Abstract
Due to increased survival among hemodialysis (HD) patients, new problems including concerns of oral health have appeared. In this study, we aimed to evaluate the oral health status and related risk factors in Iranian HD patients. Demographic information, medical history, laboratory findings, and dental health status were gathered. The decayed, missing and filled teeth (DMFT) index in accordance with the World Health Organization (WHO) criteria was obtained. Kt/V was calculated for patients. A P-value of <0.05 was considered statistically significant. Seventy-two patients were evaluated, with a mean age and HD time of 53.4±15.3 years and 36.9±33.8 months, respectively. Thirty-five (48.6%) complained of dry mouth, 33 (49.3%) of taste change, 22 (31%) of malodor mouth, and 30 (46.9%) had dental calculus. The overall mean DMFT score was 18.6±9.9. DMFT score had a negative significant correlation with Kt/V (r=–0.4, P=0.004). Women and singles as well as patients with a low educational level and/or lesser dialysis time had a significantly higher DMFT score (P<0.05). Kt/V was significantly lower in patients suffering from dry mouth and dental calculus (P<0.05). Interestingly DMFT score was significantly lower in patients with dental calculus compared to patients without it (P=0.001). It seems that our patients have a poor dental hygiene level and high DMFT score especially women, singles, patients with low Kt/V and a low education level. The oral health maintenance program for a patient receiving dialysis should be reinforced in our centers.
Keywords: Dental health, DMF, hemodialysis, Iranian patients
Introduction
Due to advances in the treatment of chronic renal failure (CRF) during the last two decades, survival of patients on dialysis has increased. But new problems including concerns of oral health have occurred.[1–4] The common oral health problems are dry mouth, uremic odor, change in taste, dental calculus, low salivary flow rate, and dental caries.[3,5–7] These manifestations may be related to a variety of factors, such as a relative state of immune suppression, medications, restriction of oral fluid intake, poor oral hygiene, malnutrition, and mouth breathing.[4,8] For the evaluation of the hemodialysis (HD) effect on oral and dental health status, it is important to know the oral health status in patients with good dialysis adequacy (Kt/V) compared with poor dialysis adequacy. Kt/V has been criticized as an accepted method for dialysis adequacy measurement.[9] HD patients as well as related dentists and nephrologists should be aware of oral health care in this condition. Poor oral care in this group, especially those who are candidates of kidney transplant, could expose the patients to a high risk of serious problems. We aimed to determine dental and oral health status of our HD patients and related risk factors.
Materials and Methods
Subjects
This is an observational, cross-sectional study based on data collected from HD patients treated at two different dialysis centers of Shiraz University of Medical Sciences in Fars province, southern Iran. Seventy-two patients (age ranged from 18 to 85 years) under HD for more than 3 months were randomly selected. The study protocol was approved by the local ethics committee. Informed written consent was obtained from all patients.
Study protocol
The patients were dialyzed for 4 h using Fresenius 4008B machines. For each patient, a four-part questionnaire was completed by the researchers. This form consisted of demographic information, medical history, laboratory findings (gathered from medical records), and dental and oral health status (such as frequency of the brushing, visiting a dentist, time of the last dentist visit, experiencing a sensation of dry mouth, bad taste, or malodor mouth). Intraoral examination was also done by two trainee dentists with a mouth mirror and light at bedside while the patients attended the HD. The DMFT index was obtained as the sum of decay (D), missing (M), and filled (F) teeth in accordance with the criterion suggested by WHO.[10] Kt/V has been criticized as an accepted method for dialysis adequacy measurement that was calculated from the Daugirdas formula {–ln(R–0.03) + [(4–3.5R) × (UF÷W)]}.[9] The target of dialysis adequacy, which was based upon the K/DOQI Clinical Practice Guidelines, was Kt/V ≥ 1.2.[11]
Statistical analysis
Data were analyzed by Statistical Package for the Social Sciences software version 15.0 (SPSS Inc. Chicago, IL, USA). Comparison of the quantitative data was made using the Student t-test or Mann–Whitney and Kruskal–Wallis tests as nonparametric tests. Correlation between quantitative data was determined by Pearson's correlation coefficient. A chi-square test was performed for the comparison of the qualitative data. A P-value of < 0.05 was considered statistically significant.
Results
A total of 72 adult HD patients were evaluated, 48 men (66.7%) and 24 women (33.3%) with a mean age of 53.4±15.3 years; the mean of HD time and Kt/V was 36.9±33.8 months and 1.4±0.6, respectively. Table 1 summarizes the distributions, mean values, standard deviations, DMFT score regarding categorical groups, statistical tests, and significance of patient's variables. The distribution of some oral health variables is shown in Table 2. The mean of the DMFT score was 18.6±9.9. Of 72 patients, 35 (48.6%) complained of dry mouth, 33 (49.3%) of taste change, 22 (31%) of malodor mouth, and 30 (46.9%) had some degree of dental calculus. These patients had a higher DMFT score than those who had not complaints of any sign and/or symptom (P=0.04).
Table 1.
Levels of Demographic data of study subjects
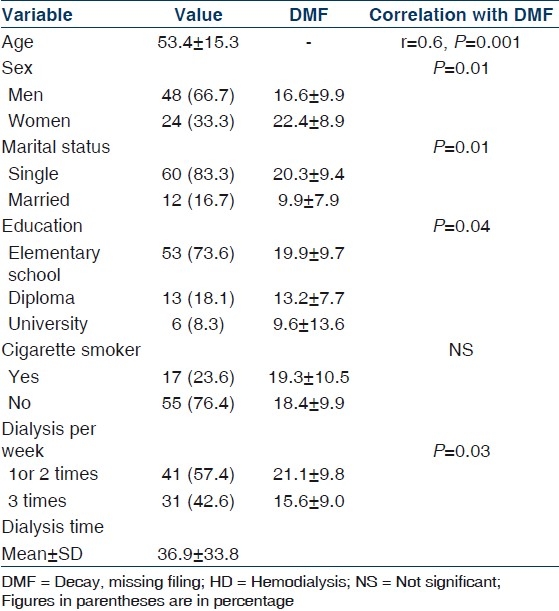
Table 2.
Distribution of dental and oral signs or symptoms among HD patients
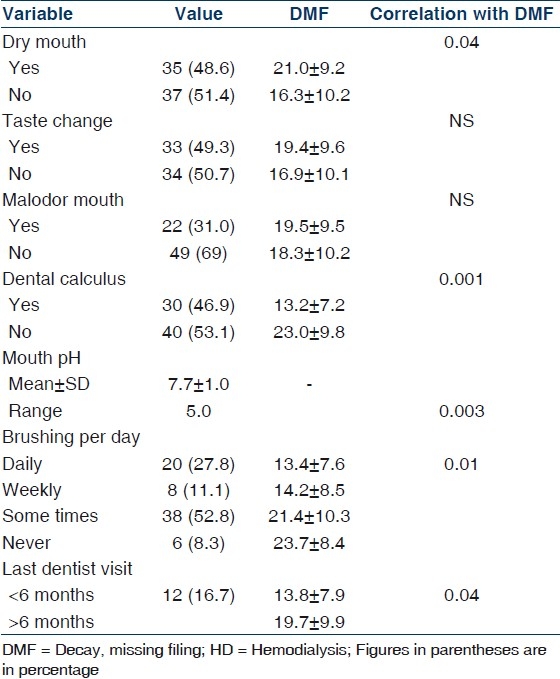
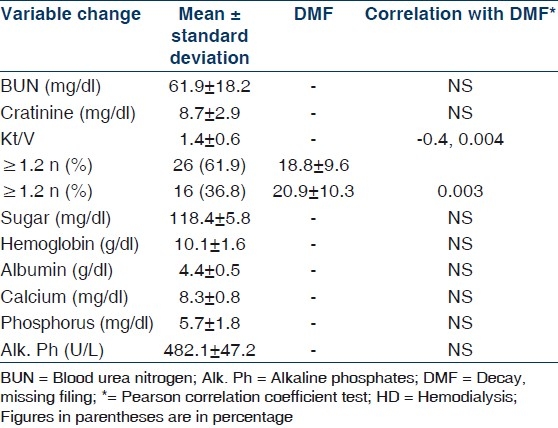
Women, singles, and those with low Kt/V, low educational level, and lesser dialysis time had a significantly higher DMFT score (P<0.05); the DMFT score was significantly different by gender (16.6±9.9 in men vs. 22.4±8.9 in women; P=0.01), marital status (20.3±9.4 in singles vs. 9.9±7.9 in married; P=0.01), educational level (P=0.04; Table 1), dialysis time per week (21.1±98 in those who had dialysis three times per week vs. 15.6±9 in those who had dialysis less than three times; P=0.03), and dialysis adequacy (20.9±10.3 in those had Kt/V < 1.2 vs. 18.8±9.6 in others, P=0.003). The DMFT score was lower in those who had dental calculus than patients without dental calculus (13.2±7.2 vs. 23.0±9.8; P=0.001).
Kt/V was significantly lower among those who had dry mouth (1.0±0.6 vs. 1.8±0.4; P=0.04) and dental calculus (1.1±0.5 vs. 1.7±0.4; P=0.01). Kt/V was lower in patients who had bad taste and malodor than who had not, but it was not significant (P=0.07 and P=0.40, respectively).
There was a positive significant correlation between the DMFT score and age (r=0.6, P=0.001). But no statistically significant correlation was seen between DMFT-score and HD time (r=0.2, P=0.07). Kt/V and DMF-T score had a negative significant correlation (r=–0.4, P=0.004).
Only 20 (27.8%) of the HD patients brushed their teeth daily and 6 (8.3%) said that they never brush their teeth [Table 2]. None of the patients in the study group had a routine dental check-up and all of them reported that they went for a dental visit only when they had a dental problem. Only 12 (16.7%) patients visited a dentist in the past 6 months due to their dental problems.
The biochemical data of our HD patients are presented in Table 3. They had no statistically significant correlation with the DMFT-score.
Table 3.
Distribution and significance levels of biochemical data among HD patients
Discussion
More than 30 oral signs and symptoms have been reported in dialysis patients.[12] Majority of our patients showed oral sign and/or symptoms. In agreement with some studies,[2,4,12,13] in most cases they were taste change, dry mouth, malodor , and dental calculus. Dry mouth in HD patients can be caused by uremic involvement of the salivary glands and dehydration due to the restriction of fluid intake,[12] also use of mouth washes containing alcohol,[4] adverse effects of drug therapy, or mouth breathing.[2] Bad taste is caused by xerostomia and the presence of urease-splitting oral organisms, which metabolize urea and elaborate ammonia.[4] The uremic fetor, an ammoniacal odor, is typical of uremic patients and is caused by a high concentration of urea in the saliva.[12,13]
Results from the present study showed that the DMFT score in HD patients was 18.6±9.9. It is similar to the results of Marinho et al. who reported the DMFT score as 17.1±7.8 compared to 15.23±7.07 in the controls.[3] In the Netherlands, the DMFT score was 13.3±7.5 in adult HD patients.[14] In Kerman, Iran, the DMFT score did not differ significantly compared with the control group.[15] Similar to the previous reports,[2] the DMFT score increases with age. There are different reports regarding the DMFT score in HD patients compared with the general population.[14,16] In this research, we did not have a control group for comparison and it was a limitation in our study, but the DMFT score in our HD patients was higher than the reported DMFT scores in the controls of some studies in the literature including Kalsbeek et al.[17] who reported a score of 14.7±6.4 in 808 dentate subjects (aged 25–54 years), Brito et al.[18] who showed a DMFT score of 13.9 in 74 healthy subjects (mean age 40.3±12.9), and Marinho et al.[3] who determined a score of 15.23±7.07 in 64 controls (mean age 60±11 years). However, we could not have a precise statistical analysis to test the significance of these observed differences due to confounding variables, especially age, sex, and educational level, not matching.
In our study, DMFT was higher in those with inadequate dialysis. The high prevalence of calculus in our study is in agreement with other studies.[1,5,14] These results could be caused by a poor oral hygiene level among HD patients probably resulted from the low socioeconomic status of patients. An altered serum phosphorus–calcium balance might be responsible with increased calculus deposition resulting from changes in salivary composition as well.[4]
Subjects with a higher calculus formation had a lower DMFT score. It could be related to a possible antibacterial effect of urea or increased calculus.[4] In agreement with the same study,[4] our patients reported brushing infrequently and also none of them had ever had a routine dental check-up. This may be related to loss of motivation, low socioeconomic status, and high cost of dental care services. Our patients had poor dental hygiene and a high DMFT score, especially women, singles, those with low dialysis adequacy, and with a low educational level. These results would imply further emphasis on the effective implementation of an oral health promotion program. The oral health maintenance plan for patients receiving dialysis should be reinforced by the dialysis team and dentists. HD patients should be given initial oral examinations and frequent follow-ups. Further studies regarding the comparison of the DMFT score of HD patients and general population are needed.
Our study was limited by study setting; intraoral examination was done only at bedside. Because of not using probing and radiography, the number of decayed teeth reported in our study could have been underestimated. Lack of control group was another limitation in our study. Also we did not have the status of dentition and oral hygiene prior to the HD for the detection of the actual severity of oral hygiene and DMFT during the HD.
Conclusion
This health situation analysis showed that dental care of dialysis patients in our center is neglected. This lack of care may put them at a high risk of serious problems. The awareness of oral care should be raised among dialysis patients, their nephrologists, and dentists in our centers.
Acknowledgments
This study was funded by Nephro-Urology Research Center of Shiraz University of Medical Sciences.
Footnotes
Source of Support: Nephro-Urology Research Center of Shiraz University of Medical Sciences
Conflict of Interest: None declared.
References
- 1.Bayraktar G, Kurtulus I, Duraduryan A, Cintan S, Kazancioglu R, Yildiz A, et al. Dental and periodontal findings in hemodialysis patients. Oral Dis. 2007;13:393–7. doi: 10.1111/j.1601-0825.2006.01297.x. [DOI] [PubMed] [Google Scholar]
- 2.Ertuğrul F, Elbek-Cubukçu C, Sabah E, Mir S. The oral health status of children undergoing hemodialysis treatment. Turk J Pediatr. 2003;45:108–13. [PubMed] [Google Scholar]
- 3.Sobrado Marinho JS, Tomás Carmona I, Loureiro A, Limeres Posse J, García Caballero L, Diz Dios P. Oral health status in patients with moderate-severe and terminal renal failure. Med Oral Patol Oral Cir Bucal. 2007;12:305–10. [PubMed] [Google Scholar]
- 4.Klassen JT, Krasko BM. The dental health status of dialysis patients. J Can Dent Assoc. 2002;68:34–8. [PubMed] [Google Scholar]
- 5.Martins C, Siqueira WL, Guimarães Primo LS. Oral and salivary flow characteristics of a group of Brazilian children and adolescents with chronic renal failure. Pediatr Nephrol. 2008;23:619–24. doi: 10.1007/s00467-007-0718-5. [DOI] [PubMed] [Google Scholar]
- 6.Castillo A, Mesa F, Liébana J, García-Martinez O, Ruiz S, García-Valdecasas J. Periodontal and oral microbiological status of an adult population undergoing haemodialysis: a cross-sectional study. Oral Dis. 2007;13:198–205. doi: 10.1111/j.1601-0825.2006.01267.x. [DOI] [PubMed] [Google Scholar]
- 7.Nakhjavani YB, Bayramy A. The dental and oral status of children with chronic renal failure. J Indian Soc Pedod Prev Dent. 2007;25:7–9. doi: 10.4103/0970-4388.31981. [DOI] [PubMed] [Google Scholar]
- 8.Proctor R, Kumar N, Stein A, Moles D, Porter S. Oral and dental aspects of chronic renal failure. J Dent Res. 2005;84:199–208. doi: 10.1177/154405910508400301. [DOI] [PubMed] [Google Scholar]
- 9.Winchester JF, Harbord N, Audia P, Dubrow A, Gruber S, Feinfeld D, et al. The 2006 KDOQI Guidelines for Peritoneal Dialysis Adequacy Are Not Adequate. Blood Purif. 2007;25:103–5. doi: 10.1159/000096405. [DOI] [PubMed] [Google Scholar]
- 10.Oral health survey, basic methods. 3rd ed. Geneva: World Health Organization; 1987. World Health Organization. [Google Scholar]
- 11.Foundation NK. Kidney Disease Outcomes Quality Initiative (K/DOQI) [cited in 2005]. Available from: http://www.kidney.org/professionals/doqi .
- 12.Kho HS, Lee SW, Chung SC, Kim YK. Oral manifestations and salivary flow rate, pH, and buffer capacity in patients with end-stage renal disease undergoing hemodialysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:316–9. doi: 10.1016/s1079-2104(99)70035-1. [DOI] [PubMed] [Google Scholar]
- 13.Chuang SF, Sung JM, Kuo SC, Huang JJ, Lee SY. Oral and dental manifestations in diabetic and nondiabetic uremic patients receiving hemodialysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:689–95. doi: 10.1016/j.tripleo.2004.06.078. [DOI] [PubMed] [Google Scholar]
- 14.Bots CP, Poorterman JH, Brand HS, Kalsbeek H, van Amerongen BM, Veerman EC, et al. The oral health status of dentate patients with chronic renal failure undergoing dialysis therapy. Oral Dis. 2006;12:176–80. doi: 10.1111/j.1601-0825.2005.01183.x. [DOI] [PubMed] [Google Scholar]
- 15.Chamani G, Zarei MR, Radvar M, Rashidfarrokhi F, Razazpour F. Oral health status of dialysis patients based on their renal dialysis history in Kerman, Iran. Oral Health Prev Dent. 2009;7:269–75. [PubMed] [Google Scholar]
- 16.Gavaldá C, Bagán J, Scully C, Silvestre F, Milián M, Jiménez Y. Renal hemodialysis patients: Oral, salivary, dental, and periodontal findings in 105 adult cases. Oral Dis. 1999;5:299–302. doi: 10.1111/j.1601-0825.1999.tb00093.x. [DOI] [PubMed] [Google Scholar]
- 17.Kalsbeek H, Poorterman JHG, Kivit MM. Tandheelkundige Verzorging Volwassen Ziekenfondsverzekerden 1995–2002. Leiden, The Netherlands: TNO Preventie en Gezondheid, rapport:2003 PG/JGD/03.219 [Google Scholar]
- 18.Brito F, de Barros FC, Zaltman C, Carvalho AT, Carneiro AJ, Fischer RG, et al. Prevalence of periodontitis and DMFT index in patients with Crohn's disease and ulcerative colitis. J Clin Periodontol. 2008;35:555–60. doi: 10.1111/j.1600-051X.2008.01231.x. [DOI] [PubMed] [Google Scholar]


