Abstract
Prosthetic mesh is now used routinely in inguinal hernia repairs, although its fixation is thought to be a potential cause of chronic groin pain. The Parietene ProGrip™ (TYCO Healthcare) mesh, which is semi-resorbable and incorporates self-fixing properties, has been shown to provide satisfactory repair in open surgery. We describe the use of this mesh in TAPP hernia repair, which has not previously been reported in the literature. A prospective study of 29 patients showed a mean operative time to be 47.6 min, with 96% of patients discharged home on the day of surgery or the day after. Visual analog pain scales (out of 10) reduced from 4 preoperatively to 0 at 6 months, and only 1 patient suffered a minor wound complication. The use of this mesh in transabdominal preperitoneal hernia repair is therefore feasible, safe, and may reduce postoperative pain.
Keywords: Hernia, inguinal, laparoscopic, mesh, self-adhesive
INTRODUCTION
Prosthetic mesh reinforcement is now a routine step in the operative management of inguinal herniae, having been shown to significantly reduce the risk of recurrence.
Postoperative pain, however, remains a significant clinical problem, which is often attributed to the characteristics of the mesh and/or the method of fixation used.[1] Current trends in transabdominal preperitoneal (TAPP) repair are to use staples or fibrin glue, the latter now known to reduce postoperative pain, complications, and time to resumption of normal activities.[2,3]
A standard laparoscopic approach for TAPP inguinal hernia repair begins with an open supraumbilical cutdown or the use of a Verres needle to establish a pneumoperitoneum. Two 5 mm working ports are placed under direct vision, one in the midline in the suprapubic region, and a second in either the left or right iliac fossa. The procedure is described in full elsewhere in the literature, but in brief comprises opening the peritoneum, identifying the boundaries of Hasselbach's triangle, and reducing the hernia.[4] Next, a polypropylene mesh is normally fashioned and fixed in place using a form of stapling device, such as the Protack™ (TYCO Healthcare) device.
MODIFICATION
A novel semi-resorbable mesh incorporating self-fixing properties has been shown to provide satisfactory repair in open inguinal herniae.[5] We describe the routine application of this system in laparoscopic TAPP inguinal hernia repair.
The Parietene ProGrip™ (TYCO Healthcare) 15 × 9 cm mesh is constructed from a low-weight polypropylene knitting fabric. One side of the mesh incorporates resorbable polyactic acid (PLA) microhooks, which provide its adhesive properties [Figure 1]. Mesh reinforcement using this technique involves holding the mesh at the centre of the nonadhesive fabric side [Figure 2], inserting it through the 10 mm supraumbilical port [Figure 3], and positioning it firmly in place within the preperitoneal envelope [Figure 4].
Figure 1.
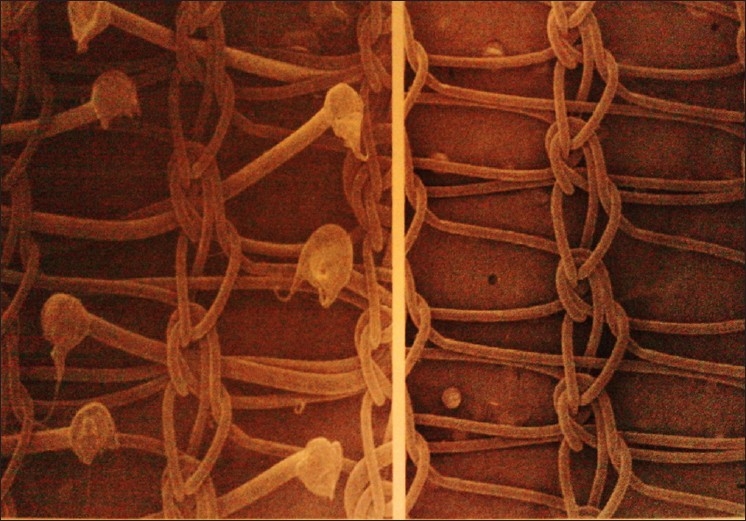
The self-adhesive mesh has resorbable polyactic acid microhooks
Figure 2.

The mesh is held in the centre of the non-adhesive side
Figure 3.
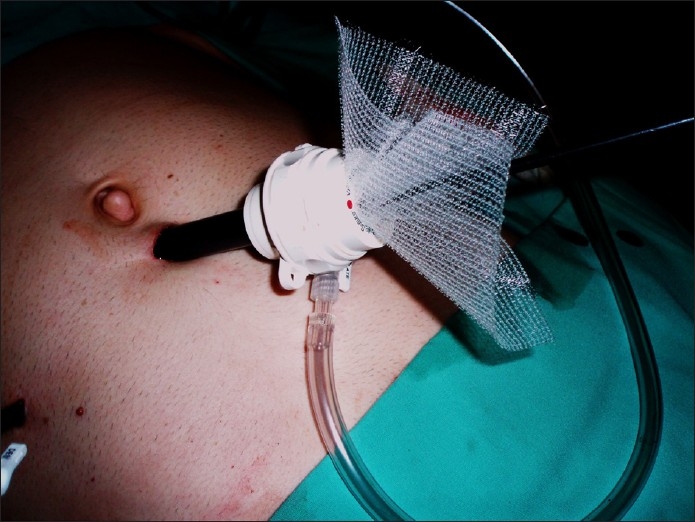
The mesh is placed through the 10 mm supra-umbilical port
Figure 4.

The mesh is placed firmly within the pre-peritoneal envelope without the need for tacs, staples or sutures
The peritoneum is finally closed with 3/0 vicryl, and the abdomen closed in the usual manner.
BENEFITS
As this technique is novel, there is little in the literature to support its use. To clarify its efficacy we undertook a prospective study. All patients undergoing laparoscopic inguinal hernia repair by the senior author between July 2009 and February 2010 had a TAPP repair with a Parietene ProGrip™ (TYCO Healthcare) mesh. Data were collected on admission and at 6 months postoperatively.
Twenty-nine patients (93% male; median [IQR] age, 55 [41–67]) had 43 inguinal herniae repaired. Fourteen (48%) were bilateral, 6 (14%) recurrent, and 23 (53%) were direct. Mean [SD] operative time per hernia was 47.6 (13.8) min. Fifteen (51%) were discharged home on the same day, 13 (45%) on day 1, and 1 (4%) on day 3.
Mean [SD] return to full activity was 24.5 (8.4) days. There were significant improvements in the visual analog pain scores (out of 10) at follow-up. The median preoperative score was 4, improving to 0 at 6 months (P < 0.01, Wilcoxon test). None had evidence of recurrence, 1 (4%) had a resolving wound hematoma and all were satisfied with their procedure.
The use of a polypropylene knitted mesh (Ethicon) and Protack™ (TYCO Healthcare) autosuture device for a standard TAPP repair would cost approximately £228.40 (US$361.25). This is considerably more than the Parietene ProGrip™ (TYCO Healthcare) mesh, which is available for £91.65 (US$144.96). This technique will therefore save £136.75 (US$216.37) per case, which totaled £3965.75 (US$6274.58) over our study period.
CONCLUSIONS
Chronic pain following inguinal hernia repair is often attributed to entrapment of nerves during mesh fixation. ProGrip™ is a revolutionary new mesh with absorbable hooks to secure it firmly in place, eliminating the need for sutures or staples. Using a self-fixing mesh such as this in laparoscopic surgery is feasible, safe, more cost-effective, and may reduce postoperative pain.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Champault G, Polliand C, Dufour F, Ziol M, Behr L. A self adhering prosthesis for hernia repair: Experimental study. Hernia. 2009;13:49–52. doi: 10.1007/s10029-008-0419-4. [DOI] [PubMed] [Google Scholar]
- 2.Lovisetto F, Zotta S, Rota E, Mazzilli M, Bardone M, Bottero L, et al. Use of Human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: A prospective, randomised study. Ann Surg. 2007;245:222–31. doi: 10.1097/01.sla.0000245832.59478.c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olmi S, Scaini A, Erba L, Guaglio M, Croce E. Quantification of pain in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernioplasty identified marked differences between prosthesis fixation systems. Surgery. 2007;142:40–6. doi: 10.1016/j.surg.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Ridings P, Evans D. The transabdominal pre-peritoneal (TAPP) inguinal hernia repair: A trip along the learning curve. J R Coll Surg Edinb. 2000;45:29–32. [PubMed] [Google Scholar]
- 5.Chastan P. Tension free open inguinal hernia repair using an innovative self gripping semi-resorbably mesh. J Minim Access Surg. 2006;2:139–43. doi: 10.4103/0972-9941.27726. [DOI] [PMC free article] [PubMed] [Google Scholar]


