medical Record/Electronic Health Record Systems of Office-based Physicians: United States, 2009 and Preliminary 2010 State Estimates.” [PubMed]
- 39.DesRoches, Catherine M., et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.” [DOI] [PubMed]
- 40.Hing Esther, et al. “Guide to Using Masked Design Variables to Estimate Standard Errors in Public Use Files of the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey.”. Inquiry. 2003;40(no. 4):401–15. doi: 10.5034/inquiryjrnl_40.4.401. [DOI] [PubMed] [Google Scholar]
- 41.Center for Study Health System Change. 2008 HSC Health Tracking Physician Survey Public Use File: User's Guide
- 42.Center for Study Health System Change. 2008 HSC Health Tracking Physician Survey Public Use File: User's Guide
- 43.Center for Study Health System Change. 2008 HSC Health Tracking Physician Survey Public Use File: User's; Guide
- 44.Center for Study Health System Change. 2008 HSC Health Tracking Physician Survey Public Use File: User's; Guide
- 45.Boukus, Ellyn, et al. A Snapshot of U.S. Physicians: Key Findings from the 2008 Health Tracking Physician Survey [PubMed]
- 46.Li, Chenghui, and Donna West-Strum. “Patient Panel of Underserved Populations and Adoption of Electronic Medical Record Systems by Office-based Physicians.” [DOI] [PMC free article] [PubMed]
- 47.DesRoches, Catherine M., et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.” [DOI] [PubMed]
- 48.Bruen Brian K, et al. “More Than Four in Five Office-based Physicians Could Qualify for Federal Electronic Health Record Incentives.”. Health Affairs. 2011;30(no. 3):472–80. doi: 10.1377/hlthaff.2010.0932. [DOI] [PubMed] [Google Scholar]
- 49.Blumenthal, David, and Marilyn Tavenner. “The ‘Meaningful Use’ Regulation for Electronic Health Records.” [DOI] [PubMed]
- 50.Li, Chenghui, and Donna West-Strum. “Patient Panel of Underserved Populations and Adoption of Electronic Medical Record Systems by Office-based Physicians.” [DOI] [PMC free article] [PubMed]
- 51.Bruen, Brian K., et al. “More Than Four in Five Office-based Physicians Could Qualify for Federal Electronic Health Record Incentives.” [DOI] [PubMed]
- 52.Blumenthal, David, and Marilyn Tavenner. “The ‘Meaningful Use’ Regulation for Electronic Health Records.” [DOI] [PubMed]
- 53.Salomon Ronald M, et al. “Openness of Patients' Reporting with Use of Electronic Records: Psychiatric Clinicians' Views.”. Journal of American Medical Informatics Association. 2009;17:54–60. doi: 10.1197/jamia.M3341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Peterson David, Wickeham Dan. “New Challenge for Academic Psychiatry: The Electronic Health Record.”. Academic Psychiatry. 2010;35(no. 2):76–80. doi: 10.1176/appi.ap.35.2.76. [DOI] [PubMed] [Google Scholar]
- 55.American Academy of Orthopaedic Surgeons. “Position Statement: Electronic Health Records.” Available at http://www.aaos.org/about/papers/position/1179.asp (accessed May 30, 2011).
- 56.American Academy of Orthopaedic Surgeons. “Position Statement: Electronic Health Records.” Available at http://www.aaos.org/about/papers/position/1179.asp (accessed May 30, 2011).
- 57.Orchard Margo C, et al. “Access to Electronic Health Records by Care Setting and Provider Type: Perceptions of Cancer Care Providers in Ontario, Canada.”. BMC Medical Informatics and Decision Making. 2009;9(no. 38):1–11.28. doi: 10.1186/1472-6947-9-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.DesRoches, Catherine M., et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.” [DOI] [PubMed]
- 59.Bramble James D, et al. “The Relationship between Physician Practice Characteristics and Physician Adoption of Electronic Health Records.”. Health Care Management Review. 2010;35(no. 1):55–64. doi: 10.1097/HMR.0b013e3181c3f9ad. [DOI] [PubMed] [Google Scholar]
- 60.Pagán, Jose J., et al. “Which Physicians Have Access to Electronic Prescribing and Which Ones End Up Using It?” [DOI] [PubMed]
- 61.Menachemi Nir, Brooks Robert G. “EHR and Other IT Adoption among Physicians: Results of a Large-Scale Statewide Analysis.”. Journal of Health Care Information Management. 2006;20(no. 3):79–87. [PubMed] [Google Scholar]
- 62.Loomis Glenn A, et al. “If Electronic Medical Records Are So Great, Why Aren't Family Physicians Using Them?”. Journal of Family Practice. 2002;51(no. 7):636–41. [PubMed] [Google Scholar]
- 63.Menachemi, Nir, and Robert G. Brooks. “EHR and Other IT Adoption among Physicians: Results of a Large-Scale Statewide Analysis.” [PubMed]
- 64.DesRoches, Catherine M., et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.” [DOI] [PubMed]
- 65.Bramble, James D., et al. “The Relationship between Physician Practice Characteristics and Physician Adoption of Electronic Health Records.” [DOI] [PubMed]
- 66.Menachemi, Nir, and Robert G. Brooks. “EHR and Other IT Adoption among Physicians: Results of a Large-Scale Statewide Analysis.” [PubMed]
- 67.Loomis, Glenn A., et al. “If Electronic Medical Records Are So Great, Why Aren't Family Physicians Using Them?” [PubMed]
- 68.Loomis, Glenn A., et al. “If Electronic Medical Records Are So Great, Why Aren't Family Physicians Using Them?” [PubMed]
- 69.Bramble, James D., et al. “The Relationship between Physician Practice Characteristics and Physician Adoption of Electronic Health Records.” [DOI] [PubMed]
- 70.Menachemi, Nir, and Robert G. Brooks. “EHR and Other IT Adoption among Physicians: Results of a Large-Scale Statewide Analysis.” [PubMed]
- 71.DesRoches, Catherine M., et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.” [DOI] [PubMed]
- 72.DesRoches, Catherine M., et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.” [DOI] [PubMed]
- 73.DesRoches, Catherine M., et al. “Electronic Health Records in Ambulatory Care—A National Survey of Physicians.” [DOI] [PubMed]
- 74.Li, Chenghui, and Donna West-Strum. “Patient Panel of Underserved Populations and Adoption of Electronic Medical Record Systems by Office-based Physicians.” [DOI] [PMC free article] [PubMed]
- 75.Hsiao, Chun-Ju, et al. “Electronic Medical Record/Electronic Health Record Systems of Office-based Physicians: United States, 2009 and Preliminary 2010 State Estimates.” [PubMed]
- 76.Blumenthal, David, and Marilyn Tavenner. “The ‘Meaningful Use’ Regulation for Electronic Health Records.” [DOI] [PubMed]
- 77.Hsiao, Chun-Ju, et al. “Electronic Medical Record/Electronic Health Record Systems of Office-based Physicians: United States, 2009 and Preliminary 2010 State Estimates.” [PubMed]
- 78.Hsiao, Chun-Ju, et al. “Electronic Medical Record/Electronic Health Record Systems of Office-based Physicians: United States, 2009 and Preliminary 2010 State Estimates.” [PubMed]
- 79.Orchard, Margo C., et al. “Access to Electronic Health Records by Care Setting and Provider Type: Perceptions of Cancer Care Providers in Ontario, Canada.” [DOI] [PMC free article] [PubMed]
- 80.Robertson Ann, et al. “Implementation and Adoption of Nationwide Electronic Health Records in Secondary Care in England: Qualitative Analysis of Interim Results from a Prospective National Evaluation.”. British Medical Journal. 2010;341:1–12. doi: 10.1136/bmj.c4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Robertson Ann, et al. “Implementation and Adoption of Nationwide Electronic Health Records in Secondary Care in England: Qualitative Analysis of Interim Results from a Prospective National Evaluation.”. British Medical Journal. 2010;341:1–12. doi: 10.1136/bmj.c4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Greenhalgh Trisha, et al. “Adoption and Non-adoption of a Shared Electronic Summary Record in England: A Mixed-Method Case Study.”. British Medical Journal. 2010;340:1–11. doi: 10.1136/bmj.c3111. [DOI] [PubMed] [Google Scholar]