Abstract
Traumatic rupture of the anterior cruciate ligament (ACL) of the knee is one of the most frequent orthopaedic sports' injuries. However, the best operative reconstruction technique is still the focus of current discussions among experts. While single-bundle reconstruction primarily addresses anterior-posterior instability, the anatomical double-bundle reconstruction aims to stabilise anterior-posterior as well as rotational instability. So far no definite evidence to favour the one or the other technique exists due to the lack of an objective method for quantifying rotational knee stability. In this context several authors have recently reported on devices for the analysis of femorotibial rotation. However, most of these tools are still in the developmental stage. Therefore, the aim of this study was (1) to develop a new instrument for assessing rotational knee stability independent from the surrounding soft tissue with an adequate method of analysis and (2) to establish the possible field of application of this device in a human cadaver study. The so-called torsiometer evaluated was designed to assess internal and external knee joint rotation objectively in different flexion angles. Measurements were performed implying internal and external rotation at 90°, 30° and 0° knee flexion with and without intact ACL, respectively. Each measurement revealed valid and reproducible values. The restraint in ACL-absent knees was clearly lower and the course of rotation explicitly higher than in knee joints with intact ACL.
Introduction
Rupture of the anterior cruciate ligament (ACL) is one of the most frequent injuries to be treated in today’s orthopaedic sports surgery [1, 2]. The ACL consists of two functional bundles with the anteromedial bundle (AM) guaranteeing anterior-posterior (AP) and the posterolateral (PL) bundle rotational stabilisation (RS) [3–5]. In this context the current literature does not clearly favour one specific surgical reconstruction technique [6–9]. Recently several authors have recommended the double-bundle technique (DB) as this is considered to restore AP stability as well as RS of the knee joint [10].
For the clinical evaluation of the AP translation the Lachman test [11, 12] is commonly used, whereas the pivot shift test is adequate for the evaluation of rotational instability [13–15]. Regarding an objective assessment of RS, recent studies have presented valuable approaches with the most recent exemplary work of Lorach et al. [16–18]. However, these published methods seem to feature a highly complex stability pattern and are difficult to perform [19]. To the best of our knowledge a widely accepted concept regarding the assessment of the overall stability of the knee joint has not been described and developed so far [20].
Therefore, the aim of our study was (1) to develop a new device for assessing the overall stability of the knee and (2) to evaluate this under in vitro conditions using cadaveric total lower limb specimens.
Materials and methods
Design and development of the device
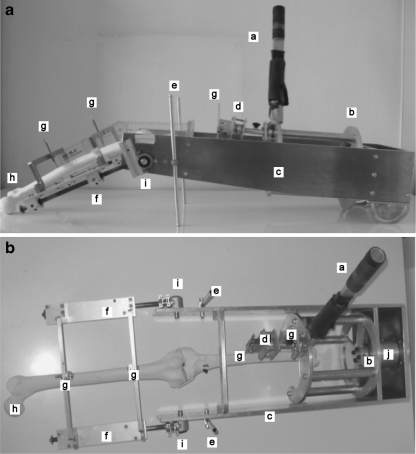
The analysis device, the so-called torsiometer, consists of five major modularly assembled parts (see Fig. 1). To compensate for warp resistance the device’s mount is made of metal. The frame of the device serves as a suspension holder for the femoral and tibial unit. The thigh holding bracket is connected to the frame via a linear conductor allowing for free linear longitudinal sliding. A pivot is used to permit the examination of the knee in different flexion angles. After adjusting the joint line to the turning point of the pivot and centring of the patella, the femoral unit is attached to the main frame. A ball bearing suspension allows for rotational movements of the tibia and serves as a deflection sensor. The thigh is affixed to the femoral unit using Schanz screws in a bicortical fashion (4.5 mm, Synthes, Solothurn, Switzerland). The stress lever and frame are made of aluminium; the stress lever is in addition tared so that no inertia disturbs the measurement and is rectangularly attached to the tibial unit in a neutral position allowing for free tibial rotation to find the position with the lowest predefined tension. This point is defined as the zero point as well as starting point of the measurement in the computer program (LabVIEW 8.0 National Instruments, Austin, TX, USA) when all screws are tightened. The rotational torque is introduced to the tibial unit through the stress lever. For each measurement the stress is manually applied by the same person with the same speed. At each side of the stress lever two precalibrated strain gauges (1-DY-13-3/350, HBM, Darmstadt, Germany) are affixed conducting the applied torque by expansion and electric potential changes. The stress lever is made of aluminium. Due to the material used, the calibration is performed before the lever is attached to the device using temporary (10 s) loading with weights from 0.1 to 5 kg. The potentials produced are recorded and the average value is calculated from 300 measurement points. This factor (k = 8.4 Nm/V) is taken for later measurements. The device’s loading capacity (Analysetool, Catia integrated FEM-Analyse) is planned and designed to bear a maximum torque of up to 100 Nm. All torques are continuously displayed so as not to overstrain either the specimen or the device. Maximum moments never exceeded 35 Nm and the maximum deflection range is limited to 30° to each side within a noncritical range regarding ligamentous ruptures or other injuries. In general, the device can be used in two different versions. For the validation process the invasive method with four-point Schanz screw fixation of the tibia and femur to the device was used. The thigh was fixed in a unilateral way with 20 cm distance between the screws predefined by the femoral unit frame. The tibial fixation was performed using an offset approach at 40° with respect to the longitudinal axis with 10 cm between the screws. The coupling of the Schanz screw mounted leg and the torsiometer was performed using jaw chucks (Synthes, Solothurn, Switzerland) fixed to the frame. The longitudinal axis of the thigh and tibia was ensured by centred fixation points of the bone and frame. To minimise pretension of the screws in relation to their insertion point and to achieve a rectangular drilling, each Schanz screw was inserted into predrilled holes using the jaw chucks as drill guidance.
Fig. 1.
Side view (a) and bird’s-eye view (b) of the torsiometer, consisting of five major parts, which are modularly assembled. a Deflection lever. b Tibia fixation unit. c Main frame. d Fine adjustment. e Stilts. f Shank fixation unit. g Schanz screws. h Sawbone. i Pivot joint. j Potentiometer unit
The other mode that can be used is a non-invasive fashion using two splints, one for the thigh and one boot-like splint to hold the shin and ankle. This mode will be used for future clinical studies on patients.
For the measurement of the rotational movements and angular deflection, a precision potentiometer (Megatron MPA20, Megatron, Munich, Germany) was used. The range of rotational movement is limited to 45° degrees in each direction (for internal and external rotation) due to the construction of the device’s frame (maximum rotation < 30° deflection). The deflection measurements result from the applied torque to the lever and the corresponding expansion of the strain gauges. The strain gauges were connected via a Wheatstone bridge and preloaded with a basic potential representing the unstressed situation. Torques applied produce different potentials and allow the registration of the torsion moment in Nm.
In vitro validation
For the in vitro validation fresh cadaveric total lower limb specimens were used. To overcome the rigor mortis each lower limb specimen underwent ten cycles of maximum passive flexion and extension movements.
Inclusion criteria were intact skin, no fractures, no signs of osteoarthritis, no previous knee surgery, full passive range of motion, intact collateral ligaments and intact ACL and posterior cruciate ligament (PCL). The integrity of the cruciate ligaments was (1) clinically assessed performing the Lachman and the pivot shift tests [11] and (2) confirmed arthroscopically. To exclude bony lesions such as fractures or evidence of osteoarthritis, a computed tomography (CT) scan of each knee was performed, which was read by an expert musculoskeletal radiologist (S. Kirchhoff).
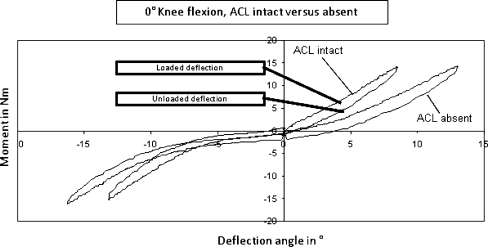
Solid conditions between the limb and the device were achieved using Schanz screws. A calibration of the device was performed before each measurement cycle. The measurements were subdivided into four torque patterns as follows: (1) loaded internal rotation, (2) unloaded internal rotation, (3) loaded external rotation and (4) unloaded external rotation (see Fig. 2). Each fraction’s deflection endpoint was accomplished after approximately 180 measuring points for each deflection side.
Fig. 2.
Graphic display of the aligned curves related to ACL-intact and ACL-absent values
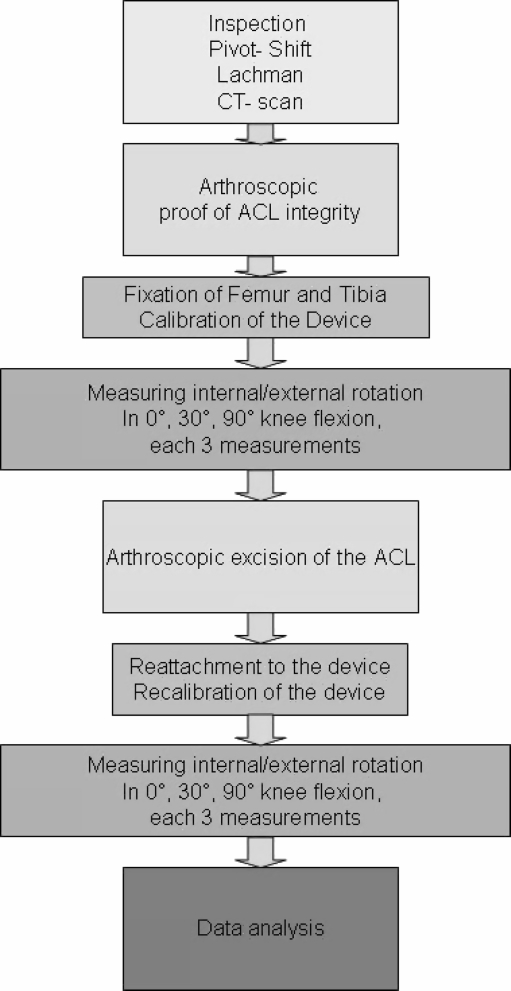
Measurements of the knee with intact ACL were repeated in 0, 30 and 90° flexion. Thereafter, the ACL was resected through standard anterolateral and anteromedial arthroscopic portals using arthroscopic basket forceps (WideBiter Punch Tip, Arthrex, Naples, FL, USA) and a shaving instrument (Full Radius Resector, Arthrex, Naples, FL, USA). The protocol was repeated until maximum deflection was reached. In order to analyse the intraobserver reliability each measurement (intact vs absent ACL: 0, 30 and 90° flexion angles) was repeated three times by the same observer. Figure 3 depicts the main steps of the experimental protocol.
Fig. 3.
Flowchart depicting the main steps of the experimental protocol
Data processing
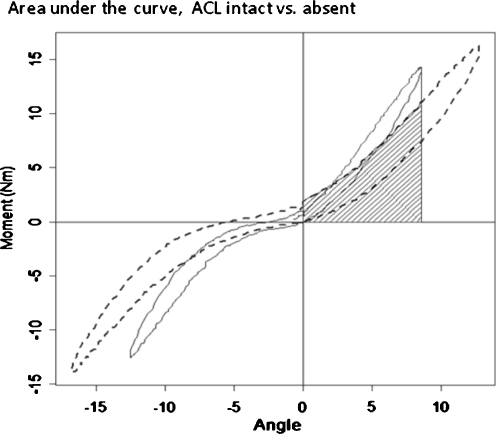
For the analyses of the areas under the curve (AUC), the measured deflection values were converted into the SI system and calculated for both situations, loaded and unloaded. The values represent the physical work applied to the specimen in joules (Fig. 4).
Fig. 4.
Example of calculated AUC of the right knee for the conditions of ACL integrity and absence, respectively. The light grey area represents the intact whereas the striped area shows the absent condition
The increase and decrease of these areas was accumulated. Every 30 minutes, one pair of rotational angle and torque was recorded and processed using the LabVIEW 8.0 software (National Instruments, Austin, TX, USA). The applied moments were visible at every time point of the measurement cycle and reached a maximum of 31 Nm (see Table 1). The deflection was applied until 180 measuring points (MP) were achieved and at least 11 up to 15° was measured and the graphical analysis was performed (for an example, see Fig. 4). The internal rotation including all angles and moments under ACL-intact conditions was measured and recorded. Thereafter, the measurement with absent ACL was performed. The applied torque of the maximum internal rotation (ACL intact) was compared to the same torque applied under ACL-absent condition to evaluate the amount of internal rotation (Table 2). In the same manner the AUC was calculated, and the area of maximum internal rotation with intact ACL was compared to the area with absent ACL (Table 3).
Table 1.
Values of maximum internal rotation with corresponding torques
| Maximum deflection angles and moments for intact versus absent ACL | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| ID | Knee flexion angle | Internal rotation, ACL absent | External rotation, ACL absent | Internal rotation, ACL intact | External rotation, ACL intact | ||||
| Angle (°) | Nm | Angle (°) | Nm | Angle (°) | Nm | Angle (°) | Nm | ||
| I | 0° | 19.0 | 18.4 | −13.6 | 16.7 | 13.3 | 12.5 | −9.2 | 11.4 |
| II | 23.1 | 28.3 | −17.8 | 23.9 | 13.5 | 16.1 | −11.3 | 19.4 | |
| III | 12.0 | 16.2 | −17.9 | 18.2 | 3.9 | 7.6 | −10.0 | 14.0 | |
| IV | 13.5 | 20.2 | −15.1 | 17.4 | 7.5 | 12.9 | −10.3 | 13.6 | |
| V | 21.9 | 20.6 | −26.3 | 21.9 | 15.1 | 13.8 | −19.8 | 15.5 | |
| VI | 13.0 | 14.4 | −16.7 | 15.8 | 8.4 | 13.7 | −13.1 | 14.6 | |
| I | 30° | 21.4 | 17.0 | −15.6 | 19.1 | 18.5 | 13.8 | −9.6 | 13.1 |
| II | 23.1 | 25.1 | −17.9 | 23.6 | 13.8 | 11.8 | −10.3 | 13.1 | |
| III | 16.8 | 16.9 | −14.3 | 16.8 | 7.1 | 6.2 | −10.7 | 9.4 | |
| IV | 13.0 | 19.4 | −13.2 | 22.2 | 8.4 | 11.3 | −9.9 | 16.6 | |
| V | 22.5 | 18.4 | −25.2 | 22.6 | 13.6 | 11.1 | −22.5 | 16.0 | |
| VI | 17.7 | 15.8 | −18.1 | 14.4 | 12.0 | 12.4 | −12.9 | 15.1 | |
| I | 90° | 22.8 | 31.6 | −12.4 | 23.3 | 18.3 | 18.5 | −8.2 | 17.8 |
| II | 18.4 | 30.2 | −10.7 | 30.1 | 10.1 | 17.6 | −5.4 | 16.3 | |
| III | 10.6 | 16.8 | −10.0 | 17.4 | 6.7 | 12.9 | −10.8 | 18.2 | |
| IV | 12.5 | 19.4 | −11.8 | 20.1 | 8.2 | 16.8 | −6.2 | 15.5 | |
| V | 22.8 | 15.8 | −26.2 | 19.9 | 14.9 | 10.8 | −15.2 | 16.9 | |
| VI | 21.8 | 29.1 | −15.7 | 28.6 | 9.0 | 13.8 | −10.8 | 26.6 | |
| Knee flexion angle | Averaged values of maximum rotation and corresponding moments | ||||||||
| Angle (°) | Nm | Angle (°) | Nm | Angle (°) | Nm | Angle (°) | Nm | ||
| Meana | 0° | 17.1 | 19.6 | −17.9 | 19.0 | 10.3 | 12.8 | −12.3 | 14.8 |
| SEMb | 2.0 | 2.0 | 1.8 | 1.3 | 1.8 | 1.2 | 1.6 | 1.1 | |
| Meana | 30° | 19.1 | 18.8 | −17.4 | 19.8 | 12.2 | 11.1 | −12.6 | 13.9 |
| SEMb | 1.6 | 1.4 | 1.8 | 1.5 | 1.7 | 1.1 | 2.0 | 1.1 | |
| Meana | 90° | 18.1 | 23.8 | −14.5 | 23.2 | 11.2 | 15.1 | −9.4 | 18.5 |
| SEMb | 2.2 | 3.0 | 2.5 | 2.1 | 1.8 | 1.2 | 1.5 | 1.7 | |
Data are given for each cadaver and each flexion angle, each for the intact and the absent ACL
aArithmetic mean
bStandard error of mean
Table 2.
Values of maximum internal and external rotation reached
| Maximum internal rotation with corresponding moments, calculated areas and work (J) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Loaded deflection | Unloaded deflection | ||||||||
| ID | Knee flexion angle | Deflection angle (°) | Nm intact | Nm absent | AUC intact (Nm/J) | AUC absent (Nm/J) | AUC intact (Nm/J) | AUC absent (Nm/J) | |
| I | 0° | 13.3 | 12.5 | 10.1 | 1.08 | 1.04 | 0.87 | 0.66 | |
| II | 13.5 | 16.1 | 11.9 | 1.66 | 1.29 | 1.27 | 0.65 | ||
| III | 3.9 | 7.6 | 4 | 0.25 | 0.12 | 0.24 | 0.05 | ||
| IV | 7.5 | 12.9 | 10 | 0.71 | 0.57 | 0.61 | 0.25 | ||
| V | 15.1 | 13.8 | 12.6 | 1.61 | 1.52 | 1.35 | 1.02 | ||
| VI | 8.4 | 13.7 | 8.8 | 0.95 | 0.55 | 0.77 | 0.35 | ||
| I | 30° | 18.5 | 13.8 | 13.3 | 1.25 | 1.3 | 0.99 | 0.67 | |
| II | 13.8 | 11.8 | 9.8 | 1.15 | 1.04 | 0.81 | 0.46 | ||
| III | 7.1 | 6.2 | 3.7 | 0.33 | 0.11 | 0.28 | 0.15 | ||
| IV | 8.4 | 11.3 | 12.3 | 0.74 | 0.86 | 0.56 | 0.59 | ||
| V | 13.6 | 11.1 | 3.9 | 1.17 | 0.87 | 0.94 | 0.39 | ||
| VI | 12 | 12.4 | 9 | 1.14 | 0.54 | 0.91 | 0.26 | ||
| I | 90° | 18.3 | 18.5 | 21.3 | 2.71 | 3.06 | 2.15 | 2.13 | |
| II | 10.1 | 17.6 | 14.2 | 1.52 | 1.44 | 1.33 | 1.07 | ||
| III | 6.7 | 12.9 | 6.7 | 0.65 | 0.54 | 0.50 | 0.37 | ||
| IV | 8.2 | 16.8 | 14.7 | 1.18 | 1.04 | 0.99 | 0.43 | ||
| V | 14.9 | 10.8 | 6.1 | 1.4 | 1.09 | 1.05 | 0.45 | ||
| VI | 9 | 13.8 | 7.8 | 1.07 | 0.64 | 0.96 | 0.42 | ||
| Averaged values of maximum internal rotation, corresponding moments and applied work (J) | |||||||||
| Knee flexion angle | Deflection angle (°) | Nm intact | Nm absent | AUC intact (Nm/J) | AUC absent (Nm/J) | AUC intact (Nm/J) | AUC absent (Nm/J) | ||
| Meana | 10.3 | 12.8 | 9.6 | 1.0 | 0.8 | 0.9 | 0.5 | ||
| SEMb | 0° | 1.8 | 1.2 | 1.2 | 0.2 | 0.2 | 0.2 | 0.1 | |
| Meana | 12.2 | 11.1 | 8.7 | 1.0 | 0.8 | 0.7 | 0.4 | ||
| SEMb | 30° | 1.7 | 1.1 | 1.7 | 0.1 | 0.2 | 0.1 | 0.1 | |
| Meana | 11.2 | 15.1 | 11.8 | 1.4 | 1.3 | 1.2 | 0.8 | ||
| SEMb | 90° | 1.8 | 1.2 | 2.4 | 0.3 | 0.4 | 0.2 | 0.3 | |
Data are given for each cadaver and each flexion angle, each for the intact and the absent ACL including the averaged deflections in each flexion angle with SEM
aArithmetic mean
bStandard error of mean
Table 3.
All measured areas under the specific curve for each specimen
| AUC | |||||
|---|---|---|---|---|---|
| ID | Flexion angle | Internal rotation, ACL intact loaded | Internal rotation, ACL intact unloaded | Internal rotation, ACL absent loaded | Internal rotation, ACL absent unloaded |
| I | 0° | 61.9 | 59.9 | 49.7 | 37.8 |
| II | 95.4 | 74.2 | 72.7 | 37.4 | |
| III | 14.7 | 6.9 | 13.8 | 2.8 | |
| IV | 41.0 | 32.9 | 35.1 | 14.5 | |
| V | 92.3 | 87.4 | 77.3 | 58.4 | |
| VI | 54.6 | 31.7 | 43.9 | 19.8 | |
| I | 30° | 72.0 | 74.9 | 56.5 | 38.3 |
| II | 66.2 | 60.1 | 46.3 | 26.5 | |
| III | 19.3 | 6.6 | 15.9 | 8.7 | |
| IV | 42.5 | 49.5 | 32.0 | 33.7 | |
| V | 67.3 | 49.9 | 54.0 | 22.2 | |
| VI | 65.7 | 31.1 | 52.2 | 15.2 | |
| I | 90° | 155.8 | 175.5 | 122.9 | 122.2 |
| II | 87.2 | 83.0 | 76.1 | 61.5 | |
| III | 37.4 | 31.0 | 28.6 | 21.4 | |
| IV | 67.9 | 59.9 | 56.6 | 24.9 | |
| V | 80.8 | 62.9 | 60.2 | 25.8 | |
| VI | 61.6 | 37.2 | 55.0 | 24.0 | |
| AUC on averaged values | |||||
| Knee flexion | Internal rotation, ACL intact loaded | Internal rotation, ACL intact unloaded | Internal rotation, ACL absent loaded | Internal rotation, ACL absent unloaded | |
| Meana | 60.0 | 48.8 | 48.8 | 28.4 | |
| SEMb | 0° | 12.6 | 12.3 | 9.7 | 8.2 |
| Meana | 55.5 | 45.3 | 42.8 | 24.1 | |
| SEMb | 30° | 8.4 | 9.7 | 6.5 | 4.5 |
| Meana | 81.8 | 74.9 | 66.6 | 46.6 | |
| SEMb | 90° | 16.4 | 21.5 | 12.9 | 16.3 |
Each area represents the physical work applied to reach a certain amount of deflection in relation to the ACL-intact and ACL-absent conditions
aArithmetic mean
bStandard error of mean
Statistics
The single measure intraclass correlation coefficient (ICC) was used to evaluate the interobserver reliability. The Wilcoxon rank test was used to determine statistical differences of torque values expected for the maximum averaged rotation between different ACL conditions. To compare the different ACL conditions, the AUC was also calculated for internal, external, loaded and unloaded deflection using the trapezoidal rule to map the entire course of the rotational movement. The Wilcoxon signed rank test was used to evaluate significances relative to the measured AUCs for both conditions (ACL intact vs ACL absent). Data are given as mean±standard deviation. PASW 17.0 software package (SPSS® Inc., Chicago, IL, USA) and R 2.9.2 (R Foundation for Statistical Computing, Vienna, Austria) were used for statistical analysis. For the analysis of different knee flexion angles of maximum internal and maximum external rotation, the nonparametric Friedman test was performed. All statistical analyses were done using a 0.05 level of significance.
Results
Six right human total lower limb specimens were used. The mean age of the cadavers was 46 ± 4 years, and the mean body weight was 75 ± 9 kg.
Reproducibility
The rotational angle rose with increasing torque applied to the stress lever. The torque changed between the assessments with intact and absent ACL, respectively (see Tables 1 and 2). The curves and values measured under the conditions of ACL integrity and absence, respectively, were highly reproducible and consistent with individual characteristic behaviour as shown in each of the three measurements. The evaluation of the three repeated measurements for each subject showed high interindividual ICCs. The ICC for the maximum deflection angles for intact and absent ACL was between 0.87 and 0.97 for internal rotation and between 0.94 and 0.98 for external rotation.
Total internal and external rotation
The intraindividual differences of femorotibial rotation and torques were high. In 0° flexion the angle for the intact ACL accounted for 10.3 ± 1.8° in internal and for 12.3 ± 1.6° in external rotation. The corresponding loads were 12.8 ± 1.2 Nm for internal and 14.8 ± 1.1 Nm for external rotation. In contrast, the assessment with absent ACL revealed an internal rotation of 17.1 ± 2° and an external rotation of 17.9 ± 1.8°. In parallel, maximum loads increased to 19.7 ± 2 Nm for internal and to 19.0 ± 1.3 Nm for external rotation. However, differences were only statistically significant for internal rotation. Comparing the torques expected for the maximum averaged internal rotation, the torque decreased significantly from the ACL-intact 12.8 ± 1.2 to 9.0 ± 1.2 Nm compared to the absent situation. This result reached significance (p = 0.031).
The calculated areas also differed significantly between the intact and absent situations (p = 0.031). Comparing the AUC for the condition of ACL integrity 60.0 ± 12.6 resulted for the internal forced rotation whereas after resecting the ACL the AUC decreased to 48.8 ± 12.3. For the unloaded or passive curve the intact internal rotation led to 48.8 ± 9.7 and decreased to 28.4 ± 8.2 after resection of the ACL. The AUC of maximum loaded internal rotation was 1.0 ± 0.2 J for the intact and 0.8 ± 0.2 J for the absent situation and was significant with a p value = 0.03125. To complete the evaluation, the area under the unloaded curve was calculated (intact 0.9 ± 0.2 vs absent 0.5 ± 0.1 J). This area was revealed to be significant at 0° knee flexion with a p value = 0.3125.
For the 30° flexion analysis the intact ACL yielded a maximum internal rotation of 12.2 ± 1.7° and external rotation of 12.7 ± 2°. The corresponding loads were 11.1 ± 1.1 Nm for internal and 13.9 ± 1.1 Nm for external rotation. Again the values increased following the excision of the ACL (rotational angle: internal 19.1 ± 1.6°, external 17.4 ± 1.8°; maximum torque: internal 18.8 ± 1.4 Nm, external 19.8 ± 1.5 Nm). The applied torques for maximum internal averaged rotation dropped from 11.1 ± 1.1 Nm for the intact to 8.7 ± 1.7 Nm for the absent condition. The AUC for forced internal rotation resulted in 55.5 ± 8.4 and decreased to 45.3 ± 9.7 in the ACL-absent condition. For the unloaded deflection 42.8 ± 6.5 resulted and turned into 24.1 ± 4.5 without the ACL. The AUC of maximum loaded internal rotation was 1.0 ± 0.1 J for the intact and 0.8 ± 0.2 J for the absent situation and was not significant with a p value = 0.2188. Also the area under the unloaded curve (intact 0.7 ± 0.1 vs absent 0.4 ± 0.1 J) at 30° knee flexion was not significant with a p value = 0.0625.
The 90° flexion analysis revealed a rotation of the intact ACL of 11.2 ± 1.8° in internal rotation and 9.4 ± 1.5° in external rotation. Values of the absent ACL increased to 18.2 ± 2.2° in internal and to 14.5 ± 2.5° in external rotation. Torques increased in parallel (intact ACL: internal 15.1 ± 1.2 Nm, external 18.6 ± 1.7 Nm vs absent ACL: internal 23.8 ± 3 Nm, external 23.2 ± 2.1 Nm). The absence of the ACL led to a decrease of the torque value for the averaged internal rotation from 15.1 ± 1.2 Nm to 11.8 ± 2.4 Nm. Again the AUC resulted in 81.8 ± 16.4 and changed to 74.9 ± 21.5 after ACL resection, but did not reach the level of significance. The unstressed deflection resulted in 66.6 ± 12.9 and changed into 46.6 ± 16.3. The areas did not show significant differences with and without ACL, respectively, during 30° (p = 0.21) and 90° knee flexion (p = 0.313). The mean values of the torque expected for the maximum averaged internal rotation in the absent situation in flexion 30° (p = 0.094) and 90° (p = 0.09) were lower, but did not reach statistical significance. There was no significant difference between the maximum internal and the maximum external deflection in 0, 30 and 90° knee flexion. The AUC of maximum loaded internal rotation was 1.4 ± 0.3 J for the intact and 1.3 ± 0.4 J for the absent situation and was significant with a p value = 0.3125. Again, also the area under the unloaded curve was calculated (1.2 ± 0.2 intact vs absent 0.8 ± 0.3 J) and was significant at 90° knee flexion with a p value = 0.03125.
Discussion
We report the evaluation of a novel tool for the assessment of femorotibial rotational stability. The feasibility of performing these measurements was proven in vitro in this study. We found that the loss of the ACL increases the arc of internal and external knee rotational movements while torque stress is applied. The highest increase was found in 0 and 90° knee flexion, whereas slightly lower values were found in 30° knee flexion.
It is commonly known that clinical testing of ACL deficiency depends greatly on the examiner’s experience [11–14]. In particular the evaluation of rotational stability using the pivot shift test is influenced by many factors including the examiner’s experience [21]. The objective measurement of AP translation using a KT1000 Arthrometer is well established and has been validated in daily routine clinical practice, but also presents some examiner-dependant disadvantages [10, 22]. In the current literature studies describe different approaches to evaluate rotational movements of the femorotibial joint, but no adequate method has been established so far [20, 23]. A consideration of the most interesting studies results in a differentiation between mechanical [16, 17], opto-/electromagnetic sensor [24, 25] and invasive navigational studies [19, 24, 26]. Studies using skin markers or mechanical splints for the attachment of the specimen to the device are carefully conceived but suffer from difficulties due to soft tissue artefacts with consequent inaccurate measurement results [16, 24, 27]. As shown in the study of Pearle et al. [26], the values measured with a navigating system reliably matched values assessed by a robot [26]. Similar studies also showed reproducible data, leading to the assumption that this method is sufficiently accurate to collect data for diagnostic purposes [20, 26, 28]. The main drawback of the studies mentioned is that due to its invasiveness the method cannot be considered for the evaluation of ligamentous laxity in outpatient conditions. As described in the literature a noninvasive device for measuring rotational movements cannot be as exact as one attached to the skeleton [16]. Therefore, the primary aim of our study was to develop a new invasive measuring device to be able to evaluate the resistance torque by the knees’ ligaments during passive rotation. The device has been evaluated in a human cadaver set up and has resulted in reproducible measurements at each flexion angle applied. In the same way the method of counting the area under the deflection curve as a parameter of physical work seems to be a relevant and reliable method for the analysis of resistance patterns. In contrast to recently published studies [4, 29], no defined torques were applied to the knee joint while rotating it along the femorotibial axis. The moment of torque was continuously measured at 33 Hz while the knee joint was rotated. The advantage of the torsiometer is the dynamic acquisition of measurements allowing for a detailed investigation of rotational torque relations of so far exact characters due to the absence of soft tissue artefacts and unstable fixation. In all specimens the absence of the ACL caused a significant increase of internal rotation at low flexion angles. The required torque for maximum internal rotation under the condition of ACL absence was significantly lower for 0 and 90° knee flexion, while for 30° it was not compared to the condition of ACL integrity. But these values did not reach significance for external rotation.
Postmortem stiffness, once broken, had no further effects on the passive joint movements and allowed for the performance of the clinical Lachman and pivot shift tests without any problems.
One current technical drawback is the use of transosseous Schanz screws for the attachment of the thigh and shin bone to the torsiometer. This limits the current device to performing ex vivo experiments. However, currently we are developing a noninvasive fixation mode on a splint basis. Of course we are aware of the fact that further studies are necessary to establish physiological and pathological reference values. Another potential drawback is the visual and palpable adjustment of the knee joint line and patella orientation to the torque axis of the device. A radiological assessment of the femoral and tibial axis could have ensured the measurement in regard to the anatomical axis. In this regard setting the device to zero has been processed after fixation to exclude pre-existing torques.
Conclusion
In this study we present a novel measuring device for the evaluation of femorotibial rotation under varying knee flexion angles. The internal deflection increases massively in the absence of the ACL. The highest increase of the rotational arc was found in 0° knee flexion when, in the case of ACL integrity, the PL bundle is the main restraint. Under natural conditions the PL bundle is under tension and the AM bundle is more relaxed. The testing device is highly reliable for a dynamic measurement of internal, external and total rotation and enables the examiner to analyse deflection and torque patterns restraining rotational motion. It might be a useful tool for a wide field of rotational measurements and can be used to compare varying ACL reconstruction techniques or ligament deficiencies and their reconstruction in cadavers. In the same way we think that the calculation of the AUC is a suitable way to investigate the restraint patterns according to the physical work needed for deflection. Further developments will enable the system to be used as a noninvasive clinical measurement device and for future application in daily routine clinical practice.
Acknowledgements
This study has been supported by a grant from the Deutsche Arthrose-Hilfe e.V. (Frankfurt am Main, Germany).
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Gianotti SM, Marshall SW, Hume PA, Bunt L (2009) Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport 12:622–627. [DOI] [PubMed]
- 2.Parkkari J, Pasanen K, Mattila VM, Kannus P, Rimpelä A. The risk for a cruciate ligament injury of the knee in adolescents and young adults: a population-based cohort study of 46 500 people with a 9 year follow-up. Br J Sports Med. 2008;42(6):422–426. doi: 10.1136/bjsm.2008.046185. [DOI] [PubMed] [Google Scholar]
- 3.Petersen W, Zantop T. Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res. 2007;454:35–47. doi: 10.1097/BLO.0b013e31802b4a59. [DOI] [PubMed] [Google Scholar]
- 4.Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W. The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med. 2007;35(2):223–227. doi: 10.1177/0363546506294571. [DOI] [PubMed] [Google Scholar]
- 5.Zantop T, Petersen W, Sekiya JK, Musahl V, Fu FH. Anterior cruciate ligament anatomy and function relating to anatomical reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):982–992. doi: 10.1007/s00167-006-0076-z. [DOI] [PubMed] [Google Scholar]
- 6.Zelle BA, Vidal AF, Brucker PU, Fu FH. Double-bundle reconstruction of the anterior cruciate ligament: anatomic and biomechanical rationale. J Am Acad Orthop Surg. 2007;15(2):87–96. doi: 10.5435/00124635-200702000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Franceschi JP, Sbihi A, Champsaur P. Arthroscopic reconstruction of the anterior cruciate ligament using double anteromedial and posterolateral bundles (in French) Rev Chir Orthop Reparatrice Appar Mot. 2002;88(7):691–697. [PubMed] [Google Scholar]
- 8.Meredick RB, Vance KJ, Appleby D, Lubowitz JH. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2008;36(7):1414–1421. doi: 10.1177/0363546508317964. [DOI] [PubMed] [Google Scholar]
- 9.Gadikota HR, Seon JK, Kozanek M, Oh LS, Gill TJ, Montgomery KD, Li G. Biomechanical comparison of single-tunnel-double-bundle and single-bundle anterior cruciate ligament reconstructions. Am J Sports Med. 2009;37(5):962–969. doi: 10.1177/0363546508330145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Araki D, Kuroda R, Kubo S, Fujita N, Tei K, Nishimoto K, Hoshino Y, Matsushita T, Matsumoto T, Nagamune K, Kurosaka M (2010) A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop. doi:10.1007/s00264-010-1110-9 [DOI] [PMC free article] [PubMed]
- 11.Prins M. The Lachman test is the most sensitive and the pivot shift the most specific test for the diagnosis of ACL rupture. Aust J Physiother. 2006;52(1):66. doi: 10.1016/S0004-9514(06)70069-1. [DOI] [PubMed] [Google Scholar]
- 12.Benjaminse A, Gokeler A, Schans CP. Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther. 2006;36(5):267–288. doi: 10.2519/jospt.2006.2011. [DOI] [PubMed] [Google Scholar]
- 13.Anderson AF, Rennirt GW, Standeffer WC., Jr Clinical analysis of the pivot shift tests: description of the pivot drawer test. Am J Knee Surg. 2000;13(1):19–23. [PubMed] [Google Scholar]
- 14.Galway HR, MacIntosh DL. The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res. 1980;147:45–50. [PubMed] [Google Scholar]
- 15.Sadoghi P, Müller PE, Jansson V, van Griensven M, Kröpfl A, Fischmeister MF (2010) Reconstruction of the anterior cruciate ligament: a clinical comparison of bone-patellar tendon-bone single bundle versus semitendinosus and gracilis double bundle technique. Int Orthop. doi:10.1007/s00264-010-1037-1 [DOI] [PMC free article] [PubMed]
- 16.Almquist PO, Arnbjörnsson A, Zätterström R, Ryd L, Ekdahl C, Fridén T. Evaluation of an external device measuring knee joint rotation: an in vivo study with simultaneous Roentgen stereometric analysis. J Orthop Res. 2002;20(3):427–432. doi: 10.1016/S0736-0266(01)00148-6. [DOI] [PubMed] [Google Scholar]
- 17.Lorbach O, Wilmes P, Maas S, Zerbe T, Busch L, Kohn D, Seil R (2009) A non-invasive device to objectively measure tibial rotation: verification of the device. Knee Surg Sports Traumatol Arthrosc 17:756–762. doi:10.1007/s00167-009-0756-6 [DOI] [PubMed]
- 18.Tsai AG, Musahl V, Steckel H, Bell KM, Zantop T, Irrgang JJ, Fu FH. Rotational knee laxity: reliability of a simple measurement device in vivo. BMC Musculoskelet Disord. 2008;9:35. doi: 10.1186/1471-2474-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seon JK, Park SJ, Lee KB, Yoon TR, Seo HY, Song EK. Stability comparison of anterior cruciate ligament between double- and single-bundle reconstructions. Int Orthop. 2009;33(2):425–429. doi: 10.1007/s00264-008-0530-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Papachristou G, Kalliakmanis A, Papachristou K, Magnissalis E, Sourlas J, Plessas S. Comparison of fixation methods of double-bundle double-tibial tunnel ACL reconstruction and double-bundle single-tunnel technique. Int Orthop. 2008;32(4):483–488. doi: 10.1007/s00264-007-0343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim SJ, Kim HK. Reliability of the anterior drawer test, the pivot shift test, and the Lachman test. Clin Orthop Relat Res. 1995;317:237–242. [PubMed] [Google Scholar]
- 22.Jardin C, Chantelot C, Migaud H, Gougeon F, Debroucker MJ, Duquennoy A. Reliability of the KT-1000 arthrometer in measuring anterior laxity of the knee: comparative analysis with Telos of 48 reconstructions of the anterior cruciate ligament and intra- and interobserver reproducibility (in French) Rev Chir Orthop Reparatrice Appar Mot. 1999;85(7):698–707. [PubMed] [Google Scholar]
- 23.Kasović M, Mejovšek M, Matković B, Janković S, Tudor A (2010) Electromyographic analysis of the knee using fixed-activation threshold after anterior cruciate ligament reconstruction. Int Orthop. doi:10.1007/s00264-010-1050-4 [DOI] [PMC free article] [PubMed]
- 24.Kubo S, Muratsu H, Yoshiya S, Mizuno K, Kurosaka M. Reliability and usefulness of a new in vivo measurement system of the pivot shift. Clin Orthop Relat Res. 2007;454:54–58. doi: 10.1097/BLO.0b013e31802b4a38. [DOI] [PubMed] [Google Scholar]
- 25.Georgoulis AD, Papadonikolakis A, Papageorgiou CD, Mitsou A, Stergiou N. Three-dimensional tibiofemoral kinematics of the anterior cruciate ligament-deficient and reconstructed knee during walking. Am J Sports Med. 2003;31(1):75–79. doi: 10.1177/03635465030310012401. [DOI] [PubMed] [Google Scholar]
- 26.Pearle AD, Solomon DJ, Wanich T, Moreau-Gaudry A, Granchi CC, Wickiewicz TL, Warren RF. Reliability of navigated knee stability examination: a cadaveric evaluation. Am J Sports Med. 2007;35(8):1315–1320. doi: 10.1177/0363546507300821. [DOI] [PubMed] [Google Scholar]
- 27.Georgoulis AD, Ristanis S, Chouliaras V, Moraiti C, Stergiou N. Tibial rotation is not restored after ACL reconstruction with a hamstring graft. Clin Orthop Relat Res. 2007;454:89–94. doi: 10.1097/BLO.0b013e31802b4a0a. [DOI] [PubMed] [Google Scholar]
- 28.Colombet P, Robinson J, Christel P, Franceschi JP, Djian P. Using navigation to measure rotation kinematics during ACL reconstruction. Clin Orthop Relat Res. 2007;454:59–65. doi: 10.1097/BLO.0b013e31802baf56. [DOI] [PubMed] [Google Scholar]
- 29.Kanamori A, Zeminski J, Rudy TW, Li G, Fu FH, Woo SL. The effect of axial tibial torque on the function of the anterior cruciate ligament: a biomechanical study of a simulated pivot shift test. Arthroscopy. 2002;18(4):394–398. doi: 10.1053/jars.2002.30638. [DOI] [PubMed] [Google Scholar]