Abstract
Purpose
The purpose of this study was to evaluate the clinical benefit of medial support screws for locking plating of proximal humerus fractures.
Methods
Seventy-two consecutive patients underwent prospective treatment for proximal humerus fractures with locking plates between October 2007 and September 2008. Sixty-eight patients accomplished a mean 30.8-month follow-up and were randomized into two groups: 39 patients were treated with only a locking plate and were classified in the –MSS (medial support screw) group, and 29 patients were included in the + MSS group, which were fixed with additional medial support screws. Clinical and radiological investigations were performed in both groups.
Results
The fractures united at an average of 13.6 weeks after final surgery. Comparably better shoulder function recovery was achieved in the +MSS group with regard to the Constant shoulder score (P = 0.01), with the respective excellent and good rates of 79% and 62%. Eleven patients developed various complications. A statistical difference (P = 0.036) was observed regarding the failure rate (23.1% in the −MSS group vs. 3.4% in the +MSS group). The early loss of fixation was related to higher age (P < 0.001) and less initial neck-shaft angle (NSA) (P = 0.011) of the patients. However, bone mineral density was not significantly associated with loss of fixation (P = 0.076). Although no difference was found in all types of the fractures between the +MSS and −MSS groups regarding immediate postoperative NSA, we observed a significantly lower final NSA in the −MSS group and greater secondary angle loss in the subgroup of Neer three-part (P = 0.033 and 0.015, respectively) and four-part fractures (P = 0.043 and 0.027).
Conclusions
Anatomical reduction can substantially decrease the risk of postoperative failure in locking plating of proximal humerus fractures. Medial support for proximal humerus fractures seems to have no benefits in Neer two-part fractures. However, the additional medial support screws inserted into the medio-inferior region of the humeral head may help to enhance mechanical stability in complex fractures and allow for better maintenance of reduction.
Introduction
Proximal humerus fractures are a common fracture of the upper extremity which accounts for about 5% of all fractures [1, 2]. Although satisfactory results can be achieved with non-operative treatment in 80% of proximal humerus fractures [3], surgical intervention is generally accepted in some unstable fractures, especially in displaced and osteoporotic cases, for the high nonunion rate of 5–23% with conservative treatment [2]. Recent studies have noted that locking plates can provide adequate mechanical support and thus have shown superior outcomes over other means of fixation methods in these patients [4, 5]. Also, various devastating complications have been addressed by using locking plating, such as varus displacement of humeral head, loss of fixation and nonunion, which may occur frequently in comminuted and unstable fractures involving the medial supporting structures [1, 2, 6].
It is well known that achieving anatomic or slightly impacted stable reduction can lead to successful outcomes in patients with proximal humerus fractures. In addition, surgeons have focused on the importance of medial support for proximal humerus fractures. Gardner et al. demonstrated the direct association between medial support and subsequent reduction loss. Hence, mechanical support of the medio-inferior region of the humeral head seems to be essential for maintaining fracture reduction in locking plating of proximal humerus fractures [6]. Lescheid et al. also confirmed in his biomechanical study the concept of medial cortical support by fixing two-part proximal humeral fractures, preferably in anatomic alignment [7]. However, those studies only observed the radiological and biomechanical evidence of medial support. The clinical outcome has not been documented yet.
For these reasons, we sought to evaluate postoperative radiological and clinical behaviours of medial support screws (MSS) in fracture fixation. The hypothesis of our study was that the mechanical support of the medial column provided by additional medial support screws could be of great importance for establishing a stable construct. Our purpose was to determine whether medial support screws could improve the mechanical stability of locking plating for proximal humerus fractures. In addition, the performance of medial support screws in different types of fracture was assessed in our study.
Materials and methods
General materials
Between October 2007 and September 2008, 72 patients with proximal humerus fractures who met the criteria in a trauma centre were consecutively enrolled in our prospective study after approval from the institutional review board. Inclusion criteria included patients with ages older than 18 years and an acute close fracture of the proximal humerus treated with open reduction and internal fixation using a locking plate. The exclusive criteria included pathological fractures, patients with primary or metastatic tumour and fractures with nonunion. Four patients were lost to follow-up within the first year after surgery due to moving out of the area and change of telephone number. The remaining 68 patients (22 males, 46 females) were available in the study with a mean follow-up of 30.8 months (range, 25–36 months). The mean age of the patients was 63.2 years (range, 32–78 years). The causes of fracture consisted of traffic accidents (12 patients), falls from a height (7 patients) and falling down (49 patients). The fractures were divided into three subgroups according to Neer classification (two-part fractures in 10 patients, three-part fractures in 37 patients and four-part fractures in 21 patients) [8].
Bone mineral density (BMD) of the lumbar vertebra (L1) was measured before surgery using GE DPX-L dual energy X-ray absorptiometry (Lunar, Madison, WI, USA). All patients were treated with PHILOS locking plates (Synthes, Switzerland). The patients were randomized into two groups for study according to computer-generated random numbers: 39 patients treated only with a locking plate were classified in the −MSS group, the remaining 29 patients with additional medial support were included in the +MSS group, which were fixed with additional medial support screws. The demographic characteristics of the patients are in Table 1.
Table 1.
General patient data for the + MSS and -MSS group
| Description | +MSS group | −MSS group | P value |
|---|---|---|---|
| Gender | 0.746 a | ||
| Males | 10 | 12 | |
| Females | 19 | 27 | |
| Mean age (y) | 62.9 ± 9.6 | 63.5 ± 8.4 | 0.801 a |
| Neer classification | 0.585 a | ||
| Two-part fracture | 6 | 4 | |
| Three-part fracture | 14 | 23 | |
| Four-part fracture | 9 | 12 | |
| BMD (g/cm2) | 0.88 ± 0.15 | 0.90 ± 0.13 | 0.327 a |
MSS medial support screw, BMD bone mineral density
a Difference of data statistically not significant (P > 0.05)
Operative technique
Operations were performed by two senior surgeons (GJY and WLW) with the patient in the beach-chair position. A standard deltopectoral approach was used for open reduction and internal fixation of the fracture. Reduction was enabled with a K-wire under fluoroscopy according to the landmarks of the long head of biceps, the greater and lesser tubercle, and the intertubercular groove. After the fracture was anatomically reduced a locking plate was placed 10-mm posterior to the intertubercular groove and 10-mm distal to the tip of greater tubercle. A cortical screw was inserted initially to fix the distal fragment. One or two locking screws were implanted afterwards to stabilize the proximal segment. The correct position was checked again with fluoroscopy. One or two additional locking screws were inserted obliquely into the medio-inferior region of the humeral head in the +MSS group after four or five locking screws were employed for the fixation of the proximal fragment (Fig. 1). All proximal screws were inserted 5 mm below subchondral bone. The tubercular fragments and rotator cuff tendon were fixed using Ethibond sutures (Johnson & Johnson, Somerville, NJ, USA) passing from these structures and the plate. Autograft bone was used in comminuted fractures where there was a mass defect and for reconstruction of the medial support structures. Fracture reduction and screw length were finally assessed with fluoroscopy.
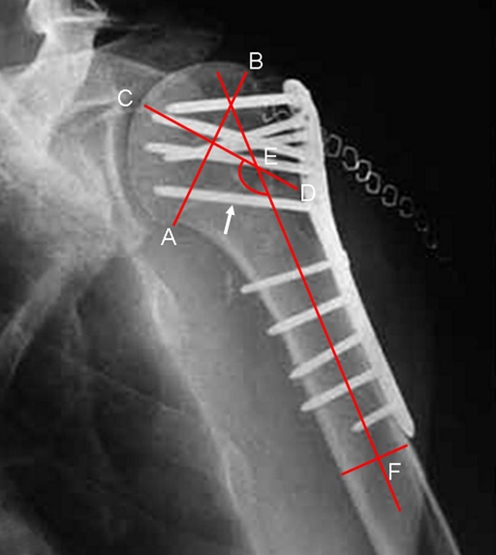
Fig. 1.
A PHILOS locking plate was applied for proximal humerus fracture. Note that a medial support screw (arrow) was used to fix the medio-inferior region of the humeral head. ∠CEF represents neck-shaft angle (about 140°). Line AB refers to the line between the superior and inferior border of the articular surface of the humeral head. Line CD is perpendicular to line AB and goes through the centre of the humeral head. Line EF refers to the axial line of the humeral shaft
All patients received prophylactic intravenous antibiotics before the procedure. Passive abduction and clock-wise rotation exercises were allowed on the day after surgery. Active rehabilitation was started six weeks postoperatively.
Follow-up
The patients were reviewed at four, eight, and 12 weeks and at six, nine, and 12 months after surgery, then yearly thereafter. The follow-up duration was determined from the date of the final surgery. Routine X-rays were taken by an experienced radiologist (JZ) at the four-, eight-, and 12-week follow-up appointment and then every 12 weeks until fracture healing. Complications, shoulder function and radiological measurement were recorded by an independent junior doctor (YJH) who did not participate in the surgery. The shoulder function was documented with scores according to the Constant shoulder score, which was graded as excellent (80–100 points), good (65 –79 points), fair (51 –64 points) and poor (less than 50 points) [9]. Fracture healing was assessed in the standard anteroposterior (AP) and axillary radiographs. Neck-shaft angle (NSA) was measured for indication of displacement of the fragments and implants (Fig. 1) [1]. Repeated measurement of NSA on the same radiograph was performed at a separate time by the junior doctor and another blind research assistant who was independent of the study. Intraobserver error was assessed with use of the Cohen kappa statistic and high intra-rater reliability of the measurement (intraclass correlation coefficient = 0.93) was found for NSA. In addition, loss of fixation was observed including varus collapse of the fracture, penetration of the screws and breakage of the plate or screws. In patients without early failure, immediate postoperative NSA and that at the final follow-up were documented respectively. Angle loss was calculated accordingly as immediate postoperative NSA minus final NSA.
Statistical analysis
We used SPSS statistical software for Windows (version 11.5, SPSS Inc., Chicago, IL, USA) for all analyses. Paired t-test and chi-square test were performed, respectively, to analyse measurement data and categorical data. Sum rank test was used to calculate the data of Neer classification, as well as the Constant shoulder score, which was considered as R × C contingency tables with ordinal classifications. P value was set at a significance level of 0.05.
Results
No significant differences were observed in gender, age, fracture type and BMD between the + MSS and −MSS groups (P > 0.05) (Table 1). All fractures united at an average of 13.6 weeks (range, 8–24 weeks) after the final surgery.
According to the Constant shoulder score, 13 patients in the + MSS group were graded as excellent, ten patients as good, five patients as fair and one patient as poor; whereas in the −MSS group ten patients were graded as excellent, 14 patients as good, nine patients as fair and six patients as poor. Comparably better shoulder function recovery was achieved in the +MSS group (79.1 ± 13.1 points, range 46–96 points) than in the −MSS group (70.1 ± 14.5 points, range, 41–94 points) (P = 0.01), with the respective excellent and good rates of 79% and 62%.
Several complications occurred in 11 patients (16.2%). One patient developed asymptomatic osteonecrosis of the humeral head but did not require revision. Ten patients developed early loss of fixation after surgery (Table 2). Varus collapse of the fracture was found in six patients, screw penetration was observed in three patients, and plate breakage occurred in one patient. Early loss of fixation was related to patients of greater age (70.3 ± 5.3 vs. 60.3 ± 6.4 years, P < 0.001) and less initial NSA of the patients (127.9 ± 2.3° vs. 131.9 ± 2.8°, P = 0.011). However, BMD was not significantly associated with loss of fixation (P = 0.076). A considerable difference was observed between the +MSS and −MSS groups regarding the failure rate (23.1% in −MSS group vs. 3.4% in +MSS group, P = 0.036), which all occurred within 12 weeks postoperatively. Eight patients (80%) were observed to lose the fixation within six weeks. Seven patients with early failure, thereafter, underwent another series of operations for revision, but the other three patients chose non-operative treatment.
Table 2.
The distribution of early failure in the +MSS and −MSS group
| Group | Neer classification | |||
|---|---|---|---|---|
| Two-part fracture | Three-part fracture | Four-part fracture | Total | |
| +MSS group | 0 | 0 | 1 | 1 |
| −MSS group | 1 | 3 | 5 | 9 |
MSS medial support screw
Among the 58 patients without failure (28 patients in the +MSS group, 30 patients in −MSS group), no difference was found in each subgroup between +MSS and −MSS groups regarding immediate postoperative NSA (Table 3). In the subgroup of Neer two-part fractures, we observed similar result between two groups with respect to NSA (P = 0.898) and secondary angle loss at the final follow-up (P = 0.712). The average final NSA values for patients with Neer three-part and four-part fractures in the +MSS group were 128.2° and 129.4°, respectively. However, a considerably lower NSA was found in the −MSS group at the final follow-up in the two subgroups (124.5° in three-part fractures, P = 0.033; 123.7° in four-part fractures, P = 0.043). In addition, a statistically significant difference was achieved between the +MSS and −MSS groups regarding secondary angle loss in both subgroups of three-part (P = 0.015) and four-part fracture (P = 0.027).
Table 3.
Radiological parameters of the patients in the +MSS and −MSS groups
| Parameters | +MSS group | −MSS group | P value |
|---|---|---|---|
| Neer two-part fracture (n) | 6 | 3 | |
| Immediate postoperative NSA (°) | 131.1 ± 2.9 | 131.6 ± 2.8 | 0.831 a |
| (128–136) | (128–135) | ||
| Final NSA (°) | 131.9 ± 3.9 | 131.6 ± 2.3 | 0.898 a |
| (127–136) | (128–134) | ||
| Angle loss (°) | 1.6 ± 1.3 | 1.3 ± 1.2 | 0.712 a |
| (0–3) | (0–2) | ||
| Neer three-part fracture (n) | 14 | 20 | |
| Immediate postoperative NSA (°) | 130.2 ± 3.4 | 131.8 ± 2.7 | 0.132 a |
| (126–136) | (127–136) | ||
| Final NSA (°) | 128.2 ± 4.4 | 124.5 ± 6.0 | 0.033 b |
| (121–136) | (115–133) | ||
| Angle loss (°) | 3.5 ± 2.4 | 6.1 ± 3.1 | 0.015 b |
| (0–7) | (0–12) | ||
| Neer four-part fracture (n) | 8 | 7 | |
| Immediate postoperative NSA (°) | 132.0 ± 2.6 | 130.4 ± 3.9 | 0.386 a |
| (129–136) | (122–135) | ||
| Final NSA (°) | 129.4 ± 4.4 | 123.7 ± 5.6 | 0.043 b |
| (123–134) | (115–129) | ||
| Angle loss (°) | 4.0 ± 1.7 | 7.1 ± 3.0 | 0.027 b |
| (0–6) | (3–12) |
MSS medial support screw, NSA neck-shaft angle
Values given as mean ± standard deviation and (range)
a Difference of data statistically not significant (P > 0.05)
b Difference of data statistically significant (P < 0.05)
Discussion
Although many novel implants and advanced minimally invasive techniques are employed for operative treatment of proximal humerus fractures, a majority of surgeons have been concerned about the high rate of postoperative complications. Recent findings have demonstrated a high positive correlation between the bone mass and early results of proximal humerus fractures [10–15]. Therefore, locking plates have been widely used in the treatment of proximal humerus fractures, especially in osteoporotic patients as they can provide the stability to resist angular and rotational forces. Moreover, anatomical plate design matches the configuration of the proximal humerus and allows multi-directional locking capability of the plate constructs, which can avoid screw back-out and loosening. The fixed-angle devices of the locking plate have been proven to increase pull-out strength of the screws and have exhibited favourable results with comparison to the traditional plate, which may also improve fixation in osteoporotic bone [13, 16, 17]. Siffri et al. investigated, in a cadaveric proximal humerus fracture-fixation model, that locking plates exhibited a greater torsional loading than blade plates (P = 0.036) [13]. Friess et al. also found that locking plates, compared with traditional fixation methods, showed high performance on both the functional range of motion and American Shoulder and Elbow Surgeons (ASES) scores after a mean 45-month follow-up [16]. Our present series indicated the satisfactory results of locking plating for proximal humerus fractures. A low incidence of complications was observed and the excellent and good rates were up to 70%. Most elderly patients were capable of resuming their daily activities within 12 weeks after surgery.
Early failures of locking plating occur frequently in patients with comminuted and osteoporotic fractures [6, 18]. Our study investigated the failure rate of 14.7%, and all the failures were found within 12 weeks after surgery. The data was in accordance with the results previously reported by Agudelo et al. (13.7%) [1].
Early loss of fixation seems to be related to the bone density of the proximal humerus, but not whole-body BMD. Our findings displayed no significant association between early failure of fixation and BMD. However, insertion of screws in proximal humerus with a higher BMD can help to prevent implant loosening and thus can avoid early failure. Tingart et al. showed regional differences in BMD of the humeral head resulting in an important impact of fixation strength of cancellous screws [19]. Therefore, osetoporosis is not a reliable predictor of mechanical failure.
Lack of medial structure support for the proximal humerus fractures may contribute to reduce loss of fixation. Biomechanical studies have demonstrated a greater compressive stress on the medial region than on the lateral during normal shoulder motion [20, 21]. Continuous varus stress of the rotator cuff may result in varus displacement of the humeral head and collapse of the articular surface during early rehabilitation, when the fracture fails to achieve anatomical reduction. Another recent biomechanical study by Lescheid et al. demonstrated that locking plating with medial cortical support could exhibit higher biomechanical performance in a two-part proximal humerus fracture model [7]. Gardner et al. also noted that the presence of medial support had a significant effect on the magnitude of subsequent reduction loss [6]. However, their studies didn’t involve entire clinical outcome and biomechanical evidence in complex fractures. Our study investigated all types of proximal humerus fractures and determined satisfactory clinical results in the +MSS group by both radiological and clinical assessment. Lower failure rate and better shoulder function recovery were achieved with stable medial column support of the proximal humerus.
A medial support screw inserted obliquely into the medio-inferior region of the humeral head can provide adequate strength to the medial column in locking plating of proximal humerus. A cadaveric biomechanical study by Liew et al. found that the grasping force of a screw placed under the subchondral bone of the medial and inferior region was comparably stronger than that of a screw placed either in the middle of the humeral head or in the lateral and superior region [22]. Another histomorphometric study by Hepp et al. showed the highest bone strength to be in the medial and dorsal aspects of the proximal humeral head [21]. As a result, the optimal fixation of a screw is in the posterior-medial-inferior aspect of the humeral head to achieve mechanical stability by medial support for the fracture.
The initial NSA seems to predict the failure of locking plating, because anatomical reduction of the humeral head plays a key role in the treatment of proximal humerus fracture. Agudelo et al. reported the results of 153 patients with a displaced fracture or fracture-dislocation of the proximal humerus treated with a 3.5-mm locking proximal humerus plate [1]. The failure rate was up to 30.4% when the postoperative NSA was < 120°; however, it decreased to 11% when the angle was ≥120°. A statistically significant association was addressed between varus reduction and loss of fixation. Our clinical results were quite similar. A high correlation was observed in our study between the initial NSA and failure rate. The mean NSA of patients with loss of fixation (127.9 ± 2.3°) was less than that of the other patients (131.9 ± 2.8°) and the healthy population (132.4 ± 4.7°). It indicates that mal-reduced proximal humerus fractures are inclined to lead to early failure of the fixation.
In our study, no benefits of medial support screws were found in locking plating of two-part proximal humerus fractures, as no significant difference was observed between the +MSS and –MSS groups regarding immediate postoperative NSA (P = 0.831), final NSA (P = 0.898) and angle loss (P = 0.712). Thus, there is no need to place additional screws to stabilize the medial structure in some simple proximal humerus fractures.
However, the medial support screw has made a great contribution to maintenance of the fracture alignment in complex fractures. Our study revealed that the angle loss of three-part and four-part fractures in the +MSS group was evidently less than that in the −MSS group during the follow-up (P = 0.015 and 0.027, respectively). We found no difference with respect to immediate postoperative NSA between the two groups (P = 0.132 and 0.386), whereas loss of the alignment after surgical treatment was clearly observed at the end-point of follow-up (P = 0.033 in three-part fractures, P = 0.043 in four-part fractures). The clinical results indicate that medial support may help to resist varus stress applied on the humeral head and therefore avoid displacement of the fracture to a certain extent. Our study shows that on the basis of anatomical reduction of the humeral head, medial support screws, combined with locking plates should be employed on three-part and four-part fractures to enhance primary mechanical stability.
However, some limitations must be addressed in our study. As most of our study was dependent on radiographic analysis, the quality of radiographs might influence the measurement results. The NSA measured in an AP film of the proximal humerus may be affected by many factors. Although a novel method for measurement was used to reduce the source of error caused by humeral rotation [1], we acknowledge that the results would be more accurate if two or more experienced observers and interrater reliability of NSA measurement were involved in the study to standardize the measurements. Besides, the measurements were only performed in the AP view. We would not attempt to measure NSA in the axillary view because the technique did not seem as accurate and had limited repeatability compared with measurements in other planes, as has been considered by some authors [1, 4]. Thirdly, this study only addressed the clinical results of medial support in proximal humerus fractures. The definite conclusions and biomechanical evidence of medial support screws have not been documented yet but will be involved in our subsequent research.
Conclusions
Satisfactory outcome of locking plating has been demonstrated for the treatment of proximal humerus fracture. Anatomical reduction can substantially decrease the risk of postoperative failures in locking plating of proximal humerus fractures. Medial support for proximal humerus fracture seems to have no benefits in Neer two-part fractures. However, the addition of medial support screws inserted into the medio-inferior region of the humeral head may help to enhance mechanical stability in complex fractures and allow for better maintenance of reduction.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
Footnotes
There was no financial support for this project. The authors have received nothing of value. The medical devices used in this study were approved by the Wenzhou Medical College Institutional Review Board (study number: 2006-1365).
References
- 1.Agudelo J, Schurmann M, Stahel P, Helwig P, Morgan SJ, Zechel W, Bahrs C, Parekh A, Ziran B, Williams A, Smith W. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007;21(10):676–681. doi: 10.1097/BOT.0b013e31815bb09d. [DOI] [PubMed] [Google Scholar]
- 2.Volgas DA, Stannard JP, Alonso JE. Nonunions of the humerus. Clin Orthop Relat Res. 2004;419:46–50. doi: 10.1097/00003086-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Iannotti JP, Ramsey ML, Williams GR, Warner JJP. Nonprosthetic management of proximal humeral fractures. J Bone Joint Surg Am. 2003;85(8):1578–1593. [Google Scholar]
- 4.Gardner MJ, Griffith MH, Demetrakopoulos D, Brophy RH, Grose A, Helfet DL, Lorich DG. Hybrid locked plating of osteoporotic fractures of the humerus. J Bone Joint Surg Am. 2006;88(9):1962–1967. doi: 10.2106/JBJS.E.00893. [DOI] [PubMed] [Google Scholar]
- 5.Roderer G, Gebhard F, Krischak G, Wilke HJ, Claes L. Biomechanical in vitro assessment of fixed angle plating using a new concept of locking for the treatment of osteoporotic proximal humerus fractures. Int Orthop. 2010 doi: 10.1007/s00264-010-1021-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma. 2007;21(3):185–191. doi: 10.1097/BOT.0b013e3180333094. [DOI] [PubMed] [Google Scholar]
- 7.Lescheid J, Zdero R, Shah S, Kuzyk PR, Schemitsch EH. The biomechanics of locked plating for repairing proximal humerus fractures with or without medial cortical support. J Trauma. 2010;69(5):1235–1242. doi: 10.1097/TA.0b013e3181beed96. [DOI] [PubMed] [Google Scholar]
- 8.Neer CS., 2nd Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077–1089. [PubMed] [Google Scholar]
- 9.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 10.Fjalestad T, Stromsoe K, Blucher J, Tennoe B. Fractures in the proximal humerus: functional outcome and evaluation of 70 patients treated in hospital. Arch Orthop Trauma Surg. 2005;125(5):310–316. doi: 10.1007/s00402-005-0803-9. [DOI] [PubMed] [Google Scholar]
- 11.Olsson C, Nordquist A, Petersson CJ. Long-term outcome of a proximal humerus fracture predicted after 1 year: a 13-year prospective population-based follow-up study of 47 patients. Acta Orthop. 2005;76(3):397–402. [PubMed] [Google Scholar]
- 12.Shahid R, Mushtaq A, Northover J, Maqsood M. Outcome of proximal humerus fractures treated by PHILOS plate internal fixation. Experience of a district general hospital. Acta Orthop Belg. 2008;74(5):602–608. [PubMed] [Google Scholar]
- 13.Siffri PC, Peindl RD, Coley ER, Norton J, Connor PM, Kellam JF. Biomechanical analysis of blade plate versus locking plate fixation for a proximal humerus fracture: comparison using cadaveric and synthetic humeri. J Orthop Trauma. 2006;20(8):547–554. doi: 10.1097/01.bot.0000244997.52751.58. [DOI] [PubMed] [Google Scholar]
- 14.Micic ID, Kim KC, Shin DJ, Shin SJ, Kim PT, Park IH, Jeon IH. Analysis of early failure of the locking compression plate in osteoporotic proximal humerus fractures. J Orthop Sci. 2009;14(5):596–601. doi: 10.1007/s00776-009-1382-3. [DOI] [PubMed] [Google Scholar]
- 15.Solberg BD, Moon CN, Franco DP, Paiement GD. Locked plating of 3- and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma. 2009;23(2):113–119. doi: 10.1097/BOT.0b013e31819344bf. [DOI] [PubMed] [Google Scholar]
- 16.Friess DM, Attia A (2008) Locking plate fixation for proximal humerus fractures: a comparison with other fixation techniques. Orthopedics 31(12) [DOI] [PubMed]
- 17.Lill H, Hepp P, Korner J, Kassi JP, Verheyden AP, Josten C, Duda GN. Proximal humeral fractures: how stiff should an implant be? A comparative mechanical study with new implants in human specimens. Arch Orthop Trauma Surg. 2003;123(2–3):74–81. doi: 10.1007/s00402-002-0465-9. [DOI] [PubMed] [Google Scholar]
- 18.Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures [corrected] J Bone Joint Surg Am. 2008;90(2):233–240. doi: 10.2106/JBJS.F.01351. [DOI] [PubMed] [Google Scholar]
- 19.Tingart MJ, Lehtinen J, Zurakowski D, Warner JJ, Apreleva M. Proximal humeral fractures: regional differences in bone mineral density of the humeral head affect the fixation strength of cancellous screws. J Shoulder Elbow Surg. 2006;15(5):620–624. doi: 10.1016/j.jse.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Clavert P, Zerah M, Krier J, Mille P, Kempf JF, Kahn JL. Finite element analysis of the strain distribution in the humeral head tubercles during abduction: comparison of young and osteoporotic bone. Surg Radiol Anat. 2006;28(6):581–587. doi: 10.1007/s00276-006-0140-x. [DOI] [PubMed] [Google Scholar]
- 21.Hepp P, Lill H, Bail H, Korner J, Niederhagen M, Haas NP, Josten C, Duda GN. Where should implants be anchored in the humeral head? Clin Orthop Relat Res. 2003;415:139–147. doi: 10.1097/01.blo.0000092968.12414.a8. [DOI] [PubMed] [Google Scholar]
- 22.Liew AS, Johnson JA, Patterson SD, King GJ, Chess DG. Effect of screw placement on fixation in the humeral head. J Shoulder Elbow Surg. 2000;9(5):423–426. doi: 10.1067/mse.2000.107089. [DOI] [PubMed] [Google Scholar]