Abstract
Pyoderma gangrenosum(PG) is a rare ulcerating inflammatory neutrophilic dermatosis. Genital involvement has been rarely reported. We report such a case of 24- year- old, male patient living with HIV/AIDS(PLHIV) who presented with progressive genital ulceration, not responding to oral antibiotics and aciclovir, gradually increasing in size over 15-18 months. Repeated biopsies showed acute on chronic inflammation. The lesion partially responded to oral and topical corticosteroids but soon increased in size after tapering the dosage of the steroids.Then patient was given Imiquimod 5% cream to be applied over the lesion once daily for 2-4 weeks. Lesion cleared completely in 4 weeks and is in remission since last 6 months. The case report highlights the successful use of topical Imiquimod 5% cream in the treatment of penile PG.
Keywords: Imiquimod, penile pyoderma gangrenosum
INTRODUCTION
Pyoderma gangrenosum (PG) is a rare, non-infectious neutrophilic dermatosis. The annual incidence of PG in the United States is approximately 1 case per 100,000 people.[1] The diagnosis of genital PG is one of exclusion, with penile lesions having a substantial differential diagnosis including infections like syphilis, herpes simplex, mycobacterial ulceration, amoebiasis and non-infectious causes of genital ulceration like squamous cell carcinoma, cutaneous crohn's disease, ulcerating sarcoidosis. PG should be suspected in any patient with ulcerative penile lesion(s) who fails to respond to adequate antibacterial or antiviral therapy and who has a negative or non-confirmatory diagnostic evaluation for infectious or other inflammatory conditions. There are very few cases of penile PG reported in patients with HIV/AIDS.[2] This is the first report of use of Imiquimod in the treatment of PG.
CASE REPORT
A 24- year- old, unmarried male PLHIV, presented with painless genital ulcer gradually increasing in size for 15–18 months. The patient had a history of paid, unprotected heterosexual exposure 6 months before the onset of the lesion. On examination, the lesion had well-defined edges, irregular border, verrucous surface and a granulomatous base with serous discharge [Figure 1] inguinal lymphadenopathy was absent.The patient was taking anti-tubercular therapy (ATT) since 4 months for scrofuloderma over neck. Complete blood count was 7200/mm3, erythrocyte sedimentation rate was 25 after 1 h and 40 after 2 h. Chest radiograph was normal. Tzanck smear and Gram stain prepared from the ulcer were negative. Local tissue culture was also negative.Histopathologic examination from the ulcer edge showed nonspecific inflammation with eosinophilic infiltrate [Figure 2] Biopsy was repeated three times to rule out sexually transmitted disease and malignancy. Histopathology every time showed acute on chronic inflammation without any specific changes.
Figure 1.

Single, well-defined erosion with granulation tissue and elevated edges on the undersurface of shaft of penis
Figure 2.
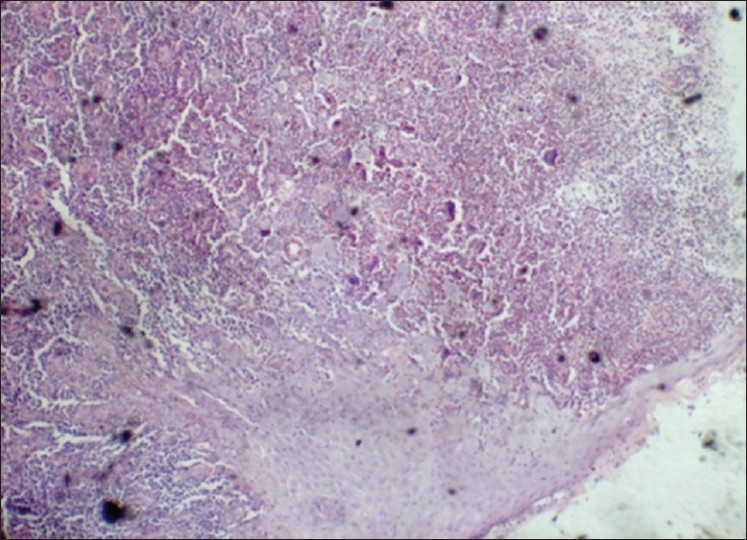
Histopathology suggestive of nonspecific chronic inflammation and ulceration of squamous mucosa, 4× low-power view
The Patient is S. HIV-1 Reactive. Patient's CD4 progression is 204/mm3 on 13/6/2008, 582 on 23/12/2008, 354 on 30/6/2009, 216 on 18/12/2009, 257 on 14/6/2010, 358 on 18/12/2010.
Serum rapid plasmareagin and serum treponema pallidum haemagglutination assay were negative. Type specific IgM and IgG antibody against both HSV-1 and HSV-2 were absent.
Currently, the patient is on antiretroviral therapy(ART). He was on first-line ART regimen of Zidovudine(ZDV)+Lamivudine(3TC)+Efavirenz(EFV) on 30/6/2008. He was started on EFV-based regimen as he was on concurrent ATT chemotherapy for scrofuloderma. After ATT completion, the patient was shifted to Nevirapine(NVP)-based regimen on 23/12/2008.
The patient was given presumptive treatment for the granuloma inguinale with Cap. Doxycycline 100 mg twice a day for 4 weeks but lesion did not show any improvement. He was also given Inj. Benzathine Penicillin 2.4 MU every week for 3 weeks without any response and tab. aciclovir 400mg 3 times a day but the lesion did not show any improvement and it continued to increase in the size. Initial size of lesion was 2×1cm in size which progressed to 6×10 cm in size over 10 months [Figure 3]. Then, the patient was put on oral tab. Prednisolone 30mg in the mornings with milk for 14 days and then tapered 5 mg every week. The lesion initially showed improvement but lesions soon started increasing in size on tapering the doses [Figure 4]. Finally, diagnosis of PG was made and the patient was asked to apply imiquimod 5% cream once a day for 4 weeks. The lesion started clearing within first 2 weeks and it was completely healed after 3 weeks of application and the patient is in remission since last 6 months without any medication [Figure 5].
Figure 3.

Lesion increased in size upto 8 × 10 cm failing to respond to therapies for conventional sexually transmitted diseases
Figure 4.

Partial response after therapy with Tab. Prednisolone
Figure 5.

Complete epithelization after 4 week topical application of 5% Imiquimod
In this case, it is possible that repeated biopsy elicited the pathergic response. Differential diagnosis of genital erosion in PLHIV is enormous but possibility of PG should always be kept in mind to avoid unnecessary surgical trauma and debridement.
DISCUSSION
PG is a rare, non-infectious neutrophilic dermatosis commonly associated with underlying systemic disease most often affecting the lower extremities but may involve the face, neck, scrotum or penis.-[2,3] Pathogenesis of PG is not fully understood, an immune-mediated process is thought to have an important role.[4,5] Penile PG may occur following local trauma, such as urological surgery or treatment for cancer, or complicate ulcerative colitis or chronic lymphocytic leukaemia, or it may be idiopathic.
Diagnosis is based on typical clinical features and exclusion of other cutaneous ulcerating diseases, as described in several reviews.[6–9] Although the histopathological findings of PG are often variable and non-specific, they can be useful in excluding other possible aetiologies.[10]
Penile PG represent one of the classic ulcerative pyoderma gangrenosum or superficial granulomatous pyoderma.[11]
Early recognition is critical in order to avoid unnecessary or potentially harmful interventions. The extension of lesions in response to trauma or surgical debridement, termed pathergy,is a hallmark of PG.[12] We present a case of penile PG as a reminder that, although PG of the penis is rare, a progressive, non-healing painful penile lesion with negative laboratory and histopathological evaluations should prompt the consideration of this entity.
Penile PG being present in PLHIV poses two important challenges:(1) differential diagnosis of genital ulceration in PLHIV is wide, including various sexually transmitted infections, tropical ulcers, mycobacterial, amoebic, deep fungal, aphae, drug-induced and malignancy. Complete diagnostic workup to exclude all the above possible causes is a must in order to establish the diagnosis. (2) Management of penile PG is also difficult in the PLHIV as these patients are more likely to develop potential adverse effects of the immunosuppressive agents.
Topical and systemic corticosteroids only gave partial control in this case and patient being PLHIV long term use of corticosteroids and other immunosuppressive agents is prohibited. Topical tacrolimus did not work in the present case.[13]
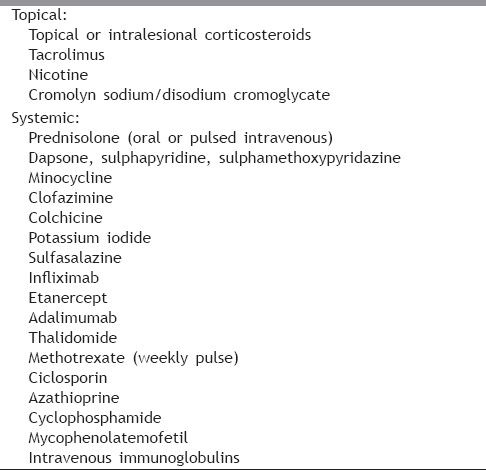
Thus, topical Imiquimod 5% cream with its immunomodulating properties could be a feasible choice for management of such patients. Choice of treatment generally depends on disease severity as well as on the presence of associated disease. For early or mild lesions, topical therapy may be sufficient. For more severe disease, or for PG resistant to topical therapy, oral corticosteroids have been the mainstay of therapy. [Table 1].Treatment of PG is usually discontinued after complete healing of lesions. Recurrences may occur but are unpredictable and therefore do not justify prolonged maintenance therapy.[14]
Table 1.
Treatment ladder for pyodermagangrenosum
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Gonzalgo ML, de Lacerda DA, De Marzo AM, Chan DY. Persistent purulent drainage from the glans penis: Atypical presentation of pyoderma gangrenosum. J Urol. 2003;169:1793–4. doi: 10.1097/01.ju.0000057721.16493.21. [DOI] [PubMed] [Google Scholar]
- 2.Ecra E, Ahogo KC, Sangaré A, Kaloga M, Kassi K, Kouamé K, et al. An uncommon localization of pyoderma gangrenosum on the penis of an HIV infected patient in the Ivory Coast] Bull Soc Pathol Exot. 2009;102:85–7. [PubMed] [Google Scholar]
- 3.Park HJ, Kim YC, Cinn YW, Yoon TY. Granulomatous pyoderma gangrenosum: Two unusual cases showing necrotizing granulomatous inflammation. Clin Exp Dermatol. 2000;25:617–20. doi: 10.1046/j.1365-2230.2000.00721.x. [DOI] [PubMed] [Google Scholar]
- 4.Jackson JM, Callen JP. Pyoderma gangrenosum: An expert commentary. Expert Rev Dermatol. 2006;1:391–400. [Google Scholar]
- 5.Wollina U. Pyoderma gangrenosum: A review. Orphanet J Rare Dis. 2007;2:19. doi: 10.1186/1750-1172-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Powell FC, Su WP. Pyoderma gangrenosum: Classification and management. J Am AcadDermatol. 1996;34:395–409. doi: 10.1016/s0190-9622(96)90428-4. [DOI] [PubMed] [Google Scholar]
- 7.Powell FC, Collins C. Pyoderma gangrenosum. Clin Dermatol. 2000;18:283–93. doi: 10.1016/s0738-081x(99)00119-4. [DOI] [PubMed] [Google Scholar]
- 8.Ahmadi S, Powell FC. Pyoderma gangrenosum: Uncommon presentations. Clin Dermatol. 2005;23:612–20. doi: 10.1016/j.clindermatol.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 9.Provost TT, Harris ML. Pyoderma gangrenosum. In: Provost TT, Flynn Ja, editors. Cutaneous Medicine: Cutaneous Manifestations of Systemic Disease. Hamilton, Ontario: Decker; 2001. pp. 464–72. [Google Scholar]
- 10.Su WP, Schroeter AL, Perry HO, Powell FC. Histopathologic and immunopathologic study of pyoderma gangrenosum. J Cutan Pathol. 1996;13:323–30. doi: 10.1111/j.1600-0560.1986.tb00466.x. [DOI] [PubMed] [Google Scholar]
- 11.Wilson-Jones E, Winkelmann RK. Superficial granulomatous pyoderma: A localized vegetative form of pyoderma gangrenosum. J Am Acad Dermatol. 1988;18:511–21. doi: 10.1016/s0190-9622(88)70074-2. [DOI] [PubMed] [Google Scholar]
- 12.Lee DK, Hinshaw M, Cripps D, Jarrard DF. Pyoderma gangrenosum of penis. J Urol. 2003;170:185–6. doi: 10.1097/01.ju.0000070820.91387.55. [DOI] [PubMed] [Google Scholar]
- 13.Petering H, Kiehl P, Breuer C, Kapp A, Werfel T. Pyoderma gangrenosum: Successful topical therapy with tacrolimus (FK506) Hautarzt. 2001;52:47–50. doi: 10.1007/s001050051261. [DOI] [PubMed] [Google Scholar]
- 14.Chow RK, Ho VC. Treatment of pyoderma gangrenosum. J Am Acad Dermatol. 1996;34:1047–60. doi: 10.1016/s0190-9622(96)90285-6. [DOI] [PubMed] [Google Scholar]


