Abstract
Background:
Yoga has been shown to have many short-term health benefits, but little is known about the extent to which these benefits accrue over a long time frame or with frequent practice.
Aims:
The purpose of this study was to examine the extent to which body mass index (BMI) and medication use in a sample of female yoga practitioners over 45 years varied according to the length and frequency of yoga practice.
Materials and Methods:
We administered online surveys to 211 female yoga practitioners aged 45 to 80 years. We used regression analyses to evaluate the relationship of extent of yoga experience to both BMI and medication use after accounting for age and lifestyle factors. We also conducted comparisons with 182 matched controls.
Results:
Participants had practiced yoga for as long as 50 years and for up to 28 hours per week. There were significant inverse relationships between yoga experience and both BMI and medication load. These significant relationships remained after accounting for age and lifestyle factors. When we computed yoga experience in terms of total calendar years, without accounting for hours of practice, significant relationships did not remain. However, there was no obesity in the 49 participants with more than 25 years of yoga practice. Yoga practitioners were less likely than non-practitioners to use medication for metabolic syndrome, mood disorders, inflammation, and pain.
Conclusions:
A long-term yoga practice was associated with little or no obesity in a non-probability sample of women over 45 years. Relationships showed a dose-response effect, with increased yoga experience predicting lower BMI and reduced medication use.
Keywords: Yoga, medication use, aging, healthy aging, women, body mass index
INTRODUCTION
Two related markers of physical well-being in adults are body mass index (BMI) and medication use.[1] Overweight (BMI 25.0 to 29.9 kg/m2) and obesity (BMI ≥30.0 kg/m2) are associated with increased all-cause mortality.[2] Older women are particularly vulnerable to overweight and obesity. A study[3] of 647 White American women aged 57 to 74 years showed that 70% of the sample was overweight or obese.
Because people use medications to address health problems, medication load can be understood as one indicator of overall illness burden[1] and as an inverse predictor of quality of life.[4] Many medications are associated with negative health outcomes, and the use of multiple medications is a known risk factor for increased morbidity and mortality in the elderly.[5] Women over 65 years are the highest users of medication, with 23% of women over 65 years taking at least five medications in the preceding week.[6]
Yoga has been shown to be useful for addressing a wide range of health conditions.[7,8] Yoga is a mind-body practice integrating ethical principles, daily behaviors, physical postures, breathing techniques, self-awareness, deep relaxation techniques, and meditation into a system for personal growth, well-being, and self-realization.[9] Approximately 6.1% of the American population was found to have engaged in some form of yoga practice for health purposes in 2007, up from 5.1% in 2002.[10,11] Hatha yoga is a form of yoga with emphasis on physical postures.
Several studies of yoga among the middle-aged and the elderly have shown positive results.[12–16] A 6-month Iyengar yoga practice in elderly people led to improvements in fatigue and in overall physical wellness.[17] Participants also improved in measures of balance, flexibility, physical strength, pain, and social functioning.[17]
Most studies of the effects of Hatha yoga experience have involved short-term interventions with beginners, lasting between a few days and a few months. Little is known about whether the benefits of yoga continue to accrue over a long time frame. Therefore, the long-term benefits of yoga may be systematically underestimated in the literature.
An observational study[18] of 15,550 adults aged between 53 and 57 years showed that yoga practitioners of normal weight (BMI <25 kg/m2) gained less weight than did other participants, and that overweight yoga practitioners on average lost weight, from age 45 years to recruitment. However, data were not available on the longevity of the yoga practice beyond 4 years. The specific types of yoga practices evaluated were not indicated in the study. Many participants reported practices of no more than 30 minutes per session, or half the length of a typical public yoga class, and few participants had practiced yoga for more than 4 years.[18] In another study,[19] adults with obesity were found to be less likely to use yoga as a therapeutic modality than were other adults. No other studies have been conducted showing evidence of whether a long-term yoga practice offers protection against obesity.
Early experimental studies showed reduced medication use for asthma,[20,21] heart disease,[22] high blood pressure,[22] Type 2 diabetes,[23,24] and obsessive-compulsive disorder[25] after yoga interventions. However, there have been no observational studies to indicate whether a long-term yoga practice is associated with a reduction in the overall use of pharmaceutical medications. As overall medication use is a marker of illness burden[1] and quality of life,[4] demonstrating a reduction in medication use with a long-term yoga practice will provide supportive evidence for the long-term effectiveness of yoga in protection from illness.
MATERIALS AND METHODS
The purpose of this correlational, cross-sectional study was to determine whether a long-term Hatha yoga practice was associated with a lower BMI and reduced medication use in a group of women over 45 years. We located participants through postings to senior lists, health clubs, religious organizations, social action networks, online university lists, and charitable organizations. In addition, we asked yoga teachers to distribute flyers and notifications to yoga students, and we invited members of online yoga lists to participate. We recruited subjects without geographical restrictions. We assumed a working knowledge of English sufficient to understand and complete the survey. As compensation for participating in the study, all respondents had the option of entering a drawing for a $75 first prize and three $25 second prizes.
All participants were females at least 45 years old. We defined yoga practitioners as individuals who reported nonzero hours per week of current yoga practice and nonzero prior history of yoga practice. We defined yoga to include asana (postures), practiced along with controlled breathing and meditation. We computed seated meditation, practiced apart from asana, as a distinct variable. To enhance the interpretation of the analysis, we recruited non-practitioner controls matched for age, ethnicity, country of residence, and education.
The Institutional Review Board of Northcentral University granted permission in October 2009 to conduct the study. We collected data online through SurveyMonkey[26] in October and November 2009. Participants indicated informed consent by a selection on the first screen of the survey. All measures were self-reported.
Measures
Predictor variables
The predictor variables for this study were current hours per week of yoga practice, total lifetime hours of yoga practice, and total calendar years of yoga practice. Participants entered one line of information for each period of yoga practice in their lives, indicating the years and months of the practice and the hours per week practiced during that period. We totaled years and months of practice to obtain total calendar years. We computed total lifetime hours by calculating the total hours for each line of information and summing the results. Participants entered current hours per week separately as a scalar value.
Outcome variables
The outcome variables for this study were BMI and number of distinct medications used per week. Participants entered height and weight information, as well as other demographic data and other indices of psychological and physical wellness. Participants reported their heights in feet, inches, and fractions of an inch in increments of one eighth. Participants then reported weight in pounds or kilograms. We then used height and weight to calculate BMI, according to the formula BMI = (WT * 703) / (HT2), where WT represented weight in pounds and HT represented height in inches.
Participants entered the number of different prescription medications used per week. Participants then completed a set of yes-no questions regarding 18 specific conditions for which they took prescription medication, including high blood pressure, diabetes or prediabetes, bone density, depression, anxiety, and sleep. We asked a separate question about the regular use of pain medication, whether or not by prescription. If a participant indicated more distinct medications in the medication list than were indicated in the total number of medications question, we raised the total number of medications to match the number indicated in the medication list.
Covariates
Participants provided data for age, educational level, marital status, levels of processed food consumption, hours of non-yogic exercise per week, and hours of seated meditation per week. We computed age as year of birth subtracted from 2009. Participants indicated level of education on an ordinal scale, with values ranging from 1 (less than high school) to 6 (doctoral degree). Participants indicated marital status on the basis of five nominal values, and we condensed the values for this analysis into a dichotomous variable, partnered vs unpartnered. Participants reported average non-yogic exercise hours per week and hours of seated meditation per week as scalar values. We computed BMI as a covariate when analyzing number of medications.
Participants reported the level of processed food consumption on a Likert-type scale in response to the question, “I eat a lot of refined sugar, refined flour, and processed food.” Although food frequency questionnaires asking individuals to recall specific food items recently consumed have been shown to be unreliable, questionnaires assessing general food consumption patterns have been found to be more robust.[27] We chose processed food consumption as an indicator of dietary health because refined and processed food consumption, but not whole-grain consumption, positively predicted ischemic heart disease, cancer, and all-cause mortality in older women.[28–30] Values ranged from 1 (very true) to 7 (not at all true), with higher scores representing lower levels of processed food consumption. The food variable was a single-item question, and a factor analysis was therefore not needed.
Statistical analyses
Bivariate correlations were computed to determine the relationship between yoga experience and BMI. Multiple linear regression analyses were then performed to determine the contribution of yoga practice to BMI after correcting for covariates. To compute the bivariate relationship between the predictor variables and number of medications used, the non-parametric Spearman's rho statistic was used. Negative binomial regression analyses were conducted to determine the contribution of yoga practice to medication use after correcting for covariates. We compared yoga practitioners and controls using independent samples t tests and analyses of variance.
RESULTS
The completion rate for usable surveys was 80.9%. Initial data for yoga practitioners consisted of 212 completed records. We removed an outlier record indicating 140 years of practice history. We transformed remaining outliers, defined as values more than 4 standard deviations from the mean, to natural logarithmic scores, but transformations did not affect the significance of any analyses. We therefore retained the original values. Seven yoga practitioners declined to enter body weight, leaving 211 yoga practitioners for the medication analyses and 204 yoga practitioners for the BMI analyses.
We included the control group to facilitate interpretation of the regression analyses. Controls consisted of 183 women aged 45 to 77 years who indicated no current yoga practice or no prior history of yoga practice. One outlier record with a birth year of 1914 was removed. Ten controls declined to enter body weight, leaving 182 controls for the comparisons involving medication use and 172 controls for the comparisons involving BMI.
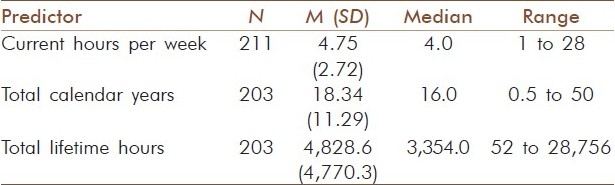
Frequency distributions
Participants ranged in age from 45 to 80 years, with a mean age of 56.4 (SD = 7.2, N = 386). Ninety-four percent of the sample participants lived in the United States or Canada, and 93.0% were Caucasian or of European origin. Eighty-six percent had graduated from college. Yoga practitioners exercised an average of 4.21 hours per week (SD = 2.80), excluding yoga practice, and engaged in seated meditation an average of 2.56 hours per week (SD = 3.26). Controls exercised an average of 3.26 hours per week (SD = 2.42), excluding yoga practice, and engaged in seated meditation an average of 0.46 hours per week (SD = 1.46). Table 1 displays the distributions of the predictor variables for the yoga practitioner group.
Table 1.
Extent of yoga practice
Body mass index
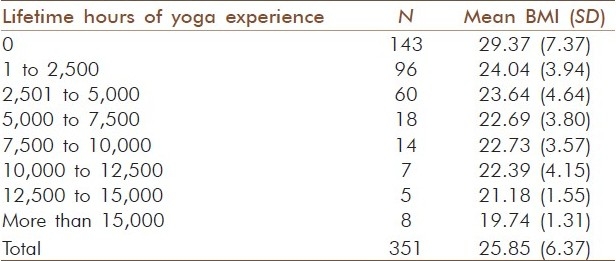
None of the 49 yoga practitioners who had practiced yoga 26 years or more were obese. Table 2 shows the distribution of mean BMI for all participants, grouped according to total lifetime hours. For all participants and for the yoga subjects, the distribution of residuals for BMI was right-skewed. To normalize the distribution, BMI was inverse-transformed. An inverse relationship between the predictor variables and BMI therefore resulted in positive coefficients in the correlation and regression analyses.
Table 2.
Body mass index distributions based on lifetime hours of yoga experience
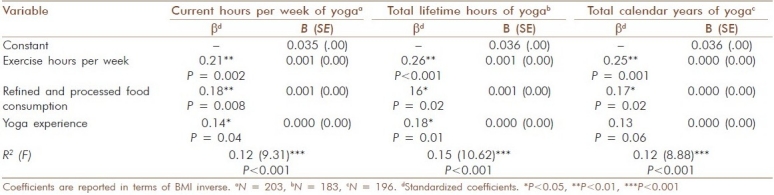
Bivariate computations showed that mean inverse BMI scores were positively correlated with current hours per week of yoga, R (202) = 0.21, P = 0.003; with total lifetime hours of yoga practice, R (182) = 0.23, P = 0.002; and with total calendar years of yoga practice, R (195) = 0.16, P = 0.02. We then performed multiple regression analyses to determine whether the extent of yoga experience predicted levels of BMI over and above significant covariates. Age, educational level, marital status, and hours of seated meditation per week did not show a significant contribution to BMI for any regression model. Therefore, we used a reduced model, including only non-yogic exercise hours per week and level of refined and processed food consumption as covariates. Both total lifetime hours (P = 0.01) and current hours per week (P = 0.04) accounted for a significant proportion of the variance in levels of BMI [Table 3]. Total calendar years of yoga practice was marginally significant, P = 0.06.
Table 3.
Predictors of body mass index
Medication use
The mean number of medications for yoga practitioners was 1.39 (N = 211, SD = 1.72, median = 1, mode = 0). Forty-six percent took no medication, and only one participant took more than seven medications regularly. No yoga practitioner in the study took more than nine medications. Table 4 displays a detailed breakdown of the number of medications used regularly.
Table 4.
Number of medications used, detailed
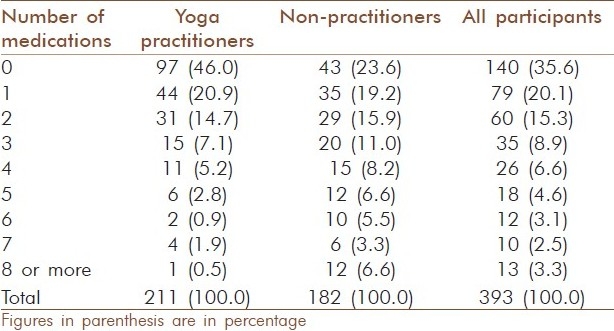
All medications were specified as prescription medications in the survey, except for pain medication. Yoga practitioners reported medications most commonly used as medications for thyroid conditions (15.6%), bone density (9.0%), high cholesterol (9.0%), high blood pressure (8.5%), depression (7.6%), and pain (7.1%). Medication use followed a non-normal, Poisson distribution. Scores peaked at 0 and sloped rapidly to the right. We therefore calculated the non-parametric Spearman's rho coefficient to compute the bivariate association between the predictor variables and number of medications used. There was a significant inverse association between current hours per week of yoga practice and number of medications, ρ(209) = -0.16, P = 0.002. There was a significant inverse association between total lifetime hours of yoga practice and number of medications, ρ(189) = -0.18, P = 0.002. There was not a significant association between total calendar years of yoga practice and number of medications, ρ(203) = -0.08, P = 0.023.
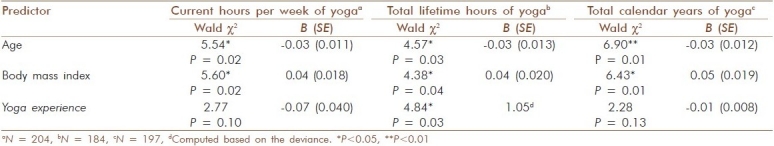
To account for the contribution of covariates to the number of medications taken, we used negative binomial regression analyses in preference to Poisson regression models, because the data did not meet the assumption of the Poisson model for equal variances. Educational level, marital status, level of processed food consumption, and weekly hours of meditation did not show a significant contribution to medication use for any negative binomial regression model. Therefore, we used a reduced model, including only age and BMI as covariates. After accounting for age and BMI, there was a significant inverse contribution of total lifetime hours to medication use, P = 0.03 [Table 5]. The association between BMI and number of medications for yoga practitioners was not significant, ρ(202) = 0.11, P = 0.13.
Table 5.
Predictors of number of medications used
Control group
Controls engaged in non-yogic exercise significantly less than yoga practitioners, T(389) = -3.58, P<0.001. Controls engaged in seated meditation significantly less than yoga practitioners, T(296) = -7.98, P<0.001. Although the obesity rate of yoga practitioners was 6.4%, 65 of 172 non-practitioners (37.8%) were obese. Of controls aged 57 to 74 years, 70.17% were overweight or obese, a rate comparable with the 70.15% combined overweight and obesity rate for White American women aged 57 to 74 years.[3]
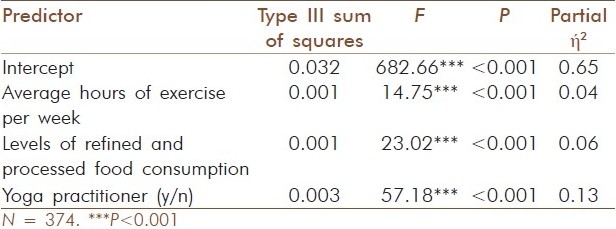
We conducted independent samples t tests to determine the differences in BMI and medication use between yoga practitioners and non-practitioners. The difference in BMI (computed as BMI inverse) between yoga practitioners (N = 204, M = 23.24, SD = 4.17) and non-practitioners (N = 172, M = 28.95, SD = 7.16) was significant, T(374) = -10.44, P<0.001. Analyses of variance showed that age, educational level, marital status, and hours of seated meditation per week did not contribute significantly to the outcome. After correction for average exercise hours per week and levels of refined and processed food consumption, differences between yoga practitioners and non-practitioners remained significant, F(3,370) = 57.18, P<0.001, partial eta square = 0.13 [Table 6]. The effect of the yoga practice was stronger than was the effect of either exercise or food consumption.
Table 6.
Mean body mass index: analyses of variance
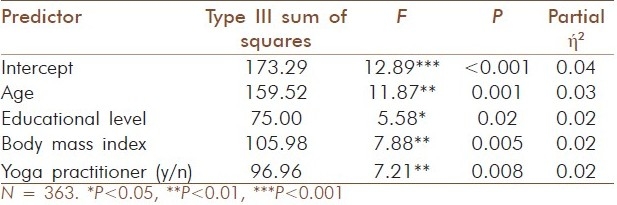
The mean number of medications for non-practitioners was 3.18 (N = 182, SD = 5.14, median = 2, mode = 0). Results of an independent samples t test showed that the difference in number of medications between yoga practitioners and non-practitioners was significant, T(391) = 5.00, P<0.001. Marital status, hours of exercise per week, level of refined and processed food consumption, and hours of seated meditation per week did not contribute significantly to the outcome. After correcting for age, educational level, and BMI, differences between yoga practitioners and non-practitioners remained significant, F(3,354) = 7.21, P = 0.008, partial eta square = 0.02 [Table 7].
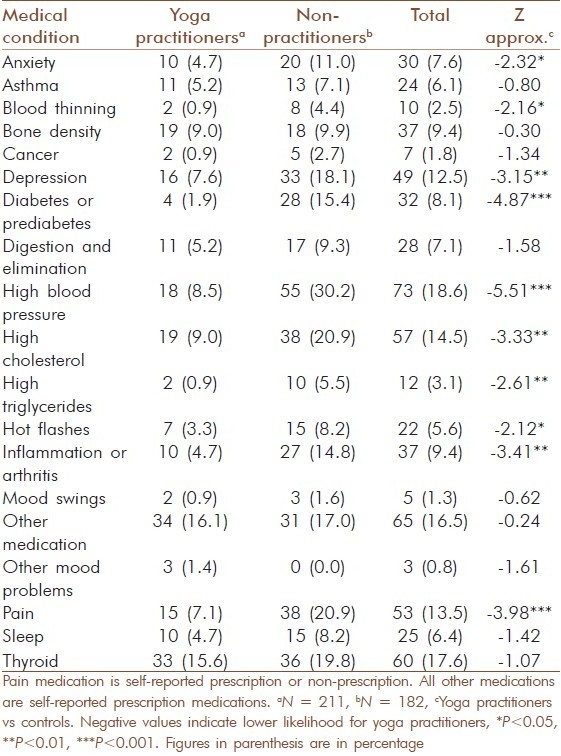
Table 7.
Mean number of medications used: analyses of variance
Among non-practitioners, 23.6% took no medication and 12 took more than seven medications regularly. Two non-practitioners reported taking 42 distinct prescription or pain medications on a regular basis. In contrast, 46% of yoga practitioners took no medication and only one yoga practitioner took more than seven medications regularly. Non-practitioners were more likely than yoga practitioners to take medications for high blood pressure, high cholesterol, high triglycerides, blood thinning, diabetes or prediabetes, hot flashes, inflammation or arthritis, depression, anxiety, and pain [Table 8]. In contrast to the lack of association between BMI and number of medications among yoga practitioners, there was a strong positive association between BMI and number of medications among non-practitioners, ρ(170) = 0.40, P<0.001.
Table 8.
Types of medications used for conditions requiring medication
DISCUSSION
Both BMI and medication use are inverse markers of physical wellness.[1] Older women are particularly vulnerable to overweight and obesity, with 36.9% of White women aged 57 to 74 years obese and 33.2% overweight.[3] Although medication use tends to increase with age, an early study[31] showed that very old individuals who remained independent and active in the community tended to use little medication regularly.
There have been few observational data about either BMI or medication use among individuals who have practiced yoga for many years or who practice yoga frequently. Bertisch et al.[19] found that persons with obesity were less likely to use yoga as a therapeutic modality, but responses were based on the practice of yoga for as little as one instance in the prior 12 months. Kristal et al.[18] compared weight gain and weight loss in middle-aged individuals with and without a yoga practice. However, reported weights were based on memories of earlier life periods, the duration of practice was reported only in total years, and distinctions were not made for individuals who had practiced yoga for more than 4 years. Until the current study, empirical data were not available associating BMI with yoga experience in the population of individuals who had practiced yoga for many years or decades.
This study was an evaluation of the relationship between extent of yoga experience and two measures of physical wellness in yoga practitioners. Extent of yoga experience was measured on three dimensions: current hours per week, total calendar years, and total lifetime hours. Use of the Internet enabled contact with a highly specific and sparsely distributed population in sufficient numbers for a well-powered study (1 – β >0.99). Although the primary purpose of the study was to investigate a possible dose-response effect between yoga experience and outcome variables, a control group was included to enhance the interpretation of the results.
Body mass index
Bivariate correlations and multiple linear regressions were performed to analyze the relationship of current hours per week, total lifetime hours, and total calendar years to BMI for yoga practitioners. Bivariate analyses showed a significant inverse relationship between extent of yoga experience and BMI. In the regression analysis, the relationship remained significant between total lifetime hours of yoga and BMI (P = 0.01), and between current hours of yoga per week and BMI (P = 0.04), after accounting for hours of weekly non-yogic exercise and refined and processed food consumption.
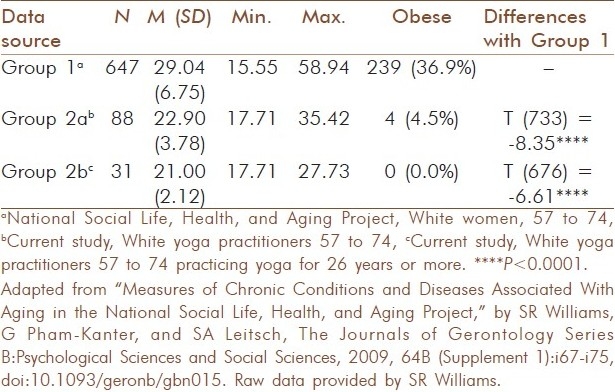
There were significant differences in BMI between yoga practitioners and non-practitioners, P<0.001. Participants who practiced yoga were on average of normal weight, and participants who did not practice yoga were on average close to the level of obesity. Whereas 37.8% of all non-practitioners in this study were obese (N = 171), none of the 49 yoga practitioners who had practiced yoga 26 years or more was obese. We compared findings with available epidemiological data for BMI among White women aged 57 to 74 years.[3] Mean differences between yoga practitioners and the comparison population were strongly significant, P<0.0001 [Table 9].
Table 9.
Body mass index comparisons, white women 57 to 74
Until present, only the study by Kristal et al.[18] demonstrated a connection between a long-term yoga practice and BMI, with a long-term yoga practice defined as a practice lasting at least 4 years. Kristal et al. showed that yoga practitioners in their 50s were more likely to lose weight, and less likely to gain weight, over a 10- to 15-year period compared with non-practitioners. However, Kristal et al. did not demonstrate a linear correlation between extent of yoga experience and BMI. Furthermore, prior weights were reported based on participant memories of body weight dating back 10 to 15 years. The current study has shown a significant inverse relationship between a yoga practice and BMI, even after controlling for other lifestyle factors. This is the first study to demonstrate a dose-response relationship between extent of yoga experience and BMI.
We evaluated BMI for yoga practitioners with minimal levels of yoga experience. The mean BMI for yoga practitioners with under 2 hours per week of current yoga practice (N = 13) was 24.56. The mean BMI for yoga practitioners with under 200 lifetime hours of yoga practice history (N = 20) was 24.08. The mean BMI for yoga practitioners with under 1.5 years of yoga practice (N = 17) was 24.52. Therefore, even at beginning levels of yoga practice, participants who chose to practice yoga had a lower BMI on average compared with participants who had never initiated a yoga practice. This finding lends support to an inference that yoga practitioners began their practice with initially lower BMI compared with non-practitioners, confirming findings by Bertisch et al.[19] that individuals with obesity were less likely to engage in even a single yoga session.
Mean BMI values declined as total lifetime hours increased. Many factors could account for this finding. Amount of non-yogic exercise and levels of processed food consumption explained a significant proportion of the variance in BMI. However, these statistics do not reveal the effect of a yoga practice in encouraging people to eat a healthy diet and engage in other forms of exercise. Levels of body awareness have been shown to be higher for yoga practitioners than for non-practitioners.[32] Yoga masters commonly claim that a yoga practice leads to other health-building practices as a result of the increased embodied awareness that is created.[33]
Medication use
We performed non-parametric correlations and negative binomial regressions to analyze the relationship of current hours per week, total lifetime hours, and total calendar years to the number of different medications used per week. There was a significant inverse relationship between yoga experience and medication use. This is the first study to show a dose-response effect between yoga practice and medication use, with more lifetime hours of a yoga practice associated with a lower level of medication use even after correcting for age and BMI.
Assumptions
We assumed in this study that if an individual was using a prescription medication to address a particular health concern, then the health concern was a condition that had been diagnosed by a physician and was considered serious enough to warrant treatment.[1] We assumed that if a person consumed pain medication, even if not prescribed by a physician, then the person was experiencing pain. On the basis of these assumptions, we reported the number of medications used as one marker of illness burden.[1] However, the reverse assumption may not be valid. A person may have a diagnosable condition, such as high blood pressure or low bone density, and decline the use of prescription medication. It is possible that people who practice yoga are more likely to decline the use of prescription medication than are people who do not practice yoga. Differences between yoga practitioners and non-practitioners in medication scores may therefore not fully reflect differences in actual health status.
We assumed that participants had a working knowledge of English sufficient to understand and respond to questions. We assumed that responses to self-report questions were truthful and accurate. Although there was no third-party verification of any responses given by participants, this assumption was needed in order to conduct the study.
Because the number of participants taking each medication was relatively small, the significance of the findings regarding the use of different forms of medication should be interpreted with caution. Significant differences were found between yoga practitioners and controls in the number of medications used for metabolic syndrome (including diabetes, high blood pressure, unhealthy cholesterol, high triglycerides, and blood composition), anxiety, depression, inflammation (including arthritis and hot flashes), and pain. There was a strong positive association between medication use and BMI in the study sample among non-practitioners. This finding was consistent with that of Jarrett et al.[1] who showed that BMI was associated with increased medication load in adults aged 40 to 70 years, although not in younger adults.
The findings regarding medication use may lend themselves to several interpretations. Individuals who practice yoga may have begun practicing with a higher level of wellness and may have needed less medication initially than did non-practitioners. Individuals who practice yoga may have philosophical objections to prescription medication, preferring to solve their health problems by other means. Individuals who require multiple medications may find themselves uninterested in a yoga practice, for whatever reason. However, there is much research evidence that yoga creates improvements in conditions for which bearers are frequently prescribed medication, including cardiovascular conditions,[34] diabetes,[35,36] chronic pain,[37] and mood disorders.[38,39] There is even biological evidence that mind/body practices create changes in genomic expression in both short and long terms.[40] The research evidence indicating that yoga is an effective treatment for many physical and psychological health conditions lends credence to an interpretation that a yoga practice is effective in reducing the number of medications used regularly, and therefore in reducing the illnesses associated with those medications.
Limitations
This study was limited by a non-probabilistic sample selection. All participants had Internet access, 81.4% had graduated from college, and 93.0% were Caucasian or of European origin. The sample distribution was therefore skewed. The group sizes (practitioners vs non-practitioners) were unequal, with 53.6% of the sample consisting of yoga practitioners. The age range of 45 to 80 years was wide. Although yoga teachers distributed information about the study to yoga students representing a range of experience, individuals more subjectively committed to a yoga practice may have been more inclined to participate in the study. Recruitment of some participants from yoga lists and through yoga networks may have also biased the sample selection.
We evaluated the generalizability of the results of the study for non-practitioners with a comparison of measures of BMI found in the study sample to other epidemiological measures of BMI. In a recent study conducted by the National Social Life, Health, and Aging Project (NSHAP), BMI was investigated in the general population.[3] The percent of White participants aged 57 to 74 years who were overweight or obese was virtually the same (White women only; 70.15%) as in the current study (White non-practitioners only; 70.17%). The BMI for White non-practitioners aged 57 to 74 years in the current study (M = 29.43, SD = 7.38, N = 143) was slightly higher than was the BMI for all White women in the NSHAP study (M = 29.04, SD = 6.75, N = 674), and the percentage of obesity was higher in the current study (43.29%) compared with the NSHAP study (36.94%). It is important to acknowledge, however, that in the current study, yoga practice was significantly correlated with healthy eating and regular exercise. Therefore, the non-practitioner subset of the current study may have been preselected against certain wellness practices and may therefore not have been representative of White women in the overall U.S. population. No measures were available to compare the yoga sample in the study with a wider population of yoga practitioners over 45 years.
This study has the known limitations of a self-report questionnaire measuring lifestyle behaviors. As all data were self-reported, the reliability of the information regarding lifestyle factors for this study is unknown. The interpretation of the meaning of the terms used in the question about food consumption was left to the respondent and may have been different among different participants. Fourteen records were unusable for the total lifetime hour calculation, because the respondents entered total years without entering corresponding hours for each period of past practice. A similar measure had been used in a study of meditators,[41] but Lazar et al. gathered the information in the course of structured interviews. Further research is needed to determine a more reliable way to gather information on the total lifetime hours of a long-term wellness practice in an anonymous Internet survey.
This study was limited by the cross-sectional, observational design. Cause and effect could not be determined. Obese women and those with existing disorders may be less attracted to yoga practice compared with healthy women of normal weight, who may be more likely to engage in a serious, long-term yoga practice. As noted above, findings lend support to an inference that yoga practitioners began their practice with initially lower BMI compared with non-practitioners. Nevertheless, a dose-response effect is sometimes considered to be evidence of a causal relationship even in the absence of a controlled experiment,[42,43] particularly when supported by prior research[18,41] and biological plausibility.[42] The dose-response effect reported in this study lends support to an inference that yoga played a catalytic role in the linear relationships found.
More reliable results would be obtained by a longitudinal study tracking beginning yoga students over a time period of 2 to 5 decades. However, the entire concept of cause and effect is problematic in a wellness practice that is long-term, acausal, unpredictable, recursive, and nonlinear in nature.[44–46] An observational design is believed to be a better approach than is an experimental design for evaluating behaviors and treatments that are complex, of indefinite duration, self-correcting (i.e., if one approach does not work well, another is tried), multifaceted, designed to address overall improvement, sought and selected by the subjects, and characteristic of large, heterogeneous populations.[43,47–49]
CONCLUSION
Most studies involving the effects of the Hatha yoga experience are conducted with beginners over brief periods, from a few days to a few months. Although there is evidence that yoga creates benefits within periods as brief as 1 hour of practice,[50–52] yoga is intended to be engaged in for a lifetime, from childhood through to old age. It is therefore likely that the gains reported in the literature for yoga systematically underestimate the potential of the practice for creating benefits that continue to accrue over time.
This observational study involving long-term yoga practitioners showed that a consistent, long-term Hatha yoga practice in a non-probability sample of women over 45 years was linearly associated with declines in BMI even after correcting for non-yogic exercise hours and processed food consumption. The study also showed a yoga practice in this sample to be associated with reduced medication use, particularly in regard to medications for metabolic disorders, inflammatory conditions, pain, and mood. When we used the calendar years of yoga practice as the independent variable, rather than total lifetime hours or current hours per week, we did not find significant associations. However, there was no obesity among the 49 participants who had practiced yoga for 26 years or more.
BMI was a strong predictor of medication use for non-practitioners, but not for women who practiced yoga. Studies are needed with larger numbers of yoga practitioners, so that differences based on specific types of medications can be investigated with the use of parametric statistics. Future studies would benefit from a more systematic sample selection, with participant selection reflecting the distribution of the yoga population in terms of educational level, ethnicity, and the use of the Internet.
Yoga practice predicted lower levels of medication use in the study sample even after correcting for age and BMI. Future research is needed to determine whether a yoga practice protects against illness even when BMI is relatively high, while at the same time protecting against obesity itself, as appeared to be the case in the current sample. Findings from this study are consistent with an interpretation that hours of yoga per week and total lifetime hours of practice are related to declines in BMI and medication use over a long time period. Findings are consistent with an interpretation that certain benefits of a Hatha yoga practice continue to accrue over a long time frame, with frequent practice. However, because a non-probability sample was used for this study, the generalizability of the findings to a larger population of women over 45 years remains unknown.
ACKNOWLEDGMENTS
This presentation is based on a dissertation that Nina Moliver completed at Northcentral University under the faculty advisement of Dr. Eva M. Mika, Dr. Max S. Chartrand, and Dr. R. Bruce McNellie. We offer our sincere thanks to the women who participated in this study and to Dr. Karen Grace-Martin for her statistical assistance. The study received the Dissertation of the Year award in 2010.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Jarrett B, Bloch GJ, Bennett D, Bleazard B, Hedges D. The influence of body mass index, age and gender on current illness: A cross-sectional study. Int J Obes (Lond) 2010;34:429–36. doi: 10.1038/ijo.2009.258. [DOI] [PubMed] [Google Scholar]
- 2.Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1.46 million White adults. N Engl J Med. 2010;363:2211–9. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams SR, Pham-Kanter G, Leitsch SA. Measures of chronic conditions and diseases associated with aging in the National Social Life, Health, and Aging Project. J Gerontol B Psychol Sci Soc Sci. 2009;64(Supplement 1):i67–75. doi: 10.1093/geronb/gbn015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Field Trial, WHOQOL-100. 1995. [Last accessed on 2009, July 12]. Available from: http://www.who.int/mental_health/who_qol_field_trial_1995.pdf .
- 5.Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5:345–51. doi: 10.1016/j.amjopharm.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population in the United States. JAMA. 2002;287:337–44. doi: 10.1001/jama.287.3.337. [DOI] [PubMed] [Google Scholar]
- 7.Khalsa SB. Yoga as a therapeutic intervention: A bibliometric analysis of published research studies. Indian J Physiol Pharmacol. 2004;48:269–84. [PubMed] [Google Scholar]
- 8.Lipton L. Using yoga to treat disease: An evidence-based review. (38, 41).JAAPA. 2008;21:34–36. doi: 10.1097/01720610-200802000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Iyengar BKS. London: Dorling Kindersley; 2008. Yoga: The path to holistic health. [Google Scholar]
- 10.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;12:1–23. [PubMed] [Google Scholar]
- 11.Birdee GS, Legedza A, Saper T, Bertisch SM, Eisenberg DM, Phillips RS. Characteristics of yoga users: Results of a national survey. J Gen Intern Med. 2008;23:1653–8. doi: 10.1007/s11606-008-0735-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen KM, Chen MH, Chao HC, Hung HM, Lin HS, Li CH. Sleep quality, depression state, and health status of older adults after silver yoga exercises: Cluster randomized trial. Int J Nurs Stud. 2009;46:154–63. doi: 10.1016/j.ijnurstu.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 13.DiBenedetto M, Innes KE, Taylor AG, Rodeheaver PF, Boxer JA, Wright HJ, et al. Effect of a gentle Iyengar yoga program on gait in the elderly: An exploratory study. Arch Phys Med Rehabil. 2005;86:1830–7. doi: 10.1016/j.apmr.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 14.Greensdale GA, McDivit A, Carpenter A, Seeger L, Huang MH. Yoga for women with hyperkyphosis: Results of a pilot study. Am J Public Health. 2002;92:1611–4. doi: 10.2105/ajph.92.10.1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kolasinski SL, Garfinkel M, Tsai AG, Matz W, Dyke AV, Schumacher HR. Iyengar yoga for treating symptoms of osteoarthritis of the knees: A pilot study. J Altern Complement Med. 2005;11:689–93. doi: 10.1089/acm.2005.11.689. [DOI] [PubMed] [Google Scholar]
- 16.Manjunath NK, Telles S. Influence of yoga and Ayurveda on self-rated sleep in a geriatric population. Indian J Med Res. 2005;121:683–90. [PubMed] [Google Scholar]
- 17.Oken BS, Zajdel D, Kishiyama S, Flegal K, Dehen C, Haas M, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: Effects on cognition and quality of life. Altern Ther Health Med. 2006;12:40–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Kristal AR, Littman AJ, Benitez D, White E. Yoga practice is associated with attenuated weight gain in healthy, middle-aged men and women. Altern Ther Health Med. 2005;11:28–33. [PubMed] [Google Scholar]
- 19.Bertisch SM, Wee CC, McCarthy EP. Use of complementary and alternative therapies by overweight and obese adults. Obesity (Silver Spring) 2008;16:1610–5. doi: 10.1038/oby.2008.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nagarathna R, Nagendra HR. Yoga for bronchial asthma: A controlled study. Br Med J (Clin Res Ed) 1985;291:1077–9. doi: 10.1136/bmj.291.6502.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nagendra HR, Nagarathna R. An integrated approach of yoga therapy for bronchial asthma: A 3-54-month prospective study. J Asthma. 1986;23:123–37. doi: 10.3109/02770908609077486. [DOI] [PubMed] [Google Scholar]
- 22.Gould KL, Ornish D, Scherwitz L, Brown S, Edens RP, Hess MJ, et al. Changes in myocardial perfusion abnormalities by positron emission tomorography after long-term, intense risk factor modification. JAMA. 1995;274:894–901. doi: 10.1001/jama.1995.03530110056036. [DOI] [PubMed] [Google Scholar]
- 23.Jain SC, Uppal A, Bhatnagar SO, Talukdar B. A study of response pattern of non-insulin dependent diabetics to yoga therapy. Diabetes Res Clin Pract. 1993;19:69–74. doi: 10.1016/0168-8227(93)90146-v. [DOI] [PubMed] [Google Scholar]
- 24.Monro RE, Power J, Coumar A, Nagarathna R, Dandona P. Yoga therapy for NIDDM. Complement Med Res. 1992;6:66–88. [Google Scholar]
- 25.Shannahoff-Khalsa DS, Beckett IR. Clinical case report: Efficacy of yogic techniques in the treatment of obsessive-compulsive disorders. Int J Neurosci. 1996;85:1–17. doi: 10.3109/00207459608986347. [DOI] [PubMed] [Google Scholar]
- 26.Finley R. SurveyMonkey. [Last accessed on 2009, Dec 30]. Available from: http://www.surveymonkey.com .
- 27.Hu FB, Rimm E, Smith-Warner SA, Feskanich D, Stampfer MJ, Ascherio A, et al. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr. 1999;69:243–9. doi: 10.1093/ajcn/69.2.243. [DOI] [PubMed] [Google Scholar]
- 28.Jacobs DR, Jr, Meyer KA, Kushi LH, Folsom AR. Whole-grain intake may reduce the risk of ischemic heart disease death in postmenopausal women: The Iowa Women's Health Study. Am J Clin Nutr. 1998;68:248–57. doi: 10.1093/ajcn/68.2.248. [DOI] [PubMed] [Google Scholar]
- 29.Jacobs DR, Jr, Meyer KA, Kushi LH, Folsom AR. Is whole grain intake associated with reduced total and cause-specific death rates in older women? The Iowa Women's Health Study. Am J Public Health. 1999;89:322–9. doi: 10.2105/ajph.89.3.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jacobs DR, Jr, Pereira MA, Meyer KA, Kushi LH. Fiber from whole grains, but not refined grains, is inversely associated with all-cause mortality in older women: The Iowa Women's Health Study. J Am Coll Nutr. 2000;19:326S–30S. doi: 10.1080/07315724.2000.10718968. [DOI] [PubMed] [Google Scholar]
- 31.Jewett SP. Longevity and the longevity syndrome. Gerontologist. 1973;13:91–9. [Google Scholar]
- 32.Daubenmier J. The relationship of yoga, body awareness, and body responsiveness to self-objectification and disordered eating. Psychol Women Q. 2005;29:207–19. [Google Scholar]
- 33.Schiffman E. New York: Simon and Schuster; 1996. Yoga: The spirit and practice of moving into stillness. [Google Scholar]
- 34.Jayasinghe SR. Yoga in cardiac health (a review) Eur J Cardiovasc Prev Rehabil. 2004;11:369–75. doi: 10.1097/01.hjr.0000206329.26038.cc. [DOI] [PubMed] [Google Scholar]
- 35.Aljasir B, Bryson M, Al-Shehri B. Yoga practice for the management of type II diabetes mellitus in adults: A systematic review. Evid Based Complement Alternat Med. 2010;7:399–408. doi: 10.1093/ecam/nen027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Innes KE, Vincent HK. The influence of yoga-based programs on risk profiles in adults with type 2 diabetes mellitus: A systematic review. Evid Based Complement Alternat Med. 2007;4:469–86. doi: 10.1093/ecam/nel103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morine NE, Greco CM. Mind-body interventions for chronic pain in older adults: A structured review. Pain Med. 2007;8:359–75. doi: 10.1111/j.1526-4637.2007.00312.x. [DOI] [PubMed] [Google Scholar]
- 38.Kirkwood G, Rampes H, Tuffrey V, Richardson J, Pilkington K. Yoga for anxiety: A systematic review of the research evidence. Br J Sports Med. 2005;39:884–91. doi: 10.1136/bjsm.2005.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Uebelacker LA, Epstein-Lubow G, Gaudiano BA, Tremont G, Battle CL, Miller IW. Hatha yoga for depression: Critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. J Psychiatr Pract. 2010;16:22–33. doi: 10.1097/01.pra.0000367775.88388.96. [DOI] [PubMed] [Google Scholar]
- 40.Dusek JA, Otu HH, Wolhueter AL, Bhasin M, Zerbini LF, Joseph MG, et al. Genomic counter-stress changes induced by the relaxation response. PLoS One. 2008;3:e2576. doi: 10.1371/journal.pone.0002576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lazar SW, Kerr CE, Wasserman RH, Gray JR, Greve DN, Treadway MT, et al. Meditation experience is associated with increased cortical thickness. Neuroreport. 2005;16:1893–7. doi: 10.1097/01.wnr.0000186598.66243.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heaney RP. Long-latency deficiency disease: Insights from calcium and vitamin D. Am J Clin Nutr. 2003;78:912–9. doi: 10.1093/ajcn/78.5.912. [DOI] [PubMed] [Google Scholar]
- 43.Seligman ME. The effectiveness of psychotherapy: The Consumer Reports study. Am Psychol. 1995;50:965–74. doi: 10.1037//0003-066x.50.12.965. [DOI] [PubMed] [Google Scholar]
- 44.Bell IR, Koithan M. Models for the study of whole systems. Integr Cancer Ther. 2006;5:293–307. doi: 10.1177/1534735406295293. [DOI] [PubMed] [Google Scholar]
- 45.Capra F. New York: Doubleday; 1996. The web of life: A new scientific understanding of living systems. [Google Scholar]
- 46.Quinn JF, Smith M, Ritenbaugh C, Swanson K, Watson MJ. Research guidelines for assessing the impact of the healing relationship in clinical nursing. Altern Ther Health Med. 2003;9(Supplement 3):A65–79. [PubMed] [Google Scholar]
- 47.Ligthelm RJ, Borzi V, Gumprecht J, Kawamori R, Wenying Y, Valensi P. Importance of observational studies in clinical practice. Clin Ther. 2007;29:1284–92. [PubMed] [Google Scholar]
- 48.Forbes B. Yoga and managed care: A cautionary tale. Int J Yoga Therapy. 2010;20:22–5. [Google Scholar]
- 49.Laurence S. The role of outcome-based standards in Yoga therapy. Int J Yoga Therapy. 2010;20:42–51. [Google Scholar]
- 50.Lavey R, Sherman T, Mueser KT, Osborne DD, Currier M, Wolfe R. The effects of yoga on mood in psychiatric inpatients. Psychiatr Rehabil J. 2005;28:399–402. doi: 10.2975/28.2005.399.402. [DOI] [PubMed] [Google Scholar]
- 51.Streeter CC, Jesens JE, Perlmutter RM, Cabral HJ, Tian H, Terhune DB, et al. Yoga asana sessions increase brain GABA levels: A pilot study. J Altern Complement Med. 2007;13:419–26. doi: 10.1089/acm.2007.6338. [DOI] [PubMed] [Google Scholar]
- 52.Woolery A, Myers H, Sternlieb B, Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Altern Ther Health Med. 2004;10:60–3. [PubMed] [Google Scholar]


