Abstract
Objectives:
The present study was undertaken to determine the prevalence of respiratory, gastrointestinal and other pathogens in 100 Human Immunodeficiency Virus (HIV) seropositive patients.
Settings:
This study was carried out on randomly selected 100 HIV seropositive patients from S. S. G. Hospital during the period from Jan 2006 to Jan 2007.
Materials and Methods:
Sputum samples, stool samples and oral swabs were collected from all the patients and cerebrospinal fluid (CSF) was collected from symptomatic patients and processed as per the standard protocol. Sputum samples were examined by microscopy and cultured for bacterial respiratory pathogens. Stool samples were concentrated and examined by microscopy for enteric parasites. Oral swabs and CSF were also examined microscopically and cultured for fungal pathogens. CSF was also examined for bacterial pathogens.
Results:
A total of 101 pathogens were detected in 60 patients. More than one pathogen was observed in 30 patients. Candida was the commonest isolate (32.67%), followed by Mycobacterium tuberculosis (22.71%) and Cryptosporidium parvum (19.8%).
Conclusions:
Since opportunistic infections are a major cause of mortality and morbidity in HIV seropositive patients, an early diagnosis and effective treatment are required to tackle them. The type of pathogens infecting HIV patients varies from region to region, and therefore such patients should be constantly screened for these pathogens.
Keywords: Candidiasis, cryptosporidiosis, HIV, tuberculosis
INTRODUCTION
Human Immunodeficiency Virus (HIV) is the most devastating plague facing us as the 21st century begins. In India, nearly 22.7 lakh people are living with HIV infection. The magnitude of the infection is second only to that of South Africa.[1] Progressive destruction of immune system by chronic HIV infection leading to progressive fall in the level of CD4 cells (<200/μl to <50 / μl) is known to be responsible for the occurrence of infections by a variety of opportunistic microorganisms.[2] This is also responsible for the recurrent, prolonged, intractable and severe nature of infection in HIV seropositive individuals.[3] Knowledge of the pattern of opportunistic infections can often guide therapy when resource limitations hamper the exact diagnosis of the etiological agent.[4] HIV/AIDS may not be curable but most of the opportunistic infections can be effectively treated. Prophylaxis against some of these infections will not only prolong the life of an HIV infected individual but also improve the quality of life. National AIDS Control Organization (NACO) data reveal that tuberculosis is the commonest infection in AIDS patients, followed by candidiasis, cryptosporidiosis and others.[5] Prevalence of different opportunistic infections is different in different geographical regions.[3] Considering this fact, the present study was conducted to determine the prevalence of bacterial, parasitic, fungal infections in HIV seropositive patients.
MATERIALS AND METHODS
The present study was carried out on 100 HIV seropositive patients in Department of Microbiology, S. S. G. Hospital, Vadodara, during the period from Jan 2006 to Jan 2007.
Eligibility criteria
Randomly selected 100 HIV seroreactive patients from in-patients and out-patients department of the hospital were included. Written consent was obtained from all the participants to be included in the study.
Their HIV status was confirmed by three tests with different principles/antigens (Enzaids ELISA, i.e. enzyme-linked immunosorbent assay, Combaids-RS, HIV Tridot) in the Integrated Counselling and Testing Centre attached to the department as per NACO guidelines.[6] Antibodies against immunodominant regions of HIV 1 (gp 120, gp 41) and HIV 2 (gp 36) and p24 antigens were detected. Necessary pre and post-test counseling of the patients was carried out and detailed history was taken.[6] Sputum samples, stool samples, oral swabs and cerebrospinal fluid (CSF) from patients were collected taking all aseptic precautions.[5]
Stool samples were processed for the investigation of parasitic pathogens. Parasite detection was done as per the standard protocol. Direct wet mount preparation (saline and iodine) and wet preparation from formal ether concentrated samples were used for the detection of protozoan trophozoites, cysts and helminthic eggs and larva. For the detection of coccidian parasites, smears of stool samples were prepared and stained with modified acid fast method.[5,7]
Early morning expectorated sputum samples were collected in sterile containers. For the detection of bacterial pathogens, samples were processed for Gram's stain, Zeihl and Nelson (ZN) stain and aerobic culture on selective and enrichment media (Lowenstein Jenson media, Chocolate agar, Macconkey agar) as per the standard methods. The bacterial isolates were identified using standard microbiological techniques.[5,8]
Two oral swabs were taken from each of the 100 patients. One swab was used for wet mount (10% KOH, i.e. potassium hydroxide) and Gram stain. The other swab was inoculated on Sabouraud's Dextrose Agar (SDA) with antibiotics. The growth obtained was identified for yeasts as per the standard protocol including germ tube test, chlamydospore formation, sugar assimilation, sugar fermentation and urease test.[5,9]
CSF samples from patients of meningitis were collected. India ink preparation, wet mount, Gram stain and culture on SDA, Chocolate agar and Macconkey agar were carried out in CSF samples. The growth obtained on SDA was identified for yeast as per the standard protocol.[5,9] No bacterial pathogens were isolated from CSF samples.
RESULTS
Out of the total 100 patients in the study, majority were males (75%, 75/100). Remaining 25% (25/100) were females. In the present study, the preponderant age group affected from HIV was 20-29 years (61%, 61/100). Heterosexual contact (94%, 94/100) was the leading cause of HIV transmission. Other routes included homosexual contact (1%, 1/100), blood transfusion (3%, 3/100) and vertical transmission (2%, 2/100).
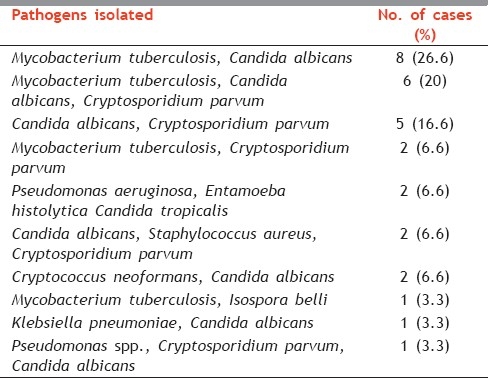
Symptomatic presentation of patients is shown in Table 1. Fever, cough, weight loss, diarrhea and oral thrush were the most common symptoms. Totally, 101 pathogens were identified from 60 patients. The microbial profile is shown in Table 2. Candida (32.67%, 32/101) was the commonest pathogen identified, followed by Mycobacterium tuberculosis (22.77%, 23/101) and Cryptosporidium parvum (19.8%, 20/101). Out of the four patients who presented with meningitis, Cryptococcus neoformans was isolated in two patients and in the remaining two patients no fungal pathogen was identified. More than one pathogen was identified in 30 patients. Their polymicrobial profile is shown in Table 3.
Table 1.
Clinical presentation of study population
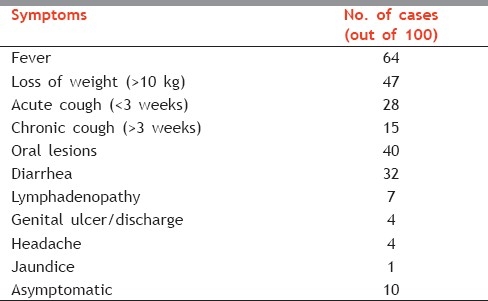
Table 2.
Microbial profile of HIV seropositive patients
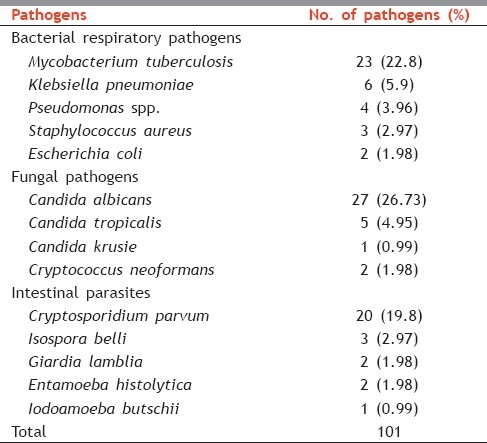
Table 3.
Polymicrobial profile of HIV seropositive patients (n=30)
DISCUSSION
In the present study, out of 100 patients, majority were in the reproductive age group, i.e. 20–29 years (61%, 61/100), with a male preponderance (75%, 75/100). Rangnathan and his colleagues reported 77.4% male patients with 81% patients in the age group of 21–40 years in their study done at South India.[10] Bhagyawatidevi et al. reported the highest number of HIV patients to be in the age group of 21–30 years (63%) with majority of male patients (94%) in their study done at Manipur.[11] Majority of the patients in the study group were laborers (42%), followed by truck drivers (18%). Majority of them were migrants staying away from home, thereby increasing the risk of HIV infection. Heterosexual contact (95%) was the commonest route of transmission in our study which correlates well with other studies. More than 80% rate of heterosexual transmission was reported by NACO (87.1%) and Rangnathan (95%).[1,10] In the present study, majority of patients had more than one symptom and 27% patients had multiple system involvement. Fever and weight loss were the predominant symptoms, followed by cough, oral lesions and diarrhea. The clinical profile reported in the present study was similar to that reported in Lucknow by Ayyagari et al.[3] and in Amritsar by Aruna Aggarwal et al.[12] Polymicrobial etiology in 30 of the HIV reactive patients is a significant finding, indicating severity of the infection in this group.
In the present study, 43% (43/100) patients had respiratory tract infections. Diseases like bacterial pneumonia occur at a rate many times higher in the HIV infected population than in the general population.[3] M. tuberculosis (60.5%, 23/38) was the commonest organism among the bacterial respiratory pathogens, followed by Klebsiella pneumoniae (15.7%, 6/38), Pseudomonas aeruginosa (10.5%, 4/38), Staphylococcus aureus (7.8%, 3/38) and Escherichia coli (1.9%, 2/38). Aruna Aggarwal et al. in their study at Amritsar reported M. tuberculosis (32.75%) as the commonest bacterial respiratory pathogen, followed by Klebsiella spp. (23.8%), P. aeruginosa (12.69%) and S. aureus (12.69%).[12] Shailja et al. reported M. tuberculosis (28%), followed by K. pneumoniae (10%), Streptococcus pneumoniae (8%) and S. aureus (4%).[13] This difference may be due to geographical differences and also possible hospital acquired superadded infections.
Oral lesions were present in 40% (40/100) of patients in the present study. Out of 33 isolates from oral lesions, 27 were Candida albicans (81.8%) and 6 were non-albicans Candida spp. (18.2%). This finding correlates well with the report of Baradkar et al. on their study carried out at Aurangabad (C. albicans 76.92%, Candida spp. 23.08%).[14] Oral and esophageal candidiasis (57.5%) is reported as the second most common opportunistic infection among HIV patients from India.[15] Crypto. neoformans was isolated from two out of four patients of meningitis in our study. It is the second most common fungal infection and the fourth commonest cause of life-threatening illness in AIDS patients in India. Aruna Aggarwal et al. also found Crypto. neoformans in 2 out of 3 patients of meningitis.[13] Singh et al. reported 7% rate of cryptococcal meningitis in their study done at Manipal.[16] An incidence of 3% of cryptococcal meningitis has been reported in HIV infected patients in India.[5]
In the present study, 32 patients suffered from diarrhea. Cryptos. parvum (71.4%, 20/28) was the commonest parasite found, followed by Isospora belli (10.7%, 3/28), Giardia lamblia (7.1%, 2/28) and Entamoeba histolytica (7.1%, 2/28). Cryptos. parvum was reported as the most common enteric parasite by Aruna Aggarwal (51.42%) and Singh (43%).[13,15] I. belli was found as the commonest parasite by Gupta at Jamnagar (17.24%) and Kumar at Chennai (18%).[4,17] Differences in the incidence of intestinal parasitic infections can be attributed to the differences in geographical distribution of parasites, sanitary practices and different selection of cases.
CONCLUSION
It is concluded that oral candidiasis, pulmonary tuberculosis and cryptosporidiosis are the commonest opportunistic infections in the HIV seropositive patients in the present study group. Improved hygienic practices, regular examination and appropriate antimicrobial prophylaxis can reduce the substantial morbidity and mortality caused by opportunistic infections in patients with HIV infections. With better knowledge and diagnosis of the opportunistic infections, clinicians and health planners can treat HIV patients more effectively. This will contribute to increased life expectancy among HIV seropositive patients.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Annual Report 2009-2010 by Department of AIDS Control, Ministry of Health and Family Welfare, National AIDS Control Organization, Government of India. Page No. 1. [last updated on 2010 Mar 22, Last accessed on 2010 Dec 22]. Available from: http://www.nacoonline.org.
- 2.Mukhopadhya A, Ramakrishna BS, Kang G, Pulimood AB, Mathan MM, Zachariah A, et al. Enteric pathogens in southern Indian HIV infected patients with and without diarrhoea. Indian J Med Res. 1999;109:85–9. [PubMed] [Google Scholar]
- 3.Ayyagiri A, Sharma AK, Prasad KN. Spectrum of opportunistic infections in Human Immunodeficiency Virus infected cases in a tertiary care hospital. Indian J Med Microbiol. 1999;17:78–80. [Google Scholar]
- 4.Gupta M, Sinha M, Raizada N. Opprtunistic Intestinal protozoan parasitic infection in HIV seropositive patient in Jamnagar, Gujarat SAARC Journal of Tuberculosis Lung diseases & HIV/AIDS. 2008;V(1):22–5. [Google Scholar]
- 5.Baveja UK, Sokhey J. National Institute of Communicable Disease and National AIDS Control Organisation. 2001. Feb, Manual on laboratory diagnosis of common opportunistic infections associated with HIV/AIDS. [Google Scholar]
- 6.HIV testing Manual on Laboratory Diagnosis, Bio safety and Quality Control by NICD and NACO. 2007 Feb [Google Scholar]
- 7.Gracia LS. Laboratory methods for the diagnosis of parasitic infections. In: Forbes Ba, Soham DF, Weissfild AS., editors. Bailey and Scott's Diagnostic Microbiology. 11th ed. Louis: Mosby Inc; 2002. pp. 604–709. [Google Scholar]
- 8.Collee JG, Miles RS, Laidlaw M. 13th ed. UK: Churchil Livingstone; 1989. Test for Identification of Bacteria; Mycobacterium Tubercle Bacilli In: Mackie and Mc Cartney Practical Medical Microbiology; pp. 141–60. (399, 416). [Google Scholar]
- 9.Hyderabad: Department of Microbiology, Nizam's Institute of Medical Sciences and Global Hospitals; 2006. Manual of Medical Mycology, VI National Conference of Society for Indian Human and animal Mycology; pp. 47–53. [Google Scholar]
- 10.Ranganathan K, Umadevi M, Saraswathi TR, Kumarasamy N, Solomon S, Johnson N. Oral lesions and conditions associated with Human Immunodeficiency Virus infection in 1000 South Indian Patients. Ann Acad Med Singapore. 2004;33(4):375–425. [PubMed] [Google Scholar]
- 11.Devi SB, Naorem S, Singh TJ, Singh KB, Prasad L, Devi TS. HIV and TB Co- infection A Study from RIMS Hospital, Manipur. J Indian Acad Clin Med. 2005;6:220–3. [Google Scholar]
- 12.Aggarwal A, Arora U, Bajaj R, Kumari K. Clinicomicrobiological study in HIV seropositive patients. J Indian Acad Clin Med. 2005;6:142–5. [Google Scholar]
- 13.Shailaja VV, Pai LA, Mathur DR, Lakshmi V. Prevalance of Bacterial and Fungal agents causing lower respiratory tract infections in patients with human immunodeficiency virus infection. Indian J Med Microbiol. 2004;22:28–33. [PubMed] [Google Scholar]
- 14.Baradkar VP, Karyakarte RP. Isolation and characterization of Candida species in Acquired Immuno Deficiency Syndrome. Indian J Med Microbiol. 1999;17:42–4. [Google Scholar]
- 15.Guidelines for Prevention and Management of Common Opportunistic Infections/Malignancy in HIV Infected Adult/ Adolscent by Department of AIDS Control, Ministry of Health and Family Welfare, National AIDS Control Organization, Government of India. Page No. 5. [last updated on 2010 Mar 22, Last accessed on 2010 Dec 22]. Available from: http://www.nacoonline.org .
- 16.Singh A, Bairy I, Shivananda PG. Spctrum of opportunistic infections in AIDS cases. Indian J Med Microbiol. 2003;57:16–21. [PubMed] [Google Scholar]
- 17.Kumar SS, Ananthan S, Lakshmi P. Intestinal parasitic infections in HIV infected patients with diarrhoea in Chennai. Indian J Med Microbiol. 2002;20:88–91. [PubMed] [Google Scholar]


