Abstract
Purpose
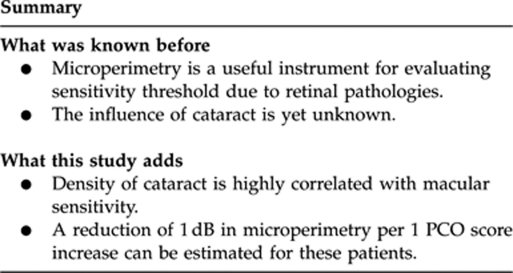
Microperimetry is a useful instrument for evaluating sensitivity threshold due to retinal pathologies. The aim of the study is to assess the impact of different forms of cataract on microperimetry results.
Methods
In a prospective design, patients were recruited for cataract surgery at the Department of Ophthalmology, Medical University of Vienna. Exclusion criteria were any other ophthalmic disease except cataract, that is, macular pathology. Using the Lens Opacities Classification System III classification, patients were classified into four groups: nuclear, cortical, subcapsular posterior, and mixed cataract. Then patients underwent microperimetry: results were analyzed for magnitude of retinal sensitivity loss and correlated to the forms and density of the cataract.
Results
Mean density of cataract was LOCS 3.2–3.5 in the four groups. Differences were not statistically significant. The best-corrected visual acuity (BCVA) was LogMAR 0.5±0.13 in nuclear, LogMAR 0.49±0.21 in cortical, and LogMAR 0.58±0.12 in mixed cataract patients, and significantly worse in patients with subcapsular posterior cataract (LogMAR 0.64±0.12). Microperimetry shows a mean sensitivity of 11.4–12.6 dB without significant group differences. The BCVA is correlated with microperimetry in patients with nuclear and cortical cataract. Density of cataract is highly correlated with microperimetry results in all groups.
Conclusion
The present study shows a good correlation of microperimetry results with the BCVA of patients with nuclear and cortical cataract. In patients with subcapsular posterior cataract, microperimetry results were better than estimated by BCVA. Density of cataract is highly correlated with macular sensitivity. A reduction of 1 dB in microperimetry per 1 posterior capsule opacification score increase can be estimated for these patients.
Keywords: microperimetry, retinal sensitivity, cataract, density of cataract, PCO score, best corrected visual acuity
Introduction
Age-related macular degeneration (AMD) is the leading cause of irreversible visual loss in the Western world in individuals over 60 years old.1, 2, 3, 4 For these patients a precise evaluation of functional vision is necessary, both for estimation of the need for therapeutic and supportive interventions and the measurement of the outcome of such care. However, high-contrast visual acuity measurements alone have been shown to be a poor predictor of visual function.5, 6, 7 One test of visual function that may help to better understand the characteristics of visual loss in these patients is microperimetry. The information given by this functional test provides valuable information about the location of the retinal sensitivity loss, its magnitude, and its potential influence on central fixation. The knowledge of sensitivity parameters and fixation in eyes with AMD, and their relationship to duration of disease may help to understand the mechanisms of visual loss in the disease, and provide a useful instrument for the early clinical assessment of visual deficits, and following recommendations concerning visual rehabilitation with low-vision aids.
In the past, the scanning laser ophthalmoscope (SLO, Rodenstock, Germany) was the only commercially available microperimeter. But important software features, such as real time fundus tracking, were lacking. Additionally, the SLO is no longer for purchase.8 A few years ago, an instrument called the Microperimeter 1 (MP1, Nidek Technologies, Padova, Italy) has been introduced. This instrument allows for fundus perimetry a larger field with automated full-threshold perimetry software, and stability of fixation is measured automatically by an integrated eye tracking system. Furthermore, real-color fundus image acquisition is possible with an overlay of the perimetric findings onto the fundus image.8, 9
As AMD-patients are aged over 50 years, most of them present cataract as well. However, until now, data concerning the influence of cataract on the evaluation of microperimetry are lacking. As there are different types of cataract (nuclear, cortical, mixed nuclear-cortical, and subcapsular), these might influence the microperimtery differently.
In a previous study by Stifter et al10 it was found that for some types of cataract (dense nuclear and subcapsular posterior) maximal reading speed is significantly reduced preoperatively, but in patients with nuclear–cortical cataract maximal reading speed remained unaffected.
We therefore believe that different types of cataract might also influence the microperimetric results, as the heterogeneity of different cataract types directly influences the retinal image and visual function. If cataract had an influence on these measures in patients with AMD, a worsening of the microperimetric results can result either from a progression of the AMD or from the cataract. However, not knowing the influence of the cataract, recommendations concerning therapy or visual rehabilitation with low-vision aids might not be the correct form of treatment.
The objective of the present study is to investigate the influence of different forms of cataract, predominantly cortical, nuclear, or subcapsular posterior, on the evaluation of microperimetry.
Materials and methods
A total of 85 patients were recruited consecutively from the Department of Ophthalmology, Medical University of Vienna, and were assigned to the study. Patients signed informed consent before the study, and then underwent standard preoperative examinations: refractive status was determined and best-corrected LogMAR visual acuity was evaluated using the ETDRS charts. Slit-lamp examination followed. After dilating the pupil, cataract was categorized and graded using the Lens Opacities Classification System (LOCS III)11 with grading of nuclear opalescence and color (N; 0.1–6.9), cortical opacity (C; 0.1–5.9), and subcapsular opacity (P; 0.1–5.9). Patients were divided into four groups according to the type of the present cataract: group 1, Nuclear cataract (N); group 2, Cortical cataract (C); group 3, Subcapsular posterior cataract (S); and group 4, Mixed cataract (M). Patients were selected for the pure cataract group if only one parameter of the LOCS grading system was higher than LOCS 2. If an eye presented more than one parameter with LOCS grading 2 or more, the patient was selected for mixed cataract group. For analysis of cataract density, the parameter with the highest LOCS was used.
Microperimetry was carried out using the MP1. For assessing visual threshold, a 4-2-1 staircase strategy was used, a test grid with 41 stimulus locations covering an area of 10° was applied. The stimuli were projected on a white background with black illumination set to 1.27 cd/m2 and a stimulus presentation time of 200 ms. A single cross of 3° was used as fixation target. For assessment of fixation, the fundus movements are tracked during examination, while the patient gazed at the fixation target. The autotracking system calculates horizontal and vertical shifts relative to a reference frame and draws a map of the patient's eye movements during the examination. The recorded fixation points are classified into three categories for fixation analysis (stable, relatively unstable, and unstable).8
Inclusion criteria were age over 50 years, age-related cataract, and normal fundus findings with no signs of age-related maculopathy. OCT scan was performed to assure absence of macular pathology.
Exclusion criteria were preoperative findings of amblyopia, glaucoma, proliferative diabetic retinopathy, macular edema, retinal detachment, uveitis, previous intraocular, or corneal surgery, including refractive surgery or corneal transplant.
History of other pathologies potentially affecting visual acuity, for example, macular degeneration, and other macular disorders, retinal vascular disease, was considered.
Corneal irregularities potentially affecting visual acuity, for example, keratoconous or corneal dystrophy, were also considered.
The patients gave written consent for participating in the study.
Microperimetry results were analyzed for the existence of retinal sensitivity loss, its magnitude, and its potential influence on central fixation, and were correlated to the forms and density of the cataract.
Statistical analysis
Statistical analysis was performed with SPSS 11.0 (SPSS Inc., Chicago, IL, USA). Data were analyzed for significance by ANOVA if showing normal distribution. For non-parametric data the Mann–Whitney U test was used. Correlations were tested by linear regression analysis and analysis of variance with Pearson's correlation test. P-values <0.05 were considered clinically significant.
Results
Patient population
Of the 85 patients, 5 were excluded, as microperimetry could not be performed owing to cognitive or physical handicap. The remaining 80 patients were divided into four groups according to their form of presenting cataract:
Group 1: Nuclear cataract (N) (n=21)
Group 2: Cortical cataract (C) (n=21)
Group 3: Subcapsular posterior cataract (S) (n=18)
Group 4: Mixed cataract (M) (n=20)
The mean patients' age was 73.5±7.8 years. There were no statistically significant differences in patients' age within the four groups. Gender distribution was similar in all four groups with a total of 72.5% female patients and 27.5% male patients. No side preference among the four groups was seen (P=0.16–0.8). Table 1 shows mean patients' age, distribution of women/men and side distribution.
Table 1. Patient demographics.
| Nuclear (N) | Cortical (C) | Subcapsular posterior (S) | Mixed (M) | Total | |
|---|---|---|---|---|---|
| Number of eyes | 21 | 21 | 18 | 20 | 80 |
| Age (years)±s.d. | 75.8±6.6 | 72.3±6.8 | 70.0±10.3 | 74.4±7.4 | 73.5±7.8 |
| Sex (female/male) | 15/6 | 14/7 | 13/5 | 15/5 | 57/23 |
| Eye (right/left) | 8/13 | 9/12 | 6/12 | 11/9 | 34/46 |
Functional outcome
The best-corrected visual acuity (BCVA) was similar in patients with nuclear (N), cortical (C), and mixed cataract (M) (P=0.4–0.8) but significantly worse in patients with subcapsular posterior cataract (S) (P=0.009). Microperimetry shows a mean sensitivity of 11.4–12.6 dB without significant group differences. Table 2 shows LOCS grade of cataract, BCVA and mean retinal sensitivity of the four groups.
Table 2. Mean BCVA, mean LOCS grade, and mean macular sensitivity (dB) of the four groups and total.
| Nuclear (N) | Cortical (C) | Subcapsular posterior (S) | Mixed (M) | Total | |
|---|---|---|---|---|---|
| Mean BCVA (LogMar±s.d.) | 0.5±0.13 | 0.49±0.21 | 0.64±0.12* | 0.58±0.12 | 0.55±0.16 |
| Mean LOCS grade | 3.48±0.56 | 3.46±0.80 | 3.80±1.07 | 3.80±0.59 | 3.58±0.76 |
| Macular sensitivity (dB) Mean±s.d. | 12.19±3.18 | 12.75±2.05 | 11.8±3.7 | 11.9±3.9 | 12.0±3.0 |
*P<0.01 indicates statistically significant result.
Relationship between functional outcomes
The correlation of visual acuity to retinal sensitivity was high in patients with nuclear and cortical cataract: r=0.75 (N) and r=0.71 (C), respectively. No correlation could be found in patients with subcapsular posterior and mixed cataract (r=0.2 and r=0.14, respectively). Although patients with subcapsular cortical cataract had worse BCVA, macular sensitivity was not statistically significantly reduced in comparison with the other groups.
Stability of fixation is illustrated in Table 3. There were no statistically significant group differences. Instability of fixation is highly correlated with density of cataract in all groups (r=0.73) (P=0.02).
Table 3. Distribution of patients with stable, relatively unstable and unstable fixation.
| Nuclear (N) | Cortical (C) | Subcapsular posterior (S) | Mixed (M) | Total | |
|---|---|---|---|---|---|
| Stable | 9 | 10 | 8 | 9 | 36 |
| Relatively unstable | 7 | 6 | 5 | 7 | 25 |
| Unstable | 5 | 5 | 5 | 4 | 19 |
Pearson's correlation coefficients for comparison of density of cataract and macular sensitivity in all four groups are high (r=0.75), and statistically significant (P=0.015).
Discussion
The present study shows that the form and density of cataract highly influences macular sensitivity measure. Cataract patients of our study had a mean macular sensitivity of 12.0±3.0 dB. The comparison to normal age-matched individuals with 14.7–15.5 dB8, 11, 12 shows the distinct overall decrease of sensitivity in the absence of absolute scotoma (as our patients had a healthy macula). Previous studies have already discussed the influence of media opacities in SLO microperimetry.13, 14, 15 However, for MP1 our study is the first to show the considerable influence of different types of cataract. The grading of the lens had a mean LOCS grade of 3.5–3.8±0.6 in our patients. A double-masked quantification of cataract was not performed, and examiners were not blinded to microperimetry results. This might be a weakness of the present study, but the results show a high correlation of visual acuity to retinal sensitivity in patients with nuclear and cortical cataract. These data indicate well-performed LOCS grading. Additionally, a previous study of our study group12 showed a good interobserver reliability for the mean threshold values in young and old people, indicating examiner-independent measurements.
As the correlation between LOCS score and microperimetry results was high, a reduction of 1 dB per 1 PCO score increase can be estimated for these patients.
In our study, patients show a relatively poor stability of fixation. This was already reported by Rohrschneider et al,13 who also found a decrease of fixation stability with increasing age, even in normal subjects, evaluating SLO. The same was found by Weingessel et al.12 As our data show that instability of fixation highly correlated with the density of cataract in all groups, we suggest that for patients with dense cataract the fixation cross should be increased to 5° instead of 3° to maintain stable fixation.
Roesel et al16 and Kriechbaum et al17 found that functional parameters like central visual acuity and fundus-related microperimetry are significantly related to morphologic parameters (eg, retinal thickness). Also, Varga et al18 showed a good correlation of density of posterior capsule opacification (PCO) and PCO-induced decrease in BCVA and macular sensitivity.
This is in accordance to our study, where we found a high correlation of microperimetry results with the BCVA of patients with nuclear and cortical cataract, and high Pearson's correlation coefficients for comparison of density of cataract and macular sensitivity in all four groups.
These cataract data have to be taken into account when microperimetry is performed in the follow-up of patients with surgically treated macular pathology (eg, macular pucker and macular hole). Our study group19 previously showed that visual distance acuity alone underestimated the functional benefit of surgery. However, the development of nuclear cataract in these patients is common. This has to be considered if follow-up of surgical results is scheduled for several months.
Previous studies regarding contrast sensitivity, glare and reading ability showed a more severe alteration in patients with subcapsular posterior cataract than in patients with nuclear and cortical cataract.10, 20, 21 However, in our patients with subcapsular posterior cataract, microperimetry results were better than the results estimated by BCVA. This might be related to the inhomogenous opacities of subcapsular posterior cataract that often are very opaque centrally, but lighten up towards the mid-periphery.
In conclusion, our study shows that existence and specification of cataract highly influence central retinal sensitivity. Especially, in the evaluation of surgical macular results, these factors have to be kept in mind.
The authors declare no conflict of interest.
References
- Hammond CJ, Webster AR, Snieder H, Bird AC, Gilbert CE, Spector TD. Genetic influence on early age-related maculopathy: a twin study. Ophthalmology. 2002;109 (4:730–736. doi: 10.1016/s0161-6420(01)01049-1. [DOI] [PubMed] [Google Scholar]
- Kanski JJ.Clinical Ophthalmology: A Systemic ApproachVol 199, 4th edn.Butterworth-Heinemann, Elsevier Ltd: New York, 1999; 403–404. [Google Scholar]
- Klaver CC, Assink JJ, van Leeuwen R, Wolfs RC, Vingerling JR, Stijnen T, et al. Incidence and progression rates of age-related maculopathy: the Rotterdam Study. Invest Ophthalmol Vis Sci. 2001;42 (10:2237–2241. [PubMed] [Google Scholar]
- Lacour M, Kiilgaard JF, Nissen MH. Age-related macular degeneration: epidemiology and optimal treatment. Drugs Aging. 2002;19 (2:101–133. doi: 10.2165/00002512-200219020-00003. [DOI] [PubMed] [Google Scholar]
- Krischer CC, Stein-Arsic M, Meissen R, Zihl J. Visual performance and reading capacity of partially sighted persons in a rehabilitation center. Am J Optom Physiol Opt. 1985;62 (1:52–58. doi: 10.1097/00006324-198501000-00007. [DOI] [PubMed] [Google Scholar]
- Legge GE, Ross JA, Isenberg LM, LaMay JM. Psychophysics of reading. Clinical predictors of low-vision reading speed. Invest Ophthalmol Vis Sci. 1992;33 (3:677–687. [PubMed] [Google Scholar]
- McClure ME, Hart PM, Jackson AJ, Stevenson MR, Chakrayarthy U. Macular degeneration: do conventional measurements of impaired visual function equate with visual disability. Br J Ophthalmol. 2000;84 (3:244–250. doi: 10.1136/bjo.84.3.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer C, Bültmann S, Völcker HE, Rohrschneider K. Fundus perimetry with the Micro Perimeter 1 in normal individuals. Ophthalmology. 2005;112:848–854. doi: 10.1016/j.ophtha.2004.11.051. [DOI] [PubMed] [Google Scholar]
- Rohrschneider K, Springer C, Bültmann S, Völcker HE. Microperimetry-comparison between the Micro Perimeter 1 and Scanning Laser Ophthalmoscope-fundus perimetry. Am J Ophthalmol. 2005;139:125–134. doi: 10.1016/j.ajo.2004.08.060. [DOI] [PubMed] [Google Scholar]
- Stifter E, Sacu S, Weghaupt H, König F, Richter-Müksch S, Thaler A, et al. Reading performance depending on the type of cataract and its preditability on the visual outcome. J Cataract Refract Surg. 2004;30 (6:1259–1267. doi: 10.1016/j.jcrs.2003.11.051. [DOI] [PubMed] [Google Scholar]
- Chylack LT, Jr, Wolf JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, et al. The lens opacities classification system III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol. 1993;111:831–836. doi: 10.1001/archopht.1993.01090060119035. [DOI] [PubMed] [Google Scholar]
- Weingessel B, Sacu S, Vécsei-Marlovits PV, Weingessel A, Richter-Mueksch S, Schmidt-Erfurth U. Interexaminer and intraexaminer reliability of the microperimeter MP-1. Eye. 2009;23 (5:1052–1058. doi: 10.1038/eye.2008.237. [DOI] [PubMed] [Google Scholar]
- Rohrschneider K, Becker M, Schumacher N, Fendrich T, Volcker HE. Normal values for fundus perimetry with the scanning laser ophthalmoscope. Am J Ophthalmol. 1998;126 (1:52–58. doi: 10.1016/s0002-9394(98)00065-8. [DOI] [PubMed] [Google Scholar]
- Johnson CA, Adams AJ, Lewis RA. Evidence for a neural basis of age-related visual field loss in normal observers. Invest Ophthalmol Vis Sci. 1989;30 (9:2056–2064. [PubMed] [Google Scholar]
- Lachenmayr BJ, Kojetinsky S, Ostermaier N, Angstwurm K, Vivell PM, Schaumberger M. The different effects of aging on normal sensitivity in flicker and light-sense perimetry. Invest Ophthalmol Vis Sci. 1994;35:2741–2748. [PubMed] [Google Scholar]
- Roesel M, Heimes B, Heinz C, Henschel A, Spital G, Heiligenhaus A.Comparison of retinal thickness and fundus-related microperimetry with visual acuity in uveitic macular oedema Acta Ophthalmol 2009. e-pub ahead of print 9 December 2009; doi: 10.1111/j.1755-3768.2009.01750.x [DOI] [PubMed]
- Kriechbaum K, Prager F, Geitzenauer W, Benesch T, Schütze C, Simader C, et al. Association of retinal sensitivity and morphology during antiangiogenic treatment of retinal vein occlusion over one year. Ophthalmology. 2009;116 (12:2415–2421. doi: 10.1016/j.ophtha.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Varga A, Sacu S, Vécsei-Marlovits PV, Richter-Mueksch S, Neumayer T, Weingessel B, et al. Effect of posterior capsule opacification on macular sensitivity. J Cataract Refract Surg. 2008;34 (1:52–56. doi: 10.1016/j.jcrs.2007.08.024. [DOI] [PubMed] [Google Scholar]
- Richter-Mueksch S, Vécsei-Marlovits PV, Sacu SG, Kiss CG, Weingessel B, Schmidt-Erfurth U. Functional macular mapping in patients with vitreomacular pathologic features before and after surgery. Am J Ophthalmol. 2007;144 (1:23–31. doi: 10.1016/j.ajo.2007.03.045. [DOI] [PubMed] [Google Scholar]
- Rouhiainen P, Rouhiainen H, Salonen JT. Contrast sensitivity in different types of early lens opacities. Acta Ophthalmol Scand. 1996;74 (4:379–383. doi: 10.1111/j.1600-0420.1996.tb00713.x. [DOI] [PubMed] [Google Scholar]
- Elliott DB, Gilchrist J, Whitaker D. Contrast sensitivity and glare sensitivity changes with three types of cataract morphology: are these techniques necessary in a clinical evaluation of cataract. Ophthalmic Physiol Opt. 1989;9 (1:25–30. doi: 10.1111/j.1475-1313.1989.tb00800.x. [DOI] [PubMed] [Google Scholar]


