Abstract
Fractures of the metacarpal and phalanges constitute 10% of all fractures. No where in the body, the form and function are so closely related to each other than in hand. Too often these fractures are treated as minor injuries resulting in major disabilities. Diagnosis of skeletal injuries of the hand usually does not pose major problems if proper clinical examination is supplemented with appropriate radiological investigations. Proper preoperative planning, surgical intervention wherever needed at a centre with backing of equipment and implants, selection of appropriate anaesthesia and application of the principle of biological fixation, rigid enough to allow early mobilisation are all very important for a good functional outcome. This article reviews the current concepts in management of metacarpal and phalangeal fractures incorporating tips and indications for fixation of these fractures. The advantages and disadvantages of various approaches, anaesthesia, technique and mode of fixation have been discussed. The take-home message is that hand fractures are equally or more worthy of expertise as major extremity trauma are, and the final outcome depends upon the fracture personality, appropriate and timely intervention followed by proper rehabilitation. Hand being the third eye of the body, when injured it needs a multidisciplinary approach from the beginning. Though the surgeon's work appears to be of paramount importance in the early phase, the contribution from anaesthetist, physiotherapist, occupational therapist, orthotist and above all a highly motivated patient cannot be overemphasised.
Keywords: Skeletal hand trauma, metacarpal fractures, phalangeal fractures
INTRODUCTION
Fractures of the metacarpal and phalanges are common and constitute 10% of all fractures.[1] P. R. Lipscomb in 1963 stated that “too often these fractures are treated as minor injuries and major disabilities occur” underlying the wrong practice of considering these fractures as trivial and worthy of being treated by the junior most resident. The right perspective is reflected in the statement of Sir Reginald Watson-Jones who stated that “an open fracture of the phalanx is no less worthy of the skills of an expert than an open fracture of Femur” and further emphasised by Sir John Charnley that “the reputation of a surgeon may stand as much in jeopardy from a fracture of proximal phalanx as from any fracture of the femur”.
Epidemiology
Thirty to forty percentages of all fractures in the hand occur in the metacarpal. Border metacarpals (1st and 5th) are more commonly involved, the base being more commonly involved in the former and neck in the latter. Diaphyseal fractures are common in non border metacarpals. Life time incidence of metacarpal fractures is 2.5%. No where in the body, the form and function are so closely related to each other than in hand. So any skeletal injury in the hand is likely to alter the function.
Surgical anatomy
Metacarpal bones are concave, short tubular bones with in built longitudinal arch and a collective transverse arch. The metacarpal bases form the CMC joints with the carpal bones, the first being the most mobile, the 2nd and 3rd being most rigid and the 4th and 5th being relatively mobile. The saw tooth articular arrangement of the 2nd and 3rd CMC joints along with reinforcement of the capsule by FCR anteriorly and ECRL, ECRB posteriorly make the joints extremely rigid and immobile and any disruption of these joints indicate a high energy injury. The attachment of APL and ECU on the base of the 1st and 5th makes these joints more prone for unstable fracture dislocations.
The cam-shaped head of the metacarpal bones makes the collateral ligaments relaxed in extension and stretched in flexion making it safer to immobilise the MP joints in Flexion (ideally 70-90°) than in extension. This flexed position of the MP joint is also the most stable position of the MP joint in power pinch and grip.
The volar plate of the MP joints is a cartilaginous structure which is thicker at the phalangeal attachment and thinner at the metacarpal attachment. The lateral extension of the volar plate constitutes the deep transverse metacarpal ligament which provides the additional volar stability of the MP joint.
Metacarpal bones are subcutaneous bones dorsally with a gentle volar concavity. Fracture of the shaft or the neck of the metacarpal caused either due to direct or axial loading injury will mostly result in dorsal apex angulation due to the deforming forces of interossei and other volarly placed muscles. For this reason when these fractures are treated conservatively, the MP joint needs to be immobilised in flexion to relax the lumbricals and the interossei.
The precise incidence of phalangeal fractures is difficult to ascertain because of the high incidence of missed terminal phalangeal fractures. Though articular and periarticular fractures of the phalanges are mostly unstable, the shaft fracture of the middle and proximal phalanges depend on the personality of the fracture and integrity of the soft tissue including the periosteum. The displacement of proximal phalangeal fracture is usually volar apex angulation due to flexion of the proximal fragments and extension of the distal fragment due to interossei and extensor tendons respectively. The displacement in the middle phalangeal fractures depends on the site of the fracture and will be generally dorsal apex angulation in proximal 1/3rd and volar apex angulation in distal 1/3rd fractures.
Diagnosis and investigations
Diagnosis of skeletal injuries of the hand does not pose major problems unless very subtle or when they are a part of polytrauma. Deformity, shortening, overriding are usually obvious in closed and open injuries. Clinical examination should be supplemented with appropriate radiological investigations. A minimum of PA and lateral views and if needed oblique views and special views like Brewerton's view[2] and skyline view[3] for fracture head of the metacarpal bone, 30° pronated and 30° supinated oblique view[4] for 2nd and 5th metacarpal shaft fracture is warranted. Stress views may be indicated in certain fracture dislocations .Sophisticated investigations like CT and MRI are rarely used in acute skeletal injuries of the hand. Block or regional anaesthesia may facilitate to make it pain free and to obtain appropriate views.
General considerations
“Hand fractures can be complicated by deformity from no treatment, stiffness from overtreatment, and both deformity and stiffness from poor treatment”- Swanson[5]
A fracture is considered functionally stable when during clinical examination it is possible to actively move the fractured digit by 50% of range of motion painlessly. The fracture is considered radiologically stable when the radiographs of the fractured fragment in two planes show minimum angulation and displacement.[6] A fracture is considered unstable if it can not be reduced or maintained in an anatomic or near anatomic position without implant fixation when the hand is placed in the safe or functional position.[7] The four factors that determine the stability are 1) external force, 2) muscle imbalance 3) fracture configuration or personality 4) integrity of soft tissue including periosteal sleeve.
Ten tips for management of metacarpal and phalangeal fractures
Emphasis on proper clinical examination, proper investigation and early intervention either conservative or operative.
Surgical intervention must be opted only when one is sure of giving better results than conservative management.
Treat the problem with cafeteria approach. Familiarise with all methods, keep everything ready for either conservative or operative methods
Choice of anaesthesia- Bier's and WASH [10] (Wide awake surgery of hand) has distinct advantage over regional blocks and GA.
Use facilities like C arm, battery operated drill, magnification, bipolar, fine instruments etc. judiciously
Approach the fracture through safe zones irrespective of the choice of fixation.
Respect the soft tissue integrity. While repairing avoid additional soft tissue damage. Restore anatomy but not at the cost of flexibility.
Aim for stable biological fixation which permits early mobilisation.
Educate the patient properly. Rehabilitation protocol should be followed and proper follow up should be done.
Remember it's a team work comprising of hand surgeon, anaesthetist, physiotherapist and occupational therapist and the final results depend upon the performance of the team.
Ten indications for fixation in metacarpal and phalangeal fractures
Failure to achieve acceptable reduction.
Compound fractures.
Rotational deformity.
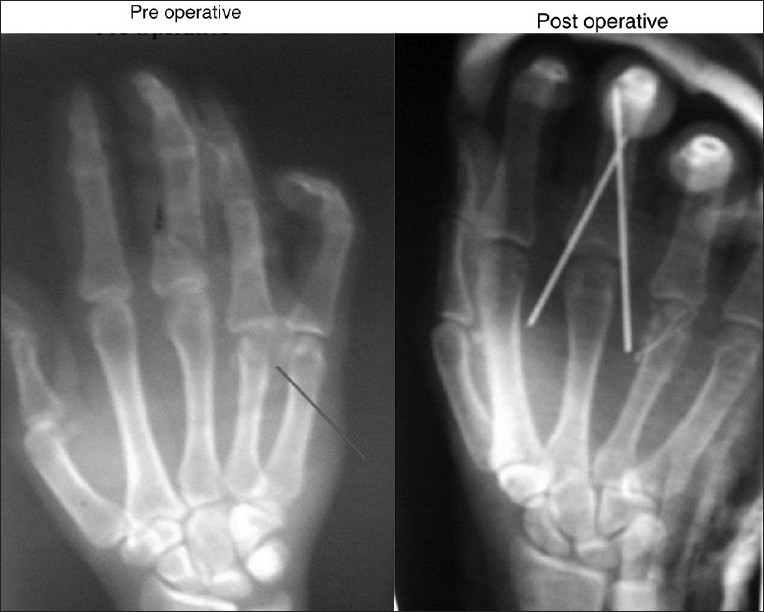
Multiple metacarpal/phalangeal fractures [Figure 1].
Intra-articular fractures.
Hand fractures associated with polytrauma.
Fractures associated with bone loss.
Phalangeal neck fractures.
Malunion / non union
Reimplantation.
Figure 1.

X-ray showing multiple fractures involving the shaft of the 4th metacarpal, basal intra articular fracture of the 5th metacarpal and open comminuted fracture of the proximal phalanx of the right little finger. ORIF is indicated in multiple fractures involving the hand. Note that the comminuted fracture of the shaft of the 4th metacarpal has been fixed with a bone tie and a neutralisation plate
Approaches and anaesthesia
Open reduction in closed fracture metacarpal is generally brought about by vertical incisions avoiding the extensor tendons, but if all the 4 metacarpals are fractured then the hand may be explored by 2 incisions one each for 2nd/ 3rd and 4th / 5th. First metacarpal is explored between EPL and EPB.
The phalangeal fracture is exposed either through a dorsal vertical[8] or a lazy ‘S’ incision. Rarely one may choose to go through one or both[9] mid lateral incision.[10] Extensor tendon on the proximal half of the proximal phalanx is incised vertically in the middle while in the distal half the plane is in between central and lateral slip. The incision over the extensor tendon on the middle phalanx is paramedian without violating the insertion of central slip at the base of middle phalanx. Though GA or regional anaesthesia are widely used in hand surgeries, there is a distinct advantage of distal blocks or WASH[11] which facilitates intraoperative movements of the fingers to confirm the rotational alignment.
TECHNIQUES OF FIXATION
K wire
These are versatile, easily available, cheap, surgeon friendly, forgiving implant which can be used either percutaneously [Figure 2] or by open methods.[12,13] It is available as smooth or threaded pins in different sizes with different tips (trocar tip and bayonet tip) for meta and diaphyseal areas. They can also be used as joysticks for reduction, drill bits for screws and pins for external fixator. They can also be used for provisional fixation. K wires can be passed by open or closed methods from one end (fragment) of the bone (proximal or distal) across the fracture site into the other end (distal or proximal)- called centripetal. [Figure 3] It can also be passed by either closed or open method through the fracture site first into (proximal or distal) and later after obtaining reduction into the other fragment(distal or proximal) called as centrifugal [Figure 4] method. These terminologies will avoid confusing terms like antegrade and retrodrade. The exact method of passage of K wire in terms of direction can be radioulnar, ulnoradial or central depending on the fracture anatomy wherein it is desirable to approach the fracture site by the K wire at an angle close to 90°. This approaching angle of the K wire should be preferably more than 45° in all the cases. Though any fracture configuration can be effectively managed with K wires with or without supplemental SS wire, K wires do have the limitations in terms of being non rigid, pin loosening, pin tract infection, tendon impalement and possible neurovascular injury.
Figure 2.

Multiple closed fractures of the phalangeal bones treated with CRIF using K wires
Figure 3.
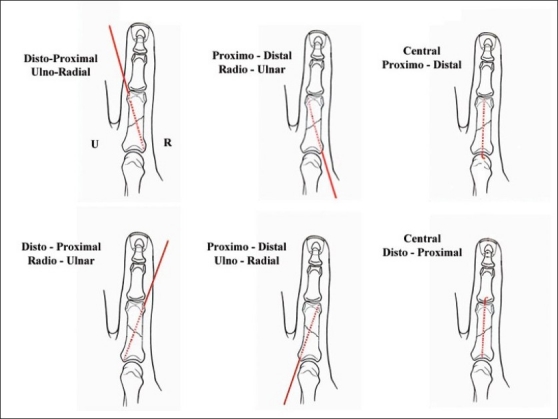
Short oblique fracture of the proximal phalanx of the index finger with six possible ways for centripetal placement of K wires
Figure 4.
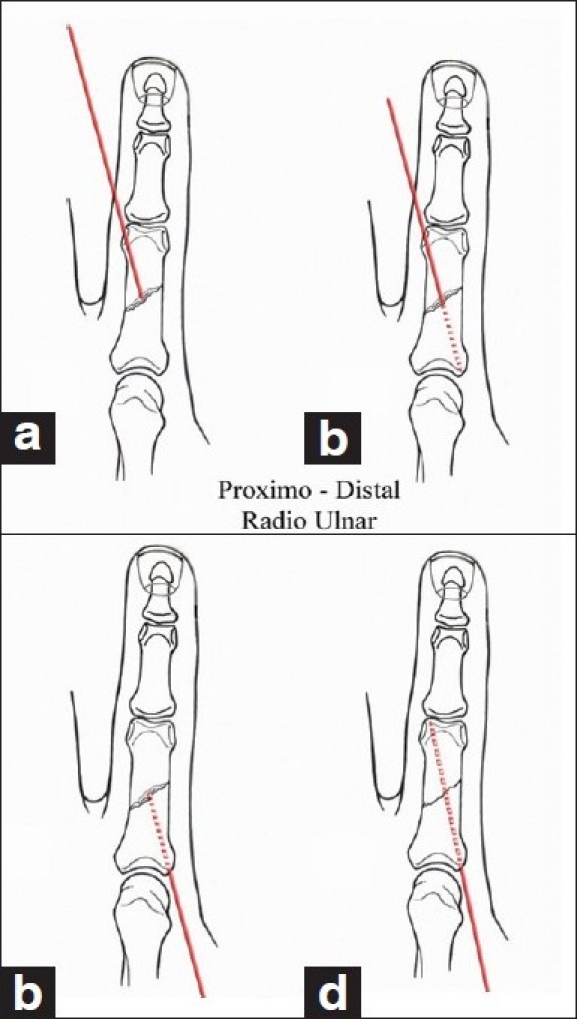
One of the methods of centrifugal placement of K wires wherein the K wire is first passed through the fracture site into the proximal fragment (a and b). After achieving reduction, the same K wire is driven back into the distal fragment (c and d).This placement is termed as centrifugal, proximo-distal, radio-ulnar.
Stainless steel interosseous wiring
This is a safe alternative for screw fixation for providing interfragmentary compression. It can be used 1)in isolation as in case of fracture neck of metacarpal or unicondylar fracture head or base of the phalanx 2) as a supplement for single or double K wires[14] 3) as a composite to provide tension band effect. SS wire can be used in different configurations such as circumferential[16] (encirclage), interosseous loop,[16] single or double. The latter itself could be parallel or perpendicular (90-90) configuration. SS wire can also be used along with bone tie to bring about interfragmentary compresssion with distinct biomechanical advantage.[17,18]
Intramedullary fixation[19]
Steinnman pin can be used as a peg to fix the metacarpal or phalangeal fractures to avoid protruding wires impaling the extensor tendons. This method is ideally suited for transverse fractures of the metacarpal and phalangeal shaft with the advantage of avoiding implant removal. The drawback is of course the rotatory instability which can be addressed by supplementary SS wire fixation.
Screws and plates
This method is technically demanding with little margin of error, but has a role in oblique unstable fracture of the metacarpal and phalanges. Based on the sound principle of AO,[20] rigid fixation is possible with minimum two screws[21] in long oblique fractures [Figure 5] of metacarpal and phalanges. Short oblique fractures of metacarpal and phalanges can be fixed using 4 or 5 holed plates (mini or micro plates).[22] Intra-articular fractures with metaphyseal extension may be fixed with condylar buttress plates.
Figure 5.

Spiral fracture of the shaft of the 4th metacarpal fixed with ORIF using two screws
External fixation
It has a definite role in compound fractures [Figure 6] and badly comminuted closed intra-articular fracture dislocations. Ideally a digit with skeletal injury should not be immobilised for more than three-four weeks to have an acceptable functional outcome. As the need for soft tissue replacement[23] is high in compound fracture of the hand, the external fixation used for skeletal stabilisation should not preclude local, regional or distant flap coverage. Dynamic spanning fixator which can achieve and maintain reduction and yet allow mobilisation makes it an ideal choice for pilon fracture of the base of the phalanges with or with out subluxation or dislocation.
Figure 6.

Open fracture of the neck of the proximal phalnx of right thumb fixed with bone tie and external fixator following repair of EPL tendon
METACARPAL FRACTURES
In the order of frequency and importance, the fracture of the metacarpal bone occurs in neck (mainly the 5th), shaft (2nd, 3rd and 4th), metacarpal base (mainly 1st) and finally in head.
Metacarpal neck fractures also called Boxers fracture are generally caused due to direct impact of the clenched fist on a solid object. Because of the compensatory movement of the basal joints, the acceptable dorsal angulations of neck fractures are 40, 30, 20 and 10° for the 5th, 4th, 3rd and 2nd respectively. Uncorrected dorsal angulation will lead to unsightly dorsal deformity, prominent metacarpal head on the palmar side, pseudo clawing and diminished flexor force at the MP joint.[24] Majority of the closed uncomplicated fracture metacarpal neck can be managed conservatively by obtaining acceptable reduction using Jahss manoeuvre,[25] where the small distal fragment is controlled and manipulated by flexing the MP joint, along with dorsally directed corrective force to obtain reduction. The reduction thus obtained can be maintained with dorsal slab or a splint immobilizing the wrist in extension and MP in flexion of 60 to 70°. The whole manoeuvre could be done under local block. If the displaced fracture is reducible but unstable, it may need percutaneous K wire fixation which can be closed intramedullary[26] or transosseous fashion.[27] Open fractures and closed irreducible fractures will need open reduction and fixation using K wire with or without SS wire or rarely mini condylar plates.[28]
Management of nonthumb metacarpal shaft fracture is dictated by the stability and personality of the fracture. Undisplaced fracture with any fracture configuration can be managed by conservative method with a slab or a splint immobilising the wrist in Extension and MP joint in flexion greater than 70° (Clam digger slab/cast),[29] allowing early IP mobilisation.
Closed unstable fracture of metacarpal bone should be subjected first for closed reduction and percutaneous K wire fixation where ever possible, with the help of image intensification. The border (2nd and 5th) metacarpal shaft fracture can also be treated with transosseous K wire fixation where the proximal and distal fracture fragments are independently fixed to the adjacent intact metacarpal bone transversely using 2 K wires on either side of the fracture following closed reduction. This method instead of impaling the extensor tendon may go through the substance of the interossei and hence should be undertaken with MP flexion. This fixation may still need external support for protection. Open fractures, irreducible fractures, multiple fractures will need open reduction and internal fixation with K wire with or without SS wire. Issues of 1) leaving the K wire percutaneously or 2) burying under the skin 3) passing the wire through the fracture site first proximally, 4) first distally or 5) passing the K wire antigrade from the base across the fracture site into the distal (Cent ripetal, proximal to distal) or 6) retrogradely first into distal fragment and than across the fracture site, into proximal fragment (Centrifugal, Disto-proximal) are debatable and subject to surgeon discretion. If the wire needs to be maintained for more than three to four weeks, it is better to bury the tip under the skin. It is preferable to spare the MP joint and the extensor hood by allowing the K wire jet out proximally around the carpus, for early and safe mobilisation of the MP joint.[30] Though these fractures can also be treated with plates and screws they may be preferred for highly unstable, segmental, severe fracture with skin, soft tissue and/or skeletal loss which need concomitant aggressive soft tissue replacement.[31]
Oblique fracture of the metacarpal shaft is divided into short or long oblique depending on the length of the fracture line. If it is more than twice the width of the bone at the centre of the fracture, such fractures are considered as long oblique. All displaced oblique (short or long) fractures are unstable and are difficult to manage by Close reduction and internal fixation (CRIF), while long oblique fracture can still be safely treated by composite wiring. They may also be treated with 2 screws (3rd screw optional) one perpendicular to the fracture site (compression screw) the other one (neutralisation screw) perpendicular to the bone. Fixation of any fracture with one screw alone is not acceptable, which is why in short oblique fractures a single screw may have to be supplemented with a neutralisation plate. The compression screw may, however, be passed through the middle hole of 5 holed plate if the obliquity of the fracture is in coronal plane. If the same is in saggital plane, then the compression screw should be outside the plate and introduced first before plate application. At least 2 screws in each of the proximal and distal fragment is ideal, which is why in metadiaphyseal fracture T, L or mini condyle plates are preferred.
Comminuted shaft fractures are dealt with rigid ORIF with any of the above-mentioned methods depending on the size of the comminuted fragment. Surgeon must not hesitate to do primary bone graft or bone graft substitutes if needed along with fixation, keeping in mind to place them on the opposite side of the plate for better and early incorporation.
Multiple metacarpal fractures closed or open suggest instability of skeleton of hand and needs more often Open reduction and internal fixation (ORIF). Opening the fracture site in closed multiple metacarpal fractures allows the surgeon to decompress the different compartments of the hand to prevent VIC of intrinsic muscles of the hand.
Metacarpal head fractures are very rare and like any other intra-articular fracture most often need ORIF unless undisplaced to begin with. The limiting factor for the surgeon is the size of the fragment, preserving blood supply of the fragment and the approach. Uncomminuted, 2 or 3 part fractures need ORIF using K wires, SS wire [Figure 7]/ headless screws and anatomical reconstruction. Small osteochondral fractures may be treated conservatively or delayed excision. Comminuted fractures of head generally need distraction non operatively or by external fixator. Since the blood supply generally comes from the collateral ligament, the fragments need careful handling to avoid avascular necrosis[32] especially if the fragment is distal to the attachment of the collateral ligament or if the split fracture is in coronal plane. The open reduction of the fracture head of metacarpal generally needs midline extensor splitting approach as it gives a wide exposure which can be later repaired anatomically.
Figure 7.
Open two part fracture of the 4th metacarpal head and fracture proximal phalanx of the middle finger fixed with SS wire and criss cross K wires respectively
Basal fractures of the metacarpal are very common in the thumb and the 5th ray. Basal fracture of the first metacarpal can be extra-articular(epi-basal), fracture dislocation(Bennet's) or comminuted intra articular (Rolando fracture).[33]
Epibasal fracture with angulation more than 20° needs closed reduction and thumb spica application.
Bennet's fracture dislocation is an intra articular basal fracture with a small volar fragment(Bennet's fragment) remaining undisplaced due to attachment of strong volar oblique ligament, while the larger distal fragment consisting of rest of the base of metacarpal pulled proximally and dorsally by the deforming pull of the APL tendon.[34] This injury is caused due to an axial load on the thumb with thumb in flexion.
The distal fragment is displaced proximally, adducted and supinated. With a special view of 15° pronation, oblique PA view with 15° disto-proximal inclination of the X rays, one can diagnose and estimate the size of the Bennet's fragment which will determine the management.[35] With the advent and wide use of C arm, most of the Bennet's fracture can be managed with CRIF, the manoeuvre of which should be axial traction, abduction ,pronation of distal fragment with corrective force over the dorsal apex angulation. Ideally 2 K wires, both across the fracture [Figure 8] or one across the fracture and the other across the carpometacarpal joint[36] or intermetacarpal (engaging first and the second) for a period of four-six weeks will generally suffice.[37] Sometimes if there is delayed presentation or the fragment involves >30 to 40% of the base of first metacarpal it may need ORIF.[37] Final result generally depends upon the degree of articular reconstruction brought about either by closed or open methods.
Figure 8.

Closed Bennet's fracture fixed with CRIF using two K wires across the fracture site
Fracture dislocation of the base of 5th metacarpal, also called reversed Bennet's fracture, is also potentially unstable injury because of the pull of the ECU tendon. These injuries also need CRIF or ORIF to avoid late degenerative changes in the 5th carpometacarpal joint.
Phalangeal fractures can involve the base, shaft, neck and the head.
Basal fractures of the phalangeal bone could be uni or bicondylar with or without communition. The management depends on the instability whether the fracture is closed or open and the size of the fragment. Closed stable small basal fracture can be treated by conservative methods using buddy splints or protective braces, while displaced uni or bicondylar basal fractures can be reasonably manipulated by closed methods and treated with nail traction over an aluminium Zimmer splint incorporated with a below elbow plaster. Percutaneous or open K wire or screws and plate generally adds morbidity and should be undertaken rarely and by experienced surgeons.
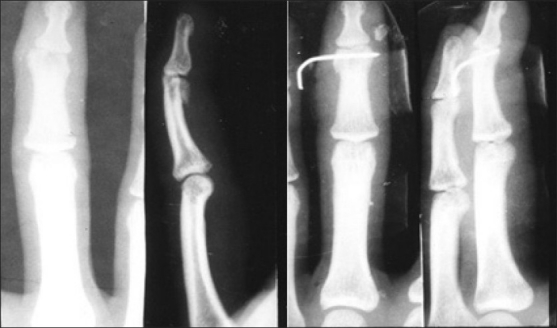
Management of diaphyseal fractures of the phalanges, like that of metacarpal depends on the plane of the fracture line. All stable undisplaced fractures can be treated by conservative methods. Transverse displaced fractures most often are amenable for acceptable closed reduction and splinting, nail traction[39] or percutaneous single or crisscross K wire fixation.
Irreducible and open fractures of the phalangeal shaft will need open reduction and fixation using K wire with or without SS wire. Though these fractures can be fixed with plate and screws, they are technically demanding and provide very little advantage over the conventional method of fixation. Moreover margin of error is very little and poorly executed plating in these fractures is unforgiving.
Oblique fractures short or long like the transverse fractures can be stabilised by conservative nail traction or percutaneous fixation. Unstable long oblique fractures of shaft of the phalynges often need ORIF with K wire (composite or supplementary wiring) or interfragmentary screw fixation(mini or micro plates when used are preferably placed on the lateral side avoiding the extensor tendons). K wires either single, double, crisscross used for fixation of the proximal phalangeal fractures should preferably avoid the PIP joint and extensor tendon around it.
Fracture neck of the phalynges are mainly seen in children and are notoriously missed for want of properly focussed X ray.[40] In addition to proper AP and lateral, an oblique view may be needed in subtly displaced fractures. The fracture itself may be classified into undisplaced, partialy displaced and completely displaced.[41] Generally this fracture will need ORIF in the form of K wire fixation. Undisplaced fracture when treated by conservative methods will need close follow up with check X rays.
Fracture head of the phalanx can be of 3 types, undisplaced, unstable unicondylar [Figure 9] and bicondylar or comminuted.[42] The unicondylar fracture itself could be of 4 types: oblique volar, long sagittal, dorsal coronal and volar coronal.[43] Hallmark of these injuries is that it can be easily missed unless true AP, lateral and oblique radiographs are carefully assessed. Most of these injuries including undisplaced fractures are unstable and will either need CRIF or ORIF with wires or screws.[43]
Figure 9.
Closed unstable unicondylar fractures of the head of the middle phalanx fixed with a closed transverse K wire following acceptable reduction
Fracture subluxation or dislocation of the PIP joint is more often on the dorsal side than on the volar side. Stability of the fracture dislocation depends mainly on the size of the volar basal fragment of the middle phalanx.[44] If the size is less than one third of the base of the middle phalanx, the injury can be generally managed by closed reduction and an extension blocking splint or pin for a period of three weeks. However if the fragment is larger than one third, such injuries need closed reduction and percutaneous fixation with K wires. Open reduction and fixation of the volar fragment to the rest of the base of the middle phalanx may occasionally be needed if closed reduction fails. In severe comminuted injuries, one may have to use dynamic external fixation as described by Suzuki[45] or one of its modifications.[46] Volar fracture subluxation or dislocation leading to button hole deformity is much less common and when encountered should be treated with CRIF or ORIF to maintain the articular congruity and hence the function.
Fracture terminal phalanges
These are extremely common and could be classified into tuft fracture, basal avulsion fracture involving the insertion of the terminal extensor tendon or FDP, transverse or longitudinal shaft fracture and epiphyseal injuries in children and adolescent age group.[47] While the tuft fractures are to be treated conservatively with proper wound care and repair of the pulp and the nail matrix, the displaced avulsion fracture of the base of the terminal phalanx needs open reduction and fixation. The unstable shaft fracture of the terminal phalanx needs axial K wire fixation. The epiphyseal injury of the terminal phalanx in children (Seymour's fracture[48]) may involve nail plate avulsion, nail matrix laceration which should be treated with manipulation, nail matrix repair under magnification and reposition of nail plate.
Bone grafting
Bony defect in metacarpal or phalanges fractures can be addressed either aggressively in primary stage with bone graft and flap coverage or composite flaps, or in the staged secondary procedures wherein the soft tissue defect is addressed in the first stage and bony defect is tackled in the second stage. In highly selected cases, there may be a role for Bone graft substitutes instead of autologous bone.
Primary arthrodesis, arthroplasties (primary or secondary) may have to be considered in certain unsalvageable intra articular injuries to optimise the results in certain selected patients whose occupation need either stability or mobility of the injured digit.
Bio-absorbable implants (wire, plates and screws) have not found acceptance universally as there are very little advantages over the conventional methods.
CONCLUSIONS
Hand fractures are equally or more worthy of expertise as major extremity trauma are, and the final outcome is a product of team work consisting of surgeon, anaesthetist, physiotherapist, occupational therapist and orthotist, amidst a highly motivated patient. The management of skeletal injuries of the hand is a fine balancing act between mobility and stability on one hand and stiffness and adhesions on the other, and the surgeon as the leader of the team should modulate within his limits to tilt the balance in favour of mobility.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Emmett JE, Breck LW. A review of analysis of 11,000 fractures seen in a private practice of orthopaedic surgery 1937-1956. J Bone Joint Surg Am. 1958;40:1169–75. [PubMed] [Google Scholar]
- 2.Lane CS. Detecting occult fractures of the metacarpal head: The Brewerton view. J Hand Surg. 1977;2:131–3. doi: 10.1016/s0363-5023(77)80098-1. [DOI] [PubMed] [Google Scholar]
- 3.Eyres KS, Allen TR. Skyline view of the metacarpal head in the assessment of human fight-bite injuries. J Hand Surg Br. 1993;18:43–4. doi: 10.1016/0266-7681(93)90194-k. [DOI] [PubMed] [Google Scholar]
- 4.Lane CS, Kennedy JF, Kuschner SH. The reverse oblique x-ray film: Metacarpal fractures revealed. J Hand Surg Am. 1992;17:504–6. doi: 10.1016/0363-5023(92)90362-s. [DOI] [PubMed] [Google Scholar]
- 5.Swanson AB. Fractures involving the digits of the hand. Orthop Clin North Am. 1970;1:261–74. [PubMed] [Google Scholar]
- 6.Venkataswami R. 1st ed. New Delhi, India: Jaypee Publishers; 2009. Surgery of the injured hand-towards functional restoration; p. 409. [Google Scholar]
- 7.Freeland AE. Philadelphia: Churchill Livingstone; 2000. Hand Fractures Repair,reconstruction and rehabilitation; pp. 7–8. [Google Scholar]
- 8.Pratt DR. Exposing fractures of the proximal phalanx of the finger longitudinally through the dorsal extensor apparatus. Clin Orthop. 1959;15:22–6. [PubMed] [Google Scholar]
- 9.Barton NJ. Fractures of the hand. J Bone Joint Surg Br. 1984;66:159–67. doi: 10.1302/0301-620X.66B2.6707048. [DOI] [PubMed] [Google Scholar]
- 10.Posner MA. Injuries to the hand and wrist in athletes. Orthop Clin North Am. 1977;8:593–618. [PubMed] [Google Scholar]
- 11.Lalonde D, Bell M, Benoit P, Sparkes G, Denkler K, Chang P. A multicentre prospective study of 3110 consecutive cases of elective epinephrine use in the fingers and hand: The Dalhousie Project clinical phase. J Hand Surg Am. 2005;30:1061–7. doi: 10.1016/j.jhsa.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Berkman EF, Miles GH. Internal fixation of metacarpal fractures exclusive of the thumb. J Bone Joint Surg. 1943;25:816–21. [Google Scholar]
- 13.Waugh RL, Ferrazzano GP. Fractures of the metacarpals exclusive of the thumb: A new method of treatment. Am J Surg. 1943;59:186–94. [Google Scholar]
- 14.Gould WL, Belsole RJ, Skelton WH., Jr Tension-band stabilization of transverse fractures: An experimental analysis. Plast Reconstr Surg. 1984;73:111–5. doi: 10.1097/00006534-198401000-00027. [DOI] [PubMed] [Google Scholar]
- 15.Gropper PT, Bowen V. Cerclage wiring of metacarpal fractures. Clin Orthop. 1984;188:203–7. [PubMed] [Google Scholar]
- 16.Gingrass RP, Fehring B, Matloub H. Intraosseous wiring of complex hand fractures. Plast Reconstr Surg. 1980;66:383–91. [PubMed] [Google Scholar]
- 17.Sammut D, Evans D. The Bone tie.A new device for interfragmentary fixation. J Hand Surg Br. 1999;1:64–9. doi: 10.1016/s0266-7681(99)90035-9. [DOI] [PubMed] [Google Scholar]
- 18.Kamath BJ, Bhardwaj P, Harshvardhan, Binoy PS, Agarwal T. In 2010 IFSSH - Hand Surgery. In: Chung MS, Baek GH, Gong HS, editors. First edition. Korea: Koon Ja Publishing Inc; 2010. pp. 372–3. [Google Scholar]
- 19.Grundberg AB. Intramedullary fixation for fractures of the hand. J Hand Surg Am. 1981;6:568–73. doi: 10.1016/s0363-5023(81)80134-7. [DOI] [PubMed] [Google Scholar]
- 20.Heim U, Pfeiffer KM. 2nd ed. New York: Springer-Verlag; 1982. Small Fragment Set Manual: Internal Fixation of Small Fractures. [Google Scholar]
- 21.Lee SG, Jupiter JB. Phalangeal and metacarpal fractures of the hand. Hand Clin. 2000;16:323–32. [PubMed] [Google Scholar]
- 22.Puckett CL, Welsh CF, Croll GH, Concannon MJ. Application of maxillofacial miniplating and microplating systems to the hand. Plast Reconstr Surg. 1993;92:699–707. [PubMed] [Google Scholar]
- 23.Hastings H., II . Open fractures and those with soft tissue damage:Treatment by external fixation. In: Barton NJ, editor. Fractures of the Hand and Wrist. Edinburgh: Churchill Livingstone; 1988. pp. 145–72. [Google Scholar]
- 24.Thurston AJ. Pivot osteotomy for the correction of malunion of metacarpal neck fractures. J Hand Surg Br. 1992;17:580–2. doi: 10.1016/s0266-7681(05)80247-5. [DOI] [PubMed] [Google Scholar]
- 25.Jahss SA. Fractures of the metacarpals: A new method of reduction and immobilization. J Bone Joint Surg. 1938;20:178–86. [Google Scholar]
- 26.Foucher G. “Bouquet” osteosynthesis in metacarpal neck fractures: A series of 66 patients. J Hand Surg Am. 1995;20:S86–90. doi: 10.1016/s0363-5023(95)80176-6. [DOI] [PubMed] [Google Scholar]
- 27.Waugh RL, Ferrazzano GP. Fractures of the metacarpals exclusive of the thumb: A new method of treatment. Am J Surg. 1943;59:186–94. [Google Scholar]
- 28.Buchler U, Fischer T. Use of a minicondylar plate for metacarpal and phalangeal periarticular injuries. Clin Orthop. 1987;214:53–88. [PubMed] [Google Scholar]
- 29.Wilson RL, Carter MS. Management of hand fractures. In: Hunter JM, Schneider LH, Mackin EJ, Callahan AD, editors. Rehabilitation of the Hand. CV Mosby: St. Louis; 1978. pp. 180–94. [Google Scholar]
- 30.Flatt AE. 3rd ed. St. Louis: CV Mosby; 1972. Fractures: The Care of Minor Hand Injuries. [Google Scholar]
- 31.Simonetta C. The use of “A.O.” plates in the hand. Hand. 1970;2:43–5. doi: 10.1016/0072-968x(70)90034-3. [DOI] [PubMed] [Google Scholar]
- 32.Kumar VP, Satku K. Surgical management of osteochondral fractures of the phalanges and metacarpals: A surgical technique. J Hand Surg Am. 1995;20:1028–31. doi: 10.1016/S0363-5023(05)80154-6. [DOI] [PubMed] [Google Scholar]
- 33.Rolando S. Fracture de la base du premier metacarpien et principalement sur une variété non encore decreite. Presse Med. 1910;33:303. [Google Scholar]
- 34.Imaeda T, An KN, Cooney WP, Linscheid RL. Anatomy of trapeziometacarpal ligaments. J Hand Surg Am. 1993;18:226–31. doi: 10.1016/0363-5023(93)90352-4. [DOI] [PubMed] [Google Scholar]
- 35.Billing L, Gedda KO. Roentgen examination of Bennett's fracture. Acta Radiol. 1952;38:471–6. doi: 10.3109/00016925209177031. [DOI] [PubMed] [Google Scholar]
- 36.Salgeback S, Eiken O, Carsam N, Ohlsson N. A study of Bennett's fracture. Scand J Plast Reconstr Surg. 1971;5:142–8. doi: 10.3109/02844317109042955. [DOI] [PubMed] [Google Scholar]
- 37.van Niekerk JL, Ouwens R. Fractures of the base of the first metacarpal bone: Results of surgical treatment. Injury. 1989;20:359–62. doi: 10.1016/0020-1383(89)90014-4. [DOI] [PubMed] [Google Scholar]
- 38.Chabon SJ, Siegel DB. Use of the Herbert bone screw compression jig to reduce and stabilize a Bennett fracture. Orthop Rev. 1993;22:97–9. [PubMed] [Google Scholar]
- 39.Moberg E. The use of traction treatment for fractures of phalanges and metacarpals. Acta Chir Scand. 1949;99:341–52. [Google Scholar]
- 40.Kilbourne BC, Paul EG. The use of small bone screws in the treatment of metacarpal, metatarsal, and phalangeal fracture. J Bone Joint Surg Am. 1958;40:375–83. [PubMed] [Google Scholar]
- 41.Al-Qattan MM. Phalangeal neck fractures in children: Classification and outcome in 66 cases. J Hand Surg Br. 2001;26:112–21. doi: 10.1054/jhsb.2000.0506. [DOI] [PubMed] [Google Scholar]
- 42.London PS. Sprains and fractures involving the interphalangeal joints. Hand. 1971;3:155–8. doi: 10.1016/0072-968x(71)90035-0. [DOI] [PubMed] [Google Scholar]
- 43.Weiss AP, Hastings II., H Distal unicondylar fractures of the proximal phalanx. J Hand Surg Am. 1993;18:594–9. doi: 10.1016/0363-5023(93)90297-G. [DOI] [PubMed] [Google Scholar]
- 44.Freeland AE. Philadelphia: Churchill Livingstone; 2000. Hand Fractures Repair, reconstruction and rehabilitation; p. 106. [Google Scholar]
- 45.Inanami H, Ninomiya S, Okutsu I, Tarui T. Dynamic external finger fixator for fracture dislocation of the proximal inter-phalangeal joint. J Hand Surg Am. 1993;18:160–4. doi: 10.1016/0363-5023(93)90265-5. [DOI] [PubMed] [Google Scholar]
- 46.Suzuki Y, Matsunaga T, Sato S, Yokoi T. The pins and rubbers traction system for treatment of comminuted intraarticular fractures and fracture-dislocations in the hand. J Hand Surg Br. 1994;19:98–107. doi: 10.1016/0266-7681(94)90059-0. [DOI] [PubMed] [Google Scholar]
- 47.Schneider LH. Fractures of the distal phalanx. Hand Clin. 1988;4:537–47. [PubMed] [Google Scholar]
- 48.Seymour N. Juxta-epiphyseal fracture of the terminal phalanx of the finger. J Bone Joint Surg Br. 1966;48:347–9. [PubMed] [Google Scholar]


