Abstract
BACKGROUND:
The study was designed to compare the effect of intraincisional vs intraperitoneal infiltration of levobupivacaine 0.25% on post-operative pain in laparoscopic cholecystectomy.
MATERIALS AND METHODS:
This randomised controlled study was carried out on 189 patients who underwent laparoscopic cholecystectomy. Group 1 was the control group and did not receive either intraperitoneal or intraincisional levobupivacaine. Group 2 was assigned to receive local infiltration (intraincisional) of 20 ml solution of levobupivacaine 0.25%, while Group 3 received 20 ml solution of levobupivacaine 0.25% intraperitoneally. Post-operative pain was recorded for 24 hours post-operatively.
RESULTS:
Post-operative abdominal pain was significantly lower with intraincisional infiltration of levobupivacaine 0.25% in group 2. This difference was reported from 30 minutes till 24 hours post-operatively. Right shoulder pain showed significantly lower incidence in group 2 and group 3 compared to control group. Although statistically insignificant, shoulder pain was less in group 3 than group 2.
CONCLUSION:
Intraincisional infiltration of levobupivacaine is more effective than intraperitoneal route in controlling post-operative abdominal pain. It decreases the need for rescue analgesia.
Keywords: Laparoscopic cholecystectomy, levobupivacaine, local anaesthetics, postoperative pain
INTRODUCTION
Minimally invasive procedures hold an important position in nowadays’ surgical practice. Laparoscopic cholecystectomy has become the main treatment of symptomatic cholelithiasis.[1] It represents the most common laparoscopic procedure performed all over the world and has been performed as a day-case procedure for over a decade.[2,3] The most important benefits of such procedure are less discomfort, shorter hospitalisation and earlier return to normal activity.[4]
Although this is the case, the patients usually suffer from post-operative pain, especially with coughing, respiratory movements and mobilisation during the first hours and shoulder pain secondary to peritoneal insufflation after the eighth post-operative hours and during the night after surgery. This can delay the patient's recovery, lengthen the hospital stay and increase morbidity and costs.[5–7]
Moreover, pain after laparoscopy may be moderate or even severe enough to require opioid treatment.[8–10] Although opioids play a major role in controlling early post-operative pain and still administered routinely in many cases, their minor side effects and the increasing availability of suitable alternatives may limit their future use in some situations.[11,12]
Multiple approaches for analgesia are therefore required to provide effective control of early post-operative pain.[13] Many trials have been carried out using intraperitoneal or incisional local anaesthetic infiltration, but the results relating to pain reduction and parenteral analgesic consumption are conflicting.[14–18] The technique has the advantage of not having adverse effects, such as those of opiates, which lead to prolonged hospitalisation.[19] Although there are many studies using bupivacaine as local anaesthetic, few studies have used levobupivacaine and the timing and route of administration of the local anaesthetic agent were different in most of them.
In the present study, we aim to compare between the effectiveness of intraincisional vs intraperitoneal infiltration of local anaesthetic agent (levobupivacaine) for the management of early post-operative pain following laparoscopic cholecystectomy.
MATERIALS AND METHODS
The present study was conducted as a randomised controlled clinical trial among patients who were subjected to laparoscopic cholecystectomy for cholelithiasis in Surgery Department, Suez Canal University Hospital in Ismailia, Egypt, between the periods from June 2008 to May 2010. After approval of our ethical committee, a total of 189 patients, classified as American Society of Anesthesiologists I and II (ASA I and II) and aged from 25 to 64 years, were recruited from the outpatient clinic and scheduled for elective laparoscopic cholecystectomy under general anaesthesia. A written informed consent was signed from all patients before enrolling them in the study. No grants or funds from any pharmaceutical industry were obtained for the study.
Patients with known allergic reactions to local anaesthetics were excluded from the study. Also, patients were excluded if they underwent surgery for acute cholecystitis or if the operation had been converted to an open procedure, as well as patients with intra-operative complications. Other exclusion criteria are morbid obesity, chronic medical diseases and chronic opioid treatment.
Included patients were randomised prospectively, using a blind envelope system, into three groups of 63 persons each; there were no dropouts after randomisation. Group 1 was the control group and did not receive either intraperitoneal or intraincisional levobupivacaine. Group 2 was assigned to receive local infiltration (intraincisional) of 20 ml solution of levobupivacaine 0.25% at the end of operation before closure of the wound. Group 3 received 20 ml solution of levobupivacaine 0.25% intraperitoneally in the gall bladder bed and under the right copula of the diaphragm at the end of the laparoscopic procedure.
Following the anaesthetic assessment, patients were admitted to the hospital the day before the operation. All patients received the same anaesthetic technique. Usual monitoring was used including heart rate, respiratory rate, continuous ECG, SpO2 and non-invasive arterial blood pressure. Creation of CO2 pneumoperitoneum at 14 mm Hg pressure was justified in all patients and standard laparoscopic cholecystectomy using the 4-port technique was performed. All the operations were performed by one team of surgeons that is experienced in laparoscopic surgery.
For intraincisional infiltration of levobupivacaine, the fascia, muscle and preperitoneal space were infiltrated using 5 ml for each port (infiltration of four trocar sites, thus using a total of 20 ml solution). For intraperitoneal instillation, the solution was instilled in the gall bladder bed and under the right diaphragm following the removal of the gallbladder. This was done using a catheter inserted through the right subcostal port. No abdominal drainage was used to any patient.
All patients received analgesics to a standard post-operative protocol with Diclofenac 75 mg intramuscularly at the end of the operation and further 50 mg per oral route twice a day. Pethidine, as a rescue analgesia, was administered on request 10 to 20 mg intravenously in the recovery room and 50 mg intramuscularly in the ward. The number of patients requiring rescue analgesia was recorded in each group.
Patients were evaluated for 24 hours post-operatively with recording of abdominal pain using the standard 10-cm visual analogue scale (VAS). The post-operative pain score was reported at 30 minutes, then at 4, 8, 12 and 24 hours. The residents in the surgery department were trained to obtain the VAS score on the determined points of time in the ward. They were blinded to the patients’ status concerning local analgesia. The time of arrival in the post-operative recovery room was defined as zero hour post-operatively. The number of patients experiencing right shoulder pain in each group was also recorded.
Statistical analysis
All data were expressed as means ± standard deviation, with the exception of rescue analgesic treatment and the occurrence of right shoulder pain that were percentages (%). Parametric data were compared between groups by analysis of variance (ANOVA). Student t-test and chi-square method were used for continuous and discrete variables, respectively. A two-sided probability value (P-value) less than 0.05 was considered statistically significant.
RESULTS
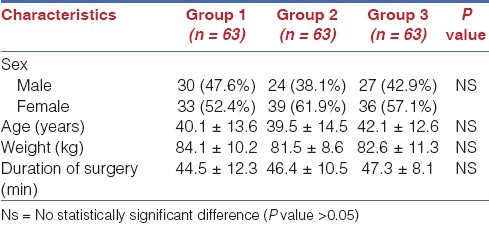
Analysis of the demographic characteristics of the studied patients has shown that all groups were matched as regarding age, gender and weight. Most of the patients were females (52.4%, 61.9% and 57.1% in group 1, 2 and 3, respectively). Mean duration of surgery was insignificantly different among the three groups (44.5, 46.4 and 47.3 minutes in group 1, 2 and 3, respectively) [Table 1].
Table 1.
Patients characteristics
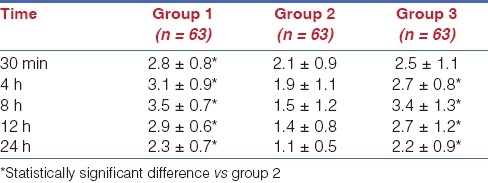
Post-operative abdominal pain was significantly lower in group 2 (intraincisional infiltration of levobupivacaine 0.25%) than control group and group 3 (intraperitoneal infiltration of levobupivacaine 0.25%). This difference was reported from 30 minutes till 24 hours post-operatively. Although pain scores are less in group 3 when compared with the control group, yet it is not statistically significant [Table 2].
Table 2.
Post-operative pain using visual analogue scale in all groups
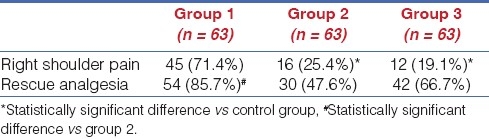
As regarding the incidence of right shoulder pain, both group 2 and group 3 showed significantly lower incidence compared to control group. Although statistically insignificant, shoulder pain was less in group 3 than group 2. Consumption of rescue analgesia was significantly lower in patients of group 2 compared to control group only. Difference between group 3 and control group concerning rescue analgesia was not statistically significant [Table 3].
Table 3.
Incidence of right shoulder pain, request of rescue analgesia at the three groups of the study
DISCUSSION
Laparoscopic cholecystectomy is one of the commonest day-case surgeries. The post-operative pain associated with this minimally invasive procedure is generally less intense and lasts a shorter time than that follow open cholecystectomy but it remains a prevalent problem of the early post-operative period and may delay discharging the patient, especially in day-case departments. It reaches a peak within the first few hours following the operation but diminishes with time.[20] The origin of pain after laparoscopic cholecystectomy is multifactorial with pain arising from the incision sites (somatic pain), from the gallbladder bed (visceral pain) and as a consequence of a pneumoperitoneum.[21]
Many researchers have suggested that the combination of somatovisceral local anaesthetic treatment reduces incisional, intra-abdominal and shoulder pain in laparoscopic cholecystectomy. These local agents induce antinociception by acting on the nerve membranes. They reversibly decrease the rate of depolarisation and repolarisation of excitable membranes (like nociceptors).[14,22] There are different routes to administrate the local anaesthetic drug; some researchers have shown that local parietal anaesthesia is effective in controlling post-operative pain,[23–25] while others have shown that it is not effective.[26]
A significant number of trials have examined the intraperitoneal administration of local anaesthetics in laparoscopic cholecystectomies as regards to post-operative pain and narcotic analgesic consumption, with promising results.[8,14,21,27] However, other studies indicate that the post-operative analgesia and narcotic usage was not significantly different in the groups that received local anaesthesia.[25,28,29]
The timing of the administration of the local anaesthetic during surgery is a matter of debate; several studies have examined this point with controversial results as some showed no statistical difference regarding the time of discharge and the post-operative pain,[18–30] while other studies support the belief that the timing of intraperitoneal administration of the local anaesthetic is crucial.[20,31,32]
In the present study, we compared intraincisional vs intraperitoneal infiltration of local anaesthetic and unlike most of the previous studies that evaluated bupivacaine, we used levobupivacaine 0.25%. We found that intraincisional infiltration of levobupivacaine is more effective than intraperitoneal route in controlling post-operative abdominal pain. It decreases the post-operative analgesia requirements.
Our results are consistent with that of Lepner et al.[25] who have compared both intraincisional and intraperitoneal infiltration of local anaesthetic. These results have reported significantly more reduction of post-operative abdominal pain with intraincisional local infiltration of the anaesthetic drug.
Some studies failed to demonstrate any pain reduction with intraperitoneal bupivacaine after laparoscopic cholecystectomy,[28,29] while others have noted only reduced shoulder pain with overall pain not affected.[33] On the contrary, Elhakim et al.[34] have shown that intraperitoneal Lidocaine reduces effectively both shoulder pain and abdominal post-operative pain after laparoscopic cholecystectomy. In the present study, post-operative right shoulder pain is less with patients assigned to intraperitoneal infiltration of local anaesthetic than those who are assigned to intraincisional infiltration, yet it is not statistically significant. This insignificant result may be due to reduced contact with the gallbladder bed as a result of continuous flux of intraperitoneal liquids. This fact also explains the large difference in results shown by different authors.
In conclusion, the present study showed that intraincisional infiltration of levobupivacaine is more effective than intraperitoneal route in controlling post-operative abdominal pain. It decreases the post-operative analgesia requirements. Although it is insignificant, shoulder pain is less with intraperitoneal infiltration.
ACKNOWLEDGEMENT
The authors would like to thank Professor Ahmed Ellabban and Professor Soliman Elkamash for their support in revising the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Zacks SL, Sandler RS, Rutledge R, Brown RS. A population-based cohort study comparing laparoscopic cholecystectomy and open cholecystectomy. Am J Gastroenterol. 2002;97:334–40. doi: 10.1111/j.1572-0241.2002.05466.x. [DOI] [PubMed] [Google Scholar]
- 2.Ji W, Ding K, Li LT, Wang D, Li N, Li JS. Outpatient versus inpatient laparoscopic cholecystectomy: A single center clinical analysis. Hepatobiliary Pancreat Dis Int. 2010;9:60–4. [PubMed] [Google Scholar]
- 3.Johansson M, Thune A, Nelvin L, Lundell L. Randomized clinical trial of day-care versus overnight-stay laparoscopic cholecystectomy. Br J Surg. 2006;93:40–5. doi: 10.1002/bjs.5241. [DOI] [PubMed] [Google Scholar]
- 4.Gadacz TR, Talamini MA. Traditional versus laparoscopic cholecystectomy. Am J Surg. 1991;161:336–8. doi: 10.1016/0002-9610(91)90591-z. [DOI] [PubMed] [Google Scholar]
- 5.Kucuk C, Kadiogullari N, Canoler O, Savli S. A Placebo-controlled comparison of bupivacaine and ropivacaine instillation for preventing postoperative pain after laparoscopic cholecystectomy. Surg Today. 2007;37:396–400. doi: 10.1007/s00595-006-3408-1. [DOI] [PubMed] [Google Scholar]
- 6.Joris J, Thiry E, Paris P, Weerts J, Lamy M. Pain after laparoscopic cholecystectomy: Characteristics and effect of intraperitoneal bupivacaine. Anesth Analg. 1995;81:379–84. doi: 10.1097/00000539-199508000-00029. [DOI] [PubMed] [Google Scholar]
- 7.Lum YW, House MG, Hayanga AJ, Schweitzer M. Postcholecystectomy syndrome in the laparoscopic era. J Laparoendosc Adv Surg Tech A. 2006;16:482–5. doi: 10.1089/lap.2006.16.482. [DOI] [PubMed] [Google Scholar]
- 8.Papadima A, Lagoudianakis E, Antonakis P, Filis K, Makri I, Markogiannakis H, et al. Repeated intraperitoneal instillation of levobupivacaine for the management of pain after laparoscopic cholecystectomy. Surgery. 2009;146:475–82. doi: 10.1016/j.surg.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 9.Bisgaard T, Klarskov B, Rosenberg J, Kehlet H. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain. 2001;90:261–9. doi: 10.1016/S0304-3959(00)00406-1. [DOI] [PubMed] [Google Scholar]
- 10.Wills VL, Hunt DR. Pain after laparoscopic cholecystectomy. Br J Surg. 2000;87:273–84. doi: 10.1046/j.1365-2168.2000.01374.x. [DOI] [PubMed] [Google Scholar]
- 11.Bisgaard T, Kehlet H, Rosenberg J. Pain and convalescence after laparoscopic cholecystectomy. Eur J Surg. 2001;167:84–96. doi: 10.1080/110241501750070510. [DOI] [PubMed] [Google Scholar]
- 12.Kehlet H, Rung GW, Callesen T. Postoperative opioid analgesia: Time for a reconsideration? J Clin Anesth. 1996;8:441–5. doi: 10.1016/0952-8180(96)00131-6. [DOI] [PubMed] [Google Scholar]
- 13.Jin F, Chung F. Multimodal analgesia for postoperative pain control. J Clin Anesth. 2001;13:524–39. doi: 10.1016/s0952-8180(01)00320-8. [DOI] [PubMed] [Google Scholar]
- 14.Louizos AA, Hadzilia SJ, Leandros E, Kouroukli IK, Georgiou LG, Bramis JP. Postoperative pain relief after laparoscopic cholecystectomy: A placebo-controlled double-blind randomized trial of preincisional infiltration and intraperitoneal instillation of levobupivacaine 0.25% Surg Endosc. 2005;19:1503–6. doi: 10.1007/s00464-005-3002-4. [DOI] [PubMed] [Google Scholar]
- 15.Gupta A. Local anaesthesia for pain relief after laparoscopic cholecystectomy-a systematic review. Best Pract Res Clin Anaesthesiol. 2005;19:275–92. doi: 10.1016/j.bpa.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Labaille T, Mazoit JX, Paqueron X, Franco D, Benhamou D. The clinical efficacy and pharmacokinetics of intraperitoneal ropivacaine for laparoscopic cholecystectomy. Anesth Analg. 2002;94:100–5. doi: 10.1097/00000539-200201000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Papagiannopoulou P, Argiriadou H, Georgiou M, Papaziogas B, Sfyra E, Kanakoudis F. Preincisional local infiltration of levobupivacaine vs ropivacaine for pain control after laparoscopic cholecystectomy. Surg Endosc. 2003;17:1961–4. doi: 10.1007/s00464-002-9256-1. [DOI] [PubMed] [Google Scholar]
- 18.Paulson J, Mellinger J, Baguley W. The use of intraperitoneal bupivacaine to decrease the length stay in elective laparoscopic cholecystestomy patients. Am Surg. 2003;69:275–8. [PubMed] [Google Scholar]
- 19.Feroci F, Kröning KC, Scatizzi M. Effectiveness for pain after laparoscopic cholecystectomy of 0.5% bupivacaine-soaked Tabotamp placed in the gallbladder bed: A prospective, randomized, clinical trial. Surg Endosc. 2009;23:2214–20. doi: 10.1007/s00464-008-0301-6. [DOI] [PubMed] [Google Scholar]
- 20.Inan A, Sen M, Dener C. Local anesthesia use for laparoscopic cholecystectomy. World J Surg. 2004;28:741–4. doi: 10.1007/s00268-004-7350-3. [DOI] [PubMed] [Google Scholar]
- 21.Kim TH, Kang H, Park JS, Chang IT, Park SG. Intraperitoneal ropivacaine instillation for postoperative pain relief after laparoscopic cholecystectomy. J Korean Surg Soc. 2010;79:130–6. [Google Scholar]
- 22.Bisgaard T, Klarskov B, Kristiansen VB, Callesen T, Schulze S, Kehlet H, et al. Multi-Regional local anesthetic infiltration during laparoscopic cholecystectomy in patients receiving prophylactic multi-modal analgesia: A randomized, double-blinded, placebo-controlled study. Anesth Analg. 1999;89:1017–24. doi: 10.1097/00000539-199910000-00036. [DOI] [PubMed] [Google Scholar]
- 23.Ure BM, Troidl H, Spangenberger W, Neugebauer E, Lefering R, Ullmann K, et al. Preincisional local anesthesia with bupivacaine and pain after laparoscopic cholecystectomy.A double-blind randomized clinical trial. Surg Endosc. 1993;7:482–8. doi: 10.1007/BF00316685. [DOI] [PubMed] [Google Scholar]
- 24.Bisgaard T. Analgesic treatment after laparoscopic cholecystectomy. Anesthesiology. 2006;104:835–46. doi: 10.1097/00000542-200604000-00030. [DOI] [PubMed] [Google Scholar]
- 25.Lepner U, Goroshina J, Samarütel J. Postoperative pain relief after laparoscopic cholecystectomy: A randomised prospective double-blind clinical trial. Scand J Surg. 2003;92:121–4. [PubMed] [Google Scholar]
- 26.Møiniche S, Jørgensen H, Wetterslev J, Dahl JB. Local anesthetic infiltration for postoperative pain relief after laparoscopy: A qualitative and quantitative systematic review of intraperitoneal, port-site infiltration and mesosalpinx block. Anesth Analg. 2000;90:899–912. doi: 10.1097/00000539-200004000-00024. [DOI] [PubMed] [Google Scholar]
- 27.Ahmed BH, Ahmed A, Tan D, Awad ZT, Al-Aali AY, Kilkenny J, 3rd, et al. Post-laparoscopic cholecystectomy pain: Effects of intraperitoneal local anesthetics on pain control-a randomized prospective double-blinded placebo-controlled trial. Am Surg. 2008;74:201–9. [PubMed] [Google Scholar]
- 28.Zmora O, Stolik-Dollberg O, Bar-Zakai B, Rosin D, Kuriansky J, Shabtai M, et al. Intraperitoneal bupivacaine does not attenuate pain following laparoscopic cholecystectomy. JSLS. 2000;4:301–4. [PMC free article] [PubMed] [Google Scholar]
- 29.Elfberg BA, Sjövall-Mjöberg S. Intraperitoneal bupivacaine does not effectively reduce pain after laparoscopic cholecystectomy: A randomized, placebo-controlled and double-blind study. Surg Laparosc Endosc Percutan Tech. 2000;10:357–9. [PubMed] [Google Scholar]
- 30.Uzunkoy A, Coskun A, Akinci OF. The value of preemptive analgesia in the treatment of postoperative pain after laparoscopic cholecystectomy. Eur Surg Res. 2001;33:39–41. doi: 10.1159/000049691. [DOI] [PubMed] [Google Scholar]
- 31.Lee IO, Kim SH, Kong MH, Lee MK, Kim NS, Choi YS, et al. Pain after laparoscopic cholecystectomy: The effect and timing of incisional and intraperitoneal bupivacaine. Can J Anaesth. 2001;48:545–50. doi: 10.1007/BF03016830. [DOI] [PubMed] [Google Scholar]
- 32.Cantore F, Boni L, Di Giuseppe M, Giavarini L, Rovera F, Dionigi G. Pre-incision local infiltration with levobupivacaine reduces pain and analgesic consumption after laparoscopic cholecystectomy: A new device for day-case procedure. Int J Surg. 2008;6:S89–92. doi: 10.1016/j.ijsu.2008.12.033. [DOI] [PubMed] [Google Scholar]
- 33.Cunniffe MG, McAnena OJ, Dar MA, Calleary J, Flynn N. A prospective randomized trial of intraoperative bupivacaine irrigation for management of shoulder-tip pain following laparoscopy. Am J Surg. 1998;176:258–61. doi: 10.1016/s0002-9610(98)00150-0. [DOI] [PubMed] [Google Scholar]
- 34.Elhakim M, Elkott M, Ali NM, Tahoun HM. Intraperitoneal lidocaine for postoperative pain after laparoscopy. Acta Anaesthesiol Scand. 2000;44:280–4. doi: 10.1034/j.1399-6576.2000.440310.x. [DOI] [PubMed] [Google Scholar]


