Abstract
Fingertip amputations are one of the most common injuries faced in an emergency department. Finger tip replantation though technically possible, are not regularly done due to the presumed complexity of the procedure and doubts about the outcome. This article deals with our experience of 24 fingertip replantations in 24 patients done over a period of 8 years since the year 2000. Twenty-one fingertips survived. The most common affected digit in the series was thumb followed by index, middle, and ring. The overall success rate was 87%. Both arterial and venous repair were done in all cases. Replantation was not done if no suitable vein was found for anastomosis. Nine patients did not have nerve repair. Seven of them survived and all of them had satisfactory sensation when examined after 1 year. No patient suffered from cold intolerance. All patients were satisfied with the functional outcome and aesthetic appearance. This article highlights the technical considerations and the outcome of these fingertip replants.
KEY WORDS: Distal replantation, finger tip replantation, tip amputations, technical considerations
INTRODUCTION
Fingertip injuries and amputations are common injuries encountered in the emergency department of any major hospital. In upper limb amputations, fingertip amputations are more frequent than proximal amputations. Treatment options range from conservative management, local flaps to replantation of the amputated part. Replantation of the fingertip when successful provides excellent cosmetic outcome by maintaining the digital length, preserving the nail and improving function. It can provide a high degree of patient satisfaction. Although replantation of fingertip is technically possible, they are not regularly done due to the presumed complexity of the procedure and doubts about the outcome.
The aim of this article is to discuss anatomical features, technical considerations of the procedure, and analyze the outcome of 24 fingertip replantations.
The fingertip is defined as the part of the digit distal to the insertion of the flexor and extensor tendons into the distal phalanx. Fingertip amputations have been classified by many authors. Tamai's[1] original classification remains clinically useful due to its simplicity and practicality. Newer classifications have been created to support decision making at each level.
CLASSIFICATIONS BASED ON THE LEVEL OF AMPUTATION
Tamai classification
This classification[1] is the most frequently used system. He classified fingertip amputations into two zones.
Zone I: Distal to lunula.
Zone II: Distal interphalangeal (DIP) Joint to lunula.
Hirase classification[2]
This divides the fingertip into three zones, with the zone II being subdivided into II A and II B, [Figure 1a].
Figure 1.
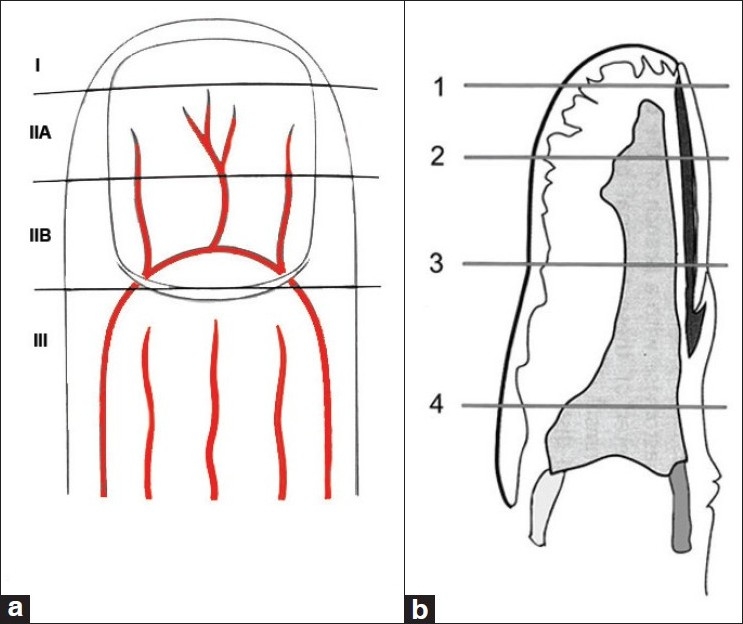
(a) Level of Amputation –Hirase’ classification. (b) Level of Amputation Allen's classification
Zone I: Distal to digital artery termination.
Zone II A: Distal to the terminal division of central artery.
Zone II B: nail fold to the distal terminal branches of artery.
Zone III: DIP joint to the nail fold.
Allen's classification[3]
Zone I: The amputated part does not include any bone fragment. No suitable vessel for anastomosis is available. In young children, the amputated part could be replaced as a composite graft.
Zone II: Amputation goes through the nail bed, preserving at least one-half of the nail bed and sterile matrix. No dorsal vein is available at this level. Venous drainage of the replanted part is achieved by repair of a palmar vein or by controlled bleeding (ie, heparinized saline or leeches).
Zone III: Similar to zone II, because the remaining nail bed is shorter, a hooked nail deformity is likely to occur if replantation fails.
Zone IV: Proximal to nail fold, a dorsal vein usually can be dissected and repaired to ensure venous drainage of the replanted part [Figure 1b].
Classification based on the nature of amputation
Yamano has classified fingertip amputation by mechanism and severity.[4]
Guillotine: A clean cut amputation (eg, knife).
Crush: Moderately crushed amputation (eg, saw).
Crush avulsion: severe crush and/or avulsion injury (eg, machine press or door).
Arterial anatomy
Knowledge of vascular anatomy of the fingertip is essential before attempting replantation. The diameter of the vessels and the wall thickness decrease as we proceed distally but the vessels are much larger than one might imagine and are easily found under magnification. It is the thinness of the vessel wall that poses the challenge than the size of the vessels in fingertip replantation. The two palmar digital arteries join in the midline at the level of lunula to form the pulp arcade [Figure 2a]. This arcade gives multiple branches adjacent to the periosteum. The central artery is usually the largest and is fit for end-to-end anastomosis. The diameter of these branches ranges from 0.3–0.7 mm.[5] There is significant tortuosity seen in the course of these arteries, which is useful for the gaining extra length after dissecting. Too much dissection should be avoided to prevent spasm.
Figure 2.
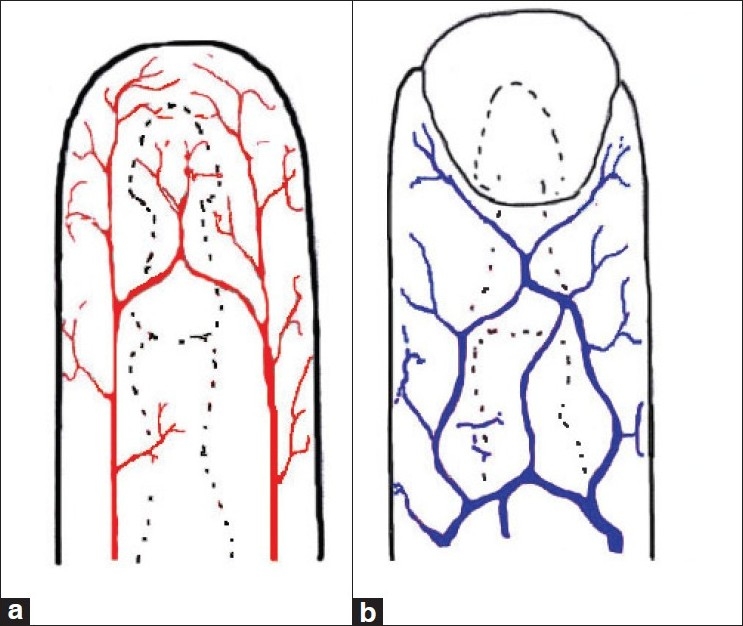
(a) Arterial anatomy at the fingertip. (b) Dorsal venous anatomy at the fingertip
Venous anatomy
The superficial dorsal veins are the main channels for venous drainage from the fingertip [Figure 2b]. The venules commence at the sides of the fingernail and converge proximal to the nail bed, forming a central vein. The vein divides into two or three branches after passing 2 to 4 mm proximally. These branches converge again after passing over the distal interphalangeal joint. The diameter of the dorsal veins in this region ranges from 0.4 to 0.7 mm. Veins on the lateral sides of the distal finger segment are 0.2 mm in diameter, which render them unsuitable for anastomosis.
Veins on the palmar aspect of the finger begin as a network at the fingertip and converge into 1 or 3 venules at the base of the distal phalanx. The largest vein, with a diameter of between 0.4 and 0.6 mm runs proximally along the midline subcutaneously. Two lateral veins with diameters between 0.3 and 0.5 mm run along the lateral side of the neurovascular bundles.
The various types of vein distribution at the dorsum of the distal finger segment are shown in Figure 3. Dorsal veins are selected for anastomosis in preference to the palmar veins, which are extremely delicate. At least 5 mm of skin beyond the nail fold is necessary to find a dorsal vein suitable for anastomosis. In amputations distal to that level, palmar veins have to be repaired.
Figure 3.
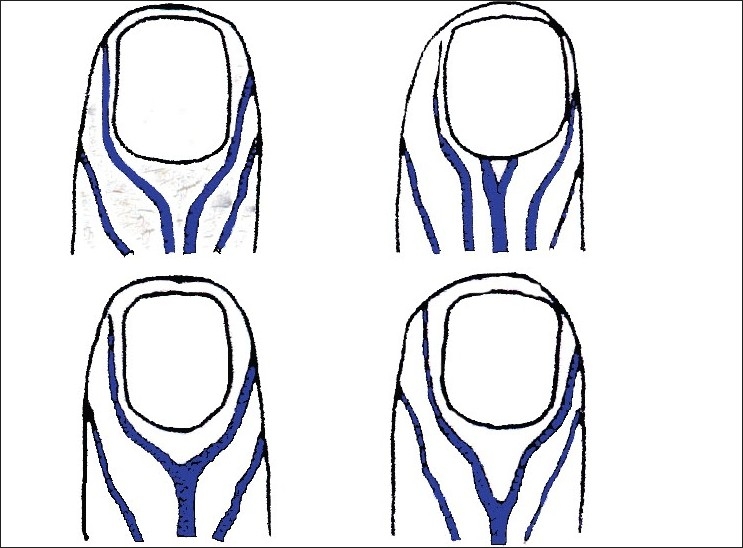
Patterns of dorsal venous anatomy
Operative technique
The patient after being received is fully evaluated for surgery. Replantation and other options of reconstruction are explained to the patient and relatives. Patient is taken up for surgery after obtaining the informed consent. The surgery is done under the brachial block. Our policy is to take the patient for surgery immediately on arrival to the hospital. There are many centers where fingertip replantations might be deferred to a more convenient time like the next morning, for logistical reasons. Although ischemia time is not as critical as for proximal amputations,[6] patient satisfaction is higher when the surgery is done on arrival. It also reinforces the message among the public that they need to rush to the microsurgery centre immediately after amputation of a digit.
Preparation of the amputated part
The amputated part is very small in zone I amputations and difficult to be held between the fingers of the assistant. There are two ways by which the part can be stabilized for this stage of the surgery. The surgeon can keep the amputated fingertip between the ring fingers of both the hands and use the thumb and index finger of the dominant hand to raise the flap while using the thumb and index of the other hand for holding the flap being dissected [Figure 4a]. In the other technique we have devised, a 4–0 prolene suture is passed through the nail plate and the part is fixed on to the plastic suture carrier.[7] The dissection and isolation of artery and vein is carried out under the microscope with the assistant holding the suture carrier [Figure 4b].
Figure 4.
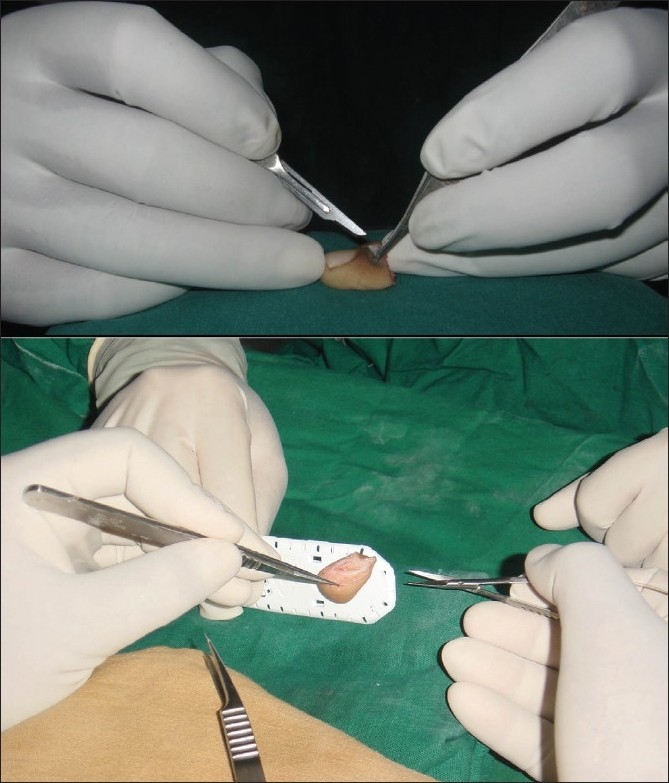
(a) Positioning the amputated part between ring fingers of both hands. (b) Positioning the amputated part on the suture carrier
Oblique full-thickness skin flaps as described by Tsai et al.[8] are raised on the palmar and dorsal aspects and sutured back with 5–0 prolene. The palmar veins are just under the subdermal level and so thin flaps have to be raised under the microscope. When the amputated part has not been completely exsanguinated by trauma, squeezing the pulp of the amputated part can fill the lumen of the artery and vein with blood, making visualization easier. This can be useful only once and therefore the part should be squeezed only under microscope by the surgeon and not earlier. If the veins are empty, they may not be clearly visible. The artery is usually located in the midline just above the periosteum. A small blood clot is usually present in the lumen of the artery when seen under magnification. To facilitate easy identification after skeletal fixation, the vessel ends are marked with 10–0 nylon suture taken through the adventitia of the vessel. This is preferred to applying microclamps as clamps can damage the intima if left on for prolonged periods.
Once the artery and veins are identified, the vessels are skeletonized by removing subcutaneous fat around them to provide adequate space for application of clamps and also to accommodate the postoperative edema. It is our practice to proceed with replantation only if we find suitable veins. Though success can be obtained without vein repair by established methods of blood drainage procedures, in our system of care patients do not like to undergo such salvage options for success.
Preparation of proximal side stump
This is easier and done under tourniquet. Similar full thickness skin flaps are raised to visualize the vessels. Usually the arterial end is found thrombosed and it is not freshened just before anastomosis. Dorsal veins are dissected out just above the extensor tendons and prepared for anastomosis. Nerve ends are identified and tagged.
Osteosynthesis
In Tamai zone I amputation where palmar veins are anastomosed, no K-wire technique[9] works well [Figure 5]. The distal part is stabilized by nail bed repair and simple skin sutures on the sides. When the entire nail bed is detached, as in avulsion amputations the nail bed is reinserted into the nail fold by horizontal mattress sutures. The deeper central artery is repaired first and skin is closed from dorsal to the palmar side and subcutaneous palmar vein is then anastomosed. In zone II amputations close to the DIP joint, if the joint is destroyed, then arthrodesis of DIP joint with single axial K-wire is carried out. Bone shortening also allows extra length of vessels for tension-free anastomosis. The flexor tendon need not be repaired when the joint is fused but its insertion into the volar plate should be retained for the better pinch strength. The K-wire is retained for 4–6 weeks, until the bone unites.
Figure 5.
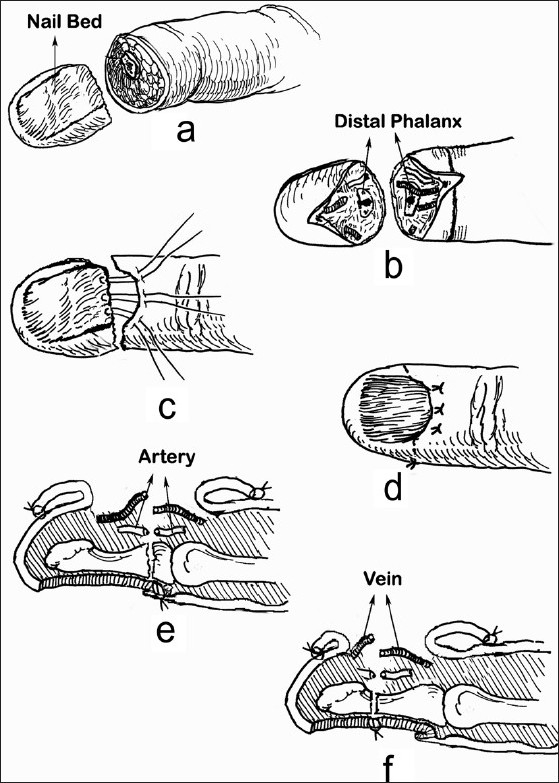
(a-e) Technique of attachment of distal part when the amputation is through the base of nail bed, using horizontal mattress, (f) When the amputation is through the more distal portions of the nail bed, nail bed is repaired with 5–0 chromic catgut interrupted sutures[19]
Artery repair
Artery repair in fingers is carried out with the hand supinated and pulp facing upwards. In the thumb, artery repair is particularly challenging because of difficulty in positioning of the hand. The forearm is fully pronated with the thumb pulp facing the ceiling and fingers held away by assistant. The surgeon sits at the head end of the patient to facilitate operator comfort during the anastomosis.
The large central artery is repaired using 10–0 nylon with 50 μm length needle. If turning of the clamp is not possible because of space constraints, the “one way up” technique is performed, wherein the posterior wall suturing is done first and repair continues to the anterior wall. Four or five sutures are usually adequate. Anastomosis should be carried out quickly as prolonged clamping of these thin-walled vessels could damage the intima and affect patency. In the case of tension at the anastomosis site, a vein graft, usually taken from volar aspect of wrist can be used to bridge the gap. If the digital nerve ends are easily approximated, they are repaired with 10–0 nylon suture.
Vein repair
In amputations at the zone II level, the dorsal veins were always available in our series and when available a minimum of two veins were anastomosed [Figures 6a,b]. In Zone I, after the arterial repair the clamps are released temporarily to identify the subdermal palmar vein. Once identified, the vessel clamp in the artery was reapplied and venous anastomosis carried out. Palmar vein anastomosis is carried out using the smallest available clamp, preferably a 1-V double clamp [Figure 6c]. If the clamp cannot be applied or is too big then open repair technique is followed, in which the two ends are brought close to each other and first the corner sutures are taken. Holding them the other sutures are put. The venous repair at this level is difficult because of the thinness of vessel wall. 11–0 suture with 50 μm needle is used. Irrigation of heparinized saline opens up the vessel lumen and facilitates the taking up of sutures. After the artery and vein repair, the clamps are released. The skin flaps are loosely approximated just to cover the anastomosis.
Figure 6.

(a) and (b) Dorsal vein repair (c) Palmar vein repair
Vein repair was always carried out in all cases. If suitable size vein is not found or it is impossible to repair, we do not proceed with replantation as we have never been successful if the venous anastomosis does not flow. Hattori et al.[10] have observed in their large published series that the failure rate is higher when veins are not repaired.
Postoperative care
The limb is kept immobilized in an above-elbow cast. This keeps the replanted part elevated, warm, and easy to inspect. The fingertip should look like the adjacent normal finger. Any change of color is an indication of an impending problem. Arterial insufficiency presents as a pale finger. Venous problems present as a bluish, congested finger. We do not re-explore a failing fingertip replant for logistical and financial reasons. Therefore, attention to detail is given during the first effort.
The patient is kept warm, well hydrated, and comfortable to avoid peripheral vasospasm.
All patients are maintained on intravenous antibiotics and a continuous daily infusion of a combination of 500 mL of Dextran 40 and 5000 units of Heparin for 5 days after replantation. This is followed by 75 mg of Aspirin for three weeks. The patient is discharged in 10 days.
The cast is retained for 2 weeks after which movements are started. The K-wire is removed at the fourth week, and then a finger splint is kept on for two more weeks. All patients are started on postoperative physiotherapy that involves massaging of the scar, sensory re-education and joint mobilization.
Representative case reports
Case number 12: a 12-year-old boy sustained a guillotine Tamai zone II amputation of the right middle finger and subtotal amputation of ring finger while trying to cut a coconut with a sickle. Two dorsal veins measuring 0.5 mm in diameter and the central artery were anastomosed. The DIP joint was arthrodesed using a longitudinal K-wire. At 2-year follow-up he had excellent cosmetic and functional result [Figure 7].
Case number 16: a 29-year-old gentleman sustained a clean cut Tamai zone I amputation of his left thumb when it got caught in a paper cutting machine. The part was fixed without K-wire by repairing the nail bed using the 6–0 chromic catgut. The artery repair was first carried out and the clamp was temporarily released to identify the veins and again reapplied. Two palmar veins were anastomosed using 11–0 nylon sutures after which the arterial clamp was released. At 1-year follow-up he had good sensation and 50° active flexion at the IP joint [Figure 8].
Case number 23: a 24-year-old male presented with total zone II amputation of thumb and index fingertips. The thumb was replanted and the index finger tip was covered with cross finger flap as suitable veins were not found. The sequence here was covering the index finger first followed by replantation of the thumb. At 2-year follow up, the thumb tip has 2 PD of 5 mm and index finger tip has good contour [Figure 9].
Figure 7.

Case no. 12, Zone II middle finger replantation
Figure 8.

Case no 16, Zone 1 thumb replantation
Figure 9.
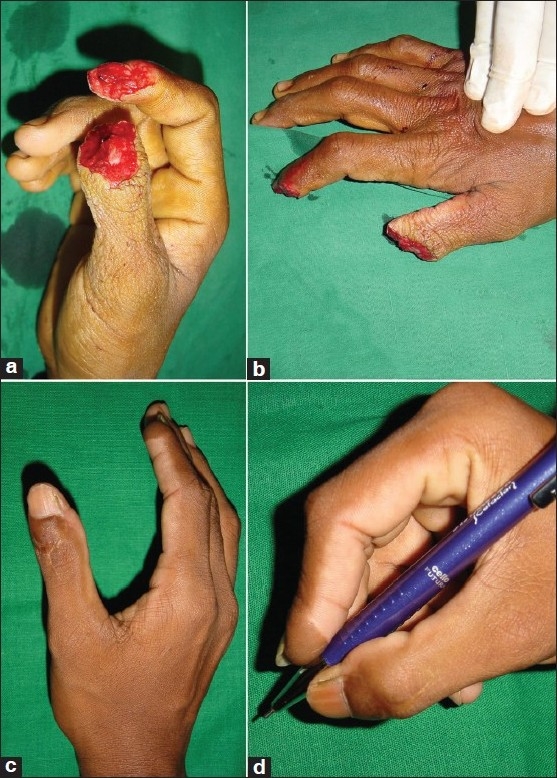
Case no 23, thumbtip replantation with cross finger flap to Index
RESULTS
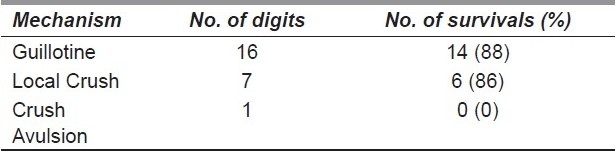
From 2000 to 2008, 24 fingertip replantations were performed, 21 of these survived. During the same period 358 other replantation were carried out in our department. The details of age, sex, finger-involved type of injury, structures repaired, fixation-type follow-up duration and outcome are provided in Table 1. The most common affected digit in the series was thumb followed by index, middle, and ring. The overall success rate was 87%, 86% in Tamai zone I and 88% in Tamai zone II [Table 2]. The survival rate was 88% in guillotine amputations and 86% in crush amputations [Table 3]. There were three failures in this series, of which two were due to venous and one because of arterial thrombosis. There were two cases of delayed partial necrosis of pulp that healed with dressings. More than 50% patients achieved 2 PD of 5–10 mm and 25% achieved a 2 PD of < 5 mm.
Table 1.
Patient details
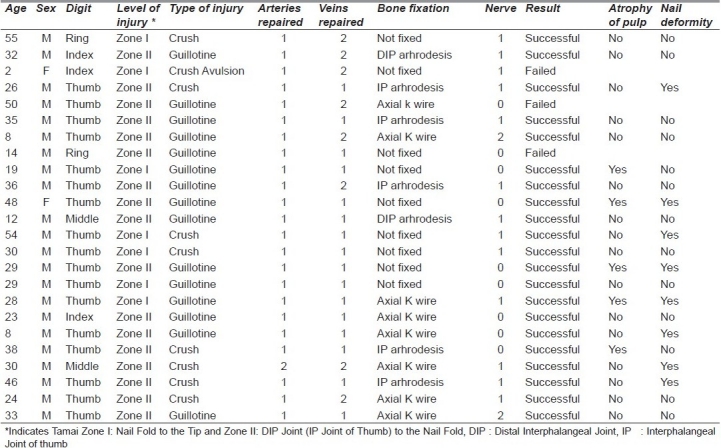
Table 2.
Relationship between survival and amputation levels
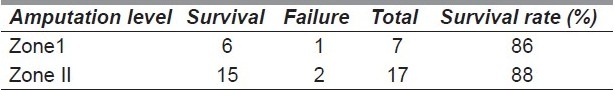
Table 3.
Relationship between survival and nature of injury:
The range of movement of DIP joints of fingers and IP joints of thumb in zone I replantation was satisfactory. Five patients had arthrodesis IP joint of thumb and two of the DIP joint of finger. Stiffness was associated with amputations in close proximity to a spared joint. However, in such cases, stiffness was in extension, with very little functional impairment.
Nail growth was near normal when the amputation was away from the germinal matrix [Figure 10a]. Nail deformity was observed in six patients in zone II and in two patients of zone I; all of these were associated with injury to the germinal matrix. Since none of these deformities interfered with daily function, no patient requested further surgery.
Figure 10.

(a) Longterm result showing good nail growth in right thumb when germinal matrix preserved (Case no 24). Left thumb had a previous nail bed injury.(b) Pulp atrophy seen following zone 2 thumb replantation (Case no 11)
Pulp atrophy was seen in five patients. Four of these had no nerve repair suggesting a possible correlation [Figure 10b]. Interestingly, a number of patients experienced significant sensory recovery even when no nerve repairs were done, especially in Tamai zone I amputation. There were nine patients in our series, who did not undergo nerve repair. Though the sensory recovery was good, 4/7 replants that survived developed pulp atrophy. There was no incidence of cold intolerance in any of these patients.
DISCUSSION
Accepted methods of treating fingertip amputation include nonoperative treatment such as allowing healing by secondary intention, shortening of the finger with primary closure, and local, regional, and even free flaps. Amputation through the nail base in adults has very little chance of survival as a composite graft. Elsahy[11] reported the 20% success rate for fingertips replaced as composite graft at or proximal to the lunula of the nail. Replantation significantly improves the chance of survival. Whenever it is technically possible, distal fingertip replantation remains superior to any alternative methods of reconstruction for the missing fingertip.
In Tamai zone I, venous anastomosis is comparatively more difficult as veins are very thin and sometime difficult to find. There are various technical tips from different authors to overcome such problems. Hattori et al.[12] reported that anastomosis in the thumb tip amputations were technically difficult due to the position of the thumb. Therefore, they apply vein graft to artery and vein before osteosynthesis and establish anastomosis using the vein graft. In our series, we did not encounter the need for this technique. Koshima et al.[13,14] have suggested arteriovenous anastomosis to eliminate the venous drainage problem. They also recommended performing arterial anastomosis first, then waiting for 24 h before re-exploring under local anesthesia so the engorged palmar veins could be more easily identified and anastomosed.
For amputation beyond the digital artery termination, a composite graft is recommended. More proximally, where the distal palmar arch is formed, anastomosis of the central digital artery and palmar vein was carried out without bone fixation.
The success rate of 87% in our series is attributable to proper patient selection and a high number of guillotine amputations.[15,16] Venous anastomosis in all patients also contributed to the overall success.
Functional outcome of replantation depends on sensory nerve recovery and pain-free movement of the finger joints. Movements of DIP (or IP in case of the thumb) can be salvaged in all Tamai zone I and most Tamai zone II amputations when the joint surface is not damaged or arthrodesed. Even if the joint is arthrodesed, normal movements at proximal inter phalangeal joint in case of fingers and metacarpophalangeal joint in case of thumb can achieve a good function. In Zone I amputations, nerve disruption is very distal, and the sensory recovery is very satisfactory in spite of not repairing the nerve. All have adequate pinch and grip strength.
The survival rate of zone I (86%) is comparable to that zone II (88%) in spite of technical difficulties involved. Bony union was achieved without any case of nonunion of distal phalanx even when no K-wire fixation was used. The no K-wire technique of osteosynthesis also allows for some venous drainage through the medullary cavity of the distal phalanx.
Cold intolerance after replantation has been reported previously. Of note, in our series none of the patients complained of cold intolerance. Shieh et al.[17] also emphasized the importance of long period of sensory re-education. We also consider that postreplantation rehabilitation and re-education have an important influence on the overall sensory recovery.
Fingertip replantation is more demanding than proximal digital replantation as the vessels are smaller and has low margin of error during vessel repair.[18] Regularly undertaking fingertip replantation should minimize the time taken and also remove apprehension that is usually associated with operating on vessels of small size at this level.
Frequently performing replantations yields higher success rates and the time shorter, making it a worthwhile endeavor. Patients are very satisfied with the outcome. Regularly performing fingertip replantation also improves microsurgical skills that are useful for performing small perforator-based free flaps.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Tamai S. Twenty years’ experience of limb replantation review of 293 upper extremity replants. J Hand Surg Am. 1982;7:549–56. doi: 10.1016/s0363-5023(82)80100-7. [DOI] [PubMed] [Google Scholar]
- 2.Hirase Y. Salvage of fingertip amputated at nail level: New surgical principles and treatments. Ann Plast Surg. 1997;38:151–7. doi: 10.1097/00000637-199702000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Allen MJ. Conservative management of finger tip injuries in adults. Hand. 1980;12:257–65. doi: 10.1016/s0072-968x(80)80049-0. [DOI] [PubMed] [Google Scholar]
- 4.Yamano Y. Replantation of the amputated distal part of the fingers. J Hand Surg Am. 1985;10:211–8. doi: 10.1016/s0363-5023(85)80107-6. [DOI] [PubMed] [Google Scholar]
- 5.Strauch B, de Moura W. Arterial system of the fingers. J Hand Surg Am. 1990;15:148–54. doi: 10.1016/s0363-5023(09)91123-6. [DOI] [PubMed] [Google Scholar]
- 6.Wei FC, Chang YL, Chen HC, Chuang CC. Three successful digital replantations in a patient after 84, 86, and 94 hours of cold ischemia time. Plast Reconstr Surg. 1988;82:346–50. doi: 10.1097/00006534-198808000-00026. [DOI] [PubMed] [Google Scholar]
- 7.Venkatramani H, Sabapathy SR. A simple technique for securing the amputated part in fingertip replantation. Br J Plast Surg. 2004;57:592–3. doi: 10.1016/j.bjps.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 8.Tsai TM, McCabe SJ, Maki Y. A technique for replantation of the finger tip. Microsurgery. 1989;10:1–4. doi: 10.1002/micr.1920100102. [DOI] [PubMed] [Google Scholar]
- 9.Sabapathy SR, Venkatramani H, Bharathi RR, Sebastin SJ. Distal fingertip replantation without skeletal fixation. J Reconstr Microsurg. 2005;21:11–3. doi: 10.1055/s-2005-862773. [DOI] [PubMed] [Google Scholar]
- 10.Hattori Y, Doi K, Ikeda K, Estrella EP. A retrospective study of functional outcomes after successful replantation versus amputation closure for single fingertip amputations. J Hand Surg Am. 2006;31:811–8. doi: 10.1016/j.jhsa.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 11.Elsahy NI. When to replant a finger tip after its complete amputation. Plast Reconstr Surg. 1977;60:14–21. [PubMed] [Google Scholar]
- 12.Hattori Y, Doi K, Ejiri S, Baliarsing AS. Replantations of very thumb distal amputations with pre-osteosynthesis interpositional vein graft. J Hand Surg Br. 2001;26:105–7. doi: 10.1054/jhsb.2000.0539. [DOI] [PubMed] [Google Scholar]
- 13.Koshima I, Soeda S, Moriguchi T, Higaki H, Miyakawa S, Yamasaki M. The use of arteriovenous anastomosis for replantation of the distal phalanx of the fingers. Plast Reconstr Surg. 1992;89:710–4. doi: 10.1097/00006534-199204000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Koshima I, Yamashita S, Sugiyama N, Ushio S, Tsutsui T, Nanba Y. Successful delayed venous drainage in 16 consecutive distal phalangeal replantations. Plast Reconstr Surg. 2005;115:149–54. [PubMed] [Google Scholar]
- 15.Kim WK, Lim JH, Han SK. Fingertip replantations: Clinical evaluation of 135 digits. Plast Reconstr Surg. 1996;98:470–6. doi: 10.1097/00006534-199609000-00017. [DOI] [PubMed] [Google Scholar]
- 16.Lee BJ, Chung HY, Kim WK, Kim SW, Dhong ES. The effects of the number and ratio of repaired arteries and veins on the survival rate in digital replantation. Ann Plast Surg. 2000;44:288–94. doi: 10.1097/00000637-200044030-00007. [DOI] [PubMed] [Google Scholar]
- 17.Shieh SJ, Chiu HY, Hsu HY. Long-term effects of sensory reeducation following digital replantation and revascularisation. Microsurgery. 1998;18:334–6. doi: 10.1002/(sici)1098-2752(1998)18:5<334::aid-micr7>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 18.Foucher G, Norris RW. Distal and very distal digital replantations. Br J Plast Surg. 1992;45:199–203. doi: 10.1016/0007-1226(92)90076-a. [DOI] [PubMed] [Google Scholar]
- 19.Sabapathy SR, Venkatramani H, Bharathi RR, Sebastin SJ. Distal fingertip replantation without skeletal fixation. J Reconstr Microsurg. 2005;21:11–3. doi: 10.1055/s-2005-862773. [DOI] [PubMed] [Google Scholar]


