Abstract
Context:
The risk of becoming a diabetic for an individual with a positive family history of diabetes increases by two- to fourfold.
Aim:
To record the anthropometric indices and the physical fitness in individuals with family history of type-2 diabetes mellitus and compare these results with those of controls.
Settings and Design:
This is a comparative study done in the department of physiology.
Materials and Methods:
Thirty-two apparently healthy medical students with family history of type-2 Diabetes Mellitus were chosen for the study and matched with equal number of controls. Anthropometric measurements (height, weight, waist circumference, hip circumference, thigh circumference, upper segment and lower segment) were recorded. Body mass index (BMI), waist–hip ratio (WHR), waist–thigh ratio (WTR), and upper to lower segment ratio (US/LS ratio) were calculated. Blood pressure and heart rate were measured. Physical fitness was evaluated using Queen's College step test protocol. Rate Pressure Product (RPP) and Physical Fitness Index (PFI) were calculated before and after exercise.
Statistical Analysis:
Statistical analysis was done using SPSS software.
Results:
BMI, WHR, US/LS ratio, and RPP at rest were significantly higher (P < 0.05), whereas WTR, PFI, and RPP after exercise lower (P > 0.05) in cases as compared to controls.
Conclusions:
It can be concluded that apparently healthy individuals with family history of type-2 diabetes mellitus have higher anthropometric values and lower physical fitness than the controls.
Keywords: Anthropometry, family history of type-2 diabetes mellitus, physical fitness index, queen's college step test, rate pressure product
INTRODUCTION
India is one of the highly populated countries and is now leading with other Western countries in having increased number of people suffering from noncommunicable diseases, such as cardiovascular disorders and type-2 Diabetes Mellitus, which are the major determinants of morbidity and mortality. The risk of becoming a diabetic for an individual with a positive family history of diabetes increases by two- to fourfold an offspring's chance and individuals with a positive family history of diabetes have higher body mass index (BMI) than controls.[1] Obesity and body fat distribution,[2] lifestyle.[3] impaired glucose tolerance (IGT), and a family history of type-2 Diabetes Mellitus,[4,5] represent risk factors for type-2 Diabetes Mellitus. First-degree relatives of patients with type-2 Diabetes Mellitus frequently show abnormal glucose tolerance and share several metabolic abnormalities of the full blown disease and have a 30%–40% risk of developing type-2 Diabetes Mellitus themselves.[5] Simple anthropometrical measurements have been used as surrogate measurements of obesity and have more practical value in both clinical practice and for large-scale epidemiological studies.[6] BMI, which relates weight to height, is a simple measure of body size. Waist circumference and waist-hip ratio (WHR) are alternatives to BMI. Waist circumference is the best simple measure of both intra-abdominal fat mass and total fat.[7,8] A larger hip circumference is associated with a lower prevalence of self-reported type-2 diabetes and lower fasting glucose concentrations, independently of BMI and waist circumference.[9,10] Individuals with a family history of diabetes have higher WHR.[11] It is a well-known fact that physical activities are less in obese individuals, and obesity is one of the important and most common risk factors of type-2 diabetes mellitus. Several studies have identified a higher heart rate as well as blood pressure as a key component of metabolic syndrome.[12] However, there are no studies relating anthropometry and cardiorespiratory fitness in children whose parents are suffering from type-2 diabetes mellitus. The present study is aimed to compare the anthropometry and physical fitness in individuals with a family history of type-2 diabetes mellitus.
MATERIALS AND METHODS
Materials
The study was done on 32 apparently healthy medical students of 1st year, SNMC, Bagalkot, in the age group of 18–20 years. Family history of type-2 diabetes mellitus was enquired. Controls were selected from the same age group with no family history of type-2 diabetes mellitus. Informed consent was obtained from all the participants and ethical approval for the study was obtained from the local ethical committee.
Anthropometric measurements
Weight and height were measured while subjects were barefoot and wearing light clothes only. Weight was measured to the nearest 0.1 kg using a digital weight recorder. Height was measured to the nearest 0.1 cm using a wall fixed stadiometer. BMI was evaluated as weight divided by height squared (kg/m2). Waist circumference was measured at a level midway between the lowest rib margin and the iliac crest in a horizontal plane using a steel measuring tape. Hip circumference was measured at the widest point over the buttocks. Thigh circumference was measured directly below the gluteal fold in the left leg.[13] WHR was calculated as waist circumference divided by hip circumference and WTR was calculated as waist circumference divided by thigh circumference. Lower segment was measured from the pubic symphysis to the plantar surface of the foot and upper segment was calculated by subtracting the lower segment measurements from the height.
Assessment of physical fitness
Resting blood pressure and heart rate were measured in sitting position in the left upper arm after the participant had rested for at least 15 min, with digital BP recorder (Braun Company). Then the subject was made to exercise for 3 min according to Queen's College Step Test protocol.[14] Blood pressure and heart rate were recorded immediately after exercise. Rate Pressure Product was determined as the product of heart rate and systolic blood pressure divided by 1000, at rest and immediately after exercise.
Physical Fitness Index[15] was calculated by
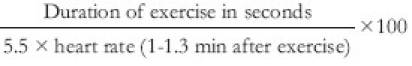
Statistical analysis
Statistical analysis between cases and controls was done by unpaired t-test for parameters, such as BMI, WHR, WTR, US/LS, PFI, and RPP, using SPSS software (version 15.0).
RESULTS
The results are expressed as mean ± standard deviation. The mean age and the distribution of cases and controls with respect to gender are shown in Table 1. Table 2 and Figure 1 show the various anthropometric indices among cases and controls. There is a significant increase (P < 0.05) in the BMI, WHR, and US/LS ratio in cases, whereas WTR was not significant (P > 0.05). The anthropometric values are high in apparently healthy individuals with a family history of type-2 Diabetes Mellitus than in the controls.
Table 1.
Distribution of cases and controls
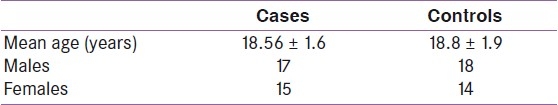
Table 2.
Anthropometric indices
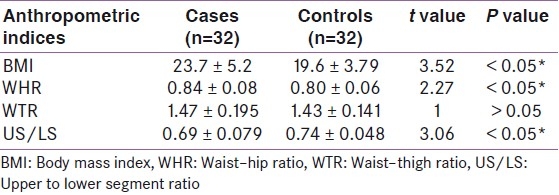
Figure 1.
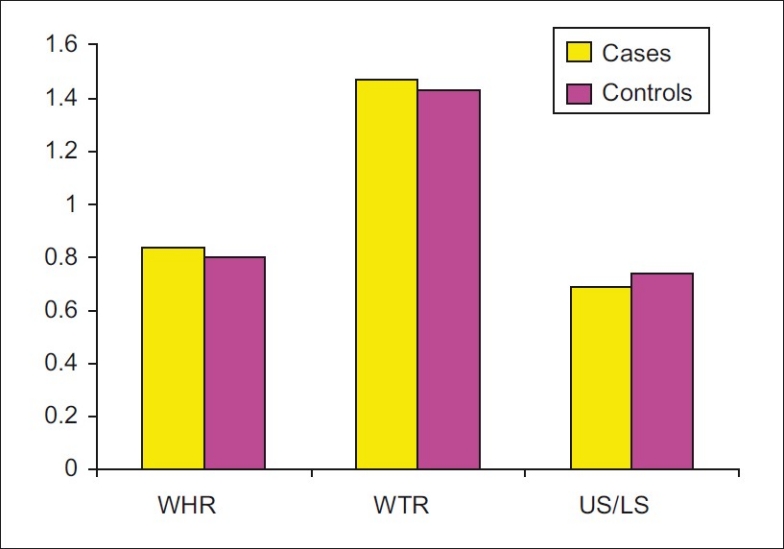
Anthropometric indices
The individuals with a family history of type-2 Diabetes Mellitus have lower physical fitness index than the controls [Table 3]. The resting rate pressure product (RPP) was more in cases than in controls and increase in RPP after exercise was less in cases [Table 4, Figure 2].
Table 3.
Physical fitness index
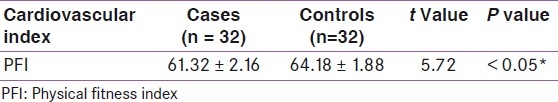
Table 4.
Rate pressure product
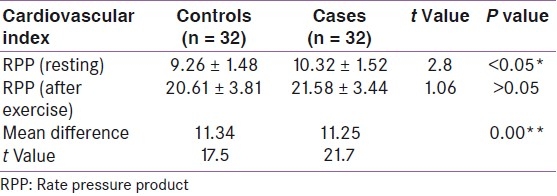
Figure 2.
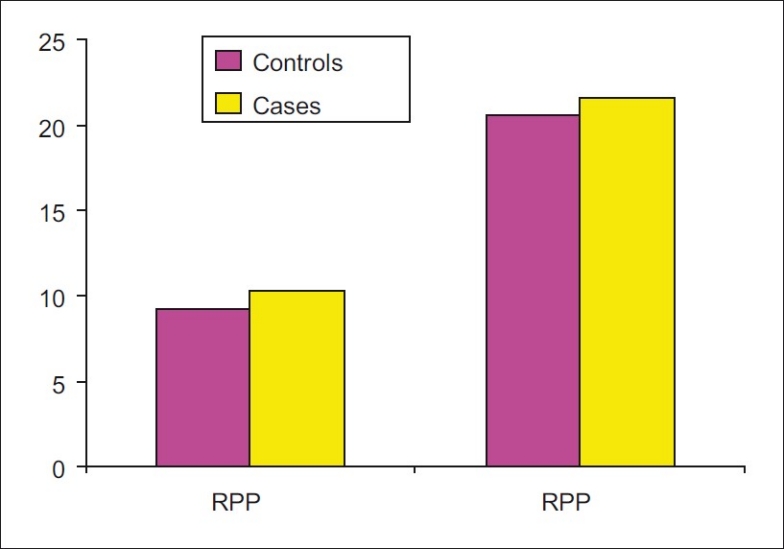
Rate pressure product before and after exercise
DISCUSSION
In a prospective study of 14 years by Sawada et al.,[16] in Japanese men, it was reported that a low cardiorespiratory fitness is associated with a higher risk of developing type-2 diabetes. Wei et al.[17] found a significant inverse relationship between cardiorespiratory fitness (measured by treadmill time) and the incidence of type-2 diabetes. Anthropometric indices in obese and type-2 diabetics are gaining lot of importance at present because of its feasibility and accuracy. There are no studies till date regarding the anthropometry and cardiovascular fitness in offsprings of type-2 diabetics who are the probable future sufferers of either diabetes or cardiovascular disorders or obesity. The present study reveals a lower physical fitness in individuals with a family history of diabetes, which could be due to their higher anthropometric values, and this could also predispose to type-2 diabetes.
The lesser thigh circumference in cases goes in favor of type-2 diabetes, which was studied and proved by Snijder et al.,[13] wherein it was found that there was a better glucose tolerance with larger thigh and hip circumference.
The limitations of this study were that we did not consider 1° relatives or 2° relatives in particular. Grossly their family history of type-2 diabetes was taken into consideration. This study is a pilot study with a small sample considering only the 1st MBBS students of SNMC, Bagalkot. The study needs to be extended to the entire population of Bagalkot urban, which is our future project.
It can be concluded that apparently healthy individuals with a family history of type-2 Diabetes Mellitus have higher anthropometric values and lower physical fitness than the controls. Hence, a check on these parameters may help in controlling the predisposing factors and therefore diabetes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sande MV, Walraven GL, Milligan PM, Banya WS, Caesay S, Nyan O, et al. Family history: An opportunity for early interventions and improved control of hypertension, obesity and diabetes. Bull World Health Organ. 2001;79:321–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Ohlson LO, Larsson B, Svardsudd K, Welin L, Eriksson H, Wilhelmsen L, et al. The influence of body fat distribution on the incidence of diabetes mellitus. 13.5 years of follow-up in the participants in the study of men born in 1913. Diabetes. 1985;34:1055–8. doi: 10.2337/diab.34.10.1055. [DOI] [PubMed] [Google Scholar]
- 3.Helmrich SP, Ragland DR, Leung RW, Paffenbarger RS., Jr Physical activity and reduced occurrence of non-insulin dependent diabetes mellitus. N Engl J Med. 1991;325:147–52. doi: 10.1056/NEJM199107183250302. [DOI] [PubMed] [Google Scholar]
- 4.Barnett AH, Eff C, Leslie RD, Pyke DA. Diabetes in identical twins.A study of 200 pairs. Diabetologia. 1981;20:87–93. doi: 10.1007/BF00262007. [DOI] [PubMed] [Google Scholar]
- 5.Pierce M, Keen H, Bradley C. Risk of diabetes in offspring of parents with non-insulin dependent diabetes. Diabet Med. 1995;12:6–13. doi: 10.1111/j.1464-5491.1995.tb02054.x. [DOI] [PubMed] [Google Scholar]
- 6.Dalton M, Cameron AJ, Zimmet PZ, Shaw JE, Jolley D, Dunstan DW, et al. Waist circumference, waist-hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. J Intern Med. 2003;254:555–63. doi: 10.1111/j.1365-2796.2003.01229.x. [DOI] [PubMed] [Google Scholar]
- 7.Han TS, McNeill G, Seidell JC, Lean ME. Predicting intra-abdominal fatness from anthropometric measures: The influence of stature. Int J Obes Relat Metab Disord. 1997;21:587–93. doi: 10.1038/sj.ijo.0800446. [DOI] [PubMed] [Google Scholar]
- 8.Lemieux S, Prud’homme D, Bouchard C, Tremblay A, Despres JP. A single threshold value of waist girth identifies normal-weight and overweight subjects with excess visceral adipose tissue. Am J Clin Nutr. 1996;64:685–93. doi: 10.1093/ajcn/64.5.685. [DOI] [PubMed] [Google Scholar]
- 9.Sedell JC, Han TS, Feskens EJ, Lean ME. Narrow hips and broad waist circumferences independently contribute to increased risk of non-insulin dependent diabetes mellitus. J Intern Med. 1997;242:401–6. doi: 10.1046/j.1365-2796.1997.00235.x. [DOI] [PubMed] [Google Scholar]
- 10.Seidell JC, Perusse L, Despres JP, Bouchard C. Waist and hip circumferences have independent and opposite effects on cardiovascular disease risk factors: The Quebec Family Study. Am J Clin Nutr. 2001;74:315–21. doi: 10.1093/ajcn/74.3.315. [DOI] [PubMed] [Google Scholar]
- 11.Pontiroli AE, Monti LD, Costa S, Sandoli PE, Pizzini A, Solerte SB, et al. In middle-aged siblings of patients with type 2 diabetes mellitus, normal glucose tolerance is associated with insulin resistance and with increased insulin secretion.The SPIDER study. Eur J Endocrinol. 2000;143:681–6. doi: 10.1530/eje.0.1430681. [DOI] [PubMed] [Google Scholar]
- 12.Shigetoh Y, Adachi H, Yamagishi S, Enomoto M, Fukami A, Otsuka M. Higher heart rate may predispose to obesity and diabetes mellitus: 20-year prospective study in a general population. Am J Hypertens. 2009;22:151–5. doi: 10.1038/ajh.2008.331. [DOI] [PubMed] [Google Scholar]
- 13.Snijder MB, Dekker JM, Visser M, Yudkin JS, Stehouwer CD, Bouter LM, et al. Larger thigh and hip circumferences are associated with better glucose tolerance: The Hoorn study. Obes Res. 2003;11:104–11. doi: 10.1038/oby.2003.18. [DOI] [PubMed] [Google Scholar]
- 14.Sadhan B, Koley S, Sandhu JS. Relationship between cardiorespiratory fitness, body composition and blood pressure in Punjabi collegiate population. J Hum Ecol. 2007;22:215–9. [Google Scholar]
- 15.Choudhuri D, Choudhuri S, Kulkarni VA. Physical fitness: A comparative study between students of residential (Sainik) and non-residential schools (aged 12-14 years) Indian J Physiol Pharmacol. 2002;46:328–32. [PubMed] [Google Scholar]
- 16.Sawada SS, Lee I, Muto T, Matuzaki K, Blair SN. Cardiorespiratory fitness and the incidence of type 2 diabetes. Diabetes Care. 2003;26:2918–22. doi: 10.2337/diacare.26.10.2918. [DOI] [PubMed] [Google Scholar]
- 17.Wei M, Gibbons LW, Mitchell TL, Kampert JB, Lee CD, Blair SN. The association between cardiorespiratory fitness and impaired fasting glucose and type 2 diabetes mellitus in men. Ann Intern Med. 1999;130:89–96. doi: 10.7326/0003-4819-130-2-199901190-00002. [DOI] [PubMed] [Google Scholar]


