Abstract
Background:
To compare the disability among patients with bipolar disorder and recurrent depressive disorder in remission.
Settings and Design:
Cross-sectional study of outpatients.
Materials and Methods:
Patients in the remission phase of the illness were taken for the study. Disability assessment was done using Indian Disability Evaluation and Assessment Scale. Treatment compliance was measured using medication adherence rating scale.
Statistical Analysis:
Between group comparison.
Results:
A total of 40 patients were included in the study, 25 in bipolar and 15 in recurrent depressive disorder group. There was no difference between the groups in the domain of self care. The bipolar patients had more impairment in interpersonal activities than recurrent depressive disorder (RDD) group, this difference was statistically significant (P=0.004). The bipolar patients had more impairment in communication and understanding (P=0.009) and in work (P=0.011). The mean total score for disability was more for bipolar patients (P=0.0001). The total duration of illness had significant influence on communication and understanding, work, and total disability scores. The total number of episodes significantly influenced the impairment in interpersonal activities, communication and understanding, work, and total disability scores. The impairment in self care was significantly associated with the total number of psychotic episodes (P=0.0013). No significant relation was found between treatment compliance and disability.
Conclusions:
The patients with mood disorders had significant disability even during the periods of remission. The impairment was more for the bipolar patients compared with the RDD patients.
Keywords: Bipolar, disability, recurrent depressive disorder, remission
INTRODUCTION
Disability is a limitation in functioning that may be associated with many disorders, both physical and mental. Oxford dictionary defines disability as “a state of incapacity,” “a state that disqualifies one.” According to International Classification of Impairment, Disability and Handicap (ICIDH, 1980), disability is the interference with activities of the whole person in relation to the immediate environment.[1]
Psychiatric conditions account for almost 13% of disease burden worldwide. Psychiatric disorders are highly prevalent and begin early in life, frequently resulting in inability to work or function, and as a result, prolonged periods of disability. Globally neuropsychiatric conditions account for 31.7% of years of life lost to disability. Major depression alone accounts for more than one in every 10 years of life lived with disability worldwide. Global burden of disease study recognized that the consequences of disease include not only death but also disability. Unipolar depression ranks first among causes for disability, cutting across both genders, and bipolar disorder is ranked seventh among males and eighth among females.[2]
A complex set of factors contributed to the qualification of disability: Patients’ own perception, self-reported restrictions in performances, evaluation of patients’ performance by key figures in his environment and by medical professional (not only based on dysfunctions but also on diagnosis and prognosis), and normative response from the community.
The self-reported well being and functioning is found to be low in euthymic bipolar patients.[3] Women are more functionally impaired than men among bipolar patients.[4] The functional recovery is late in psychotic affective disorder.[5,6] Premorbid low socioeconomic status,[7] long hospitalization, onset of age <30 years, Axis I comorbidity, and single marital status were associated with poor functional recovery.[5] The self-reported depressive symptoms are more frequent than manic symptoms and cause greater dysfunction in occupational, family, and social functioning in bipolar patients.[8] In a study on disability associated with seven psychiatric disorders, Chaudhury et al.[9] found that 33.3% had disabilities due to depression and 30% due to bipolar disorder, and primary areas of dysfunction in depression was in self care and work, while bipolar disorders tend to cause dysfunction in all area. The presence of depressive spectrum symptoms[10] and the past number of episodes also influence the functional outcome.[11] The affective disorder groups were significantly more likely to report decline in psychosocial functioning compared with that of their first-degree relative who had no lifetime history of affective disorders.[12] The long-term overall functional outcome was found to be poorer for bipolar patients compared with unipolar patients.[13]
Studies on the disability of mood disorder patients in Indian population are rare. Proper assessment of the severity and areas of disability is important for the management and prognostication. Hence, this comparative study was planned in patients with bipolar disorder and recurrent depressive disorder in remission.
MATERIALS AND METHODS
Indian Disability Evaluation and Assessment Scale for disability assessment: It has four domains–self care, interpersonal activities, communication and understanding, and work. Each domain is scored from 0 to 4 depending upon the level of impairment and total score is obtained by adding the individual scores.[14]
Medication Adherence Rating Scale: It is a 10-item checklist for the assessment of treatment adherence. Each item has score 1, a total score of 6 or more is taken as good treatment adherence.[15]
The patients in the remission phase of bipolar disorder and recurrent depressive disorder attending the psychiatry OPD diagnosed as per the ICD10 criteria by the consultants were taken for the study. Remission is defined as those patients having no symptoms of mania or depression for at least 2 months. The sociodemographic and other relevant clinical data are obtained using the proforma. Disability is assessed in the four domains, namely self care, interpersonal activity, communication and understanding, and work. The disability in each domain is categorized as normal, mild, moderate, severe, and profound and the total score is obtained. Treatment compliance is assessed using medication adherence rating scale. Study was conducted for a period of 1 month. The statistical tests used are independent sample t test, Fischer's exact test, Spearman's correlation coefficient, and Pearson's coefficient.
RESULTS
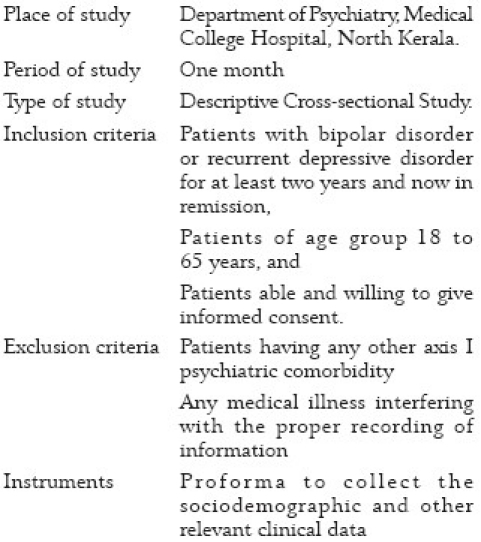
There were a total of 40 patients; 25 bipolar patients in remission and 15 recurrent depressive disorder (RDD) patients in remission. The two groups were comparable with respect to age, sex, education, age of onset, duration of illness, duration of last episode, period of remission, and duration of treatment (all P values >0.05, not significant) [Tables 1 and 2].
Table 1.
Comparison of sociodemographic details
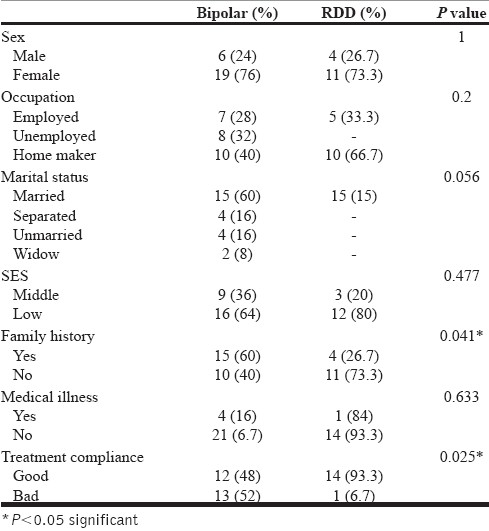
Table 2.
Comparison of sociodemographic details and illness variables
Bipolar patients had a statistically significant (P=0.016) higher mean number of episodes compared with RDD patients. Treatment compliance was found to be better for RDD patients compared with bipolar patients (P=0.025). Total duration of illness was more for bipolar patients compared with RDD patients, but the result was not statistically significant (P=0.095). Duration of treatment was more for bipolar patient (mean 7.72 years).
Statistically no significant difference was observed in two groups with regard to occupation, socioeconomic status, and marital status. However, 60% bipolar patients had family history of mental illness, whereas only 26.7% of RDD patients had a positive family history of mental illness and the difference was statistically significant (P=0.041). Sixteen percent of bipolar patients had medical illness, while only 6.7% of RDD patients had medical illness; this difference was not statistically significant. Forty-eight percent of bipolar patients and 93.3% of RDD patients had good treatment compliance and the difference was statistically significant (P=0.005). The total number of psychotic episodes were more in bipolar patients compared with RDD group (P=0.0001).
Disability
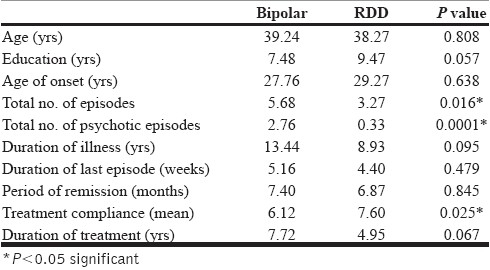
There was no difference between the two groups in the domain of self care. Twelve percent of bipolar patients had self care score ranging from mild to moderate, but none of RDD patients had impaired self care. Eighty four percent of bipolar patients had impairment in interpersonal activities, while majority (48%) scored for moderate impairment, but only 53.3% RDD patients had impairment in interpersonal activities. The difference in impairment in interpersonal activity was statistically significant (P=0.004). Seventy-six percent of the bipolar patients and 33% of RDD patients had impairment in communication and understanding; this difference was statistically significant (P=0.009). Sixty-four percent of bipolar patients had impairment in work, while only 6.7% of RDD patients had impairment in the domain work (P=0.011) [Table 3].
Table 3.
Comparison of disability
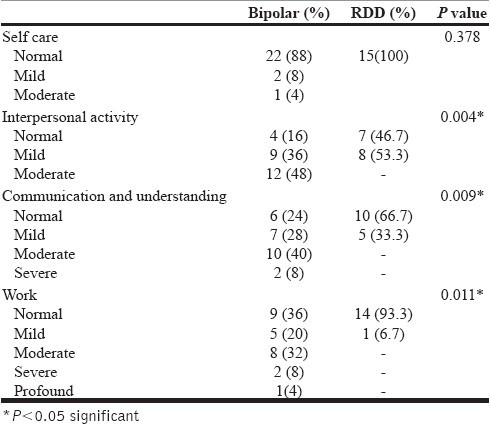
Duration of illness was positively correlated with impairment in communication and understanding among BPAD patients. Severity of impairment in communication and understanding increases with increase in the duration of illness (Spearman's correlation coefficient, r=0.451, P=0.023). The severity of impairment in work, and the total disability score was increased with the duration of illness, and this relation was statistically significant (r=0.522, P=0.007; r=0.516, P=0.008).
The severity of impairment in interpersonal activities, communication and understanding, and work was higher in patients with more number of episodes (r=0.539, P=0.005; r=0.712, P=0.00001; r=0.53, P=0.006). The total score of disability also was found to be high in patients with more number of episodes [Table 4].
Table 4.
Correlation of illness variables with disability domains
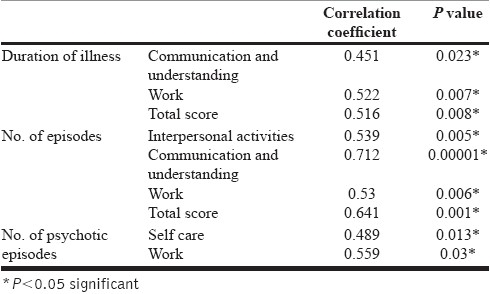
The severity of impairment in self care and work increased with the number of psychotic episodes (r=0.489, P=0.013; r=0.559, P=0.03). It was also found that the severity of impairment in interpersonal activity, communication and understanding, work as well as the total score of disability was increased with the duration of treatment. The total score for disability was more for bipolar patients (mean, 4.04) compared with RDD patients (mean, 0.3) and the difference was statistically significant (P=0.0001).
No significant correlation was noticed between the domains of disability and other factors like age, sex, education, socioeconomic status, age of onset of illness, duration of last episode, family history, treatment compliance, period of remission, chronic medical illness, etc.
DISCUSSION
The study population had no significant difference in their socioeconomic status and occupational status, which was made evident by the nil significant correlation in the study. No significant difference was seen in disability between the two groups with relation to gender. Robb et al.[4] reported that women with bipolar disorder are more likely to have an overall impairment in functioning, but this finding was not replicated in our study. A significantly higher positive family history in bipolar patients is consistent with the earlier studies.[16] In this study, RDD patients had good treatment compliance compared with the other group. We could not establish any significant difference in medical illness in between the two groups, while earlier study showed that there is significant disability associated with patients having comorbid chronic medical illness.[17]
No significant difference was observed in the domain of self care between the two groups, while another study showed significant dysfunction in self care in depression.[9] The majority of bipolar patients had moderate impairment in interpersonal activities, but RDD patients had only mild impairment. Bipolar patients had more dysfunction in the area of communication and understanding than RDD patients. In the domain of work, bipolar patients were more impaired than RDD patients. These findings are in accordance with an earlier study by Chaudhury et al.,[9] where he found bipolar patients had dysfunction in all four domains.
The duration of illness had a significant influence on functional outcome; this was a finding which was not found significant in an early study by Rosen et al.[6] The patients with more number of psychotic episodes had more disability scores; this finding is consistent with earlier studies.[11] In this study, it was found that as duration of treatment increases, disability also increases, but this can be explained by the fact that patients with long duration of treatment in turn had more number of episodes and more duration of illness. The nil difference observed in disability among the patients with respect to their education and socioeconomic status, which is not consistent with earlier studies, can be attributed to the fact that patient population included in the study had no much difference in these two domains. It was found that as the total duration of illness increases, the impairment in areas of communication and work also increases in bipolar patients. The total number of episodes influenced the impairment in communication and understanding and in the areas of work. The total number of psychotic episodes adversely affected the self care and work.
To conclude, this study found that patients with mood disorder have significant disability even during the periods of remission, which is a finding consistent with earlier researches. The disability was more with the bipolar patients compared with RDD patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Geneva: World Health Organisation; 1980. International classification of impairment, disability and handicap (ICIDH) [Google Scholar]
- 2.Geneva: World Health Organisation; 2008. Global burden of disease 2004; p. 37. [Google Scholar]
- 3.Cooke RG, Robb JC, Young LT, Joffee RT. Well-being and functioning in patients with bipolar disorder assessed using the MOS 20-item short form (SF-20) J Affect Disord. 1996;39:93–7. doi: 10.1016/0165-0327(96)00016-x. [DOI] [PubMed] [Google Scholar]
- 4.Robb JC, Young LT, Cooke RG, Joffe RT. Gender differences in patients with bipolar disorder influence outcome in the medical outcomes survey (SF-20) subscale scores. J Affect Disord. 1998;49:189–93. doi: 10.1016/s0165-0327(98)00003-2. [DOI] [PubMed] [Google Scholar]
- 5.Tohen M, Hennen J, Zarate CA, Jr, Baldessarini RJ, Strakowski SM, Stoll AL, et al. The Mclean First Episode Project: Two-year syndromal and functional recovery in 219 cases of major affective disorders with psychotic features. Am J Psychiatry. 2000;157:220–8. doi: 10.1176/appi.ajp.157.2.220. [DOI] [PubMed] [Google Scholar]
- 6.Rosen LN, Rosenthal NE, Dunner DL, Fieve RR. Social outcome compared in psychotic and nonpsychotic bipolar I patients. J Nerv Ment Dis. 1983;l7I:272–5. doi: 10.1097/00005053-198305000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Strakowski SM, Keck PE, Jr, McElroy SL, West SA, Sax KW, Hawkins JM, et al. Twelve-month outcome after a first hospitalization for affective psychosis. Arch Gen Psychiatry. 1988;55:49–55. doi: 10.1001/archpsyc.55.1.49. [DOI] [PubMed] [Google Scholar]
- 8.Calabrese JR, Hirschfeld RM, Frye MA, Reed ML. Impact of depressive symptoms compared with manic symptoms in bipolar disorder: results of a U.S. community-based sample. J Clin Psychiatry. 2004;65:1499–504. doi: 10.4088/jcp.v65n1109. [DOI] [PubMed] [Google Scholar]
- 9.Chaudhury PK, Deka K, Chetia D. Disability associated with mental disorders. Indian J Psychiatry. 2006;48:95–101. doi: 10.4103/0019-5545.31597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fagiolini A, Kupfer DJ, Masalehdan A, Scott JA, Houck PR, Frank E. Functional impairment in the remission phase of bipolar disorder. Bipolar disord. 2005;7:281–5. doi: 10.1111/j.1399-5618.2005.00207.x. [DOI] [PubMed] [Google Scholar]
- 11.MacQueen GM, Young LT, Robb JC, Marriott M, Cooke RG, Joffe RT. Effect of number of episodes on wellbeing and functioning of patients with bipolar disorder. Acta Psychiatr Scand. 2000;101:374–381. doi: 10.1034/j.1600-0447.2000.101005374.x. [DOI] [PubMed] [Google Scholar]
- 12.Coryell W, Scheftner W, Keller M, Endicott J, Maser J, Klerman GL. The enduring psychosocial consequences of mania and depression. Am J Psychiatry. 1993;150:720–7. doi: 10.1176/ajp.150.5.720. [DOI] [PubMed] [Google Scholar]
- 13.Harrow M, Goldberg JF, Grossman LS, Meltzer HY. Outcome in manic disorders: a naturalistic follow-up study. Arch Gen Psychiatry. 1990;47:665–71. doi: 10.1001/archpsyc.1990.01810190065009. [DOI] [PubMed] [Google Scholar]
- 14.Indian Disability Assessment and Evaluation Scale. Rehabilitation committee of Indian Psychiatric Society. 2000 Dec [Google Scholar]
- 15.Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res. 2000;42:241–7. doi: 10.1016/s0920-9964(99)00130-9. [DOI] [PubMed] [Google Scholar]
- 16.Gershon ES, Guroff JJ. Information from relatives diagnosis of affective disorders. Arch Gen Psychiatry. 1984;41:173–80. doi: 10.1001/archpsyc.1984.01790130069010. [DOI] [PubMed] [Google Scholar]
- 17.Tharoor H, Chauhan A, Sharma PS. A cross-sectional comparison of disability and quality of life in euthymic patients with bipolar affective or recurrent depressive disorder with and without comorbid chronic medical illness. Indian J Psychiatry. 2008;50:24–9. doi: 10.4103/0019-5545.39755. [DOI] [PMC free article] [PubMed] [Google Scholar]


