Abstract
Background:
Child care is mostly the responsibility of mothers. Several studies have revealed that the mothers’ education has a positive impact on their knowledge and practice in child health matters.
Objectives:
The study was undertaken to assess the level of mothers’ knowledge on certain aspects of child health care and whether there is any correlation between their level of knowledge and the number of years of formal education they have had.
Materials and Methods:
A two-part questionnaire was distributed. The first part comprised information about mother's nationality, age, work, level of education and number of children, in addition to sources of health information and the role of school education in child health matters. The second part contained 40 statements about different aspects of child health matters. A structured interview with the mothers who attended with their children at the pediatric outpatient clinic of King Khalid University Hospital in Riyadh during July and August 2007, was conducted by a trained non-medical research assistant using the items and statements of the questionnaire as a base. A knowledge score was calculated from the number of correct answers. The maximum score was 40. An arbitrary cut-off score of 25 was considered satisfactory.
Results:
Three-hundred-seventy-three questionnaires were completed. The mean score of the total sample was 25 (out of 40) and the minimum score obtained was 14, and the maximum 36. Fifty-eight percent scored 25 or more. Scrutiny of individual items on the questionnaire revealed significant and serious gaps in mother's knowledge. No statistically significant correlation was evident between mothers’ knowledge of child health related matters and level of education, age, or number of children.
Conclusion:
Mothers’ knowledge of child health related matters is deficient. At present, knowledge on child health matters taught in schools in the Kingdom is inadequate. Health care institutions play a limited role in health education. There should be proper effective practical means of disseminating information on child health matters among mothers in our community.
Keywords: Child health matters, health care professionals, mothers’ knowledge, school education
INTRODUCTION
Child care is mostly the responsibility of mothers. Therefore, the mother's knowledge about child care influences the nature and quality of care that is given to the child.[1] Several studies have revealed that the mothers’ level of education has a positive impact on her knowledge and how she deals with child health care issues.[2–13] Our experience in pediatric practice has revealed significant gaps pertaining to child health issues in the mothers’ knowledge. There seems to have been very little improvement in the knowledge of mothers on common child health matters over the years inspite of the many years of girls education in the country.
This descriptive cross-sectional survey aimed to answer the following questions: (1) What is the level of mothers’ knowledge of certain aspects of child health matters? (2) What are the main sources of health information and which ones are the most useful? (3) Is there a correlation between mothers’ level of knowledge and the number of years spent in formal education? (4) In the mother's view, does the current formal education of girls in schools/colleges have a significant impact on mothers’ knowledge of child health matters.
MATERIALS AND METHODS
A two-part questionnaire was designed by the author. It was reviewed and refined by two other colleagues who have a lot of experience in pediatrics. The first part comprised information about mothers’ nationality, age, work, level of education and the number of children she has in addition to sources of health information and the role of formal school education in child health matters. The second part contained 40 statements about different aspects of child health issues including nutrition, immunization, development, accident prevention, certain neonatal and infants’ problems or behaviors and some common childhood illnesses. Mothers who attended with their children at the pediatric outpatient clinic of King Khalid University Hospital in Riyadh during the months of July and August, in 2007, were invited to participate in the study. Those who agreed were interviewed by a trained non-medical research assistant using the items and statements of the questionnaire as a basis for the structured interview. It was indicated clearly to the mothers that participation was voluntary and their non- contribution would have no adverse effect on the quality of care given to their child in the hospital. The mothers were requested to indicate whether each statement was correct or not. They scored one point for each knowledge question answered correctly and zero for wrong and “do not know” answers. A knowledge score was calculated from the number of correct answers. The maximum score was 40. An arbitrary cut-off score of 25 was considered satisfactory. The first 20 questionnaires completed were used as a pilot test to evaluate the clarity of language and level of information in the questionnaire. This resulted in a few modifications to the questionnaire. These questions were not included in the final analysis of results.
Data was entered in MS Excel and analyzed using SPSS PC+ 11.5 Version statistical software.[14] Descriptive statistics, mean and standard deviation and proportion were used to quantify the study and outcome variables. Chi-square test was used to observe the association between two categorical variables. A p-value of < 0.05 was considered statistically significant.
RESULTS
Three-hundred-seventy-three questionnaires were completed. Demographic data regarding nationality, age, work, education, and number of children are represented in Table 1. As the main source of health information, 295 (80%) cited family members (grandmothers, mothers, sisters, relatives etc.), 30 (8.2%) cited schools, 68 (17.2%) cited TV and radio, 60 (16%) cited journals and magazines, 52 (14.2%) cited friends, colleagues and other members of society, 101 (27.1%) cited books and only 25 (7.1%) cited health care professionals.
Table 1.
Demographic data of the mothers

Two hundred twenty-five (60.6%) of the mothers believe that formal girls’ education in schools and colleges does not provide sufficient child health education. On the question of where to obtain useful information of child health, 287 (77.6%) of the mothers supported the increase in instruction on child health in the curriculum in schools, 284 (77%) supported specific courses on child health targeting girls and women, 321 (86.8%) supported the use of the mass media, and 311 (84.1%) supported programs run by health care professionals.
The mean knowledge score of the total sample was 25 (out of 40), the minimum score obtained was 14 and the maximum was 36. Two hundred and eighteen (58.4%) scored 25 or more. We found no statistically significant correlation between the total score on mothers’ knowledge or any of the items on the knowledge questionnaire and mothers’ level of education.
Table 2 indicates total knowledge score in relation to mothers’ education, age and number of children. The results of mothers’ responses to individual items on the knowledge questionnaire are indicated in Table 3.
Table 2.
Association between the scores of mother's knowledge and mother's age, educational status and number of children
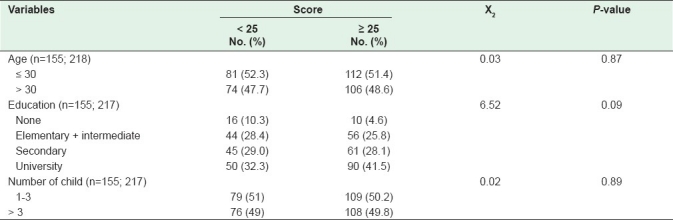
Table 3.
Mother's response to the knowledge questionnaire
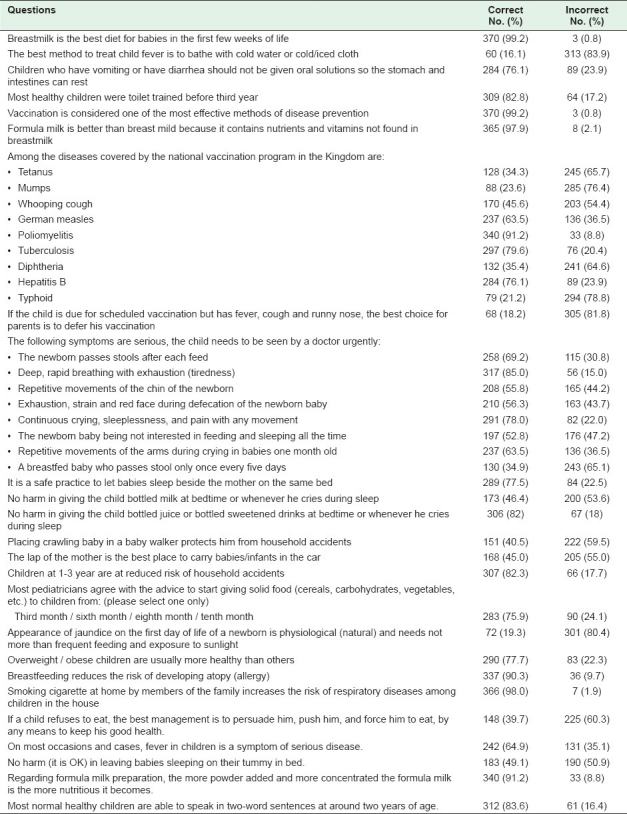
Incorrect knowledge on certain specific items of the questionnaire included 131 (35.1%) who believed that on most occasions, fever in children was a symptom of serious disease, 313 (83.9%) believed that the best method to treat a child with a fever was to bathe him/her with cold water or wipe with cold or iced cloth. Questions on diseases covered by the national vaccination program revealed that 285 (76.4%) believed that mumps was not targeted, 245 (65.7%) believed that tetanus was not targeted, 203 (54.4%) believed that whooping cough (pertussis) was not targeted and 241(64.6%) believed that diphtheria was not targeted by the national vaccination program. However, 294 (78.8%) believed that typhoid was targeted by the program. Three-hundred and five (81.8%) of the mothers believed that the best course of action for parents of a child who was due for a scheduled vaccination but has a fever, cough and runny nose (symptoms of upper respiratory infection) was to defer the vaccination until he was completely symptom free. On the question of conditions which were regarded as serious and warranted urgent attention by a doctor, 176 (47.2%) did not see the need for the newborn baby who was sleeping all the time and was not interested in feeding to be seen by a doctor. Another 82 (22%) disagreed with seeking medical help for a child who cries continuously, does not sleep and who has pain with every movement. Three-hundred and one (80.7%) of mothers believed that the appearance of jaundice on the first day of the life of a newborn was physiological (natural) and so nothing other than more frequent feeding and exposure to sunlight was required. It is noteworthy that more than 30% of the mothers believed that a newborn baby who passes stools after each feed, or a newborn who is otherwise healthy but has repetitive movements of the chin, or one who strains and becomes red in the face during defecation, or a breast fed baby who passes stools only once every 5 days, may have a serious illness and needed urgent medical attention.
On feeding practices, 200 (53.6%) of the mothers believed that there was no harm in giving a child a bottle of milk at bedtime in bed or whenever he cried during sleep; 90 (24.1%) did not agree that the most acceptable time to start solid food for children was at 6 months of age, 225 (60.3%) agreed with force-feeding when children refused to eat.
Results on the items on safety practices revealed that only 84 (22.5%) of the mothers believed that it was harmless to let babies sleep by their mothers in the same bed. One-hundred and ninety (50.9%) thought that it was not harmful to let babies sleep on their tummy in bed (prone sleep position). Two hundred two (59.5%) believed that putting a baby who crawls in a walker protected him from household accidents. Two-hundred and five (55%) believed that the best place for a baby/an infant to sit or be carried in a car was the mother's lap.
DISCUSSION
Our results revealed that the mean score of the sample which was just above the cut-off score, was an indication of a satisfactory knowledge level. The score was arbitrarily fixed at 25. If it had been fixed at 20, the knowledge of more than 90% would have been satisfactory, on the other hand, if it had been raised to 30 the knowledge of only 12% would have been satisfactory.
A closer look at some items revealed significant and sometimes serious gaps in the mothers’ knowledge. Similar gaps have been reported from different societies.[7,15–21]
Our results indicated that a majority of mothers believed that the best method to treat a child with a fever was to bathe him with cold water or rub him with ice cold cloth. This was worse than that reported by Al Eissa et al where 50% of the parents would use cold water and 7% ice water for the treatment of fever.[22] Impicciatore et al reported that 9% of the mothers used iced packing to reduce fever.[23]
Knowledge of the diseases covered by the national vaccination program revealed that a high proportion of mothers were not fully informed about certain diseases targeted by the program. Impicciatore et al reported that only 26% of Italian mothers were able to state the vaccinations which were compulsory.[6]
Our results revealed no statistically significant correlation between mother’s knowledge score and their level of education, age or number of children. This is similar to the results of Jan et al (Jeddah, KSA, 2000) who found no correlation between parents’ level of education and safety practices,[24] but contrary to the finding of Moawed et al (Riyadh, KSA, 2000) who found a statistically significant correlation between mothers’ knowledge and their practices during infants’ diarrheal episodes and mothers’ age, education and birth order.[7] It is also not in accord with Shawky et al (Jeddah, KSA, 2001) who reported on the effect of maternal education on the rate of childhood handicap and found that the risk of having a handicapped child declined sharply with the increase in the level of maternal education.[9] One possible explanation of this difference in the results could be the use of different research methodology (sample selection, data gathering and others).
It is worrying to find that the majority of mothers believed that jaundice on the first day of life of a newborn was physiological (natural) and required no more than frequent feeding and exposure to sun light. Also disturbing is the fact that nearly half did not realize that a newborn baby who slept all the time and was not interested in feeding could be seriously sick and needed to be seen urgently by a doctor; another quarter did not realize that a child who cried continuously, who did not sleep and was in pain with every movement was sick enough to require urgent medical attention. Dongre et al from rural India reported that 23% of mothers were not aware of any danger signs in a newborn such as, poor sucking, low birth weight, lethargy/ unconsciousness, rapid/difficult breathing. These were indicated as danger signs by 34.4%, 25.8%, 25.5%, 10.3% mothers respectively, while hypothermia and convulsions were referred to as danger signs by 10.3% and 8.6% mothers respectively.[16]
The majority of mothers cited family members as their main source of health information, which is higher than what was reported by Al Eissa et al, where some 35% of the parents mentioned friends and relatives as their main source of information.[22]
Only few mothers cited health care professionals as their main source of health information. In the report by Impecciatore et al from Italy, only 42% of the mothers said that the pediatricians had spontaneously spoken to them about vaccination during consultation with a child.[6] Al Eissa et al reported that only a group of 37% of parents cited medical personnel as their source of information.[22] These findings reflect a lack of active educational intervention by professionals.[22]
It is encouraging to find that more than three-fourths of the mothers believed that it was harmful to let babies sleep with them in the same bed. This is contrary to the finding of Jan et al on which 75% of the mothers reported sleeping next to their infants in the same bed, though it is difficult to discern whether mothers were compelled to do so by social circumstances or they believed it was safer for their infant.[24]
Few mothers cited schools as the main source of health information. Around two-thirds believed that schools did not provide sufficient information on child health and more than two-thirds supported the increase of education of child health in the curriculum of schools.
According to Kolbe, behaviors and attitudes about health that began during childhood were responsible for most of the deaths, illnesses and disability. Comprehensive health education programs in schools represent one effective way of providing students with the knowledge and skills to prevent health-impairing behavior.[25]
Several previous studies stressed that health education in school curricula was not adequate,[26] and that the knowledge of high school girls and university students on health matters was deficient.[27–30]
Furthermore, studies have shown that school teachers were not trained to give health education in schools.[26,31] Their college curriculum did not equip them for such a role[29] and so the teachers refrained from teaching health subjects.[32]
According to Summerfield and others, health education works. Hundreds of studies have evaluated health education and concluded that it was effective, but its effectiveness depended upon factors such as teacher training, comprehensiveness of the health program, time available for instruction, family involvement and community support.[25,32–34]
The responsibility for health education was not to be left solely to schools. In addition to all other sectors of the community, health care personnel and other health care institutions should play a major role in health education.
Milaat et al, Agble et al and Kari et al, reported successful involvement of health care personnel and medical students in targeted health education classes for school children and university students.[26,30,35] Such efforts may prove more effective than formal general health education classes taught by uninterested, unenthusiastic, untrained school teachers. Health care professionals’ advice has a good influence on patients and parents.[36] Every visit to a health care professional or every health care facility or institution by patients/parents should be an opportunity for the delivery of a short course in health education.
Possible limitations of the study are that the sample of mothers selected may not have been representative of the community; mothers who volunteered to participate in the survey may prove to be different from the non-participants. Whether the respondents were serious in completing the questionnaire and whether research assistant had influenced the responses of the mothers to the questionnaires is not known.
CONCLUSION
The study revealed significant gaps in mothers’ knowledge of certain child health matters. It also revealed that health education in schools was deficient and it also exposed the limited involvement of health care personnel and institutions in health care education.
There is a need for health education programs that target high school girls, university students, mothers and other caregivers (e.g. fathers). These should be delivered by trained personnel in classes, courses, and special sessions. In addition, health care facilities should be reformed to make health education an essential and compulsory part of health care delivery. Involvement in these educational activities should be a mandatory requirement for the issue of a license to practice.
Acknowledgments
The author would like to thank Dr. Khalid Al Mobaireek and Dr. Abdullah Al Angari for assistance in the design of the questionnaire, Ms. Latifa Abunayyan for data collection, Mr. Nayeemudin Abdulqader for data entry, Dr. Shaffi Sheikh for help in statistical analysis, Ms. Loida M. Sese and Ms. Liza Antonio for their secretarial help. I am also most grateful to Prof. Mustafa Salih, Prof. Zabidi Hussain and Prof. Jamal Al Jarallah for reviewing the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
REFERENCES
- 1.Kamau-Thuita F, Omwega AM, Muita JW. Child care practices and nutritional status of children aged 0-2 years in Thika, Kenya. East Afr Med J. 2002;79:524–9. doi: 10.4314/eamj.v79i10.8814. [DOI] [PubMed] [Google Scholar]
- 2.Birenbaum E, Fuchs C, Reichman B. Demographic factors influencing the initiation of breast-feeding in an Israeli urban population. Pediatrics. 1989;83:519–23. [PubMed] [Google Scholar]
- 3.Yeung DL, Pennel Md, Leung M, Hall J. Breastfeeding: Prevalence and influencing factors. Can J Public Health. 1981;72:323–30. [PubMed] [Google Scholar]
- 4.Kolahi AA, Tahmooresdeh S. First febrile convulsions: Inquiry about the knowledge, attitudes and concerns of the patients’ mothers. Eur J Pediatr. 2009;168:167–71. doi: 10.1007/s00431-008-0724-z. [DOI] [PubMed] [Google Scholar]
- 5.Vereecken CA, Kaulelier E, Maes L. Influence of mother's educational level on food parenting practices and food habits of young children. Appetite. 2004;43:93–103. doi: 10.1016/j.appet.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Impicciatore P, Bosetti C, Schiavio S, Pandolfini C, Bonati M. Mothers as active partners in the prevention of childhood disease: Maternal factors related to immunization status of preschool children in Italy. Prev Med. 2000;3l:49–55. doi: 10.1006/pmed.2000.0677. [DOI] [PubMed] [Google Scholar]
- 7.Moawed SA, Saeed AA. Knowledge and practices of mothers about infants’ diarrheal episodes. Saudi Med J. 2000;21:1147–51. [PubMed] [Google Scholar]
- 8.McCune YD, Richardson MM, Powell JA. Psychosocial Health Issues in Pediatric Practices: Parents’ knowledge and concerns. Pediatrics. 1984;74:183–90. [PubMed] [Google Scholar]
- 9.Shawky S, Milaat WM, Abalkhail BA, Soliman NK. Effect of maternal education on the rate of childhood handicap. Saudi Med J. 2001;22:39–43. [PubMed] [Google Scholar]
- 10.Akpabio A, Klausner CP, Inglehart MR. Mothers / guardians’ knowledge about promoting children's oral health. J Dent Hyg. 2008;82:12. [PubMed] [Google Scholar]
- 11.Thein MM, Lee J, Yoong T. Knowledge about developmental screening in mothers attending a maternal and child health clinic in Singapore. Ann Acad Med Singapore. 1992;21:735–40. [PubMed] [Google Scholar]
- 12.Rahman MM, Islam MA, Mahalanabis D. Mothers’ knowledge about vaccine preventable diseases and immunization coverage in a population with high rate of illiteracy. J Trop Pediatr. 1995;4l:376–8. doi: 10.1093/tropej/41.6.376. [DOI] [PubMed] [Google Scholar]
- 13.Saeed AA, Bani IA. Prevalence and correlates of acute respiratory infections in children less than two years of age. Saudi Med J. 2000;21:1152–6. [PubMed] [Google Scholar]
- 14.SPSS Inc. SPSS for Windows. 11.0.1 ed. Chicago, IL: SPSS Inc; 2001. [Google Scholar]
- 15.Subbiah N. Knowledge of mothers on prevention of childhood accidents – a study with particular reference to selected area of New Delhi. Nurs J India. 2006;97:229–31. [PubMed] [Google Scholar]
- 16.Dongre AR, Deshmukh PR, Garg BS. Perceptions and health care seeking about newborn danger signs among mothers in rural Wardha. Indian J Pediatr. 2008;75:325–9. doi: 10.1007/s12098-008-0032-7. [DOI] [PubMed] [Google Scholar]
- 17.Blinkhorn AS, Wainwright-Stringer YM, Holloway PJ. Dental Health knowledge and attitudes of regularly attending mothers of high-risk, pre-school children. Int Dent J. 2001;51:435–8. doi: 10.1002/j.1875-595x.2001.tb00856.x. [DOI] [PubMed] [Google Scholar]
- 18.Baker LM, Wilson FL, Nordstrom CK, Legwand C. Mother's knowledge and information needs relating to childhood immunizations. Issues Compr Pediatr Nurs. 2007;30:39–53. doi: 10.1080/01460860701366666. [DOI] [PubMed] [Google Scholar]
- 19.Linder N, Sirota L, Snapir A, Eisen I, Davidovitch N, Kaplan G, et al. Parental knowledge of the treatment of fever in children. Isr Med Assoc J. 1999;1:158–60. [PubMed] [Google Scholar]
- 20.Al Nouri L, Basheer K. Mothers’ perceptions of fever in children. J Trop Pediatr. 2006;52:113–6. doi: 10.1093/tropej/fmi076. [DOI] [PubMed] [Google Scholar]
- 21.Parmar RC, Sahu DR, Bavdekar SB. Knolwedge, attitude and practices of parents of children with febrile convulsion. J Postgrad Med. 2000;47:19–23. [PubMed] [Google Scholar]
- 22.al-Eissa YA, al-Zamil FA, al-Sanie AM, al-Salloum AA, al-Tuwaijri HM, al-Abdali NM, et al. Home management of fever in children: Rational or ritual? Int J Clin Pract. 2000;54:138–42. [PubMed] [Google Scholar]
- 23.Impicciatore P, Nannini S, Pandolfini C, Bonati M. Mother's knowledge of, attitudes toward, and management of fever in preschool children in Italy. Prev Med. 1998;27:268–73. doi: 10.1006/pmed.1998.0262. [DOI] [PubMed] [Google Scholar]
- 24.Jan MM, Hasanain FH, Al-Dabbagh AA. Infant and child safety practices of parents. Saudi Med J. 2000;21:1142–6. [PubMed] [Google Scholar]
- 25.Kolbe LJ. An essential strategy to improve the health and education of Americans. Prev Med. 1993;22:1–17. doi: 10.1006/pmed.1993.1047. [DOI] [PubMed] [Google Scholar]
- 26.Milaat WA, Al Bar HM. Education of female students in reproductive health issues in Jeddah: The role of school workers. Saudi Med J. 1998;19:185–8. [PubMed] [Google Scholar]
- 27.Al Almaie S. Knowledge of healthy diets among adolescents in eastern Saudi Arabia. Ann Saudi Med. 2005;25:294–8. doi: 10.5144/0256-4947.2005.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al Dabal BK. Breastfeeding: Knowledge and attitude of college girls. Saudi Med J. 1998;19:437–40. [PubMed] [Google Scholar]
- 29.Milaat WA, Al Bar HS, Ghabrah TM, Abalkhail BS. Factors affecting knowledge and practices of female school students in reproductive life issues in Jeddah, Saudi Arabia. Saudi Med J. 1996;17:704–8. [Google Scholar]
- 30.Kari JA, Bardisi ES, Baitalmal RM, Ageely GA. Folic acid awareness among female college students.Neural tube defects prevention. Saudi Med J. 2008;29:1749–51. [PubMed] [Google Scholar]
- 31.Alnasir FA. Health attitudes of school teachers. Saudi Med J. 2004;25:326–30. [PubMed] [Google Scholar]
- 32.Summerfield LM. National Standards for School Health Education. ERIC Digest. [Last accessed on 2009 Mar 22]. Available from: http://ericdigest.org/1996-2-/health.html .
- 33.Allensworth DD. Health Education: State of the art. J Sch Health. 1993;63:14–20. doi: 10.1111/j.1746-1561.1993.tb06052.x. [DOI] [PubMed] [Google Scholar]
- 34.Lavin AT. Comprehensive school health education: Barriers and opportunities. J Sch Health. 1993;63:24–7. doi: 10.1111/j.1746-1561.1993.tb06054.x. [DOI] [PubMed] [Google Scholar]
- 35.Agble YM, Arafa M. Health Education in schools: The Tabuk experience. Saudi Med J. 1999;20:649–50. [PubMed] [Google Scholar]
- 36.De Chateau P, Holmberg H, Jakobsson K, Winberg J. A study of factors promoting and inhibiting lactation. Dev Med Child Neurol. 1997;19:575–84. doi: 10.1111/j.1469-8749.1977.tb07989.x. [DOI] [PubMed] [Google Scholar]


