Abstract
Background & objectives:
Three countries, Bangladesh, India and Nepal, set out to eliminate kala-azar by 2015. This study was aimed to document the knowledge and practices in kala-azar case management of public and private health providers in these three countries.
Methods:
A health care provider survey was conducted in 2007 at 4 study sites, viz., Muzaffarpur and Vaishali districts in India, Mahottari district in Nepal, and Rajshahi district in Bangladesh. Interviews were conducted with formal and informal health care providers at their home or practice.
Results:
About half of the providers in India and Nepal knew the rapid diagnostic test rK39 recommended by the elimination initiative, but this was not in Bangladesh. Knowledge of the recommended first-line drug, miltefosine, was good in India and Nepal but less so in Bangladesh.
Interpretation & conclusions:
Innovative tools for VL care have not yet been fully taken up by private for profit care providers in the three countries that launched a VL elimination initiative. The elimination initiative needs to address these gaps in private providers’ knowledge, given their substantial share in the care of VL patients.
Keywords: Bangladesh, control, elimination, India, Nepal, provider survey, visceral leishmaniasis
Sixty per cent of the world's cases of visceral leishmaniasis (VL) or kala-azar occur in a well-defined area in North-east India (mainly in Bihar State, extending to Jharkand and West Bengal), and in adjacent regions in Nepal and Bangladesh. The World Health Organization estimates that the annual number of cases in this region is about 100,0001. Epidemiological surveillance figures in the region-based on patients reporting to the public sector only, are considered an underestimate of the true number of VL cases with a factor up to 82.
In 2005 the governments of India, Bangladesh and Nepal decided to eliminate VL by 2015. Elimination of this anthroponotic disease is deemed achievable because technological innovation has paved the way: a rapid diagnostic test, rK39, and an oral drug, miltefosin, are now available3. Accordingly to Murray “the real obstacle now, almost entirely a matter of cost, is proper translation, distribution, and expansion of the advances that have been made so that they can have an effect in the field and save lives”4. While this emphasis on budget allocation is correct, one should not underestimate the need for proper translation of technical advances to the local context. A correct analysis of the health system challenges will be critical to the elimination target, as VL control hinges for a major part on early case detection and treatment5. Therefore, TDR/WHO initiated a number of studies to examine the community and health services perspective on this disease, as part of its support to the elimination initiative.
While several investigators have addressed the community perception of kala-azar6–8 only a few have analysed that of the health care providers. Ahluwalia et al6 pointed to the huge challenge health professionals faced in Bangladesh when specific kala-azar drugs were no longer available in that country. Sundar et al9 showed a clear need to revise control approaches if early and more exhaustive case detection is to be achieved. Passively waiting in poorly attended public health clinics will not bring disease spread to a halt. There is a need for a much more active approach, and it will need to consider the available human resources that could potentially be mobilized for the effort.
The objectives of this study were to assess kala-azar related knowledge and practices of health providers practicing in the endemic areas in the three countries, India, Bangladesh and Nepal.
Material & Methods
This multi-country study was conducted in 2007 to assess the knowledge and practice in kala-azar management of health care providers working in endemic areas in Bangladesh, India, and Nepal, the region presently targeted by the kala-azar elimination initiative. This region is far from homogeneous, and the epidemiological picture of the disease varies substantially across the countries and even within countries. VL foci in Muzaffarpur district in India report very high kala-azar incidence rates, approximating 1 per cent per year2. Vaishali district in India, Rajshahi in Bangladesh and Mahottari district in Nepal report lower incidence rates in the realm of 1 to 2 per 1000 per year9, though the difference might be due to the level of aggregation of the data. Also, the health systems vary substantially. In India, patients will preferentially consult private practitioners or one of the not-for-profit private clinics in Muzaffarpur town specializing in kala-azar treatment. In Nepal, kala-azar care is fairly well available in the public health services, at primary as well as secondary level10. In Bangladesh in 2007 the situation was characterized by a dramatic shortage of antileishmanial drugs and diagnostics at all levels of the public health service.
Sampling approach: We purposefully selected the 4 study sites in Muzaffarpur and Vaishali districts in India (about 31,800 population each), in Mahottari district in Nepal (17,241 population) and Rajshahi district in Bangladesh (25,470 population) to maximally reflect the regional heterogeneity. Health care providers working in the study area were identified through several sources; for the formal sector existing lists were used, while providers in the informal sector were identified during an exhaustive household survey in the area10 and by snowballing techniques11. The aim was to select a purposive sample of 100 health care providers from these lists in each study site, including approximately equal numbers of providers practicing modern allopathic medicine, those practicing other systems of medicine, and those without medical degree (paramedicals and others).
Data collection: Current and retrospective data were collected cross-sectionally using the same semi-structured and pre-tested questionnaires at each of the four sites. Information regarding provider characteristics, number of VL cases treated, their knowledge and their actual practice in the field of diagnosis, treatment and referral of kala-azar cases was collected. The interviewers were trained before the survey in order to ensure uniform data collection practices.
Categories of health care providers: In India, the formal public health system includes the facilities established under the ‘Indian System of Medicine’ such as Ayurveda, Unani and Homeopathy. For the purpose of this study, health care providers in the three countries were categorized as ‘formal’ if they had a recognized medical or para-medical degree. This included allopathic doctors employed in government health services as well as those working in private institutions or in own private practice and those formally trained in indigenous medical systems (Ayurveda or others). All unqualified care providers were categorized as ‘informal’, including traditional healers as herbalists and faith healers , but also local chemists and the so-called “jhola chap doctors” or “quacks”. A Jhola chap doctor (medical salesman with shoulder bag) is an untrained and unlicensed medicine seller offering mainly curative services on an ambulatory basis.
Ethical aspects: Ethical approval was obtained from the respective institutions (Rajendra Memorial Research Institute, Patna, India; Banaras Hindu University, Varanasi, India; International Centre of Diarrhoeal Disease Research in Dhaka, Bangladesh; Institute of Medicine, Tribhuvan University, Kathmandu, Nepal) as well as from the Ethical Review Committee, WHO/TDR, Geneva, Switzerland.
Data analysis: Data were entered into Epi Info and analyzed using SPSS V.16.0. Continuous variables were summarized by means and medians as appropriate. Means were compared with t-tests, medians with the non-parametric Mann-Whitney test. Proportions were compared with Pearson's Chi-square without continuity correction.
Results
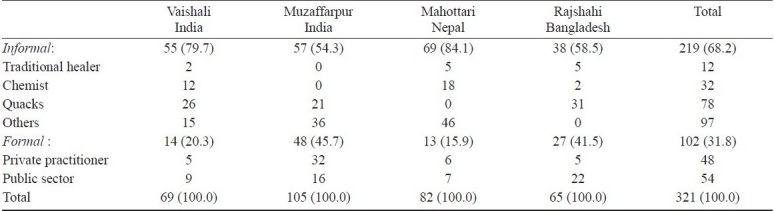
Table I shows the numbers of health care providers in each category; 219 providers from the informal sector and 102 from the formal sector were interviewed. Most informal healers were indigenous healers or so-called “quacks” (i.e., untrained members of the community practicing health care). The major proportion of ‘others’ in the Indian and Nepali sample of informal providers mainly reflects a high number of nurses delivering curative care on a for-profit basis. Roughly half of the formal providers belonged to the private and the other half to the public sector.
Table I.
Number (%) and category of health care providers enrolled in the study
Overall, 82.6 per cent of providers were male, 91.3 per cent in Vaishali, 68.5 per cent in Muzaffarpur, 87.8 per cent in Nepal and 89.2 per cent in Bangladesh. There was no significant difference in sex between formal and informal providers in Vaishali, India and Nepal sites compared to a significantly higher proportion of male formal sector providers in Muzaffarpur, India (P<0.001) and informal sector male providers in Bangladesh (P<0.05). The mean age of providers was 42.5 ± 10.1; 44.6 ± 10.62 in Vaishali, 43.9 ± 9.79 in Muzaffarpur, 38.1 ± 8.15 in Nepal and 42.8 ± 10.98 yr in Bangladesh. The formal health care providers were on average 5 yr older than those of the informal sector, mean 45.9 vs 40.9 yr (P<0.001). The majority of the respondents had no formal qualifications, and their mean experience in the job was 13.4 ± 11.0 yr in Vaishali, 17.5 ± 8.5 in Muzaffarpur, 11.1 ± 6.9 in Nepal and 16.1 ± 9.4 yr in Bangladesh. The mean duration of experience was slightly but not significantly longer in the formal (15.5 yr) compared to the informal sector (14.5 yr).
The absolute number of cases seen in the past year per provider ranged from 0 to 500, with the median number of kala-azar cases seen per provider varying from 1 in Bangladesh, to 2 in Vaishali, India and Nepal and 100 Muzaffarpur, India. Formal providers had seen a significantly higher number of kala-azar cases in the past year than informal providers, with a median of 6 cases versus 3 in the latter group, (P=0.003; Mann-Whitney).
Providers seemed well acquainted with the symptoms of VL, with 76.8 to 100.0 per cent correctly indicating fever as the main symptom and splenomegaly evoked by close to 90 per cent of providers in all countries, except for Bangladesh (52.3%). Bangladesh providers insisted on the darkening of skin as one of the main symptoms. There was no significant difference in the frequency with which the formal and informal providers evoked fever as a kala-azar symptom, 89.3 versus 94.0 per cent, whereas a significantly higher percentage of formal providers evoked splenomegaly as a sign, 79.6 vs. 63.8 per cent of informal providers, P=0.004.
Table II shows the providers’ knowledge and practice related to kala-azar diagnosis. About 70 per cent of Bangladesh providers established their diagnosis on purely clinical grounds, without any laboratory test, contrasting to only 11.6, 5.7, 9.7 per cent who did so respectively in Vaishali, Muzaffarpur and Nepal (P<0.001).
Table II.
Provider's knowledge and practice (%) related to kala-azar diagnosis
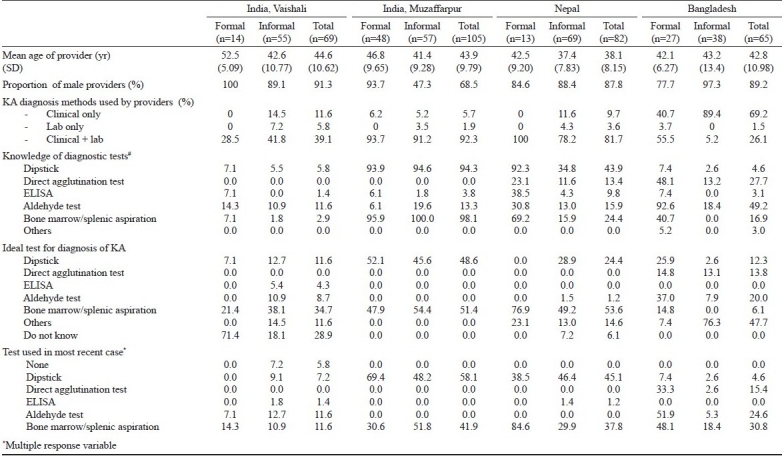
Parasitological techniques as spleen biopsy and bone marrow aspirates were considered as the preferred test for kala-azar by 39.25 per cent of providers, with 34.7 per cent in Vaishali, 51.4 per cent in Muzaffarpur, 53.6 per cent in Nepal and 6.1 per cent in Bangladesh. The immunochromatographic test rK39 (or rK39 strip test) was deemed the best test by 27.1 per cent of providers: 11.6 per cent in Vaishali, 48.6 per cent in Muzaffarpur, 24.4 per cent in Nepal and 12.3 per cent in Bangladesh, respectively. The most recent case was diagnosed by a rK39 strip test in 7.2 per cent of providers in Vaishali, 58.1 per cent in Muzaffarpur, 45.1 per cent in Nepal and 4.6 per cent in Bangladesh. Overall, 39.8 per cent of formal providers used the rK39 strip test in the most recent diagnosis against 29.8 per cent of informal providers (P<0.001).
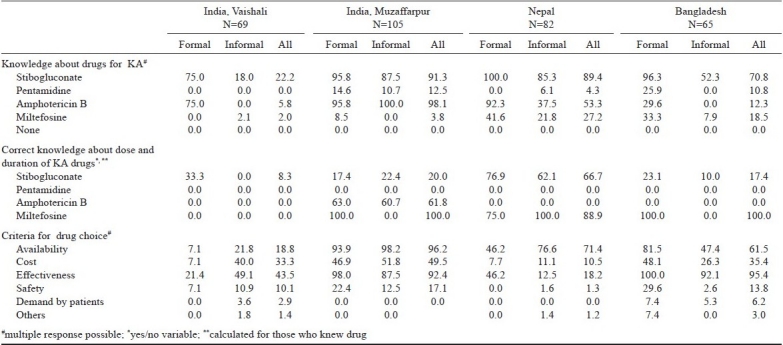
Table III shows the providers’ knowledge and practice related to kala-azar treatment. Knowledge of drugs varied strikingly. Miltefosin was known by 2.0 per cent of providers in Vaishali, 27.2 per cent in Muzaffarpur, 27.2 per cent in Nepal and 18.5 per cent in Bangladesh. The main criteria for drug choice evoked by providers were the drug's availability (66.1%) and its effectiveness (64.2%). Cost was an important determinant for drug choice in India and Bangladesh, and was cited by 35 to 50 per cent of providers, but less frequently in Nepal (10.5%), where the government was providing anti-VL drugs for free in the public sector.
Table III.
Provider's knowledge and practices related to kala-azar treatment (%)
Discussion
This multi-country study of health providers’ knowledge and practice reflects the differences in disease burden and health system organization of the three countries. The high number of VL cases seen by providers in Muzaffarpur, India is consistent with the higher incidence of kala-azar in this country compared to Nepal12.
Provider knowledge on the newer tests and drugs was good in Muzaffarpur, in India, the epicentre of the current epidemic, and was much better than in the three other study sites. Given the major shortage of antileishmanial drugs and diagnostics in Bangladesh at the time of the study, it was not surprising that the providers there hardly knew any of these therapeutic innovations. The samples of providers were purposefully selected, and one should be cautious in comparing the data across countries, as the composition of these samples varied. Nonetheless, because of the built-in stratification we believe that the findings are fairly reflecting the spectrum of health provider practice in the region. Though it is hard to find any comparative data in the literature, the observed differences between countries are plausible given the contrasting epidemiological and health service context.
Qualitative research on kala-azar so far concentrated on the community perspective on the disease, usually showing a high level of awareness in areas with sustained epidemics. In Bihar, India, 97 per cent of the respondents in Kanti block, the epicentre of the ongoing epidemic, were aware of the disease, 84 per cent could cite at least one symptom and 85 per cent knew it was a vector born disease8. The disease was perceived as more serious than malaria. Ahluwalia et al6 documented high awareness about kala-azar in a Bangladeshi community with an incidence rate of 2 per cent per year and 19 per cent case fatality amongst women, with rather good knowledge about disease causation. The demand for proper treatment and prevention of kala-azar was very high. In Nepal, Koirala et al7 found somewhat lower awareness about the disease, its causes and management in communities in Morang district, in a relatively recent outbreak. A recent multi-country study showed high awareness about the disease, with a high number of respondents in India (98%), Bangladesh (91%) and Nepal (82%) having heard about kala-azar. Fever as the leading symptom was identified by 92 per cent of interviewees in India, 72 per cent in Nepal, but only 30 per cent in Bangladesh. Likewise the knowledge about mosquitoes transmitting the disease was frequent in India (71%) and Nepal (88%) but almost absent in Bangladesh (21%)10. These data from qualitative research seem to indicate that the community awareness of the disease as well as the demand for treatment are high in those areas that are seriously afflicted by it, most likely because of its serious health and economic consequences. More detailed knowledge about transmission routes may be lower in areas that are relatively underserved or where the outbreak is of recent origin. Many authors also emphasized the lack of access to proper VL care, in part due to huge economic barriers6,8,13,14.
In India, Singh et al8 showed how private providers were the first choice for seeking care for kala-azar, only a minority of community respondents indicated the governmental health services as their first choice. The main reasons evoked for avoiding public providers were the fear of toxic and ineffective drugs. Many public health facilities in Bihar continue till today to prescribe sodium stibogluconate, despite widespread drug resistance15 and a VL elimination programme that recommends miltefosin as the first-line drug.
In conclusion, this study shows a potential to involve the informal sector in case-finding, though innovative tools for VL care have not yet been fully taken up by private for profit care providers. However, a descriptive study as this one will by itself not diminish the knowledge gap among providers. VL elimination initiative in the region may consider these results to increase awareness of the VL problem. Short orientation programmes may be undertaken to update the knowledge of private physicians and paramedics. Further, it should be explored how these health providers can be more effectively involved. Given their substantial share in the care of VL patients, the VL elimination initiative will need to address the gaps in private provider's knowledge while regulating their practice.
Acknowledgments
This study was funded by a grant from WHO/TDR's - Implementation research programme.
Footnotes
Conflict of Interest: There is no conflict of interest.
References
- 1. [accessed on April 4, 2009]. http://searo.who.int/EN/Section10/Section2163_11668.htm .
- 2.Singh SP, Reddy DCS, Rai M, Sundar S. Serious underreporting of visceral leishmaniasis through passive case reporting in Bihar, India. Trop Med Int Health. 2006;11:899–905. doi: 10.1111/j.1365-3156.2006.01647.x. [DOI] [PubMed] [Google Scholar]
- 3.Bhattacharya SK, Sur D, Sinha PK, Karbwang J. Elimination of leishmaniasis (kala-azar) from the Indian subcontinent is technically feasible & operationally achievable. Indian J Med Res. 2006;123:195–6. [PubMed] [Google Scholar]
- 4.Murray HW. Kala-azar - progress against a neglected disease. N Engl J Med. 2002;347:1793–4. doi: 10.1056/NEJMe020133. [DOI] [PubMed] [Google Scholar]
- 5.Boelaert M, Criel B, Leeuwenburg J, Van Damme W, Le Ray D, Van der Stuyft P. Visceral leishmaniasis control: a public health perspective. Trans R Soc Trop Med Hyg. 2000;94:465–71. doi: 10.1016/s0035-9203(00)90055-5. [DOI] [PubMed] [Google Scholar]
- 6.Ahluwalia IB, Bern C, Costa C, Akter T, Chowdhury R, Ali M, et al. Visceral leishmaniasis: consequences of a neglected disease in a Bangladeshi community. Am J Trop Med Hyg. 2003;69:624–8. [PubMed] [Google Scholar]
- 7.Koirala S, Parija SC, Karki P, Das ML. Knowledge, attitudes, and practices about kala-azar and its sandfly vector in rural communities of Nepal. Bull World Health Organ. 1998;76:485–90. [PMC free article] [PubMed] [Google Scholar]
- 8.Singh SP, Reddy DC, Mishra RN, Sundar S. Knowledge, attitude and practices related to kala-azar in a rural area of Bihar state, India. Am J Trop Med Hyg. 2006;75:505–8. [PubMed] [Google Scholar]
- 9.Sundar S, Mondal D, Rijal S, Bhattacharya S, Ghalib H, Kroeger A, et al. Implementation research to support the initiative on the elimination of kala azar from Bangladesh, India and Nepal - the challenges for diagnosis and treatment. Trop Med Int Health. 2008;13:2–5. doi: 10.1111/j.1365-3156.2007.01974.x. [DOI] [PubMed] [Google Scholar]
- 10.Mondal D, Singh SP, Kumar N, Joshi A, Sundar S, Das P, et al. Visceral leishmaniasis elimination programme in India, Bangladesh, and Nepal: reshaping the case finding/case management strategy. PLoS Negl Trop Dis. 2009;3:e355. doi: 10.1371/journal.pntd.0000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moser CA, Kalton G. London: Heinemann Educational Book; 1977. Survey methods in social investigation. [Google Scholar]
- 12.Joshi A, Narain JP, Prasittisuk C, Bhatia R, Ghalib H, Alvar J, et al. Can visceral leishmaniasis be eliminated from Asia? J Vector Borne Dis. 2008;45:105–11. [PubMed] [Google Scholar]
- 13.Rijal S, Koirala S, Van der Stuyft P, Boelaert M. The economic burden of visceral leishmaniasis for households in Nepal. Trans R Soc Trop Med Hyg. 2006;100:838–41. doi: 10.1016/j.trstmh.2005.09.017. [DOI] [PubMed] [Google Scholar]
- 14.Meheus F, Boelaert M, Baltussen R, Sundar S. Costs of patient management of visceral leishmaniasis in Muzaffarpur, Bihar, India. Trop Med Int Health. 2006;11:1715–24. doi: 10.1111/j.1365-3156.2006.01732.x. [DOI] [PubMed] [Google Scholar]
- 15.Sundar S. Drug resistance in Indian visceral leishmaniasis. Trop Med Int Health. 2001;6:849–54. doi: 10.1046/j.1365-3156.2001.00778.x. [DOI] [PubMed] [Google Scholar]


