Abstract
Purpose
The aim of the study was to evaluate whether arthroscopic (ASC) repair of rotator cuff ruptures causes less postoperative pain and better range of motion (ROM) in the early postoperative period than a mini-open (MO) technique.
Methods
Inclusion criteria were a rupture of the supraspinatus tendon with retraction with a maximum to the apex of the humeral head and minor fatty degeneration and atrophy of the muscle. Each group (n = 17) had similar demographics and preoperative magnetic resonance imaging (MRI) findings (mean age 60.1 years, SD 8.8, range 43–71). The ASC group underwent double-row repair with resorbable anchors; the MO group received a transosseous repair. The postoperative rehabilitation was standardised and equivalent in both groups.
Results
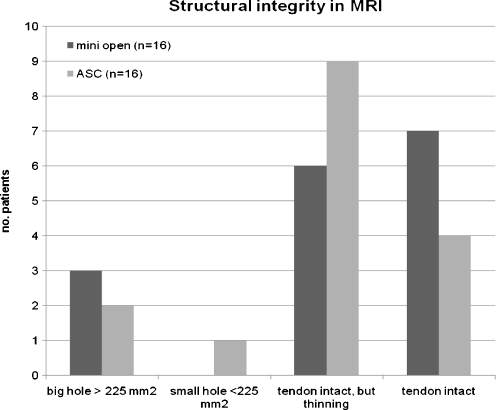
In the first week fewer nonsteroidal anti-inflammatory drug (NSAID) tablets were needed in the ASC group. Pain scores on the visual analogue scale were similar in the first three weeks; however, from week four to eight the MO group had less pain (p < 0.05). After six months, the Constant-Murley score and the ROM improved significantly (p < 0.05) in both groups without differences between the groups. Postoperative MRI revealed in three of 16 patients a discontinuity of the tendon in both groups; in the ASC group there were more patients (n = 9) with a thinning of the tendon compared to the MO group (n = 6).
Conclusions
There was less use of NSAIDs in the first postoperative week in the ASC group, indirectly indicating less pain, but higher pain scores in the later course (weeks four to eight) compared to the MO group. ROM, MRI findings and the scores were similar after six months, demonstrating that both techniques are equivalent regarding the outcome in this period.
Introduction
Symptomatic rotator cuff ruptures (RCR) can be repaired with good outcome if fatty degeneration, atrophy of the muscle and retraction of the tendon are not too severe and the tendon can be repaired without tension to its original insertion site [1–6]. With the evolution of all-arthroscopic (ASC) techniques there is a strong tendency to perform this procedure arthroscopically [7]. Possible advantages of the ASC technique include less trauma to the deltoid, less risk of axillary nerve palsy and better cosmetic results [5, 8–12]. This technique has to be evaluated in comparison to established and successful open techniques [8, 9]. The latter can be categorised into completely open and mini-open (MO) procedures. In the open procedure, an open acromioplasty with release and reattachment of the coracoacromial ligament and a part of the anterior deltoid is performed, and followed by an open repair of the tendon. The MO technique includes an ASC subacromial decompression and an open repair through a deltoid muscle split.
Recent mainly retrospective comparative studies of RCR have demonstrated a similar outcome of ASC compared to MO refixation of RCR. There are few studies that have shown that the ASC patients had less pain and fewer incidences of arthrofibrosis [13–16]. These studies are, however, retrospective and non-randomised. The hypothesis of this prospective randomised comparative study was that ASC repair causes less postoperative pain and gives a better range of motion (ROM) in the early postoperative period. In this study design the authors opted to compare a MO transosseous repair with an ASC double-row refixation technique. The transosseous repair was chosen because it provides a stable [17–19], cost-effective [20, 21] and potentially biologically favourable fixation, since it obviates high stress concentrations of a point fixation with an anchor [22]. For the ASC technique a double-row fixation was used because it provides a similarly stable fixation with comparable footprint coverage [23, 24].
Patients and methods
At a university shoulder department, 34 consecutive patients with an isolated rupture of the supraspinatus tendon were randomised according to an initially established protocol into two groups between July 2007 and July 2009. According to the randomisation protocol the first 17 patients were treated by the MO technique and the next 17 patients by the ASC technique. In this period a total number of 127 patients had surgery for various degrees of RCR. The ASC group underwent a double-row repair of the RCR of the supraspinatus with resorbable anchors (as described below); the other group (MO) received a transosseous repair with Mason-Allen stitches [25]. The local Ethics Committee approved the study (No. S-265/2007) and all patients consented to the study. Inclusion criteria were a rupture of the supraspinatus tendon with no involvement or less than one third involvement of the anterior infraspinatus, retraction to a maximum of the apex of the humeral head (less than category 2 according to Patte [26]), minor fatty degeneration (less than category 3 according to Fuchs et al. [27]) and atrophy of the muscle (less than category 3 according to Thomazeau et al. [28]). Symptomatic acromioclavicular (AC) degeneration requiring the additional procedure of a lateral clavicular resection was an exclusion criterion. There were two smokers in the ASC and three smokers and two diabetics in the MO group. Each group (n = 17) had similar demographics and preoperative magnetic resonance imaging (MRI) findings that were not significantly different between the groups in the Wilcoxon test.
The ASC group (mean age 60.1 years, SD 8.6, range 47–71; nine men/eight women, nine right/eight left side) included 12 with no or minimal retraction and five up to the apex of the humeral head (17×1° according to Patte), fatty degeneration according to Fuchs et al. 12×0°, 4×1° and 1×2°, and atrophy according to Thomazeau et al. 15×1° and 2×2°. The extent of the rupture in the anteroposterior (AP) dimensions averaged 2.9 cm (SD 1.07).
The MO group (mean age 60.1 years, SD 9, range 43–70; 12 men/five women, 12 right/five left side) also included 12 with no or minimal retraction and five up to the apex of the humeral head (17×1° according to Patte), fatty degeneration according to Fuchs et al. 8×0°, 7×1° and 2×2°, and atrophy according to Thomazeau et al. 16×1° and 1×2°. The extent of the rupture in the AP dimensions averaged 2.2 cm (SD 0.86).
Preoperative (n = 17 in both groups) and six month (n = 16 in both groups) postoperative MRI (1.5 T) included standard parasagittal, coronal and axial T1-weighted, T2-weighted and fast spin echo sequences. A blinded senior radiologist (TG) rated the size of the rupture and the postoperative integrity of the tendon according to a new classification system that was adapted from the one of Sugaya et al. [29]: (1 = tendon intact with regular thickness, 2 = tendon intact, but thinning, 3 = small hole < 225 mm24 = big hole > 225 mm2). We chose to use this slightly modified classification system because the differentiation of tendon of sufficient thickness with homogeneously low intensity (type 1 according to Sugaya et al.) and type 2 (sufficient thickness with partial high intensity) appeared less relevant in our situation. These two types were summarised in one category in our classification, because six months after the operation it is unusual to have a homogeneously low intensity of the tendon. Type 3 according to Sugaya et al. is identical to our category 2. Furthermore, Sugaya et al. distinguish between a minor (type 4) and a major discontinuity (type 5) without specifying the extent in mm2. Consequently, for a more reliable differentiation, we determined a minor discontinuity to be less than 225 mm2 (e.g. 1.5 × 1.5 cm) and a major discontinuity to be more than 225 mm2.
Surgical technique
The patients were operated upon in the beach chair position under general anaesthesia. All patients received perioperative nonsteroidal anti-inflammatory drugs (NSAIDs) (diclofenac 50 mg 1-0-1) and opioids for pain medication and an interscalene block for two days. All operations were performed by two senior shoulder surgeons. One surgeon (PK) performed all arthroscopic operations and the MO patients were treated by PK in ten cases and the remaining seven by ML. All patients received an ASC subacromial decompression with release of the coracoacromial ligament and anterior of the acromion with bony resection depending on the individual anatomy ranging from 5 to 8 mm for signs of mechanical impingement (fraying of the bursal side of the supraspinatus tendon) [30]. Furthermore, a biceps tenodesis was performed in all patients to avoid increased pressure of the repaired supraspinatus tendon on the posterior pulley system of the biceps tendon, which in our experience can cause postoperative biceps tendinitis and pain. In the ASC group the biceps tenodesis was done with the first anchor (made out of polylactic acid, SPIRALOK, DePuy Mitek, Norderstedt, Germany) placed medially at the footprint of the supraspinatus just posterior to the bicipitalgroove with a lasso-loop stitch [31] and in the MO group by transosseous sutures through the posterior wall of the sulcus. If the tendon/muscle unit was rather stiff, care was taken to perform a periglenoidal release of the supraspinatus tendon to allow tension-free reduction of the edge of the tear to the original insertion site of the supraspinatus in both techniques. The bursa was removed as much as necessary to allow sufficient visualisation to perform the repair in both groups.
If the tear was larger than 2.0 cm in the AP dimension in the ASC technique two medial anchors (made of polylactic acid, SPIRALOK, DePuy Mitek, Norderstedt, Germany) were used, otherwise one medial anchor was used in the ASC group. The sutures were passed through the tendon approximately 2.5 cm medial of the tear edge by penetrating graspers (CleverHook, DePuy Mitek, Norderstedt, Germany) in a mattress configuration. A lateral anchor (SPIRALOK, DePuy Mitek, Norderstedt, Germany) was placed just lateral of the footprint and the sutures were passed through the tendon in a lasso-loop [31] and single-stitch configuration approximately 1 cm medial of the edge. The lateral row was tied first and then the medial row to enable ideal coverage of the footprint.
In the MO technique through an anterior lateral deltoid split, two (or three in the case of a tear larger than 2.5 cm anterior/posterior) FiberWire (Arthrex, Karlsfeld, Germany) No. 2 sutures were passed through the tendon in a Mason-Allen configuration approximately 2.5 cm medial of the tear edge by round needles. A shallow laterally based trough was created and the sutures were passed from the medial part of the footprint to a site approximately 2.5 distal of the lateral edge of the footprint.
Pain medication, scores and postoperative rehabilitation programme
Pain was monitored with a standardised form on a weekly basis including the visual analogue scale (VAS, min. 0, max. 10), the amount of NSAIDs per day and opioid tablets per day for three months. The patients were advised to use NSAIDs up to a maximum dose of 200 mg diclofenac (i.e. four tablets per day as needed) and tramadole 300 mg (i.e. two tablets per day), but to refrain from taking tablets if they did not have pain. The patients were asked to rate the pain beginning from the end of the first week before taking pain medication. In the ASC group 14 patients (82% follow-up rate) and in the MO group 16 patients (94% follow-up rate) returned the questionnaire after three months. The patients were scored preoperatively, after three (n = 17 in both groups) and six months (n = 17 in the ASC and n = 16 in the MO group) with the Constant-Murley score [32] and the American Shoulder and Elbow Society (ASES) shoulder index score (min. 0, max. 100).
The postoperative rehabilitation for both groups consisted of four weeks abduction pillow with 30° of abduction and passive ROM exercises by a physiotherapist. Afterwards, active ROM of the arm without limitations was allowed. The amount of postoperative physical therapy was monitored by a questionnaire and was equivalent for both groups: The ASC group received 27.9 (SD 11.2) physiotherapy sessions and the MO group 25.4 sessions (SD 13.1) [difference not significant (NS)]. Afterwards, the patients continued home exercises with a frequency of 2.5×/week (SD 0.7) in the ASC group and 2.6×/week (SD 0.6) in the MO group (NS).
Statistics
The statistical analysis was performed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). Group mean values (MV) and standard deviations (SD) were calculated. A p value <0.05 was considered significant. The primary outcome parameter was the VAS; secondary outcome parameters were the amount of pain medication the patients used throughout the first three months, the ASES score, the Constant-Murley score, the integrity of the repair in the MRI and the ROM after six months. A power analysis with 80% with an expected difference on the VAS of 1.9 points yielded n = 14 for both groups. Differences between the groups and the values at different time points were compared with the Wilcoxon test.
Results
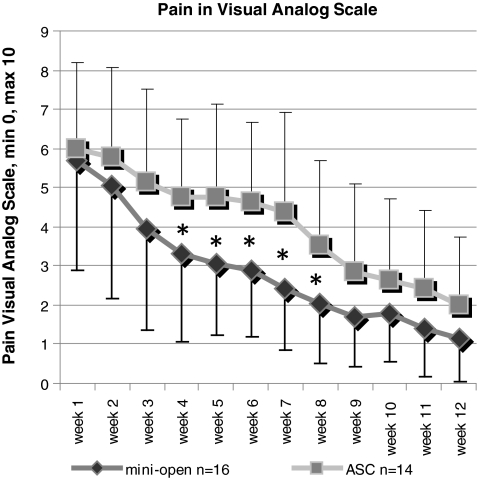
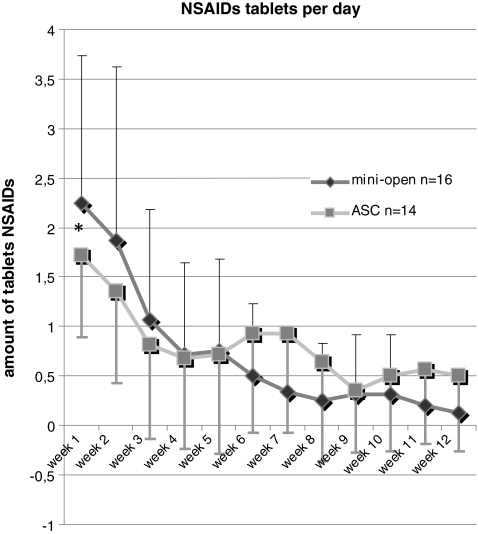
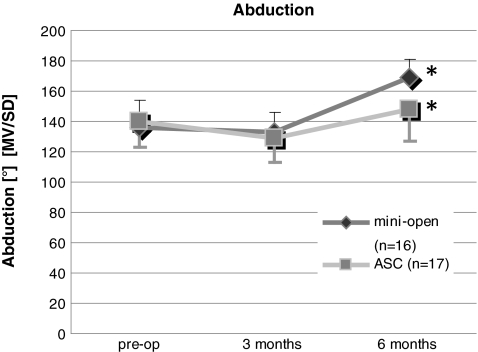
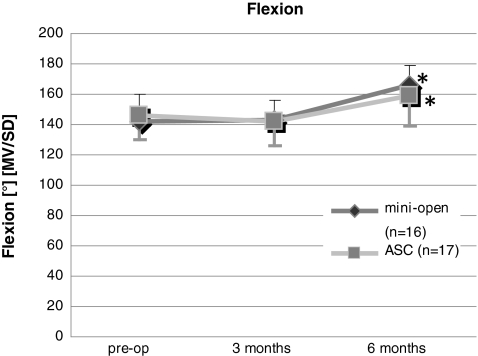
Pain scores on the VAS were similar in the first three weeks; however, from week four to eight the MO group had less pain (Fig. 1, p < 0.042). The VAS scores in the MO group were 3.3 (SD 2.3) after four weeks compared to the ASC group with 4.7 (SD 1.9), and after eight weeks in the MO group 2 (SD 1.5) compared to the ASC group with 3.5 (SD 2.1). In the first week fewer NSAID tablets were needed in the ASC group with 2.2 tablets (SD 1.4) versus 1.6 tablets (SD 0.9) in the MO group (Fig. 2, p = 0.027). The need for opioids was low after the first postoperative weeks in both groups, and there was no significant difference between the groups. Flexion, abduction and external rotation improved in both groups mainly from three to six months postoperatively (Figs. 3, 4, 5, p < 0.047). However, there were no significant differences between the ASC and MO groups.
Fig. 1.
Pain was monitored with the VAS (min. 0, max. 10) for 3 months in weekly intervals beginning from the end of the first week postoperatively. There were significantly lower numbers in the MO group in weeks 4–8 in the Wilcoxon test (*p < 0.042). Mean values and standard deviations are shown
Fig. 2.
Pain was also indirectly monitored by the amount of NSAIDs per day for 3 months in weekly intervals beginning from the end of the first week postoperatively. There were significantly lower numbers in the ASC group in the first week (*p = 0.027), but an increase in weeks 6–9 was noted that did not reach significance. Mean values and standard deviations are shown
Fig. 3.
Abduction increased from 3 to 6 months postoperatively (*p < 0.05). There were no significant differences between the ASC and MO groups. Mean values and standard deviations are shown
Fig. 4.
Flexion increased from 3 to 6 months postoperatively (*p < 0.05). There were no significant differences between the ASC and MO groups. Mean values and standard deviations are shown
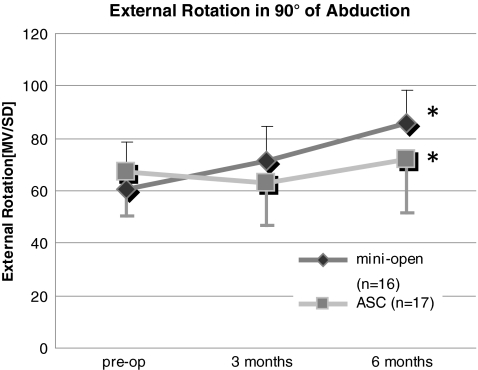
Fig. 5.
External rotation at 90° abduction increased from 3 to 6 months postoperatively (*p < 0.05). There were no significant differences between the ASC and MO groups. Mean values and standard deviations are shown
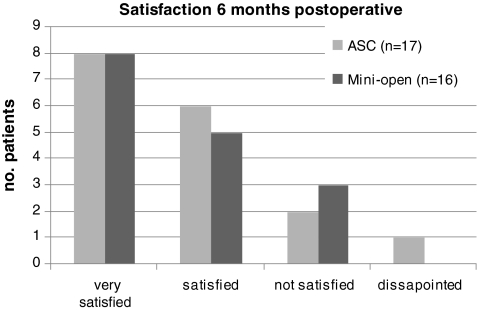
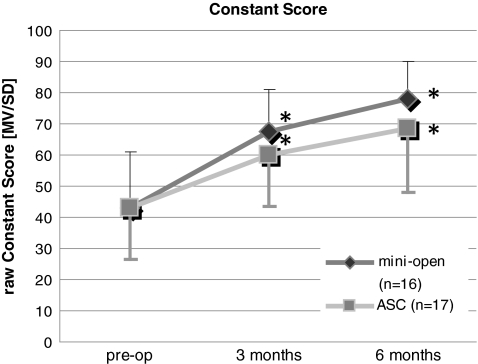
Satisfaction was high in both groups (NS between both groups) after six months (Fig. 6). In the ASC group 14 of 17 rated their condition as being better than preoperatively and three of 17 as the same. In the MO group 13 of 15 reported an improvement of their postoperative condition and two of 15 a deterioration. After six months, the raw Constant-Murley score improved both from preoperatively to three months and from three to six months in both groups (p < 0.01, Fig. 7). The Constant-Murley score improved in the first six months by 20.8. points (SD 35.5) in the MO group and 25.2 (SD 21.5) in the ASC group. However, there was no significant difference between the ASC and MO groups. The shoulder score index of the ASES reflecting the activities of daily living improved significantly (p < 0.05) in both groups without differences between the groups [ASC group from 44.3 points (SD 14.5) to 81 (SD 20) and MO group from 48.26 points (SD 20) to 86.9 (SD 16.3)]. In both groups three of 16 patients had a discontinuity of the tendon in the MRI. In the MO group the mode of failure was at the lateral insertion site in three of three cases, and in the ASC group at the lateral insertion in one case and medial of the medial anchors in two cases. In the ASC group there were more patients (n = 9) with a thinning of the tendon compared to the MO group (n = 6) (Fig. 8). In these cases there was tendon material in all slices of the MRI, but the tendon appeared to have less thickness than a regular tendon.
Fig. 6.
Satisfaction was high in both groups (NS between both groups) after 6 months
Fig. 7.
The raw Constant-Murley score improved both from preoperative to 3 months and from 3 to 6 months in both groups (p > 0.01). There was no significant difference between the ASC and MO groups
Fig. 8.
In the MRI 3 of 16 patients had a discontinuity of the tendon in both groups; however, in the ASC group there were more patients (n = 9) with a thinning of the tendon compared to the MO group (n = 6)
Discussion
The data demonstrate that there is no clear superiority of the ASC technique regarding postoperative pain and ROM compared to the MO group in the first three months. Advocates of the ASC technique often argue that the ASC technique causes less pain and allows for better ROM in the earlier postoperative period. This might reduce the period patients have to be off work and indirectly reduce disease-associated costs. In this study, however, pain scores from week four to eight were higher in the ASC group than in the MO group. The reasons for this finding might be technical: Possibly in the MO group the periglenoidal release was done more extensively because bleeding is less of an issue compared to ASC where clear vision of the repair is required. However, a more extensive release is said to be beneficial for tension reduction in the muscle tendon unit which could relieve postoperative pain. Having said that, it is important to mention that with further improvement of surgical technique an arthroscopic release can be done as well as or with even greater control than in the open technique. Another issue is the swelling of the soft tissues during ASC that could impair healing in the very short term. However, clinically the swelling recedes relatively quickly within one day postoperatively which makes this issue less relevant. Another issue is the bursa: During ASC slightly more bursa must be removed to obtain good visualisation. However, the bursa has a high vascularity and contains cells that could facilitate healing [33]. On the other hand, elevated levels of cytokines associated with inflammation and pain mediators can be found in cases of patients with bursitis [34–36] and removal of this tissue might be beneficial. From our current state of knowledge we cannot define the role of the bursa. In our approach we remove only as much bursa as necessary to perform the surgery.
The majority of studies including meta-analyses comparing ASC and MO techniques have not shown a better outcome either by the ASC or the MO technique [10–12, 21, 37–39] (Table 1). However, some studies indicate that the ASC technique yields a better outcome: Buess et al. retrospectively reviewed a case series including heterogeneous pathological conditions (e.g. partial ruptures, AC joint resections, subscapularis ruptures) by subjective scores such as the VAS, the simple shoulder test (SST) and patient satisfaction [15]. The authors found a higher improvement of pain scores in the ASC than in the MO group. The SST and patient satisfaction were similar. Limitations of the latter study are its retrospective nature, the heterogeneous pathology and the sole use of a questionnaire. Severud et al. published a retrospective series comparing the ASC and MO techniques [16]. Motion was slightly better in the ASC group (significant at six and 12 weeks, NS at final follow-up) with no shoulder stiffness compared to the MO group with 14% stiffness. While interpreting the results, one has to take into account the heterogeneity of the study groups. The MO group had more (n = 18) large tears than the ASC (n = 9) group. A selection bias might also be the problem with another study by Colegate-Stone et al. [13]: tears with less than 3 cm in diameter were repaired arthroscopically while tears larger than 3 cm were done with a MO procedure. Accordingly, the ASC group performed better regarding the Constant-Murley, disabilities of the arm, shoulder and hand (DASH) and Oxford scores over 24 months. Millar et al. found 20% better ASES scores and less retears in ultrasound studies in the ASC groups than in a MO double-row anchor fixation [14]. Other scores were similar in the groups (Table 1). Limitations of that study are the retrospective cohort design, a large proportion (48%) of patients lost to follow-up by two years post-surgery and various sonographers performing the imaging.
Table 1.
Studies comparing approaches to rotator cuff repair
| Authors (year) | Comparison | Type of study | Mean follow-up period, months (min.) | Outcome |
|---|---|---|---|---|
| Kim et al. (2003) [2] | ASC (n = 42) vs MO (n = 34) | Retrospective | 39 (24) | UCLA and ASES scores, pain equivalent |
| Severud et al. (2004) [16] | ASC (n = 35) vs MO (n = 29) | Retrospective | 44.6 (24) | UCLA, ASES equivalent, ASC less fibrous ankylosis |
| Buess et al. (2005) [15] | ASC (n = 66) vs MO and open (n = 30) | Retrospective | 24.6 (15) | ASC less pain on VAS |
| Sauerbrey et al. (2005) [5] | ASC (n = 28) vs MO (n = 26) | Retrospective | 33 (18) | ASES equivalent |
| Youm et al. (2005) [12] | ASC (n = 42) vs MO (n = 42) | Retrospective | 36.3 (24) | ASES, UCLA equivalent |
| Warner et al. (2005) [11] | ASC (n = 9) vs MO (n = 12) | Retrospective | 50 (27) | SST, pain scores equivalent |
| Ide et al. (2005) [39] | ASC (n = 50) vs MO (n = 50) | Retrospective of prospective data | 49 ( 25) | UCLA and JOA equivalent |
| Verma et al. (2006) [10] | ASC (n = 38) vs MO (n = 33) | Retrospective | 39.9 (24) | ASES, SST, VAS equivalent |
| Mohtadi et al. (2008) [40] | Open (n = 29) vs MO (n = 31) | Prospective randomised | 24 | RC-QOL index better in the MO than the open group at 3 months; at 1 and 2 years NS |
| Köse et al. (2008) [21] | ASC (n = 25) vs MO (n = 25) | Retrospective | ASC 21, MO 31 | CS and UCLA scores equivalent |
| Colegate-Stone et al. (2009) [13] | ASC (tear <3 cm) (n = 92) vs MO (>3 cm) (n = 31) | Retrospective of prospective data | 24 | Attention: BIAS due to tear size, ASC superior in CS, DASH and Oxford scores |
| Osti et al. (2010) [38] | ASC (n = 32) vs MO (n = 32) | Retrospective | 31 (24) | ROM, SF-36 and UCLA scores equivalent |
| Millar et al. (2009) [14] | ASC knotted (n = 53) vs ASC knotless (n = 57) vs MO (n = 49) | Retrospective of prospective data | 24, n = 106 (6) | ASC 20% better ASES index, other scores (pain, stiffness, function) equivalent; higher retear rates (39%) in MO group compared to ASC knotted 25% and ASC knotless 16% |
ASES American Shoulder and Elbow Society, UCLA University of California, Los Angeles, SST simple shoulder test, VAS visual analogue scale, CS Constant-Murley score, JOA Japanese Orthopaedic Society, ROM range of motion, DASH disabilities of the arm, shoulder and hand, RC-QOL rotator cuff quality of life
Recently, some studies have compared the costs of the two techniques. Indeed, costs of both techniques differ tremendously: the ASC technique is more expensive mainly due to longer operating time and implants [20, 21].
A limitation of our study is the relatively small number of patients within the groups. In spite of this fact significant differences were seen between the groups. Future studies should address this issue. Furthermore, two different surgeons performed the surgery, which might influence the outcome. However, one surgeon was the senior resident of the other surgeon, having been trained by him, so one can assume a similar technique. The short-term results are another limitation; however, the focus was on the potential advantage of the ASC in the early postoperative period with less operative trauma, less pain and quicker rehabilitation. Another issue is the fact that the repair techniques were not identical. However, the aim of this study was not a comparison of an arthroscopic double-row repair to an open double-row repair, but comparison of what we considered the gold standard of each technique. It did not make sense to us to perform an open double-row with its known disadvantages such as anchor point fixation, implantation of multiple anchors in the bone with potential “toxic overload” and increased costs without a known benefit in comparison to a traditional transosseous suture repair.
Conclusion
In conclusion, there was less use of NSAIDs in the first postoperative week in the ASC group, indirectly indicating less pain, but higher pain scores in the later course (weeks four to eight) compared to the MO group. ROM, MRI findings and the scores were similar after six months, demonstrating that both techniques are equivalent regarding the outcome in this period. Based on these results, both surgical techniques are good options to repair a rupture of the supraspinatus tendon and to improve the symptoms of the patients.
Acknowledgments
Funding This work was supported by the research fund of the Orthopaedic Surgery Hospital of the University of Heidelberg. The local Ethics Committee approved the study (No. S-265/2007) and all patients consented to the study.
Conflict of interest The authors declare that they have no conflict of interest.
Footnotes
Level of evidence
Level III treatment study
References
- 1.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 2.Kim SH, Ha KI, Park JH, Kang JS, Oh SK, Oh I. Arthroscopic versus mini-open salvage repair of the rotator cuff tear: outcome analysis at 2 to 6 years’ follow-up. Arthroscopy. 2003;19:746–754. doi: 10.1016/S0749-8063(03)00395-5. [DOI] [PubMed] [Google Scholar]
- 3.Lafosse L, Brozska R, Toussaint B, Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Bone Joint Surg Am. 2007;89:1533–1541. doi: 10.2106/JBJS.F.00305. [DOI] [PubMed] [Google Scholar]
- 4.Lichtenberg S, Liem D, Magosch P, Habermeyer P. Influence of tendon healing after arthroscopic rotator cuff repair on clinical outcome using single-row Mason-Allen suture technique: a prospective, MRI controlled study. Knee Surg Sports Traumatol Arthrosc. 2006;14:1200–1206. doi: 10.1007/s00167-006-0132-8. [DOI] [PubMed] [Google Scholar]
- 5.Sauerbrey AM, Getz CL, Piancastelli M, Iannotti JP, Ramsey ML, Williams GR., Jr Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcome. Arthroscopy. 2005;21:1415–1420. doi: 10.1016/j.arthro.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 6.Yamaguchi K, Ball CM, Galatz LM. Arthroscopic rotator cuff repair: transition from mini-open to all-arthroscopic. Clin Orthop Relat Res. 2001;390:83–94. doi: 10.1097/00003086-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Yamaguchi K, Levine WN, Marra G, Galatz LM, Klepps S, Flatow EL. Transitioning to arthroscopic rotator cuff repair: the pros and cons. Instr Course Lect. 2003;52:81–92. [PubMed] [Google Scholar]
- 8.Motycka T, Kriegleder B, Landsiedl F. Results of open repair of the rotator cuff–a long-term review of 79 shoulders. Arch Orthop Trauma Surg. 2001;121:148–151. doi: 10.1007/s004020000199. [DOI] [PubMed] [Google Scholar]
- 9.Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J Bone Joint Surg Am. 2001;83-A:71–77. doi: 10.2106/00004623-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Verma NN, Dunn W, Adler RS, Cordasco FA, Allen A, MacGillivray J, Craig E, Warren RF, Altchek DW. All-arthroscopic versus mini-open rotator cuff repair: a retrospective review with minimum 2-year follow-up. Arthroscopy. 2006;22:587–594. doi: 10.1016/j.arthro.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 11.Warner JJ, Tétreault P, Lehtinen J, Zurakowski D. Arthroscopic versus mini-open rotator cuff repair: a cohort comparison study. Arthroscopy. 2005;21:328–332. doi: 10.1016/j.arthro.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 12.Youm T, Murray DH, Kubiak EN, Rokito AS, Zuckerman JD. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcomes and patient satisfaction. J Shoulder Elbow Surg. 2005;14:455–459. doi: 10.1016/j.jse.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Colegate-Stone T, Allom R, Tavakkolizadeh A, Sinha J. An analysis of outcome of arthroscopic versus mini-open rotator cuff repair using subjective and objective scoring tools. Knee Surg Sports Traumatol Arthrosc. 2009;17:691–694. doi: 10.1007/s00167-008-0661-4. [DOI] [PubMed] [Google Scholar]
- 14.Millar NL, Wu X, Tantau R, Silverstone E, Murrell GA. Open versus two forms of arthroscopic rotator cuff repair. Clin Orthop Relat Res. 2009;467:966–978. doi: 10.1007/s11999-009-0706-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buess E, Steuber KU, Waibl B. Open versus arthroscopic rotator cuff repair: a comparative view of 96 cases. Arthroscopy. 2005;21:597–604. doi: 10.1016/j.arthro.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Severud EL, Ruotolo C, Abbott DD, Nottage WM. All-arthroscopic versus mini-open rotator cuff repair: a long-term retrospective outcome comparison. Arthroscopy. 2003;19:234–238. doi: 10.1053/jars.2003.50036. [DOI] [PubMed] [Google Scholar]
- 17.Rickert M, Witzel U, Kölbel R, Georgousis H. Primary strength of conventional and alternative suture techniques of the rotator cuff. A biomechanical study. Unfallchirurg. 2002;105:23–30. doi: 10.1007/s113-002-8161-9. [DOI] [PubMed] [Google Scholar]
- 18.Schneeberger AG, Roll A, Kalberer F, Jacob HA, Gerber C. Mechanical strength of arthroscopic rotator cuff repair techniques: an in vitro study. J Bone Joint Surg Am. 2002;84-A:2152–2160. doi: 10.2106/00004623-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Park MC, Cadet ER, Levine WN, Bigliani LU, Ahmad CS. Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med. 2005;33:1154–1159. doi: 10.1177/0363546504273053. [DOI] [PubMed] [Google Scholar]
- 20.Churchill RS, Ghorai JK. Total cost and operating room time comparison of rotator cuff repair techniques at low, intermediate, and high volume centers: mini-open versus all-arthroscopic. J Shoulder Elbow Surg. 2010;19:716–721. doi: 10.1016/j.jse.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 21.Köse KC, Tezen E, Cebesoy O, Karadeniz E, Guner D, Adiyaman S, Demirtas M. Mini-open versus all-arthroscopic rotator cuff repair: comparison of the operative costs and the clinical outcomes. Adv Ther. 2008;25:249–259. doi: 10.1007/s12325-008-0031-0. [DOI] [PubMed] [Google Scholar]
- 22.Sano H, Yamashita T, Wakabayashi I, Itoi E. Stress distribution in the supraspinatus tendon after tendon repair: suture anchors versus transosseous suture fixation. Am J Sports Med. 2007;35:542–546. doi: 10.1177/0363546506296310. [DOI] [PubMed] [Google Scholar]
- 23.Tuoheti Y, Itoi E, Yamamoto N, Seki N, Abe H, Minagawa H, Okada K, Shimada Y. Contact area, contact pressure, and pressure patterns of the tendon-bone interface after rotator cuff repair. Am J Sports Med. 2005;33:1869–1874. doi: 10.1177/0363546505278256. [DOI] [PubMed] [Google Scholar]
- 24.Meier SW, Meier JD. The effect of double-row fixation on initial repair strength in rotator cuff repair: a biomechanical study. Arthroscopy. 2006;22:1168–1173. doi: 10.1016/j.arthro.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Cofield RH. Rotator cuff disease of the shoulder. J Bone Joint Surg Am. 1985;67:974–979. [PubMed] [Google Scholar]
- 26.Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990;254:81–86. [PubMed] [Google Scholar]
- 27.Fuchs B, Gilbart MK, Hodler J, Gerber C. Clinical and structural results of open repair of an isolated one-tendon tear of the rotator cuff. J Bone Joint Surg Am. 2006;88:309–316. doi: 10.2106/JBJS.E.00117. [DOI] [PubMed] [Google Scholar]
- 28.Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand. 1996;67:264–268. doi: 10.3109/17453679608994685. [DOI] [PubMed] [Google Scholar]
- 29.Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21:1307–1316. doi: 10.1016/j.arthro.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 30.Sampson TG, Nisbet JK, Glick JM. Precision acromioplasty in arthroscopic subacromial decompression of the shoulder. Arthroscopy. 1991;7:301–307. doi: 10.1016/0749-8063(91)90132-H. [DOI] [PubMed] [Google Scholar]
- 31.Lafosse L, Raebroeckx A, Brzoska R. A new technique to improve tissue grip: “the lasso-loop stitch”. Arthroscopy. 2006;22:1246.e1–1246.e3. doi: 10.1016/j.arthro.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 32.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 33.Yanagisawa K, Hamada K, Gotoh M, Tokunaga T, Oshika Y, Tomisawa M, Lee YH, Handa A, Kijima H, Yamazaki H, Nakamura M, Ueyama Y, Tamaoki N, Fukuda H. Vascular endothelial growth factor (VEGF) expression in the subacromial bursa is increased in patients with impingement syndrome. J Orthop Res. 2001;19:448–455. doi: 10.1016/S0736-0266(00)90021-4. [DOI] [PubMed] [Google Scholar]
- 34.Ko JY, Wang FS, Huang HY, Wang CJ, Tseng SL, Hsu C. Increased IL-1beta expression and myofibroblast recruitment in subacromial bursa is associated with rotator cuff lesions with shoulder stiffness. J Orthop Res. 2008;26:1090–1097. doi: 10.1002/jor.20631. [DOI] [PubMed] [Google Scholar]
- 35.Blaine TA, Kim YS, Voloshin I, Chen D, Murakami K, Chang SS, Winchester R, Lee FY, O’Keefe RJ, Bigliani LU. The molecular pathophysiology of subacromial bursitis in rotator cuff disease. J Shoulder Elbow Surg. 2005;14:84S–89S. doi: 10.1016/j.jse.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 36.Gotoh M, Hamada K, Yamakawa H, Yanagisawa K, Nakamura M, Yamazaki H, Ueyama Y, Tamaoki N, Inoue A, Fukuda H. Interleukin-1-induced subacromial synovitis and shoulder pain in rotator cuff diseases. Rheumatology (Oxford) 2001;40:995–1001. doi: 10.1093/rheumatology/40.9.995. [DOI] [PubMed] [Google Scholar]
- 37.Morse K, Davis AD, Afra R, Kaye EK, Schepsis A, Voloshin I. Arthroscopic versus mini-open rotator cuff repair: a comprehensive review and meta-analysis. Am J Sports Med. 2008;36:1824–1828. doi: 10.1177/0363546508322903. [DOI] [PubMed] [Google Scholar]
- 38.Osti L, Papalia R, Paganelli M, Denaro E, Maffulli N. Arthroscopic vs mini-open rotator cuff repair. A quality of life impairment study. Int Orthop. 2010;34:389–394. doi: 10.1007/s00264-009-0796-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ide J, Maeda S, Takagi K. A comparison of arthroscopic and open rotator cuff repair. Arthroscopy. 2005;21:1090–1098. doi: 10.1016/j.arthro.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 40.Mohtadi NG, Hollinshead RM, Sasyniuk TM, Fletcher JA, Chan DS, Li FX. A randomized clinical trial comparing open to arthroscopic acromioplasty with mini-open rotator cuff repair for full-thickness rotator cuff tears: disease-specific quality of life outcome at an average 2-year follow-up. Am J Sports Med. 2008;36:1043–1051. doi: 10.1177/0363546508314409. [DOI] [PubMed] [Google Scholar]