Abstract
The diagnosis and treatment of the acute compartment syndrome is of paramount importance. Unless the viscious cycle is intervened at an appropriately early time it will result in irreversible damage leading to disability. In this review article we are discussing the basic pathophysiological process through which the various aetiological factors causing increased compartmental pressure lead to the progressive death of muscles and nerves. We also discuss the various clinical features that aid in the diagnosis and the role of intracompartmental pressure measurements. Finally we hope to ascertain the basic principles and the surgical techniques for treating this condition effectively.
Keywords: Acute compartment syndrome, fasciotomy of forearm and hand, intracompartmental pressure measurement
INTRODUCTION
Acute compartment syndrome results from high tissue fluid pressure in a closed osseofascial compartment like the forearm that leads to reduced capillary perfusion below the level necessary for tissue viability.
HISTORICAL REVIEW
Richard von Volkmann[1] in 1881 published an article in which he described the conditions of irreversible contractures of the flexor muscles of the hand because of ischemic processes occurring in the forearm. Hildebrand (1906) was the first to suggest that elevated tissue pressure may be related to ischemic contracture. In 1906, Bardenheuer suggested that surgical decompression (fasciotomy) of the forearm fascia might be a method of treatment.
PATHOPHYSIOLOGY
Compartment syndrome is defined as a symptom complex resulting from increased tissue pressure within a limited space that compromises the circulation and function of the contents of that space. This occurs when intramuscular pressure is elevated to a level and for a period of time sufficient to reduce capillary perfusion.[2]
Rowland described the arteriovenous (AV) gradient theory that has been supported by Matsen. The relationship between the local blood flow (LBF) and the AV gradient can be expressed by the following equation:
LBF = (Pa – Pv)/R.
The local blood flow (LBF) in a compartment equals the local arterial pressure (Pa) minus the local venous pressure (Pv) divided by the local vascular resistance.
The muscle component of the various compartments is the primary target of the pathological process; the nerves are the secondary targets.
Following sustained vascular compromise, the muscle undergoes necrosis, fibrosis, and contracture; associated nerve injury causes further muscle dysfunction, sensibility deficits, or chronic pain. The end result is a dysfunctional muscle compartment with local and distant manifestations that depend upon the compartment involved and the degree of muscle contracture and nerve dysfunction.[3,4]
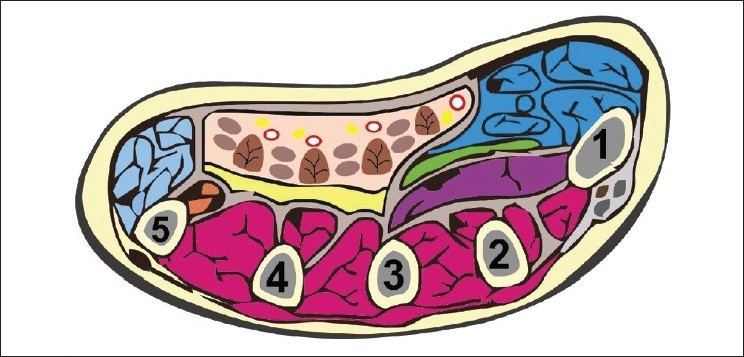
SEDDON'S ELLIPSOID INFARCT CONCEPT
Circulation in the middle of muscle belly is more affected and muscle degeneration occurs [Figure 1]. Muscles centered around anterior interosseous artery are mostly affected—FPL, FDP.
Figure 1.
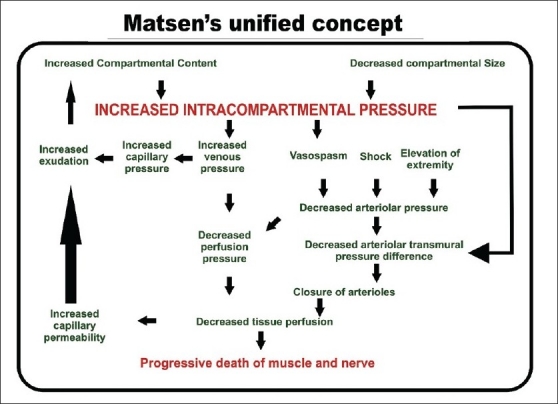
Matsen's unified concept
In the acute stage nerves are involved because of ischemia and in later stages due to entrapment in the fibrous tissue.
CRITICAL TIME LIMITS
Muscles retain the electrical response up to 3 h. They can tolerate ischemia up to 4 h and irreversible damage occurs at 8 h. Nerves can conduct impulses up to 1 h. They can survive up to 4 h (neuropraxia) and at 8 h irreversible damage occurs.
SURGICAL ANATOMY
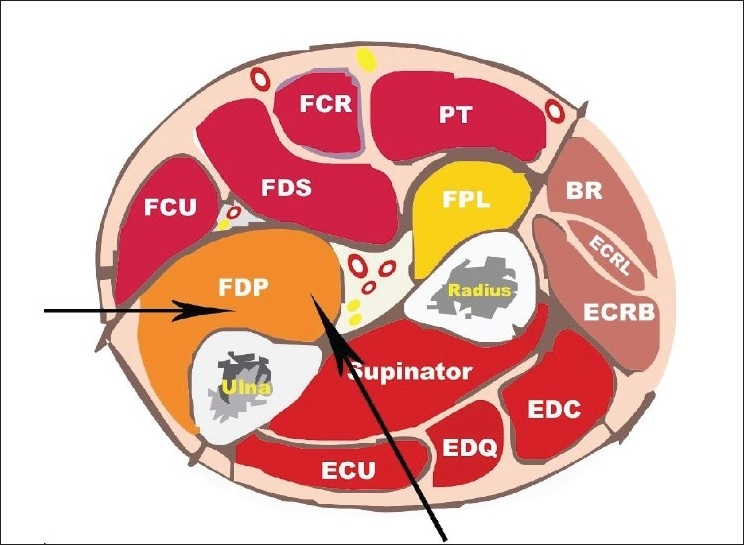
Forearm
The three forearm compartments are the flexor compartment containing the finger, thumb, and wrist flexors; the extensor compartment containing the finger, thumb, and ulnar wrist extensor (ECU) and the lateral compartment containing the mobile wad of Henry which is represented by the brachioradialis and the ECRL and ECRB [Figure 2].
Figure 2.
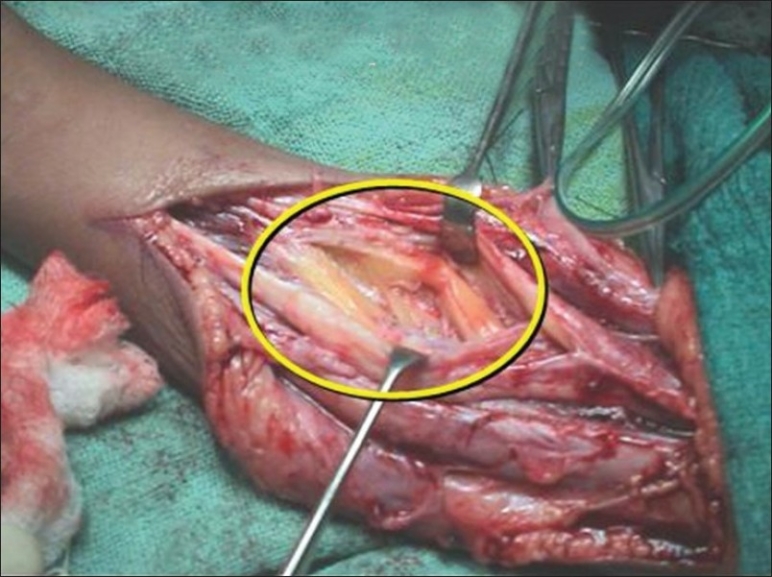
Ellipsoidal infarct in FDP
Hand
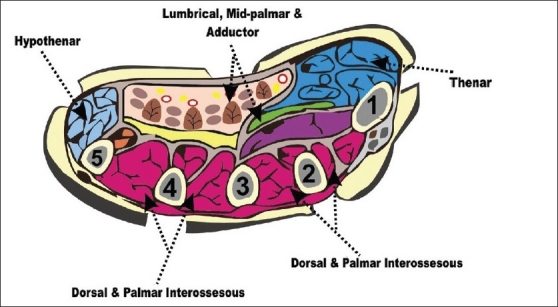
In the hand, there are 10 separate osteofascial compartments including dorsal interossei (4), Palmar interossei (3), Thenar and Hypothenar (2), and adductor pollicis (1) [Figure 3].
Figure 3.
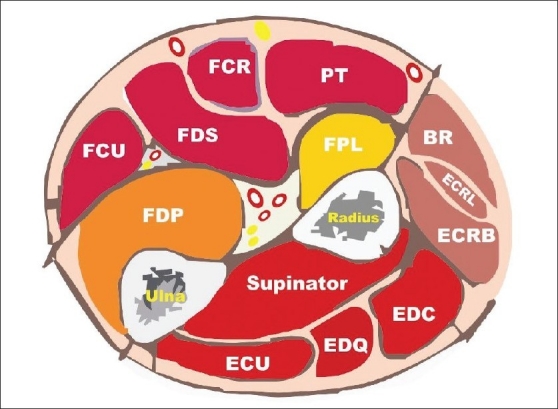
Schematic sectional anatomy of forearm
Etiology
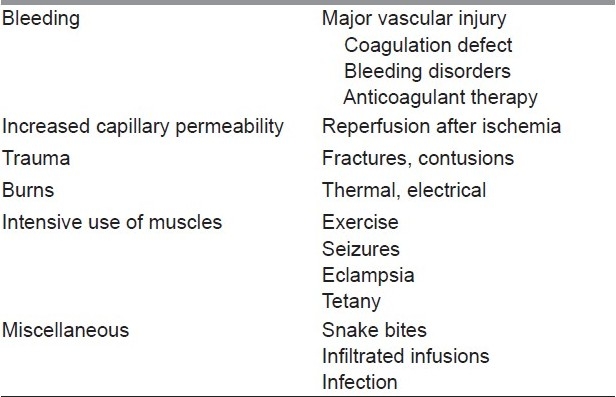
The compartment syndrome can occur either due to decreased compartment size or increased compartment contents. The causes of increased comprtments are given in Table 1. The decreased compartment size may be due to tight closure of fascial defects, excessive traction to fractured limbs, tight dressings, and plaster casts.
Table 1.
The causes of increased compartment contents
Clinical features
Acute compartment syndrome of the forearm
-
The diagnosis of forearm compartment syndrome is made by clinical findings, and may be confirmed by measurement of intracompartmental pressure.
- A swollen, tense, tender compartment with overlying skin that is often pink or red.
- Pain that may seem out of proportion to the injury especially with passive stretching of the fingers which is the pathognomonic sign.
- Sensory deficits or paresthesias.
- Paresis or paralysis (sensory changes usually occur before motor deficits).
- Radial and ulnar pulses are usually intact, since systolic arterial pressure (±120 mm Hg) exceeds the pressure within the involved compartment.
In children, anxiety associated with an increasing analgesic requirement is a very reliable indicator of compartment syndrome.
Acute compartment syndrome of the hand
The carpal tunnel, although not a true compartment, may act as a closed space, and the median nerve may be subjected to the adverse effects of increased pressure.[7]
The hand compartments that may be involved in compartment syndrome are the interossei (both dorsal and palmar), the thenar and hypothenar, the adductor, and the fingers.
The clinical findings in compartment syndrome in the hand are similar to the previously described findings in the forearm, and include pain in the region, pain with passive stretching of the involved muscles, localized swelling, paresthesia in the involved nerve distribution, and muscle paresis.
In the hand, all the intrinsic muscles may be evaluated by passively abducting and adducting the digits with the metacarpophalangeal (MCP) joints in extension and the proximal interphalangeal (PIP) joints in flexion.
The adductor compartment in the thumb is tested by positioning the thumb in palmar abduction to produce stretching of the adductor.
The thenar muscles are stretched by abduction and extension of the thumb, and the hypothenar muscles are stretched by abduction and extension of the little finger.
Swelling and increased tissue turgor may be noted over the individual involved compartments.
In the fingers, the amount of swelling and the nature of the injury—as well as the presence of a nonyielding burn eschar—may indicate increased pressure and the need for a fasciotomy.
Potential compartments are present in the finger due to the presence of fascial bands around the neurovascular bundles, including Grayson's and Cleland's ligaments.
Intracompartmental pressure measurements
Although the diagnosis of compartment syndrome may be made clinically, the measurement of the intracompartmental pressure is an additional diagnostic tool that may aid in confirmation of the diagnosis in unconscious patients and when the diagnosis is in doubt.[8]
Normal intracompartmental pressure is 0–8 mmHg and critical pressure is >30 mm Hg.
Methods of measurement
Infusion technique—Whitesides[9]
Intracompartmental pressure monitor systems—Stryker and Whitesides
Approaches for needle/catheter placement for measurement of compartment pressure
The starting point for both dorsal and ulnar approaches is at the junction of the proximal and middle third of the supinated forearm [Figure 4].[4]
Figure 4.
Schematic sectional anatomy of hand
-
(A)
The ulnar approach inserts the needle/catheter into the deep or profundus compartment using the ulna as a guide [Figure 5].
-
(B)
The dorsal approach [Figure 5] permits measurement of the dorsal compartment pressures, as well as the deep compartment depending on the depth of insertion
Figure 5.
Ulnar and dorsal approaches for measurement
Portals for compartment pressure measurements in the hand
-
(A)
Interosseous compartment pressures may be measured through these four portals on the dorsum of the hand [Figure 6a].
-
(B)
The thenar (T), midpalmar (MP), and hypothenar (H) compartments may be measured through these portals [Figure 6b].
Figure 6.
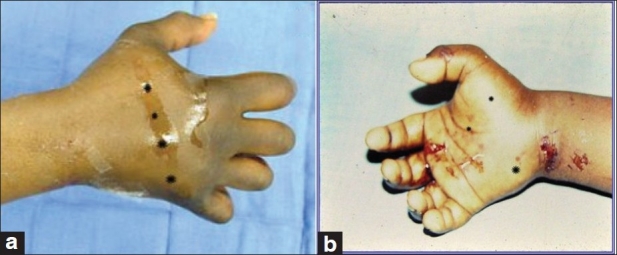
Portals for measurement of intracompartmental pressure of hand compartments on the dorsal (a) and palmar (b) sides
Noninvasive methods
-
Ultrasonic device
Measures submicrometric displacement of fascia caused by volume expansion.
-
Near-Infrared Spectroscopy (NIRS)
Tracking of variations in the oxygenation of muscle tissue.
Laser Doppler Flowmetry
Flexible fibre optic wire is introduced into the muscle compartment and signals from this wire are recorded on a computer.
TREATMENT OF ACUTE COMPARTMENT SYNDROMES
Forearm compartment syndrome
The goals of treatment are to restore microcirculation to the compartment through decompression.
Nonsurgical treatment
This includes splitting or removing a tight cast.
Ensure patient is normotensive, as hypotension reduces prefusion pressure and facilitates further tissue injury.
Maintain the limb at the level of the heart as elevation reduces the arterial inflow and the arteriovenous pressure gradient on which perfusion depends.
Maintain perfusion pressure = 20 mmHg, Arterial pressure (30–35 mmHg); venous pressure (10–15 mmHg).
Supplemental oxygen administration.
Role of hyperbaric oxygen therapy: Hyperbaric oxygen may be useful in helping the revitalization of the involved muscles, but only in borderline cases and only after fasciotomies have been performed. However, still this is in the experimental stage. Strauss has stated that muscle necrosis and edema formation are reduced following immediate treatment with hyperbaric oxygen.
But all these maneuvers have got a limited role. Whenever compartment syndrome is suspected, immediate operative decompression is performed.
Decompression is typically achieved by extensive fasciotomy. There is no role for limited fasciotomy.
Surgical treatment
Indications for fasciotomy
Unequivocal clinical findings
Pressure within 15–20 mmHg of DBP
Rising tissue pressure
Significant tissue injury or high-risk patient
6 h of total limb ischemia[12]
Injury at high risk of compartment syndrome
Contraindication
Delayed cases>24 h because of the risk of septicemia and death.[12]
Forearm fasciotomy: Surgical steps
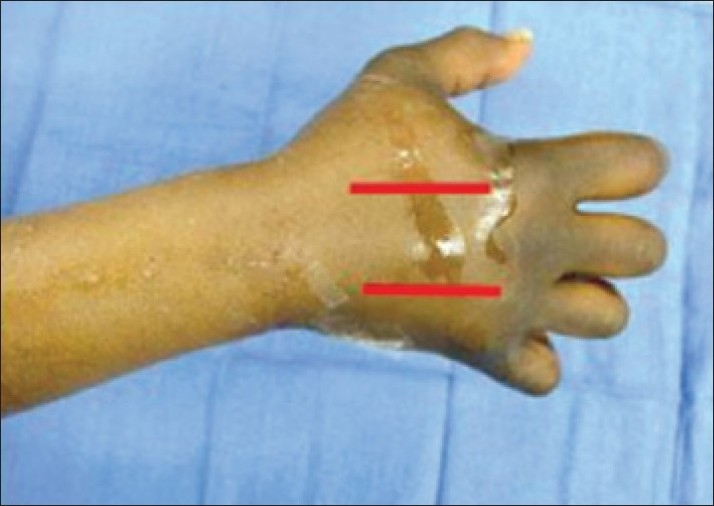
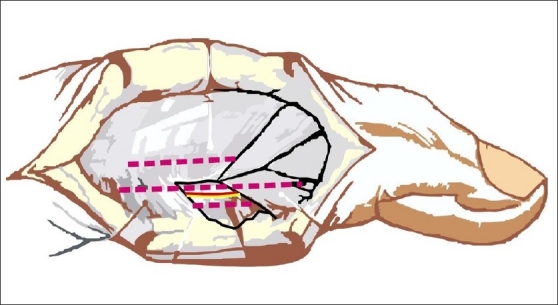
The forearm compartments (involving the forearm flexor compartment and the mobile wad compartment) are decompressed by a comprehensive incision from the distal arm to the midpalm [Figures 7–9].
Preserve cutaneous nerves and as many veins as possible.
Skin flaps created for coverage of median and ulnar nerves.
-
The deep fascia is incised from the region of the distal arm to, and including, the carpal canal.
- The underlying flexor muscles will often bulge dramatically into the wound.
- Check to see if its overlying fascia or epimysium is tight, and incise it longitudinally.
Epimysiotomy of individual muscle bellies is done if muscles look pale and tense after fasciotomy.[13]
The median nerve is at risk at four locations: the lacertusfibrosus, the pronator teres, the deep fascial arcade of the flexor digitorum superficialis, and the carpal tunnel.
If preoperative findings indicate that the ulnar nerve is involved, it is also decompressed as indicated at the cubital tunnel, forearm, and Guyon's canal at the wrist and hand.
If signs of radial nerve dysfunction are present, decompression of the radial tunnel may also be indicated.
In any acute compartment syndrome due to trauma, after relieving the pressure of the compartment, one must look for a direct injury to vessels and nerves inside and/or outside of the compartment; if these exist, repair should be done at this first operation.
Coexisting forearm fractures are usually stabilized operatively at the time of fasciotomy.
Skin incisions are left open to accommodate swelling, but are loosely reapproximated to cover the nerves.
If fractures are open and contaminated, fasciotomy is performed, wounds debrided, and fractures stabilized.
In contaminated wounds, external fixation or limited internal fixation may be preferable to standard internal fixation methods.
Skin grafting and limited secondary closure is performed when wounds demonstrate clean granulation tissue.
If closure is not possible within 5 days, a split-thickness skin graft should be applied. Alternatively, closure of fasciotomy wounds can be accomplished gradually with progressive tension using vessel loops (Shoe lace technique).[14] The vessel loops are tightened progressively postoperatively during dressing changes. Wound closure by this method usually can be accomplished in 2 weeks.
Figure 7.

A case of compartment syndrome due to electrical burns
Figure 9.

Incision for release of the volar forearm compartment syndrome. Note that the incision includes the distal arm and should include the carpal tunnel
Figure 8.

The same patient after extensive decompression
Release of extensor forearm compartment
Compartment syndromes involving the forearm extensor compartment are released through a dorsal incision.
When both the flexor and extensor compartments are involved, it is preferable to release the flexor compartment first; the relaxation afforded by the skin and fascia often decompresses the dorsal compartments.
Dorsal compartment pressures are used to determine whether or not to release the extensor compartment.
If required, it is released through a longitudinal incision 2 cm lateral and distal to the lateral epicondyle. The incision is continued distally to the myotendinous junction of the extensor muscles in the midforearm.
Fasciotomy is also indicated at the time of limb revascularization if the duration of ischemia has been as much as 4–6 h.
Postrevascularization edema may precipitate compartment syndrome, and prophylactic fasciotomy is indicated.
Hand compartment syndrome
The principles of treatment of hand compartment syndromes [Figure 10] are similar to those of the forearm. Figures 11 and 12 show incisions for decompression of various compartments of the hand. The deeper dissection for decompression of the hand compartments is done as follows:
Figure 10.

An example of compartment syndrome of hand
Figure 11.
Incisions for decompression of the interossei compartments
Figure 12.
Approaches to decompress hand compartments
Release of swollen fingers may be required based on the amount of swelling and the nature of the skin envelope [Figure 13].
If a significant burn eschar or swelling is present, digital fasciotomies are performed through midlateral incisions on the nondominant or noncontact side of the digits. The incisions are dorsal to the neurovascular bundles; Cleland's and Grayson's ligaments are incised. The dissection usually ends at the flexor sheath.
The incision is centered over the PIP joint and may extend 2 cm proximal and 2 cm distal to the PIP joint [Figure 13].
Figure 13.
Incision for decompression of digits
CONCLUSIONS
The prognosis depends on the intensity and duration of the elevated compartment pressure. Therefore, time is of the essence in the management of compartment syndrome. If clinical findings and/or pressure readings are suggestive, but not conclusive, remember that the scar from a fasciotomy incision is of relatively minimal consequence compared to an untreated compartment syndrome that results in a Volkmann's ischemic contracture. Therefore, whenever in doubt, fasciotomy should be done.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Volkmann R. Die ischaemischen Muskellahmungen and Kontrakturen. Zentralbl Chir. 1881;8:801–3. [Google Scholar]
- 2.Hargens AR, Mubarak SJ, Akeson WH. Current concepts in the pathophysiology, evaluation and diagnosis of compartment syndrome. Hand Clin. 1998;14:371–83. [PubMed] [Google Scholar]
- 3.Matsen FA, 3rd, Winquist RA, Krugmire RB., Jr Diagnosis and management of compartmental syndromes. J Bone Joint Surg Am. 1980;62:286–91. [PubMed] [Google Scholar]
- 4.Doyle JR. Compartment syndrome. In: Doyle JR, editor. Hand and Wrist. 1st ed. Philadelphia: Lippincott Williams &Wilkins; 2006. [Google Scholar]
- 5.Green DP, Hotchkiss RN, Pederson WC, Wolfe SW, editors. Operative Hand Surgery. 5th ed. New York: Elsevier, Churchill Livingstone; 2008. Ayan Gulgonen: Compartment syndrome. [Google Scholar]
- 6.Jobe MT. Compartment syndromes and Volkmann contracture. In: Canale, Beaty, editors. Campbell's Operative Orthopaedics. 11th ed. Philadelphia, PA: Mosby, Elsevier; 2008. pp. 4259–66. [Google Scholar]
- 7.Dresing K, Peterson T, Schmit-Neuerburg KP. Compartment pressure in the carpal tunnel in distal fractures of the radius.A prospective study. Arch Orthop Trauma Surg. 1994;113:285–9. doi: 10.1007/BF00443819. [DOI] [PubMed] [Google Scholar]
- 8.Gelberman RH, Garfin SR, Hergenroeder PT, Mubarak SJ, Menon J. Compartment syndromes of the forearm: diagnosis and treatment. Clin Orthop. 1981;161:252–61. [PubMed] [Google Scholar]
- 9.Whitesides TE, Jr, Haney TC, Harada H, Holmes HE, Morimoto K. A simple method for tissue pressure determination. Arch Surg. 1975;110:1311–3. doi: 10.1001/archsurg.1975.01360170051006. [DOI] [PubMed] [Google Scholar]
- 10.Mubarak SJ, Hargens AR. Acute compartment syndromes. Surg clin north Am. 1983;63:539–65. doi: 10.1016/s0039-6109(16)43030-6. [DOI] [PubMed] [Google Scholar]
- 11.Matsen FA, 3rd, Mubarak SJ, Rorabeck CH. Instructional Course Lectures The American Academy of Orthopaedic Surgeons. Vol. 32. St Louis Missouri: CV Mosby; 1983. A practical approach to compartment syndromes; pp. 88–113. [Google Scholar]
- 12.Lagerstrom CF, Reed RL, 2nd, Rowlands BJ, Fischer RP. Early fasciotomy for acute clinically evident posttraumatic compartment syndrome. Am J Surg. 1989;158:36–9. doi: 10.1016/0002-9610(89)90312-7. [DOI] [PubMed] [Google Scholar]
- 13.Eaton RG, Green WT. Epimysiotomy and fasciotomy in the treatment of Volkmann's ischemic contracture. Orthop Clin North Am. 1972;3:175–85. [PubMed] [Google Scholar]
- 14.Asgari MM, Spinelli HM. The vessel loop shoelace technique for closure of fasciotomy wounds. Ann Plast Surg. 2000;44:225–9. doi: 10.1097/00000637-200044020-00017. [DOI] [PubMed] [Google Scholar]


