Abstract
Objectives
Few studies have examined dentists' subjective ratings of importance of caries risk factors or tested whether dentists use this information in treatment planning. This study tested several hypotheses related to caries risk assessment and individualized caries prevention.
Methods
Data were collected as part of a questionnaire entitled “Assessment of Caries Diagnosis and Caries Treatment”, completed by 547 practitioners who belong to The Dental Practice-Based Research Network (DPBRN), a consortium of participating practices and dental organizations.
Results
Sixty-nine percent of DPBRN dentists perform caries risk assessment on their patients. Recently-graduated dentists, dentists with busier practices, and those who believe a dentist can predict future caries were the most likely to use caries risk assessment. The association between caries risk assessment and individualized prevention was weaker than expected (r=.21). Dentists who perform caries risk assessment provide individualized caries prevention to 57% of their patients, compared to 42% for dentists who do not perform caries risk assessment. Based on their responses to radiographic and clinical scenarios in the questionnaire, dentists who use caries risk assessment appear to use this information in restorative decisions.
Conclusion
A substantial percentage of DPBRN dentists do not perform caries risk assessment, and there is not a strong linkage between its use and use of individualized preventive regimens for adult patients. More progress in implementation of current scientific evidence in this area is warranted.
INTRODUCTION
The potential for utilizing approaches that incorporate risk assessment as an integral component of a caries management strategy has been demonstrated (1–3). The first step in this process is the consideration of each patient's caries risk. Risk assessment is the determination of the probability of a person's developing new carious lesions during a specific period and of the probability of a change in the size or activity of existing lesions across time (4–6). This risk determination for each patient is then followed by the implementation of an individualized caries prevention program or intervention strategy (7,8).
A small number of key disease indicators (e.g., socioeconomic status) and risk factors (e.g., microflora) determine whether the individual is at low, moderate, or high risk, although most of this type of research has been conducted with children, not adults (9). The clinician's subjective assessment has also been documented as a valid means to assess caries risk (10,11). Few studies have examined dentists' subjective ratings of the importance of specific caries risk factors or tested whether dentists use this information in treatment planning (12,13).
The Dental Practice-Based Research Network (DPBRN) allowed us to examine caries risk assessment and subjective caries risk factors, and test whether they are linked to use of individualized caries prevention regimens for adult patients. Therefore, the aims of this study were to: 1) quantify dentist's subjective ratings of the importance of specific caries risk factors; 2) quantify the percentage of dentists who report using caries risk assessment on adult patients and to test the hypothesis that certain practice, dentist, and patient characteristics are associated with its use; 3) test the hypothesis that dentists who use caries risk assessment use this information to make clinical decisions; 4) test the hypothesis that dentists who perform caries risk assessment provide individualized caries prevention to a greater percentage of their adult patients than dentists who do not perform caries risk assessment.
METHODS
Network Dentists
DPBRN is a consortium of participating practices and dental organizations committed to advancing knowledge of dental practice and ways to improve it. DPBRN comprises five regions: AL/MS: Alabama/Mississippi, FL/GA: Florida/Georgia, MN: dentists employed by HealthPartners [ref: HealthPartners® (2009) Retrieved online January 15, 2010 from http://www.healthpartners.com/] and private practitioners in Minnesota, PDA: Permanente Dental Associates [ref: PDA: Permanente Dental Associates (2009) Retrieved online January 15, 2010 from http://xnet.kp.org/pda/index.html] in cooperation with Kaiser Permanente Center for Health Research, and SK: Denmark, Norway, and Sweden. DPBRN has a wide representation of practice types, treatment philosophies, and patient populations, including diversity with regard to the race, ethnicity, geography and rural/urban area of residence of both its practitioner-investigators and their patients (14). Analyses of these characteristics confirm that DPBRN dentists have much in common with dentists at large (15), while at the same time offering substantial diversity with regard to these characteristics (16).
Procedure
As part of the enrollment process, DPBRN dentists complete the DPBRN Enrollment Questionnaire, during which they provide information about themselves and their practices. A questionnaire entitled “Assessment of Caries Diagnosis and Caries Treatment Questionnaire” was subsequently sent to DPBRN member dentists who reported on the Enrollment Questionnaire that they do at least some restorative dentistry. This latter questionnaire asked a range of questions including about caries related diagnostic and clinical decision-making processes, caries risk assessment, and use of prevention techniques. These questionnaires are publicly available at the DPBRN Supplement page [ref: Dental Practice-Based Research Network. Supplements to specific DPBRN publications. (2010) Retrieved online January 15, 2010 from www.dentalpbrn.org/users/publications/Supplement.aspx].
This manuscript focuses on data related to caries risk assessment. The 564 DPBRN dentists who returned the caries questionnaire represent an overall return rate of 58%. There were no significant differences in participation by gender, area of specialty, or years since dental school graduation compared to non-respondents. Five hundred forty-seven of the dentists who completed the survey and perform restorative dentistry based on follow-up information from the regional center are included in this report. This comprised 445 male dentists (81%) and 102 female dentists (19%). Participating dentists were distributed by region as follows: AL/MS=303, FL/GA=104, HP=31, PDA=51, SK=47. An additional 11 dentists from areas outside of the five regions also completed the survey and are included in the following analyses. Eighty-four percent work on a full-time basis (32+hours per week). A more-detailed presentation of the characteristics of these dentists is publicly available [http://www.dentalpbrn.org/users/publications/Supplement.aspx].
Measures
Caries risk assessment (CRA)
The questionnaire asked network dentists whether they “assess caries risk for individual patients in any way?” If they responded yes, then they were asked if they “record the assessment on a special form that is kept in the patient chart?” The dentist was then asked a series of question about caries risk factors (see Table 1). They were also asked “How strongly do you agree with this statement: “A dentist's assessment of caries risk for a patient can predict whether or not that patient will develop new caries in the future “? The response choices were 1= strongly disagree, 2=somewhat disagree, 3=neither agree nor disagree, 4=somewhat agree, 5=strongly agree.
Table 1.
Ratings of importance of caries risk factors for treatment plan.
| Rating of importance Mean (SD) | |
|---|---|
| Current oral hygiene (n=521) | 4.5 (0.6) |
| Decreased salivary function (n=518) | 4.5 (0.8) |
| Commitment to return for follow-up (n=519) | 4.1 (0.8) |
| One or more active caries (n=523) | 4.1 (0.9) |
| Current diet (n=523) | 3.9 (0.9) |
| Dentist's subjective assessment (n=523) | 3.9 (0.9) |
| Recent caries (n=522) | 3.8 (0.8) |
| Patients understanding of caries progression (n=521) | 3.8 (0.8) |
| Presence of dental appliances (n=520) | 3.7 (0.9) |
| Presence of several large restorations (n=522) | 3.6 (0.9) |
| Recession of root exposure (n=507) | 3.6 (0.9) |
| Current use of fluorides (n=522) | 3.4 (0.9) |
| Age of patient (n=520) | 3.3 (0.9) |
| Socioeconomic status (n=520) | 2.7 (1.0) |
Network dentists rated these risk factors that were preceded with the following question: How important is each of the factors below when you decide on a treatment plan? Scoring: 1=not at all important, 2=slightly important, 3=moderately important, 4=very important, 5=extremely important.
Individualized caries prevention (ICP)
ICP was assessed by asking: “On what percentage of patients in your practice do you provide an individualized caries prevention regimen?” Dentists were also asked “What percentage of patients in your practice are interested in an individualized caries prevention regimen?” The percentages were coded to the categories' medians as follows to maintain the interval nature of the data: 0%=0%, 1–24%=12.5%, 25–49%=37%, 50–74%=62%, 75–99%=87%, 100%=100%.
Caries case scenarios
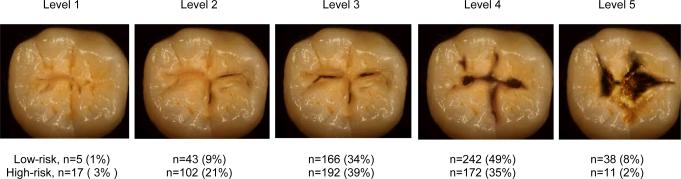
Dentists were given series of scenarios involving interproximal and occlusal lesions that varied on lesion severity/depth. For Figure 1, they were asked to select the treatment they would recommend for each of the coronal surfaces based on the following two clinical scenarios that described a patient of low and high caries risk.
Figure 1.
Percent of dentists who choose to first restore at this level of lesion severity/depth for occlusal lesion (Reprinted from Espelid et al41 with permission)
Note: All dentists chose to restore at subsequently greater lesion severity.
“The patient is a 30-year old female with no relevant medical history. She has no complaints and is in your office today for a routine visit. She has attended your practice on a regular basis for the past 6 years. Low-risk scenario: She has no other restorations than the one shown, no dental caries, and is not missing any teeth. High-risk scenario: She has 12 teeth with existing dental restorations, heavy plaque and calculus, multiple Class V white spot lesions, and is missing 5 teeth.”
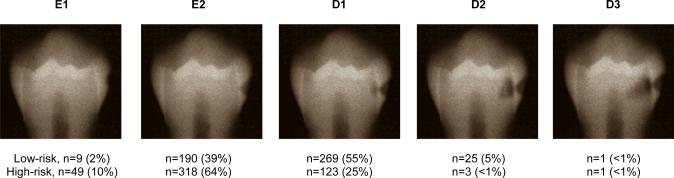
Treatment codes categorized as conservative/preventive were: no treatment today, follow the patient regularly; instruct the patient in plaque removal for the affected area; in-office fluoride; prescription fluoride; recommend non-prescription fluoride; use sealant or unfilled resin over the tooth; chlorhexidine treatment; minimal drilling and sealant; minimal drilling and preventive resin restoration; air abrasion and a sealant; air abrasion and preventive resin restoration. Codes categorized as restoration were: amalgam restoration; composite restoration; indirect restoration. When multiple codes were selected, the treatment was scored as “restoration” if any of the restoration codes were endorsed. For example, if the treatment codes for Levels 1–3 were in-office fluoride, codes for Level 4–5 were in-office fluoride and composite restoration, this case was scored as Level 4. For Figure 2, dentists were asked to circle the lesion depth at which they think it is best to do a permanent restoration for each of the clinical scenarios. Level 1/E1 was scored 1, Level 2/E2 as 2, Level 3/D1 as 3, etc., with scores ranging from 1–5.
Figure 2.
Percent of dentists who chose to first restore at this level of lesion severity for the interproximal lesion. (Reprinted from Espelid et al41 with permission)
Note: All dentists chose to restore at subsequently deeper lesions depth.
Each of these four variables (“interproximal low-risk”, “interproximal high-risk”, “occlusal low-risk”, “occlusal high-risk”) represent an intent to restore treatment continuum based in lesion severity/depth what we refer to as a “restoration index”. We also calculated two risk variables where the level of restorative intervention for the higher-risk patient scenario was subtracted from low-risk scenario for both the occlusal lesion and proximal lesion (“interproximal risk”, “occlusal risk”). These variables reflect a change in the treatment continuum based on patient risk and were coded 0=restoration at the same stage and 1=postpone the restoration. We interpret these “risk index” variables to reflect a dentist whose treatment decisions “were” and “were not” influenced by perceived risk.
Statistical methods
Descriptive statistics were calculated for the caries risk assessment questions. A logistic regression model was used to test for practice, dentist, and patient characteristics as predictors of CRA. ICP was not used as a predictor of CRA because, theoretically, risk assessment would be a clinical precursor to ICP. Associations between CRA and the restoration indices and then risk indices were tested separately in a second step. A backward elimination approach was used in step 2 that removed the least significant index variable from the model in subsequent steps until all remaining variables were significant using p <0.10 for retention (17). Linear regression was used to test for significant associations between the percent of patients who receive ICP and the CRA and “dentists can predict future caries” variables. Practice, dentist, and patient characteristics were entered in the first step as covariates, and the two caries assessment variables were entered in a second step as described above. Caries risk assessment (no=0, yes=1), gender (male=0, female=1); SK region (US regions=0, SK region=1), type of practice model (PHS/LGP=0, PP=1) were coded as indicated. Dentists associated with PDA or HealthPartners were categorized as large group practice model (LGP). Other practices were assigned by regional coordinators to the categories of private practice (PP) or public health service (PHS). It is acknowledged that some dentists assigned to a private practice model were also members of small (less than 4 dentists) group practices. An alpha level of .05 was used as the level for statistical significance.
RESULTS
Importance of risk factors
Of the 547 eligible dentists, 490 completed all of the questions about caries risk factors and consequently are included in the following analyses. Completers and non-completers did not differ in gender, region, or practice model, graduation year, number of days patients wait for an exam appointment, or percentage of time spent doing restorative dentistry procedures. However, dentists who completed all of the caries risk items reported were more likely to perform CRA than those who did not complete all of the caries risk questions [χ2 (1) =6.639, p=.010]. Ratings of importance of caries risk factors for treatment planning are presented in Table 1. Current oral hygiene, decreased salivary flow, commitment to return for follow-up, and one or more active caries were rated as the most important risk factors, whereas the patient's age and socioeconomic status were rated as the least important.
Case scenarios
The distributions for restoration indices are presented in Figures 1 and 2. Fifty-three dentists did not complete all four clinical scenarios; consequently, risk indices were calculated for 494 dentists. The occlusal risk index indicated that 182 (37%) dentists would postpone the restorative treatment on the lower-risk patient and 312 (63%) would surgically restore at the same level of caries lesion depth. The interproximal risk index indicated that 230 (47%) dentists would delay the restoration on the low-risk patient and 264 (53%) at the same level of caries development.
Caries risk assessment
Sixty-nine percent (n=379) of the dentists reported that they assess caries risk for individual patients in some way. Of those who assess risk, 17% (n=64) use a special form. Practice, dentist, and patient characteristics associated with dentist's assessment of caries risk are presented in Table 2.
Table 2.
Practice, dentist, and patient characteristics associated with dentist's assessment of caries risk.
| Variable | B (SE) | OR (95% CI) | p. value |
|---|---|---|---|
| SK region | 1.299 (.666) | 3.67 (0.99–11.3) | .051 |
| Private practice | −1.747 (.486) | 0.17 (0.07–0.45) | <.001 |
| Years of practice | −.031 (.011) | 0.97 (0.95–0.99) | .006 |
| Days wait for exam appointment | .020 (.010) | 1.02 (1.01–1.04) | .034 |
| Percent of patients that are 65+ | −.100 (.086) | 0.85 (0.71–1.01) | .088 |
| Patients that self-pay for dental treatment | .071 (.055) | 1.07 (0.97–1.24) | .099 |
| Dentist can predict new caries | .270 (.105) | 1.31 (1.07–1.61) | .010 |
| Step 2 for the restoration index | |||
| Interproximal – high risk | .789 (.246) | 2.20 (1.36–3.57) | .001 |
| Step 2 for the risk index | |||
| Occlusal lesion | .387 (.217) | 1.47 (0.97–2.25) | .074 |
| Interproximal lesion | .440 (.212) | 1.55 (1.03–2.35) | .038 |
Coding: Caries risk assessment (no=0, yes=1), gender (male=0, female=1); SK region (US regions=0, SK region=1), private practice model (PHS/LGP=0, PP=1). Dentist can predict caries was coded 1= strongly disagree, 2=somewhat disagree, 3=neither agree or disagree, 4=somewhat agree, 5=strongly agree.
Practice, dentist, and patient model. χ2(9) =70.437, p<.001
Restoration index, Step 2. Δχ2(1) =8.117, p=.004
Risk index, Step 2. Δχ2(2) =6.789, p=.041
Probabilities of p <.10 are shown.
The results of logistic regression indicated that increased likelihood of practicing CRA was significantly associated with a PHS or LGP practice model (p<.001), dentists' fewer years in practice (p=.006), greater numbers of days patients wait for an exam appointment (p=.034), and the dentists' belief that they can predict future caries variable (p=.010). In the second step, only the restoration index for the interproximal high-risk case was significantly associated with CRA, and indicated that dentists who perform CRA would perform a restoration at a later lesion stage for this case than dentists who do not perform CRA. The risk indices from the occlusal and interproximal scenarios were both significant and combined to significantly improve the risk model at the second step, indicating that dentists who delayed a restoration to a later stage for the low-risk patients compared to the high-risk case were more likely to perform CRA than dentists who chose to restore at the same lesion level for both patients. Regression coefficients are presented in Table 2.
Individualized caries prevention
Practice, dentist, and patient characteristics associated with the percentage of patients that receive individualized caries prevention are presented in Table 3. Network dentists reported that 52% (SD=34) of their patients received ICP and 40% (SD=29) of their patients are interested in ICP. These two ICP variables correlated r=.60, p<.001; consequently, the patient's interest variable was not used in the regression models because of multicollinearity. Dentists who perform caries risk assessment provide individualized caries prevention to 57% (SD=34) of their patients, compared to 42% (SD=32) for dentists who do not perform caries risk assessment. Dentist responses to the statement that a dentist can predict the development of caries in the future was as follows: 24% (n=134) strongly agreed, 53% (n=284) somewhat agreed, 12% (n=65) were neutral, 7% (n=39) somewhat disagreed, and only 3% (n=17) strongly disagreed with the statement.
Table 3.
Practice, dentist, and patient characteristics associated with the percentage of patients who receive individualized caries prevention.
| Variable | B (SE) | t | p. value |
|---|---|---|---|
| SK region | −15.598 (6.360) | −2.453 | .015 |
| Private practice | −28.057 (4.595) | −6.106 | <.001 |
| Gender (female) | 15.341 (3.983) | 3.852 | <.001 |
| Years of practice | .266 (.145) | 1.835 | .067 |
| Days wait for exam appointment | .198 (.094) | 2.108 | .036 |
| Patients that self-pay for dental treatment | 2.101 (.736) | 2.854 | .005 |
| Percent of time spent on restorative work | −1.470 (.719) | 2.044 | .041 |
| Step 2 – risk assessment | |||
| Dentist can predict new caries | 3.857 (1.499) | 2.574 | .010 |
| Performs caries risk assessment | 11.404 (3.229) | 3.532 | <.001 |
Coding: Caries risk assessment (no=0, yes=1), gender (male=0, female=1); SK region (US regions=0, SK region=1), private practice model (PHS/LGP=0, PP=1). Dentist can predict caries was coded 1= strongly disagree, 2=somewhat disagree, 3=neither agree or disagree, 4=somewhat agree, 5=strongly agree.
Step 1. F=9.050, p<.001, R2=.13.
Step 2. F to change =9.792, p=.001, ΔR2=.04.
Probabilities of p<.10 are shown.
Although statistically significant, the correlation between caries risk assessment and the percentage of patients who receive individualized caries prevention was modest (r=.21, p<.001). Multiple regression indicated that dentists from the US regions (p=.015), LGP or PHS practice model (p<.001), female gender (p<.001), greater numbers of days patients wait for an exam appointment (p=.036), greater percentage of patients who are 65+ years of age (p<.001), and less income from restorative work (p=.041) were associated with providing individualized caries prevention to a greater percentage of patients. In the second step, “the dentist can predict future caries” variable and the CRA variable were both significantly positively associated with providing ICP to a greater percentage of patients (p=.01 and p<.001, respectively). The parameter estimate for the CRA variable indicated that dentists who practice caries risk assessment provide, on average, ICP to 11% more of their patients than dentists who do not perform CRA.
DISCUSSION
The 2001 National Institutes of Health Consensus Statement officially recognized the paradigm shift in caries management toward more-conservative treatment of caries (18). As a result, current standards of care recommend that treatment planning for caries include a risk assessment for each patient so that an individualized prevention and treatment program could be developed (7,19,20). Whether most dentists incorporate some form of CRA into their practices based on their overall impression of the patient is poorly documented in the literature. Some authors have suggested that risk information is not effectively used in treatment decisions (12,13).
This study found that the majority of DPBRN dentists practice some form of CRA. We are unable to find another peer-reviewed study that has reported rates of CRA for adult patients. However, a recent postal survey of members of the Texas Academy of Pediatric Dentists provides a non-network comparison (21). They reported that 36% of the respondent 204 practices provided CRA on more than 76% of their patients and only 9% of dentists did not assess caries risk. Our study did not ask the percentage of patients who receive CRA, but asked whether it was performed on patients in the practice. Similar to our methodology, a survey of dentists practicing in the city of Indianapolis, Indiana found that 72% of respondents used some type of risk assessment (13).
What types of dental practices are using CRA?
The current emphasis on CRA in the didactic and clinical curriculum of dental schools indicates that dental students receive training in these skills (22,23). Higher use in clinical practice among recent graduates is consistent with the notion that students leave dental school confident in their abilities to determine caries risk. This is supported by data that showed fourth-year dental students scored significantly higher than first-year students on knowledge about caries risk, and by another study that found 80% of dental students rated a CRA form as easy to use and that they would assess caries risk in their clinical practice (24). Consistent with the above hypothesis, members of the DPBRN who were more-recent dental school graduates were more likely to be using CRA in their practices. In fact, 83% of network dentists with 10 or fewer years of practice reported performing CRA, compared to only 67% of dentists with 11+ years of practice and 60% of dentists with 30+ years of practice. Consequently, there is a clear pattern of higher use among those with more-recent dental training, although even the majority of the most-senior practitioners have incorporated CRA into their practices. Nevertheless, our data indicate that some dentists may not use CRA if they do not believe in their ability to predict future caries activity.
The busiest practices were the most likely to be performing CRA. Our data do not allow us to explain why; however, it is possible that patients are more drawn to dental offices that practice the most-up-to-date techniques, perhaps because of better treatment outcomes associated with CRA. In addition, we do not know whether the dentist or an auxiliary within the practice is performing the CRA. Another finding was that the dentists practicing in a large group setting (or public health clinics) were more likely to perform CRA. In these practices, clinical decisions may be influenced more by organizational standards and less by personal judgment (25). The SK region variable approached significance, suggesting that Scandinavian dentists may be more likely to use CRA. The SK region was underrepresented in the DPBRN sample and this reduction in statistical power may have restricted our ability to detect a difference in its use of CRA.
Our data also support the hypothesis that dentists who use CRA have different thresholds for lesion restoration than dentists who do not perform CRA, as both clinical restoration indices were associated with assessing caries risk. Dentists who would restore lesions at lower depth of caries progression based on radiographic images were less likely to perform CRA than dentists who chose to postpone the surgical treatment for one of the high-risk cases. It is possible that dentists without the benefit of the information from a risk assessment would chose to opt for surgical intervention. We also found that dentists who practice CRA are more likely to consider risk in their clinical decisions. This could be interpreted to indicate that the use of CRA allows dentists to better adjust/tailor clinical decisions to specific patients based on caries risk, rather than using a single criterion for the restoration of carious lesions.
A special form was used by 17% of network dentists. Trueblood et al (21) found that among Texas pediatric dentists, 39% of respondents used both verbal and written caries risk assessments. A study at a US dental school that examined the impact of initiating the use of a CRA form found that faculty were slow to incorporate its use, but by the end of the second year, a level of 80% compliance was reached (26). The authors suggested that the faculty, some of whom may have been trained at a time when caries restoration was the standard treatment for caries, were skeptical about the importance of CRA in a caries management program.
Does caries risk assessment precede individualized caries prevention?
Successful use of regular CRA is based on the assumption that patients who are at increased risk will be identified, and that once identified; these patients will receive the appropriate treatment to reduce the likelihood that caries will occur or progress (2,3,9). Empirically supported treatments include fluoride, sealants, and anti-bacterial rinses (6). Some data suggest that patients who are at high risk of developing disease are not necessarily receiving the needed preventive or management therapy (27). Results from the current study suggest that only about 50% of patients of network practitioners receive ICP.
There have been multiple reasons proposed for why not all dental patients would receive caries preventive agents based on their need. Underutilization of an effective preventive agent in adults at risk has been noted previously (10) and may reflect clinicians' reluctance to recommend preventive treatments not covered by insurance plans or lack of knowledge about its effectiveness (28,29). Similarly, preventive and conservative interventions for caries may not be used because practitioners believe the evidence regarding the effectiveness of this approach is lacking (30). Our data suggest that some dentists may lack confidence in the validity of CRA. In either case, restorations could be placed regardless of patient risk or the radiographic depth of the lesion. It has been suggested that practicing dentists may lack the skills to evaluate the scientific literature or that they may not know where to access information on the best current evidence in dentistry (25,31). For whatever reason, our data are consistent with other studies that indicate there is considerable variability in clinical practice related to caries regardless of where the study was performed (32–36).
CRA was associated with higher use of ICP, but the association was weaker than expected. The zero-order correlation was a modest r = .21 and when adjusting for the control variables in the multivariate model, dentists who perform CRA provided ICP to an additional 11% of their patients. Post-hoc data analysis indicated that 66 of the 195 dentists who do not assess caries risk, reported providing ICP from 25% to 74% of their patients. The basis for ICP among dentists who do not assess patient caries risk is unclear. A disconnect between ICP and CRA was also seen by Bahleda and Fontana (13), who found that only 51% of dentists provided a treatment or management plan based on the patient's risk status for adult patients with a white-spot lesion. Less-than-optimal treatment follow-up after CRA has also been reported in a predoctoral teaching clinic. In this program, patients assessed as having high caries risk were supposed to receive a bacterial assessment however this was not followed in most cases (26). On the other hand, a study by Bader et al (27) has shown that when dentists performed CRA, patients at higher risk did receive more caries treatment than patients with lower levels of risk.
That the SK region was less likely to use ICP was surprising because in northern Europe, an overtly preventive philosophy has existed for many years (37,38). However, these countries make greater use of population-based prevention that includes the widespread use of public education, increased oral hygiene, and an emphasis on improved diet (39).
Importance of caries risk factors
Several caries risk factors and indicators have been proposed as targets for CRA (5–7,9). However, there are few studies that report the perspectives of practicing dentists. DPBRN dentists rated current oral hygiene and salivary flow as the two most important risk factors. The Trueblood (21) study found a very different set of responses, with dentists selecting diet and caries history as the most important. A study from a national dental insurance carrier that examined practitioners' reasons for assigning risk level found that multiple restorations, multiple carious lesions, poor oral hygiene, and exposed root surfaces accounted for the vast majority of assignments in both high- and moderate-risk patients (27). Consequently, there appears to be little consensus among practicing dentists towards prioritizing caries risk factors. A potential limitation of this study was that we did not specify a time period in the series of questions about risk factor importance. However, the goal was to capture dentist's priorities in the context of their practice and we suggest each dentist used their own idiosyncratic time period in each rating which indicates the importance of each risk factor.
Bader and colleagues have suggested that risk classification should be based on current caries activity and prior caries experience, with all other caries risk factors applied at the dentist's discretion (11). Their data indicated that consideration of prior caries experience improves the sensitivity of a CRA compared to using current caries activity only. The Bader study also supports the conclusion that dentists subjective judgment can contribute to overall success through greater sensitivity. It should be noted that patients who do not have active disease or clinical signs of caries are not necessarily at low-risk of developing the disease (40).
It is acknowledge that some dentists chose to first restore at relatively late stages in the clinical scenarios. The reader is reminded that no dentist chose not to restore at level 5/D3, rather the correct interpretation is that some chose not to restore at level 4/D2. Evidence that supports that dentists correctly understood and responded to the scenarios is the consistency of their responses. For example, 33 of the 38 dentists who choose D3 for the low-risk case also chose D2 or D3 for the high-risk case. Furthermore, dentists who chose this conservative approach were among the most likely to provide individualized caries prevention for their patients.
Clinical implications and conclusion
Models of CRA are still being developed' as are evidenced-based definitions for risk factors (6,9,11,31). Our understanding of caries as a disease of multifactorial etiology certainly requires that CRA evaluate a wide range of variables so that factors responsible for caries in a particular patient can be identified. It is also true that no single model can be recommended for all patients; rather multiple risk assessment models are needed. For example, a practice with a 12-month recall system will require a different model than some public health models wherein patients may not return for several years.
We found that just over two-thirds of network dentists perform CRA on their patients and recently-trained dentists are more likely to use CRA than their colleagues with older tenure. The connection between CRA and individualized prevention was weaker than we expected. However, we found that dentists who use CRA appear to use this information in clinical decisions involving the timing of when to restore a tooth. It is incumbent on dental schools and professional associations to promote CRA as the current standard of care and educate dentists on how to better use this information in treatment and prevention of caries.
Acknowledgement
This investigation was supported by National Institutes of Health, National Institute of Dental and Craniofacial Research grants U01-DE-16746 and U01-DE-16747. An Internet site devoted to details about DPBRN is located at www.DPBRN.org. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully.
References
- 1.Anderson MH, Omnell KA. Modern management of dental caries: the cutting edge is not the dental bur. N Mexico Dent J. 1995;46(1):10–4. [PubMed] [Google Scholar]
- 2.Pitts NB. Risk assessment and caries prediction. J Dent Educ. 1998;62:762–70. [PubMed] [Google Scholar]
- 3.Powell L. Caries risk assessment: relevance to the practitioner. J Am Dent Assoc. 1998;129:349–53. doi: 10.14219/jada.archive.1998.0209. [DOI] [PubMed] [Google Scholar]
- 4.Reich E, Lussi A, Newbrun E. Caries-risk assessment. Int Dent J. 1999;49(1):15–26. doi: 10.1111/j.1875-595x.1999.tb00503.x. [DOI] [PubMed] [Google Scholar]
- 5.Fontana M, Zero DT. Assessing patients' caries risk. J Am Dent Assoc. 2006;137(9):1231–1239. doi: 10.14219/jada.archive.2006.0380. [DOI] [PubMed] [Google Scholar]
- 6.Twetman S, Fontana M. Patient caries risk assessment. Monogr Oral Sci. 2009;21:91–101. doi: 10.1159/000224214. [DOI] [PubMed] [Google Scholar]
- 7.Fontana M, Young DA, Wolff MS. Evidence-based caries, risk assessment, and treatment. Dent Clin North Am. 2009;53(1):149–61. doi: 10.1016/j.cden.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Jenson L, Budenz AW, Featherstone JD, Ramos-Gomez FJ, Spolsky VW, Young DA. Clinical protocols for caries management by risk assessment. J Calif Dent Assoc. 2007;35(10):714–23. [PubMed] [Google Scholar]
- 9.Zero D, Fontana M, Lennon AM. Clinical applications and outcomes of using indicators of risk in caries management. J Dent Educ. 2001;65(10):1126–32. [PubMed] [Google Scholar]
- 10.Bader JD, Perrin NA, Maupomé G, Rindal B, Rush WA. Validation of a simple approach to caries risk assessment. J Public Health Dent. 2005;65(2):76–81. doi: 10.1111/j.1752-7325.2005.tb02790.x. [DOI] [PubMed] [Google Scholar]
- 11.Bader JD, Perrin NA, Maupomé G, Rush WA, Rindal BD. Exploring the contributions of components of caries risk assessment guidelines. Community Dent Oral Epidemiol. 2008;36(4):357–62. doi: 10.1111/j.1600-0528.2007.00399.x. [DOI] [PubMed] [Google Scholar]
- 12.Bader JD, Shugars DA. What do we know about how dentists make caries-related treatment decisions? Community Dent Oral Epidemiol. 1997;25(1):97–103. doi: 10.1111/j.1600-0528.1997.tb00905.x. [DOI] [PubMed] [Google Scholar]
- 13.Bahleda L, Fontana M. Indiana University School of Dentistry Proceedings. Printing Partners of Indianapolis; Indianapolis: 2003. Evaluating the use of caries risk assessment procedures by Indianapolis area dentists (abstract P8) p. 25. [Google Scholar]
- 14.Gilbert GH, Bader JD, Litaker MS, Shelton BJ, Duncan RP. Patient-level and practice-level characteristics associated with receipt of preventive dental services: 48-month incidence. J Public Health Dent. 2008;68(4):209–17. doi: 10.1111/j.1752-7325.2007.00069.x. [DOI] [PubMed] [Google Scholar]
- 15.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, DPBRN Collaborative Group Dentists in practice-based research networks have much in common with dentists at large: evidence from The Dental PBRN. Gen Dent. 2009;57(3):270–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, Qvist V, DPBRN Collaborative Group Practices participating in a dental PBRN have substantial and advantageous diversity even though as a group they have much in common with dentists at large. BMC Oral Health. 2009;159:26. doi: 10.1186/1472-6831-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Menard S. Applied Logitic Regression. Sage Publications; Thousand Oaks: 1995. [Google Scholar]
- 18.National Institutes of Health Diagnosis Management of Dental Caries throughout Life. NIH Consensus Statement. 2001;181:1–30. [PubMed] [Google Scholar]
- 19.Young DA, Featherstone JD, Roth JR, Anderson M, Autio-Gold J, Christensen GJ, Fontana M, Kutsch VK, Peters MC, Simonsen RJ, Wolff MS. Caries management by risk assessment: implementation guidelines. J Calif Dent Assoc. 2007;35(11):799–805. [PubMed] [Google Scholar]
- 20.Evans RW, Pakdaman A, Dennison PJ, Howe EL. The Caries Management System: an evidence-based preventive strategy for dental practitioners. Application for adults. Aust Dent J. 2008;53(1):83–92. doi: 10.1111/j.1834-7819.2007.00004.x. [DOI] [PubMed] [Google Scholar]
- 21.Trueblood R, Kerins CA, Seale NS. Caries risk assessment practices among Texas pediatric dentists. Pediatr Dent. 2008;30(1):49–53. [PubMed] [Google Scholar]
- 22.Brown LJ, Kaste LM, Selwitz RH, Furman LJ. Dental caries and sealant usage in U.S. children, 1988–1991: selected findings from the Third National Health and Nutrition Examination Survey. J Am Dent Assoc. 1996;127:335–43. doi: 10.14219/jada.archive.1996.0203. [DOI] [PubMed] [Google Scholar]
- 23.Yorty JS, Brown KB. Caries risk assessment/treatment programs in U.S. dental schools. J Dent Educ. 1999;63(10):745–7. [PubMed] [Google Scholar]
- 24.Nainar SM, Straffon LH. Predoctoral dental student evaluation of American Academy of Pediatric Dentistry's caries-risk assessment tool. J Dent Educ. 2006;70(3):292–5. [PubMed] [Google Scholar]
- 25.Baelum V. Caries management: technical solutions to biological problems or evidence-based care? J Oral Rehabil. 2008;35(2):135–51. doi: 10.1111/j.1365-2842.2007.01784.x. [DOI] [PubMed] [Google Scholar]
- 26.Doméjean-Orliaguet S, Gansky SA, Featherstone JD. Caries risk assessment in an educational environment. J Dent Educ. 2006;70(12):1346–54. [PubMed] [Google Scholar]
- 27.Bader JD, Shugars DA, Kennedy JE, Hayden WJ, Jr, Baker S. A pilot study of risk-based prevention in private practice. J Am Dent Assoc. 2003;134:1195–1202. doi: 10.14219/jada.archive.2003.0354. [DOI] [PubMed] [Google Scholar]
- 28.Wright D, Batchelor PA. General dental practitioners' beliefs on the perceived effects of and their preferences for remuneration mechanisms. Br Dent J. 2002;192(1):46–9. doi: 10.1038/sj.bdj.4801288. [DOI] [PubMed] [Google Scholar]
- 29.Grytten J. Models for financing dental services. A review. Community Dent Health. 2005;22(2):75–85. [PubMed] [Google Scholar]
- 30.Narendran S, Chan JT, Turner SD, Keene HJ. Fluoride knowledge and prescription practices among dentists. J Dent Educ. 2006;70(9):956–64. [PubMed] [Google Scholar]
- 31.Ismail AI, Bader JD, ADA Council on Scientific Affairs and Division of Science. Journal of the American Dental Association Evidence-based dentistry in clinical practice. J Am Dent Assoc. 2004;135(1):78–83. doi: 10.14219/jada.archive.2004.0024. [DOI] [PubMed] [Google Scholar]
- 32.Ghasemi H, Murtomaa H, Torabzadeh H, Vehkalahti MM. Restorative treatment threshold reported by Iranian dentists. Community Dent Health. 2008;25(3):185–90. [PubMed] [Google Scholar]
- 33.Qudeimat MA, Al-Saiegh FA, Al-Omari Q, Omar R. Restorative treatment decisions for deep proximal carious lesions in primary molars. Eur Arch Paediatr Dent. 2007;8(1):37–42. doi: 10.1007/BF03262568. [DOI] [PubMed] [Google Scholar]
- 34.Tubert-Jeannin S, Domejean-Orliaguet S, Riordan PJ, Espelid I, Tveit AB. Restorative treatment strategies reported by French university teachers. J Dent Educ. 2004;68(10):1096–103. [PubMed] [Google Scholar]
- 35.Brennan DS, Spencer AJ. Service patterns associated with coronal caries in private general dental practice. J Dent. 2007;35(7):570–7. doi: 10.1016/j.jdent.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 36.Bader JD, Shugars DA. Variation, treatment outcomes, and practice guidelines in dental practice. J Dent Educ. 1995;59:61–95. [PubMed] [Google Scholar]
- 37.Pitts NB. Clinical diagnosis of dental caries: a European perspective. J Dent Educ. 2001;65(10):972–8. [PubMed] [Google Scholar]
- 38.Lith A, Lindstrand C, Grondahl HG. Caries development in a young population managed by a restrictive attitude to radiography and operative intervention: II. A study at the surface level. Dentomaxillofac Radiol. 2002;31:232–9. doi: 10.1038/sj.dmfr.4600705. [DOI] [PubMed] [Google Scholar]
- 39.Burt BA. Prevention policies in the light of the changed distribution of dental caries. Acta Odontologica Scandinavica. 1998;56:3, 179–86. doi: 10.1080/000163598422956. [DOI] [PubMed] [Google Scholar]
- 40.Beck JD, Kohout F, Hunt RJ. Identification of high caries risk adults: attitudes, social factors and diseases. Int Dent J. 1988;38(4):231–8. [PubMed] [Google Scholar]
- 41.Espelid I, Tveit AB, Mejàre I, Sundberg H, Hallonsten AL. Restorative treatment decisions on occlusal caries in Scandinavia. Acta Odontol Scand. 2001;59(1):21–7. doi: 10.1080/000163501300035724. [DOI] [PubMed] [Google Scholar]