Abstract
Patients with glucocorticoid (GC) excess, Cushing's syndrome, develop a classic phenotype characterized by central obesity and insulin resistance. GCs are known to increase the release of fatty acids from adipose, by stimulating lipolysis, however, the impact of GCs on the processes that regulate lipid accumulation has not been explored. Intracellular levels of active GC are dependent upon the activity of 11β-Hydroxysteroid dehydrogenase type 1 (11β-HSD1) and we have hypothesized that 11β-HSD1 activity can regulate lipid homeostasis in human adipose tissue (Chub-S7 cell line and primary cultures of human subcutaneous (sc) and omental (om) adipocytes. Across adipocyte differentiation, lipogenesis increased whilst β-oxidation decreased. GC treatment decreased lipogenesis but did not alter rates of β-oxidation in Chub-S7 cells, whilst insulin increased lipogenesis in all adipocyte cell models. Low dose Dexamethasone pre-treatment (5 nM) of Chub-S7 cells augmented the ability of insulin to stimulate lipogenesis and there was no evidence of adipose tissue insulin resistance in primary sc cells. Both cortisol and cortisone decreased lipogenesis; selective 11β-HSD1 inhibition completely abolished cortisone-mediated repression of lipogenesis. GCs have potent actions upon lipid homeostasis and these effects are dependent upon interactions with insulin. These in vitro data suggest that manipulation of GC availability through selective 11β-HSD1 inhibition modifies lipid homeostasis in human adipocytes.
Introduction
The magnitude of the obesity epidemic has heightened the urgency to understand the mechanisms that contribute to the regulation of adipose tissue mass. The morbidities associated with obesity, especially central obesity, are well described and include dyslipidaemia, insulin resistance, type 2 diabetes (T2DM), hypertension and cardiovascular disease, all of which contribute to increased mortality [1].
The regulation of adipose tissue mass is complex. Increases in adipose tissue arise as a consequence of both hyperplasia (increase in fat cell number) and hypertrophy (increase in fat cell size) [2]. Hyperplasia relies on pre-adipocyte proliferation and differentiation into mature adipocytes. Adipocyte differentiation is a tightly regulated process orchestrated by the temporal expression of key transcription factors resulting in cyto-skeletal changes as well as the induction of key genes involved in lipid metabolism, namely lipogenesis, fatty acid uptake, lipolysis and β-oxidation. In mature adipocytes the relative balance of these processes is crucial in determining adipocyte size (and hence fat mass). Increased lipogenesis and fatty acid uptake favour lipid accumulation within the adipocyte, whilst lipolysis and β-oxidation promote lipid loss.
Lipogenesis occurs either as a consequence of re-esterification of free fatty acids (FFA) with glycerol or de novo synthesis of triacylglycerol (TAG). De novo lipogenesis may account for up to 20% of lipid turnover within adipose tissue [3]. During de novo lipogenesis, acetyl CoA is carboxylated to malonyl-CoA by acetyl CoA carboxylase (ACC) which is subsequently converted by a multi-step reaction to palmitate by fatty acid synthase (FAS) [4]. There are two isoforms of ACC (ACC1 and ACC2); in lipogenic tissues ACC1 predominates and is the key regulatory step of fatty acid synthesis. ACC2 is localized to the mitochondrial membrane, and its role is to limit β-oxidation through malonyl-CoA mediated inhibition of carnitine palmitoyl transferase I (CPT I) which catalyses the transfer of long-chain fatty acyl-CoA into the mitochondrion. ACC1 and 2 are highly regulated at the level of mRNA expression, protein phosphorylation and also by ubiquitination and proteasomal degradation. Phosphorylation by AMP-kinase (AMPK) at ser-79 on ACC1 and ser-218 on ACC2, negatively regulates activity [5].
Patients with glucocorticoid (GC) excess, Cushing's syndrome, develop a classical phenotype characterized by insulin resistance, proximal myopathy and central obesity. Whilst it is clear that GCs are essential for adipocyte differentiation [6], their impact upon many of the processes that regulate lipid accumulation within the adipocyte have not been explored in detail. In vivo and in vitro, GCs appear to stimulate lipolysis through a putative action upon hormone sensitive lipase [7], [8] and the resultant generation of FFA may contribute to the development of insulin resistance [9]. This is consistent with their role as ‘stress’ hormones, mobilizing FFA for β-oxidation, but a potential impact upon ACC activity and lipogenesis and β-oxidation has not been investigated. This may be important in explaining the clinical impact of endogenous and exogenous GC excess.
There has been much interest in the role of endogenous GC secretion and metabolism in the pathogenesis of human obesity. GC availability and action depend not only upon circulating levels but also on tissue specific intracellular activation or inactivation by 11β-hydroxysteroid dehydrogenases (11β-HSD). 11β-HSD1 is highly expressed in adipose tissue and predominantly converts inactive cortisone to cortisol, thus amplifying local GC action independent of circulating cortisol concentrations [10]. Within subcutaneous (sc) adipose tissue, there is increased 11β-HSD1 expression and activity that positively correlates with obesity and insulin resistance [11], [12]. Furthermore, studies employing 11β-HSD1 inhibitors have demonstrated clinical efficacy in improving insulin sensitivity in patients with type 2 diabetes [13].
Based upon the hypothesis that GC-mediated changes in lipid homeostasis in adipose tissue are a crucial driver to the Cushing's phenotype, we have performed a detailed characterization of the impact of GC on lipid flux in human adipose tissue. Furthermore we have proposed that the action of selective 11β-HSD1 inhibitors to improve insulin sensitivity may be in part medicated by suppression of lipid mobilization from adipose tissue decreasing FFA availability.
Methods
Cell Culture
Chub-S7 cell culture
The Chub-S7 cell line is a transformed human subcutaneous pre-adipocyte cell line derived from an obese female that has been validated as a good model of human adipocyte biology [14], [15]. Proliferating cells were cultured in Dulbecco's MEM/Nutrient Mixture F12, DMEM-F12 (Sigma, Poole, UK) with 10% foetal calf serum. At confluence, cells were differentiated for 14 days into mature adipocytes in chemically defined media (DMEM-F12 media with Biotin 33 µM, Pantothenate 17 µM, T3 0.2 nM, Insulin 167 nM, Cortisol 1 µM and Rosiglitazone 1 µM).
Primary subcutaneous and omental pre-adipocyte cell culture
Paired primary human subcutaneous and omental pre-adipocytes were obtained from ZenBio (Durham, US) and were isolated from adipose tissue of healthy, non-diabetic donors aged 18–60 years undergoing elective surgery. Pre-adipocytes were cultured to confluence as per the manufacturer's guidelines using the supplied media. Once confluent, media were changed to a chemically defined media (ZenBio) and were differentiated into adipocytes for 14 d.
RNA extraction and Reverse Transcription
Total RNA was extracted from cells using the Tri-Reagent system. RNA integrity was assessed by electrophoresis on 1% agarose gel. Concentration was determined spectrophotometrically at OD260. In a 50 µl volume 500 ng of total RNA was incubated with 250 µM random hexamers, 500 µM dNTPs, 20 U RNase inhibitor, 63 U Multiscribe reverse transcriptase, 5.5 mM MgCl and 1× reaction buffer (Applied Biosystems, Foster City, CA, USA). The reverse transcription reaction was carried out at 25°C for 10 min, 48°C for 30 min and then the reaction was terminated by heating to 95°C for 5 min.
Real-Time PCR
mRNA levels were determined using an ABI 7500 sequence detection system (Perkin-Elmer Applied Biosystems, Warrington, UK). Reactions were performed in 10 µl volumes on 96-well plates in reaction buffer containing 2× TaqMan Universal PCR Master mix (Applied Biosystems). All primers and probes were supplied by applied biosystems ‘assay on demand’ and reactions normalised against the house keeping gene 18S rRNA, provided as a preoptimized control probe. All target genes were labelled with FAM and the housekeeping gene with VIC. The reaction conditions were as follows: 95°C for 10-minutes, then 40 cycles of 95°C for 15-seconds and 60°C for 1 min.
Data were obtained as ct values (ct = cycle number at which logarithmic PCR plots cross a calculated threshold line) and used to determine Δct values (Δct = (ct of the target gene)−(ct of the housekeeping gene). Data were expressed as arbitrary units using the following transformation [expression = 1000*(2−Δct) arbitrary units (AU)].
Protein extraction and Immunoblotting
Total protein was extracted from cells using RIPA buffer (50 mM Tris pH 7.4, 1% NP40, 0.25% sodium deoxycholate, 150 mM NaCl, 1 mM EDTA, 1 mM PMSF and protease inhibitor cocktail (Roche, Lewes, UK) dissolved in 10 mL of distilled water) and freeze thawing. Protein concentrations were measured using a commercially available assay (Bio-Rad Laboratories Inc., Hercules, CA). 15 µg of protein was resolved on a 12.5% SDS PAGE gel and transferred onto nitrocellulose membrane, Hybond ECL (GE Healthcare, Chalfont St Giles, UK). Primary (anti-AMPK, pAMPK(Thr172), ACC1/2 and pACC(ser79/218), (Cell Signalling Technology, Danvers, MA) and secondary antibodies (Dako, Glostrop, UK) were used at a dilution of 1/1000. Membranes were re-probed for β-Actin. Primary and secondary antibodies were used at a dilution of 1/5000 (Abcam plc, Cambridge, UK). Bands were quantified with Genesnap by Syngene (Cambridge, UK) and expressed relative to β-actin to normalise for gel loading.
Lipogenesis
Lipogenesis was measured by the uptake of 1-[14C]-acetate into the lipid component as described previously [16]. At confluence or after 14 days of differentiation Chub-S7 cells, or primary sc and om cells were washed and cultured for 4 h in serum free media. Cells were then incubated in 500 µl of serum free media with or without insulin (5 nM), glucorticoids (5 or 500 nM) and the selective 11β-HSD1 inhibitor (PF-877423, 5 µM, provided through a material transfer agreement with Pfizer inc. (La Jolla, CA, USA) [17]) for 18 h, 0.12 µCi/L 1-[14C]-acetic acid with cold sodium acetate [10 µM] was added to the treatments for a further 6 h. After incubation cells were washed and scraped into 250 µl of PBS. The lipid fraction was recovered in Folch solvent, the solvent was evaporated and the radioactivity retained in the cellular lipid was determined by scintillation counting and expressed as disintegrations per minute (dpm)/per well.
β-oxidation
Rates of β-oxidation were measured by the conversion of [3H]-palmitate to [3H]-H2O. At confluence or after 14 days of differentiation, Chub-S7 cells were washed and cultured in serum free media for 4 h. Cells were then incubated with 300 ul of low glucose serum free media with 0.12 µCi/L [3H]-palmitic acid with cold palmitate to a final concentration of 10 µM palmitate and treated with or without insulin (5 nM) or Dex (5 or 500 nM) for 24 h. After incubation medium was recovered and precipitated with an equal volume of 10% tricholoroacetic acid. The aqueous component of the supernatants was extracted with 2∶1 choloform methanol solution. Radioactivity was determined by scintillation counting and expressed as disintegrations per minute (dpm)/per well.
Fatty acid uptake
Fatty acid uptake was measured by intracellular accumulation of [3H]-palmitate. At confluence or after 14 days of differentiation, Chub-S7 cells were washed and cultured in serum free media for 4 h. Cells were then incubated with 300 ul of low glucose serum free media with 0.12 µCi/L [3H]-palmitic acid with cold palmitate to a final concentration of 10 µM palmitate and treated with or without Dex (5 or 500 nM) for 24 h. The cells were incubated at 37°C for 24 h. After incubation cell lysate was recovered and radioactivity was determined by scintillation counting and expressed as disintegrations per minute (dpm)/per well.
Statistical analysis
Data are presented as mean ± standard error. Where data were normally distributed, t-tests (paired or unpaired where appropriate) were used to compare single treatments to control. If normality tests failed, non-parametric tests were used. ANOVA was used to compare multiple doses and/or treatments. (SigmaStat 3.1, Systat Software, Inc. Point Richmond, CA). Statistical analysis on real-time PCR data was performed on mean Δct values and not fold changes.
Results
Lipid metabolism across human adipocyte differentiation
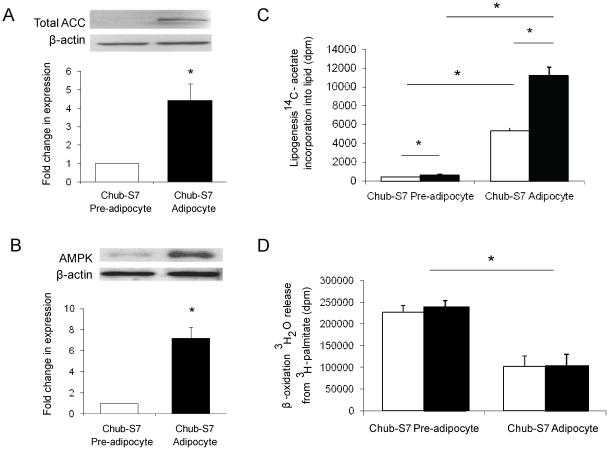
Across differentiation, mRNA expression levels of genes involved in lipid metabolism increased significantly in Chub-S7 cells (FAS 13.6-fold p<0.01; ACC1 2.2-fold p<0.05; ACC2 4.5-fold p<0.005). This was comparable to human cultures of primary sc pre-adipocytes (FAS 3.6-fold p<0.05, ACC2 24.1-fold p<0.05) although in primary sc cultures, ACC1 expression did not increase significantly across adipocyte differentiation (table 1). mRNA expression of AMPKα1 or AMPKα2 did not change across differentiation in Chub-S7 or sc pre-adipocytes. Endorsing our findings at the mRNA level, ACC1/2 protein expression increased in Chub-S7 cells (data expressed relative to undifferentiated cells, 1.0 vs. 4.3±1.8, p<0.05) (figure 1a). Although AMPK mRNA expression did not change, protein levels increased (1.0 vs. 7.2±1.8, p<0.001) (figure 1b).
Table 1. mRNA expression levels in primary cultures of undifferentiated (day 1) and differentiated (day 14) pre-adipocytes from Chub-S7 cells and subcutaneous pre-adipocytes tissue as measured by real-time PCR.
| Chub-S7 cells | Subcutaneous Pre-adipocytes | |||||
| Gene | Pre-adipocytes (day 1) | Differentiated (day 14) | p | Pre-adipocytes (day 1) | Differentiated (day 14) | p |
| FABP4 | 0.01±0.003 | 75.5.±6.79 | <0.005 | 1.46±0.41 | 37.57±11.86 | <0.005 |
| FAS | 0.57±0.05 | 7.15±0.9 | <0.01 | 1.23±0.23 | 6.54±1.39 | <0.005 |
| ACC1 | 0.35±0.04 | 0.79±0.05 | <0.05 | 0.28±0.03 | 0.54±0.09 | ns |
| ACC2 | 0.05±0.01 | 2.03±0.14 | <0.005 | 0.07±0.04 | 2.88±0.74 | <0.005 |
| AMPKα1 | 0.63±0.07 | 0.41±0.02 | ns | 0.88±0.53 | 0.70±0.24 | ns |
| AMPKα2 | 0.07±0.01 | 0.04±0.004 | ns | 0.05±0.02 | 0.09±0.05 | ns |
| COP1 | 0.56±0.04 | 0.48±0.04 | ns | 0.48±0.12 | 0.28±0.08 | ns |
| TRB3 | 0.41±0.13 | 0.13±0.01 | ns | 0.94±0.26 | 0.16±0.01 | <0.05 |
Data are presented as arbitrary units (mean±se, n = 3–6 experiments).
Figure 1. Across Chub-S7 differentiation, total ACC (a) and AMPK (b) levels increase.
Data are presented as the mean±se fold change compared to undifferentiated cells and quantified relative to β-actin with representative western blots above (n = 3–5 experiments, * p<0.05). 1-[14C]-acetate incorporation into lipid increased across differentiation and was stimulated by insulin in both undifferentiated pre-adipocytes and differentiated adipocytes (c). In contrast, 3H release from 3H-palmitate decreased across differentiation and was not regulated by insulin. Data are expressed as disintegrations per minute (dpm) and are the mean±se of n≥3 experiments performed in triplicate. Basal (open bars) and insulin stimulated (black bars) and *p<0.05.
Consistent with an increase in the expression of genes involved in lipid metabolism 1-[14C]-acetate incorporation into lipid was higher in differentiated Chub-S7 adipocytes compared to undifferentiated cells (412±44 vs. 5351±304 dpm/well, p<0.05) (figure 1c). Furthermore, insulin-stimulated 1-[14C]-acetate incorporation into lipid in both undifferentiated and differentiated cells (undifferentiated: 412±44 vs. 662±93 dpm/well, p<0.05; differentiated: 5351±304 vs. 11250±880 dpm/well, p<0.05) (figure 1c). In contrast, [3H]-palmitate breakdown into water, reflecting β-oxidation, decreased across differentiation (227058±15548 vs. 101687±24079 dpm/well, p<0.05). Insulin treatment did not impact β-oxidation in either differentiated or undifferentiated cells (undifferentiated: 227058±15548 vs. 238677±16261 dpm/well, p = ns; differentiated: 101687±24079 vs. 100251±29916 dpm/well, p = ns) (figure 1d).
Glucocorticoid and insulin regulation of lipid metabolism in human adipocytes
Lipogenesis
In Chub-S7 cells high (500 nM, 24 h), but not low (5 nM, 24 h) dose Dex, decreased ACC1 mRNA expression, but increased expression of FAS and ACC2 (table 2a and b). Although it did not reach significance Dex increased expression of FAS and ACC2 in sc, but not om cells (FAS sc: 4.87±2.04 (control): 10.27±1.04 (5 nM, 24 h), 10.35±0.97 (500 nM, 24 h) p = ns) (ACC2 sc: 0.67±0.14 (control): 1.92±0.26, p = ns (5 nM, 24 h), 1.92±0.06, p = ns (500 nM, 24 h)).
Table 2. mRNA expression measured by real-time PCR of genes involved in adipocyte lipid homeostasis in differentiated Chub-S7 cells following treatment with Dexamethasone (Dex) alone (a) or in combination with insulin (b) for 24 h.
| a | No insulin | b | Insulin (5 nM) | ||||
| No Dex | Dex (5 nM) | Dex (500 nM) | No Dex | Dex (5 nM) | Dex (500 nM) | ||
| SDC1 | 362.8±37.3 | 388.9±34.7 | 344.9±13.1 | SDC1 | 286.5±28.4 | 233.3±29.5§ | 224.7±30.6 |
| ACC1 | 2.5±0.5 | 2.4±0.4 | 1.7±0.8* | ACC1 | 1.3±0.4§ | 1.3±0.2‡∥ | 0.9±0.5*§ |
| FAS | 25.6±4.5 | 33.3±9.2* | 47.4±7.1* | FAS | 15.6±4.6 | 29.5±6.4 | 39.6±10.3* |
| DGAT1 | 2.4±0.37 | 2.7±0.4 | 2.5±0.3 | DGAT1 | 1.5±0.4 | 1.9±0.4 | 1.8±0.3 |
| GPAT | 0.69±0.14 | 0.75±0.15 | 0.57±0.13 | GPAT | 0.42±0.10 | 0.50±0.13§ | 0.49±0.13 |
| COP-1 | 1.3±0.4 | 1.5±0.5 | 1.6±0.5 | COP-1 | 1.2±0.3 | 1.2±0.4 | 1.2±0.3 |
| MCD | 0.69±0.15 | 0.87±0.18 | 0.90±0.17 | MCD | 0.56±0.20 | 0.56±0.18 | 0.76±0.23 |
| CPT-1 | 0.70±0.29 | 0.81±0.30 | 0.68±0.30 | CPT-1 | 0.79±0.29 | 0.78±0.27 | 0.83±0.25 |
| ACC2 | 2.8±0.7 | 4.3±0.9* | 7.2±2.2‡ | ACC2 | 3.3±0.9 | 5.3±1.1* | 6.0±1.3† |
| FAT | 81.4±12.4 | 87.1±8.1 | 83.9±11.5 | FAT | 63.6±14.2 | 65.0±11.4§ | 60.5±12.8 |
| FABP4 | 133.1±16.0 | 165.2±13.1* | 178.0±16.8* | FABP4 | 89.2±13.6§ | 123.7±15.3‡§ | 120.1±16.6†§ |
| ACS | 3.3±1.1 | 3.5±1.0 | 2.0±0.5 | ACS | 1.3±0.5 | 1.2±0.5§ | 0.81±0.26‡§ |
| AMPKα1 | 0.96±0.07 | 1.1±0.3 | 1.5±0.2 | AMPKα1 | 1.3±0.1 | 1.2±0.2 | 1.4±0.2 |
| PDK4 | 2.5±0.6 | 4.3±1.2 | 9.1±2.5‡ | PDK4 | 3.2±0.4 | 6.0±1.1 | 10.9±2.0‡ |
Data are presented as arbitrary units±standard error and are the mean of n = 5–7 experiments (* p<0.05, † p<0.01, ‡ p<0.005 vs. no Dex; § p<0.05, ∥ p<0.005 vs. no insulin at same concentration of Dex).
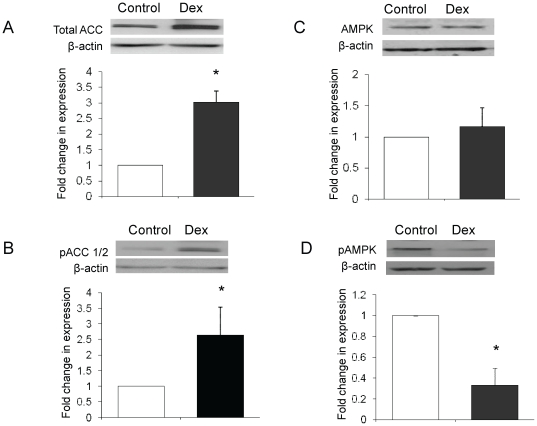
Whilst Dex (500 nM, 24 h) treatment increased total ACC protein levels (3.0±0.4-fold, p<0.05) in Chub-S7 cells, inactivating ser-79/218 phosphorylation of ACC also increased (2.6±0.9-fold, p<0.05) (figure 2a and b and figure 3b). AMPK protein expression did not change, however phosphorylation of AMPK at thr172 decreased following Dex treatment (figure 2c and d).
Figure 2. Dexamethasone (Dex, 500 nM, 24 h) increases both total ACC levels (a) and ser-79/218 phosphorylation of ACC (b) in differentiated Chub-S7 cells.
Total AMPK levels are not changed (c), but Thr172 phosphorylation is decreased (d). Data are presented as the mean±se fold change compared to untreated cells and quantified relative to β-actin with representative western blots above (n = 3–5 experiments, control open bars, Dex black bars, * p<0.05).
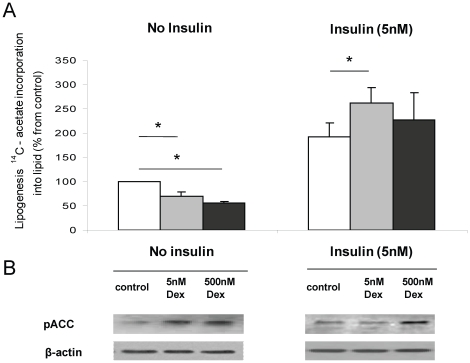
Figure 3. In the absence of insulin, dexamethasone (Dex) decreases lipogenesis as measured by 1-[14C]-acetate incorporation into lipid in differentiated Chub-S7 cells in a dose dependent manner (a) and is associated with increasing ser79/218 phosphorylation of ACC (b).
Insulin stimulates lipogenesis and the actions of insulin are augmented in the presence of low dose (5 nM), but not high dose (500 nM) Dex (a), where Dex is only able to increase phosphorylation at the higher dose. Control cells are shown in the white bars, low dose dexamethasone treatment (5 nM) grey bars, high dose (500 nM) black bars, * p<0.05) representative western blot is shown.
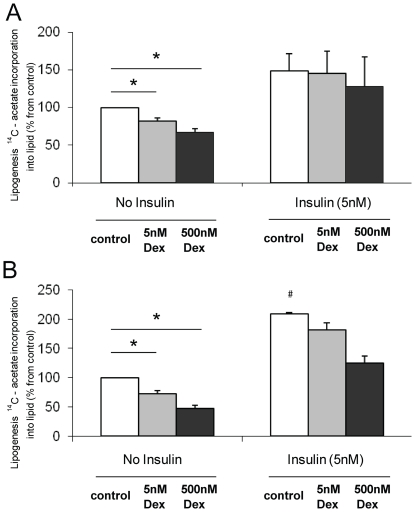
Consistent with increased ser-79/218 phosphorylation of ACC, Dex caused a dose dependent decrease in lipogenesis (100% (control): 70.0±8.2, p<0.005 (5 nM, 24 h), 56.0±3.9%, p<0.01 (500 nM, 24 h)), in Chub-S7 cells (figure 3a and b). These findings were endorsed in primary cultures of differentiated sc and om pre-adipocytes. In cells from both depots, Dex decreased lipogenesis (sc: 81.9±3.9, p<0.005 (5 nM), 67.3±4.8%, p<0.001 (500 nM); om: 72.0±5.4, p<0.005 (5 nM), 46.9±5.7%, p<0.01 (500 nM)) (Figure 4).
Figure 4. In primary cultures of differentiated subcutaneous (a) and omental (b) pre-adipocytes, Dex decreases lipogenesis in the absence of insulin.
Insulin stimulates lipogenesis in both subcutaneous and omental cells (a and b). In omental cells only, Dex impairs the ability of insulin to stimulate lipogenesis (b). (Activity data are expressed relative to untreated cells (no insulin, no Dex) and are the mean±se of n = 3–5 experiments. Control cells are shown in the white bars, low dose dexamethasone treatment (5 nM) grey bars, high dose (500 nM) black bars, * p<0.05 vs. Ctrl and § p<0.05 om, 5 nM insulin vs. sc, 5 nM insulin).
Insulin Stimulated lipogenesis
In Chub-S7 cells low dose Dex (5 nM, 24 h) significantly enhanced the response to insulin (no insulin, no Dex (100%), 192.5±25.3 (5 nM insulin) vs. 248.3±31.4%, (5 nM Dex+5 nM insulin), p<0.05) (figure 3a). Similarly in sc cells, in the presence of insulin (5 nM, 24 h), Dex no longer inhibited lipogenesis and did not impair insulin-stimulated lipogenesis (no insulin, no Dex (100%), 149.0±22.1% (5 nM insulin), 145.5±29.4% (5 nM Dex+5 nM insulin) p = ns) (figure 4a). In contrast, Dex (5 nM and 500 nM, 24 h) decreased lipogenesis in om cells in the presence of insulin, reflecting either a persistence of the direct action of Dex, or its ability to induce insulin resistance and limit insulin-stimulated lipogenesis (no insulin, no Dex (100%), 208.9±1.9 (5 nM insulin), 181.5±11.8%, (5 nM Dex+5 nM insulin) p<0.001) (Figure 4b). In Chub-S7 cells Dex, in the presence of insulin high dose (500 nM, 24 h), but not low (5 nM, 24 h) dose Dex, decreased ACC1 mRNA expression, but increased expression of FAS and ACC2, complete data are presented in table 2a and b. In the primary cells Dex in the presence of insulin increased expression of FAS in sc, but not om, cells although this did not reach significance (FAS sc: 3.84±0.74 (5 nM insulin): 8.81±0.28 (5 nM Dex+5 nM insulin, 24 h), 7.82±0.65 (500 nM Dex+5 nM insulin, 24 h) p = ns). ACC2 expression increased in both sc and om cells (sc: 0.78±0.07 (5 nM insulin): 2.35±0.43, p = ns (5 nM Dex+5 nM insulin, 24 h), 2.45±0.04, p = ns (500 nM Dex+5 nM insulin, 24 h)), (om: 0.08±0.04 (5 nM Dex+5 nM insulin, 24 h): 0.15±0.04, p = ns (5 nM, 24 h), 0.13±0.03, p = ns (500 nM Dex+5 nM insulin, 24 h)) but did not reach significance.
11β-HSD1 as a regulator of lipogenesis in human adipose tissue
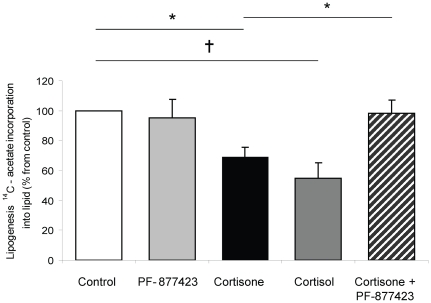
We have previously demonstrated the expression of 11β-HSD1 in Chub-S7 cells and characterized its regulation across adipocytes differentiation [17]. 24 h incubation with both cortisol and cortisone decreased basal lipogenesis to a similar extent (100% (control); 65.7±6.2 (cortisone, 500 nM) p<0.001, 50.8±10.9% (cortisol, 500 nM) p<0.005). Incubation with the selective 11β-HSD1 inhibitor (PF-877423, 5 µM) (17) alone was without effect. However, when co-incubated with cortisone (that requires intact 11β-HSD1 activity to generate active cortisol), cortisone-induced repression of lipogenesis was completely abolished (100% (control); 65.7±6.2% (cortisone, 500 nM), 96.4±9.1 (cortisone 500 nM+ PF-877423 5 µM) p<0.01) (figure 5).
Figure 5. Cortisone (500 nM, 24 h, black) and cortisol (500 nM, 24 h, dark grey) decrease lipogenesis in differentiated Chub-S7 cells.
The effects of cortisone are blocked by the 11β-hydroxysteroid dehydrogenase inhibitor, PF877423 (5 µM, 24 h, hashed bar). (Data are expressed relative to untreated cells (white bars) and are the mean±se of n = 3–5 experiments, * p<0.05 and † p<0.01).
β-oxidation
24 h Dex treatment increased ACC2 and PDK4 mRNA expression (ACC2: 2.8±0.7 (control) 4.3±0.9 (5 nM Dex) p<0.05, 7.2±2.2 (500 nM Dex) p<0.01; PDK4: 2.5±0.6 (control) 4.3±1.2 (5 nM Dex) p = ns, 9.1±2.5 (500 nM Dex) p<0.005) (Table 1a). Dex and insulin treatment, both alone and in combination did not alter β-oxidation, as measured by the conversion of [3H]-palmitate to [3H]-H2O, in differentiated Chub-S7 cells. (100% (control); 102.3±0.6% (5 nM Dex), 104.8±5.5% (500 nM Dex), 105.8±2.2 (5 nM insulin), 102.6±2.6% (5 nM Dex+5 nM insulin), 103.7±2.1% (500 nM Dex+5 nM insulin)
Fatty acid uptake
In differentiated Chub-S7 cells both low (5 nM, 24 h) and high (500 nM, 24 h) dose Dex increased FABP4 expression (table 1a) and in the absence of insulin increased [3H]-palmitate uptake (100% (control); 118.2±5.1% (5 nM Dex), 127.4±6.1% (500 nM Dex) p<0.05).
Depot Specific Differences
Sc pre-adipocytes differentiated to a greater degree than om pre-adipocytes, with higher mRNA expression of lipid metabolism genes (ACC1 3.2-fold, FAS 10.9-fold, ACC2 17.8-fold, LPL 44.7-fold) and higher 1-[14C]-acetate incorporation into lipid compared to om cells (3.8-fold, 564±117 vs. 2154±222 dpm/well, p<0.005). However, lipogenesis in om cells was more responsive to insulin stimulation (100% (control): sc 149±22.14%, om 209±1.86%, p = 0.05) (Figure 4a and b).
Discussion
The actions of GCs upon adipose tissue are complex, but they are essential for adipocyte differentiation [6]. In this paper, we have performed a detailed characterization of lipid homeostasis in the human pre-adipocyte cell line Chub-S7. Across differentiation, total ACC protein levels increased, although, we were unable to distinguish ACC1 and 2 (due to lack of suitable antibodies) the net effect would be to promote lipid accumulation. Increased ACC1 drives lipogenesis, whilst increased ACC2 will limit β-oxidation and it is this pattern of dynamic lipid flux that we observed across adipocyte differentiation. Consistent with published data [18], insulin was able to stimulate lipogenesis in both undifferentiated and differentiated cells as well as in primary sc and om cultures but failed to regulate β-oxidation. Whilst for the most part the data from the Chub-S7 cell line matched very well with data from primary cultures, it is possible that the transformations used to generate the Chub-S7 cell line could potentially have modified their behaviour and characteristics.
In mature adipocytes, GCs stimulate FFA uptake, via lipoprotein lipase activity, as well as driving lipolysis though hormone sensitive lipase [8], [19] and AGTL [20]. In addition, we have previously shown that limiting GC exposure to adipose tissue in vivo decreases lipolysis [21]. Dietary TAG is the main source of lipid stored within adipocytes, however, over feeding studies in humans suggest 40% of increases in fat mass are due to de novo lipogenesis [22]. In rodent models, GCs inhibit insulin-stimulated de novo lipogenesis by decreasing FAS and ACC activity [23], [24]. In the only human study published to date, GC action in isolation was not examined. GCs and insulin, (when compared to insulin alone), increased FAS activity and lipogenesis in sc adipocytes, as measured by glucose incorporation into cellular lipids [25]. In our study, GCs increased ACC2 (but not ACC1) and FAS mRNA expression as well as total ACC protein levels (which may reflect ACC2) but decreased functional lipogenesis in all adipocyte cell models.
Global deletion of ACC1 in rodents results in embryonic lethality [26], but targeted liver-specific deletion, decreases lipogenesis and lipid accumulation without alteration in β-oxidation or glucose homeostasis [27]. In contrast, ACC2 knockout mice have unaltered adipocyte malonyl CoA levels [28] suggesting that it is not involved in lipogenesis. The changes that we have observed in 1-[14C]-acetate incorporation into lipid are therefore most likely to reflect regulation of specific ACC1 activity. ACC 1 and 2 are negatively regulated by phosphorylation at Ser-79 and 218 respectively by AMPK [5]. We observed an increase in serine phosphorylation of ACC following GC treatment and this translated to a net decrease in lipogenesis. However, in contrast to observations in hepatocytes where GCs increase AMPK expression [29] this was unchanged in Chub-S7 cells, sc and om human primary cultures (data not shown). Furthermore, activating phosphorylation of AMPK at Thr172 was decreased by GC treatment suggesting that regulation of ACC1 through serine phosphorylation is likely to be independent of AMPK in human adipose tissue. Our data are in agreement with studies on adipocytes differentiated from mesenchymal stem cells where Dex did not alter gene or protein expression, but decreased AMPK activity [30] and with obervations in adipose tissue fom patients with Cushing's syndrome, where AMPK phosporylation is decreased [31].
In Chub-S7 cells, Dex augmented insulin-stimulated lipogenesis and this is in agreement with our previous studies [14] as well as others [32] that have shown enhanced activation of the insulin signalling cascade and glucose uptake following pre-treatment of adipocytes with GC. In sc and om cells in this study, the incremental response to insulin stimulation was similar with and without low dose Dex and suggests that this dose (5 nM) is not sufficient to cause insulin resistance. At the highest dose (500 nM) in om, but not sc cells, Dex in combination with insulin decreased lipogenesis. Although these changes were not matched by the expected pattern of changes in mRNA expression, it is possible that this may reflect the complex post-translational regulation of lipogenesis and it is entirely plausible that there may exist a depot-specificity of regulation. In addition, extrapolating these observations to the in vivo situation is complex and represents a balance of ‘direct’ GC actions to decrease lipogenesis as well as any potential action to cause insulin resistance and abrogate the effect of insulin treatment.
These observations do raise the intriguing possibility of differential nutritional regulation of lipogenesis. In the fasting state, low insulin levels and high endogenous GC levels will stimulate lipolysis and simultaneously switch off lipogenesis though serine phosphorylation of ACC1, decreasing fuel storage and increasing FFA availability for other more metabolically active tissues. Conversely, in the fed state, insulin levels are high, and here insulin and GC may act together to promote lipid storage. However, we must exert a note of caution as extrapolating from in vitro models to in vivo observations is fraught with difficulty and these hypotheses will need to be tested in dedicated, well designed clinical studies.
Whilst obesity per se is detrimental to health, regional distribution of adipose tissue is crucially important. Intra-abdominal, as opposed to sc adipose deposition, correlates with insulin resistance [33] and increased cardiovascular morbidity and mortality [34]. The molecular mechanisms that underpin depot specific differences in fat accumulation are therefore of great interest. This study used differentiated pre-adipocytes from paired sc and om depots and as sc cell in culture differentiate to a greater degree comparisons of hormone responsiveness between cell types is difficult. Differences in insulin action between adipose tissue depots have been described [35]–[38]. Interestingly, despite a lower level of differentiation, lipogenesis in om cells responded more dramatically to insulin treatment, however, a dedicated study in a more suitable model is required.
GC availability and action not only depend upon circulating levels, but also on the tissue specific intracellular activation or inactivation by 11β-HSD. In vitro, rodent and clinical data have endorsed 11β-HSD1 as a metabolic therapeutic target [39]– and inhibitor studies including phase II studies in man are now published [13]. Improvements in lipid profiles as well as insulin sensitivity have been demonstrated for a number of compounds, but the precise mechanisms by which they convey their metabolic benefit remains to be confirmed. In skeletal muscle, selective 11β-HSD1 inhibitors alter lipid metabolism decreasing FFA availability [42] and this may underpin their ability to cause insulin sensitization through a putative impact to limit protein kinase C activation [43]. In adipose tissue we have previously demonstrated that 11β-HSD1 inhibition decreases lipolysis [21] and have now shown that these compounds can enhance lipogenesis. Taken together, these observations suggest that decreased lipid mobilization may represent a potential mechanism by which these compounds improve metabolic phenotype.
In conclusion, we have demonstrated that GCs have potent actions upon lipid homeostasis and also interact with insulin in human adipocyte cell lines and primary cultures. Manipulation of GC availability through selective 11β-HSD1 inhibition has therapeutic potential by altering lipid homeostasis in key metabolic target tissues and this may underpin their putative action as insulin sensitizers.
Acknowledgments
We would like to thank Dr C Darimont (Nestle, Switzerland) for providing the Chub-S7 cells.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by a Medical Research Council senior clinical fellowship (JWT), Wellcome Trust programme grant 066357 (PMS). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript
References
- 1.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW., Jr Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 2.Hausman DB, DiGirolamo M, Bartness TJ, Hausman GJ, Martin RJ. The biology of white adipocyte proliferation. Obes Rev. 2001;2:239–254. doi: 10.1046/j.1467-789x.2001.00042.x. [DOI] [PubMed] [Google Scholar]
- 3.Strawford A, Antelo F, Christiansen M, Hellerstein MK. Adipose tissue triglyceride turnover, de novo lipogenesis, and cell proliferation in humans measured with 2H2O. Am J Physiol Endocrinol Metab. 2004;286:E577–E588. doi: 10.1152/ajpendo.00093.2003. [DOI] [PubMed] [Google Scholar]
- 4.Ruderman NB, Saha AK, Kraegen EW. Minireview: malonyl CoA, AMP-activated protein kinase, and adiposity. Endocrinology. 2003;144:5166–5171. doi: 10.1210/en.2003-0849. [DOI] [PubMed] [Google Scholar]
- 5.Scott JW, Norman DG, Hawley SA, Kontogiannis L, Hardie DG. Protein kinase substrate recognition studied using the recombinant catalytic domain of AMP-activated protein kinase and a model substrate. J Mol Biol. 2002;317:309–323. doi: 10.1006/jmbi.2001.5316. [DOI] [PubMed] [Google Scholar]
- 6.Hauner H, Schmid P, Pfeiffer EF. Glucocorticoids and insulin promote the differentiation of human adipocyte precursor cells into fat cells. J Clin Endocrinol Metab. 1987;64:832–835. doi: 10.1210/jcem-64-4-832. [DOI] [PubMed] [Google Scholar]
- 7.Djurhuus CB, Gravholt CH, Nielsen S, Mengel A, Christiansen JS, et al. Effects of cortisol on lipolysis and regional interstitial glycerol levels in humans. Am J Physiol Endocrinol Metab. 2002;283:E172–E177. doi: 10.1152/ajpendo.00544.2001. [DOI] [PubMed] [Google Scholar]
- 8.Slavin BG, Ong JM, Kern PA. Hormonal regulation of hormone-sensitive lipase activity and mRNA levels in isolated rat adipocytes. J Lipid Res. 1994;35:1535–1541. [PubMed] [Google Scholar]
- 9.Gao Z, Zhang X, Zuberi A, Hwang D, Quon MJ, et al. Inhibition of insulin sensitivity by free fatty acids requires activation of multiple serine kinases in 3T3-L1 adipocytes. Mol Endocrinol. 2004;18:2024–2034. doi: 10.1210/me.2003-0383. [DOI] [PubMed] [Google Scholar]
- 10.Tomlinson JW, Walker EA, Bujalska IJ, Draper N, Lavery GG, et al. 11beta-hydroxysteroid dehydrogenase type 1: a tissue-specific regulator of glucocorticoid response. Endocr Rev. 2004;25:831–866. doi: 10.1210/er.2003-0031. [DOI] [PubMed] [Google Scholar]
- 11.Paulmyer-Lacroix O, Boullu S, Oliver C, Alessi MC, Grino M. Expression of the mRNA coding for 11beta-hydroxysteroid dehydrogenase type 1 in adipose tissue from obese patients: an in situ hybridization study. J Clin Endocrinol Metab. 2002;87:2701–2705. doi: 10.1210/jcem.87.6.8614. [DOI] [PubMed] [Google Scholar]
- 12.Rask E, Walker BR, Soderberg S, Livingstone DE, Eliasson M, et al. Tissue-specific changes in peripheral cortisol metabolism in obese women: increased adipose 11beta-hydroxysteroid dehydrogenase type 1 activity. J Clin Endocrinol Metab. 2002;87:3330–3336. doi: 10.1210/jcem.87.7.8661. [DOI] [PubMed] [Google Scholar]
- 13.Rosenstock J, Banarer S, Fonseca VA, Inzucchi SE, Sun W, Yao W, et al. The 11-beta-hydroxysteroid dehydrogenase type 1 inhibitor INCB13739 improves hyperglycemia in patients with type 2 diabetes inadequately controlled by metformin monotherapy. Diabetes Care. 2010;33:1516–1522. doi: 10.2337/dc09-2315. dc09-2315 [pii];10.2337/dc09-2315 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gathercole LL, Bujalska IJ, Stewart PM, Tomlinson JW. Glucocorticoid modulation of insulin signaling in human subcutaneous adipose tissue. J Clin Endocrinol Metab. 2007;92:4332–4339. doi: 10.1210/jc.2007-1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qiao L, Maclean PS, Schaack J, Orlicky DJ, Darimont C, et al. C/EBPalpha regulates human adiponectin gene transcription through an intronic enhancer. Diabetes. 2005;54:1744–1754. doi: 10.2337/diabetes.54.6.1744. [DOI] [PubMed] [Google Scholar]
- 16.Jamdar SC. Glycerolipid biosynthesis in rat adipose tissue. Influence of adipose-cell size and site of adipose tissue on triacylglycerol formation in lean and obese rats. Biochem J. 1978;170:153–160. doi: 10.1042/bj1700153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bujalska IJ, Gathercole LL, Tomlinson JW, Darimont C, Ermolieff J, et al. A novel selective 11beta-hydroxysteroid dehydrogenase type 1 inhibitor prevents human adipogenesis. J Endocrinol. 2008;197:297–307. doi: 10.1677/JOE-08-0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simacopoulos-Jeannet F, Brichard S, Rencurel F, Cusin I, Jeanrenaud B. In vivo effects of hyperinsulinemia on lipogenic enzymes and glucose transporter expression in rat liver and adipose tissues. Metabolism. 1995;44:228–233. doi: 10.1016/0026-0495(95)90270-8. [DOI] [PubMed] [Google Scholar]
- 19.Zammit VA. The malonyl-CoA-long-chain acyl-CoA axis in the maintenance of mammalian cell function. Biochem J. 1999;343 Pt 3:505–515. [PMC free article] [PubMed] [Google Scholar]
- 20.Villena JA, Roy S, Sarkadi-Nagy E, Kim KH, Sul HS. Desnutrin, an adipocyte gene encoding a novel patatin domain-containing protein, is induced by fasting and glucocorticoids: ectopic expression of desnutrin increases triglyceride hydrolysis. J Biol Chem. 2004;279:47066–47075. doi: 10.1074/jbc.M403855200. [DOI] [PubMed] [Google Scholar]
- 21.Tomlinson JW, Sherlock M, Hughes B, Hughes SV, Kilvington F, et al. Inhibition of 11{beta}-HSD1 activity in vivo limits glucocorticoid exposure to human adipose tissue and decreases lipolysis. J Clin Endocrinol Metab. 2007;92:857–64. doi: 10.1210/jc.2006-2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lammert O, Grunnet N, Faber P, Bjornsbo KS, Dich J, et al. Effects of isoenergetic overfeeding of either carbohydrate or fat in young men 1. Br J Nutr. 2000;84:233–245. [PubMed] [Google Scholar]
- 23.Volpe JJ, Marasa JC. Hormonal regulation of fatty acid synthetase, acetyl-CoA carboxylase and fatty acid synthesis in mammalian adipose tissue and liver. Biochim Biophys Acta. 1975;380:454–472. doi: 10.1016/0005-2760(75)90113-7. [DOI] [PubMed] [Google Scholar]
- 24.Diamant S, Shafrir E. Modulation of the activity of insulin-dependent enzymes of lipogenesis by glucocorticoids. Eur J Biochem. 1975;53:541–546. doi: 10.1111/j.1432-1033.1975.tb04097.x. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y, Jones VB, Urs S, Kim S, Soltani-Bejnood M, Quigley N, et al. The human fatty acid synthase gene and de novo lipogenesis are coordinately regulated in human adipose tissue. J Nutr. 2004;134:1032–1038. doi: 10.1093/jn/134.5.1032. [DOI] [PubMed] [Google Scholar]
- 26.Abu-Elheiga L, Matzuk MM, Kordari P, Oh W, Shaikenov T, et al. Mutant mice lacking acetyl-CoA carboxylase 1 are embryonically lethal. Proc Natl Acad Sci U S A. 2005;102:12011–12016. doi: 10.1073/pnas.0505714102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mao J, DeMayo FJ, Li H, Abu-Elheiga L, Gu Z, Shaikenov TE, et al. Liver-specific deletion of acetyl-CoA carboxylase 1 reduces hepatic triglyceride accumulation without affecting glucose homeostasis. Proc Natl Acad Sci U S A. 2006;103:8552–8557. doi: 10.1073/pnas.0603115103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oh W, Abu-Elheiga L, Kordari P, Gu Z, Shaikenov T, et al. Glucose and fat metabolism in adipose tissue of acetyl-CoA carboxylase 2 knockout mice. Proc Natl Acad Sci U S A. 2005;102:1384–1389. doi: 10.1073/pnas.0409451102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Viana AY, Sakoda H, Anai M, Fujishiro M, Ono H, et al. Role of hepatic AMPK activation in glucose metabolism and dexamethasone-induced regulation of AMPK expression. Diabetes Res Clin Pract. 2006;73:135–142. doi: 10.1016/j.diabres.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 30.Christ-Crain M, Kola B, Lolli F, Fekete C, Seboek D, Wittmann G, et al. AMP-activated protein kinase mediates glucocorticoid-induced metabolic changes: a novel mechanism in Cushing's syndrome. FASEB J. 2008;22:1672–1683. doi: 10.1096/fj.07-094144. fj.07-094144 [pii];10.1096/fj.07-094144 [doi] [DOI] [PubMed] [Google Scholar]
- 31.Kola B, Christ-Crain M, Lolli F, Arnaldi G, Giacchetti G, et al. Changes in adenosine 5′-monophosphate-activated protein kinase as a mechanism of visceral obesity in Cushing's syndrome. J Clin Endocrinol Metab. 2008;93:4969–4973. doi: 10.1210/jc.2008-1297. jc.2008-1297 [pii];10.1210/jc.2008-1297 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tomlinson JJ, Boudreau A, Wu D, Abdou SH, Carrigan A, et al. Insulin sensitization of human preadipocytes through glucocorticoid hormone induction of forkhead transcription factors. Mol Endocrinol. 2010;24:104–113. doi: 10.1210/me.2009-0091. me.2009-0091 [pii];10.1210/me.2009-0091 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pouliot MC, Despres JP, Nadeau A, Moorjani S, Prud'homme D, et al. Visceral obesity in men. Associations with glucose tolerance, plasma insulin, and lipoprotein levels. Diabetes. 1992;41:826–834. doi: 10.2337/diab.41.7.826. [DOI] [PubMed] [Google Scholar]
- 34.Fontbonne A, Thibult N, Eschwege E, Ducimetiere P. Body fat distribution and coronary heart disease mortality in subjects with impaired glucose tolerance or diabetes mellitus: the Paris Prospective Study, 15-year follow-up. Diabetologia. 1992;35:464–468. doi: 10.1007/BF02342445. [DOI] [PubMed] [Google Scholar]
- 35.Zierath JR, Livingston JN, Thorne A, Bolinder J, Reynisdottir S, et al. Regional difference in insulin inhibition of non-esterified fatty acid release from human adipocytes: relation to insulin receptor phosphorylation and intracellular signalling through the insulin receptor substrate-1 pathway. Diabetologia. 1998;41:1343–1354. doi: 10.1007/s001250051075. [DOI] [PubMed] [Google Scholar]
- 36.Fried SK, Russell CD, Grauso NL, Brolin RE. Lipoprotein lipase regulation by insulin and glucocorticoid in subcutaneous and omental adipose tissues of obese women and men. J Clin Invest. 1993;92:2191–2198. doi: 10.1172/JCI116821. 10.1172/JCI116821 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Laviola L, Perrini S, Cignarelli A, Natalicchio A, Leonardini A, De SF, et al. Insulin signaling in human visceral and subcutaneous adipose tissue in vivo. Diabetes. 2006;55:952–961. doi: 10.2337/diabetes.55.04.06.db05-1414. 55/4/952 [pii] [DOI] [PubMed] [Google Scholar]
- 38.Lundgren M, Buren J, Lindgren P, Myrnas T, Ruge T, Eriksson JW. Sex- and Depot-specific Lipolysis Regulation in Human Adipocytes: Interplay between Adrenergic Stimulation and Glucocorticoids. Horm Metab Res. 2008;40:854–60. doi: 10.1055/s-0028-1087168. [DOI] [PubMed] [Google Scholar]
- 39.Alberts P, Nilsson C, Selen G, Engblom LO, Edling NH, Norling S, et al. Selective inhibition of 11{beta}-hydroxysteroid dehydrogenase type 1 improves hepatic insulin sensitivity in hyperglycemic mice strains. Endocrinology. 2003;144:4755–4762. doi: 10.1210/en.2003-0344. [DOI] [PubMed] [Google Scholar]
- 40.Masuzaki H, Paterson J, Shinyama H, Morton NM, Mullins JJ, Seckl JR. A transgenic model of visceral obesity and the metabolic syndrome. Science. 2001;294:2166–2170. doi: 10.1126/science.1066285. [DOI] [PubMed] [Google Scholar]
- 41.Berthiaume M, Laplante M, Festuccia W, Gelinas Y, Poulin S, Lalonde J, et al. Depot-specific modulation of rat intraabdominal adipose tissue lipid metabolism by pharmacological inhibition of 11beta-hydroxysteroid dehydrogenase type 1. Endocrinology. 2007;148:2391–2397. doi: 10.1210/en.2006-1199. [DOI] [PubMed] [Google Scholar]
- 42.Morgan SA, Sherlock M, Gathercole LL, Lavery GG, Lenaghan C, Bujalska IJ, et al. 11{beta}-hydroxysteroid dehydrogenase type 1 regulates glucocorticoid-induced insulin resistance in skeletal muscle. Diabetes. 2009;58:2506–15. doi: 10.2337/db09-0525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim JK, Fillmore JJ, Sunshine MJ, Albrecht B, Higashimori T, et al. PKC-theta knockout mice are protected from fat-induced insulin resistance. J Clin Invest. 2004;114:823–827. doi: 10.1172/JCI22230. [DOI] [PMC free article] [PubMed] [Google Scholar]