Abstract
Small bowel obstruction associated with abdominal cocoon (AC) is a rarely encountered surgical emergency. This condition is characterised by a thick fibrous membrane which encases the small bowel partially or completely. It is usually difficult to be able to make a definitive diagnosis in the presence of obscure clinical and radiological findings. Diagnosis is usually made at laparotomy when the encasement of the small bowel within a cocoon-like sac is visualised. Here, we report on a 29-year-old male patient who presented with acute small bowel obstruction and was eventually diagnosed with AC at laparoscopy. In this case, laparoscopic excision of the fibrous sac and extensive adhesiolysis resulted in complete recovery. Although rare, the diagnosis of AC should be kept in cases of patients with intestinal obstruction combined with relevant imaging findings. Laparoscopy should also be considered for the management of this condition in suitable patients.
Keywords: Abdominal cocoon, laparoscopy, management, small bowel obstruction
INTRODUCTION
Bowel obstruction is a common surgical emergency. However, at times, unusual cases of bowel obstruction such as abdominal cocoon (AC) may be encountered. In this condition, the small bowel is partially or totally encased by a thick fibrocollagenous membrane which gives a cocoon-like appearance. Its clinical features are nonspecific; therefore, AC is not often suspected preoperatively.[1] Herein, we report a case of intestinal obstruction secondary to AC and its laparoscopic management.
CASE REPORT
A 29-year-old man was admitted to our emergency surgery unit with a 2-day history of recurrent bilious vomiting, colicy abdominal pain and distension. He had no significant medical history.
The patient's vital signs were normal. The abdomen was distended, with increased bowel sounds, but no tenderness or mass were noted. Routine laboratory blood analysis was within normal limits. A plain upright abdominal radiograph showed air-fluid levels in the upper quadrants. Abdominal ultrasonography suggested mechanical obstruction. A computed tomography (CT) scan demonstrated the small bowel loops clustered to the left of the abdomen within a sac-like structure [Figure 1]. A decision for laparoscopic management was taken on the basis of these clinical and radiological findings.
Figure 1.
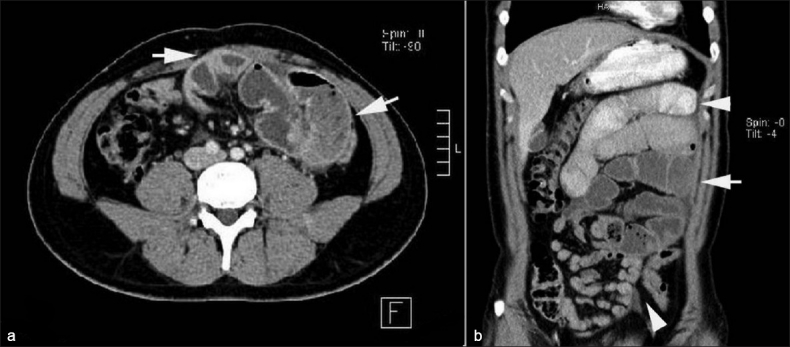
Mid-abdominal transaxial CT scan (a) shows the encasement of small bowel loops within a sac (arrows) resulting in bowel obstruction. Coronal CT scan (b) reveals the markedly distended pre-obstructive jejunal loops (upper arrowhead) and post-obstructive distal small bowel collapse (lower arrowhead)
The operation was performed using five trocars with Hasson's technique. At laparoscopy, the small bowel loops were seen dilated in the proximal part of the jejunum to a distance of approximately 40 cm from the duodenojejunal flexure. Beyond this point, the rest of the jejunal loops and the proximal ileum were conglomerated within a whitish fibrous sac. The other organs including the distal ileal loops were normal. Following extensive adhesiolysis using endoscissors and endograspers, the entire entrapped small bowel was freed from the sac [Figure 2] and the sac was excised. There was a dense adhesion band in the proximal jejunum which caused the obstruction. Following the lysis of this band, the obstructed jejunal loops were relieved without bowel resection. The loops within the cocoon were also adhered to each other by thin flimsy adhesions which could be separated easily. Following thorough peritoneal cleansing, the operation was terminated with no intraoperative complications.
Figure 2.
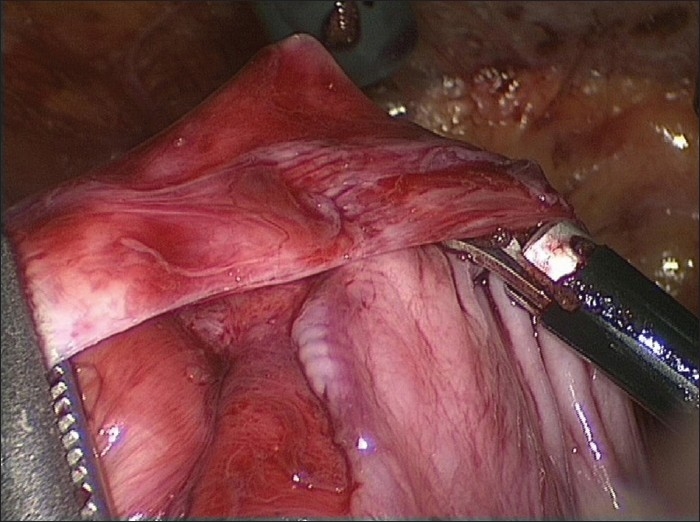
Laparoscopic dissection of the dense fibrocollagenous sac
Histopathologic examination of the sac showed proliferation of fibroconnective tissue with nonspecific inflammatory reaction. Cytologic studies and cultures of the ascitic fluid were negative for malignant cells and bacteria, respectively. Following an uneventful recovery, the patient was discharged home on the fourth postoperative day. During a six-month postoperative period, he showed no obstructive symptoms.
DISCUSSION
AC, also known as idiopathic encapsulating peritonitis, was first described and named by Foo et al. in 1978.[2] A number of factors have been proposed for the aetiopathogenesis of this condition. These include previous abdominal surgery, tuberculosis and certain medicines (e.g., practolol).[1,3] However, at present, there is no objective evidence to substantiate the aetiology and pathogenesis of this rare entity. We do not think our patient's condition was due to any of the aforementioned factors and the absence of mesothelial cells on our histopathologic examination was inconsistent with a diagnosis of congenital dysplasia.
Clinically, patients with AC present with symptoms of acute or subacute small bowel obstruction with or without multiple episodes that could sometimes resolve spontaneously. The preoperative diagnosis might be manifested with nonspecific imaging findings. Compared with other imaging techniques, CT can give a more complete picture of this entity as well as any associated complications and may help to exclude other causes of small bowel obstruction.[3]
In the presence of bowel obstruction, surgery is warranted and the diagnosis is usually made on surgical exploration.[3] Careful dissection of the sac with extensive adhesiolysis is the treatment of choice which results in complete recovery. Laparotomy has been the procedure of choice in the majority of the reported AC cases, whereas laparoscopy appears to be a rarely preferred approach.[4,5] Indeed, laparoscopy needs surgical expertise in order to avoid the risk of bowel injury.[4] It is also noteworthy that early postoperative small bowel obstruction is a potential complication of extensive adhesiolysis. Therefore, special intraoperative care including gentle tissue dissection, careful haemostasis and thorough peritoneal cleansing should be taken.
The long-term prognosis of AC after lysis of adhesions is usually excellent.[4] In our case, laparoscopy was a useful tool both for the definitive diagnosis and the treatment of this condition, leading to a favourable postoperative outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hur J, Kim KW, Park MS, Yu JS. Abdominal cocoon: Preoperative diagnostic clues from radiologic imaging with pathologic correlation. AJR Am J Roentgenol. 2004;182:639–41. doi: 10.2214/ajr.182.3.1820639. [DOI] [PubMed] [Google Scholar]
- 2.Foo KT, Ng KC, Rauff A, Foong WC, Sinniah R. Unusual small intestinal obstruction in adolescent girls: The abdominal cocoon. Br J Surg. 1978;65:427–30. doi: 10.1002/bjs.1800650617. [DOI] [PubMed] [Google Scholar]
- 3.Wei B, Wei HB, Guo WP, Zheng ZH, Huang Y, Hu BG, et al. Diagnosis and treatment of abdominal cocoon: A report of 24 cases. Am J Surg. 2009;198:348–53. doi: 10.1016/j.amjsurg.2008.07.054. [DOI] [PubMed] [Google Scholar]
- 4.Makam R, Chamany T, Ramesh S, Potluri VK, Varadaraju PJ, Kasabe P. Laparoscopic management of abdominal cocoon. J Minim Access Surg. 2008;4:15–7. doi: 10.4103/0972-9941.40992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu YJ, Zhu YM. Laparoscopic examination and treatment of abdominal cocoon with infertility: A report of 6 cases. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2004;33:462–4. doi: 10.3785/j.issn.1008-9292.2004.05.020. [DOI] [PubMed] [Google Scholar]


