Abstract
Background:
Left ventricular hypertrophy (LVH) is an independent cardiac risk factor in hypertensives and the structural classification of left ventricular (LV) geometry provides additional prognostic information. Ambulatory blood pressure (ABP) monitoring has been shown to be superior to office blood pressure (BP) in relation to hypertension LVH. We investigated ambulatory BP variables in relation to LV geometric patterns in Nigerian hypertensives.
Materials and Methods:
A total of 130 patients (males = 96, females = 34) with hypertension had their 24-hours ambulatory BP and trans-thoracic 2D/M- mode echocardiography. Data were analyzed with SPSS 13.0. P < 0.05 was considered statistically significant.
Results:
The mean age of the patients was 54.08±11.88 years. The prevalence rate of abnormal LV geometry was 48.4%. Mean ambulatory Systolic BP (day time, night time and 24-hour-average) was significantly higher in patients with LVH compared with those without LVH. Day-night systolic and diastolic BP decay (i.e. percentage nocturnal decline in BP) was also significantly lower in LVH group than in the group without LVH. Patients with eccentric LVH had abnormal day time mean ambulatory systolic BP, night time mean ambulatory systolic BP, elevated day time and night time systolic BP loads, as well as non-dipping diastolic BP pattern. Significant correlates of LV mass index in this study population were mean ambulatory systolic BP (day time: r = 0.355, P = 0.004; night time: r = 0.343, P = 0.005; 24- hour average: r = 0.358, P = 0.004) and day-night decay (systolic: r = -0.388, P = 0.007; diastolic: r = -0.290, P = 0.022) as well as 24-hour systolic BP variability.
Conclusion:
The presence of LVH in hypertension was associated with higher mean ambulatory systolic BP and lower percentage nocturnal decline in systolic and diastolic BP than its absence which appeared to be worse in patients with eccentric LV geometry when compared with other geometric patterns.
Keywords: Ambulatory blood pressure, left ventricular geometry, hypertensives, Nigerians
INTRODUCTION
Ambulatory blood pressure (ABP) monitoring has been shown to be superior to office blood pressure (BP) in relation to hypertension target organ damage.[1] A large number of studies, mostly among white population, have been investigated - on a cross-sectional basis, the organ damage accompanying hypertension is more closely related to 24-hour average than to office BP. The results have almost invariably shown this to be the case regardless of whether the damage is quantified in the heart (LVH or dysfunction), in the kidney (proteinuria), in the brain (cerebral lacunae or white matter lesions as identified by nuclear magnetic resonance), in the small and large arteries, or by a comprehensive organ damage score.[2,3]
In addition to left ventricular hypertrophy (LVH), which has been widely documented to be an independent cardiac risk factor in both the general population and hypertensive patients,[4,5] the structural classification of LV geometry also provides useful and additional prognostic information.[6–8]
Though some authors have described LV geometric patterns in newly presenting hypertensive patients in Nigerian population,[9] no studies, to the best of our knowledge had investigated ABP variables in relation to LV geometric patterns in Nigerian hypertensive. This study, therefore sought to determine the relationship between ABP and LV geometric patterns in Nigerian hypertensive patients.
MATERIALS AND METHODS
The study population consisted of 130 patients (males = 96, females = 34) with hypertension (mean age 54.08±11.88 years) consecutively selected from those who were referred to the cardiac laboratory of Tender heart Specialist Clinic, Akure, Southwest Nigeria for non-invasive cardiac assessment. Ethical clearance for the study was approved by the Ethics and Research Committee of the University Teaching Hospital Ado Ekiti which the laboratory serves and all the participants gave written consent to participate in the study. Demographic parameters of subjects were noted and recorded. All subjects were clinically examined to evaluate their body mass index (BMI) and cardiovascular status. They were considered hypertensive if they had a resting systolic blood pressure (SBP) >140mmHg and/or diastolic blood pressure (DBP) > 90mmHg measured after at least 15 minutes of rest in the sitting position with a mercury sphygmomanometer and adapted cuff at the brachial artery or if they were on antihypertensive therapy.[10] Korotkoff phase 1 was used for SBP and phase 5 for DBP. Three consecutive measurements were performed at 5-min intervals and the mean values for SBP and DBP were noted as office SBP and DBP, respectively. Excluded were patients with established chronic renal failure (CRF) or serum creatinine >1.5mg% (132 umol/L), ischemic heart disease, congestive heart failure, valvular heart disease, hemoglobinipathy and diabetes mellitus.
Ambulatory BP monitoring
Ambulatory BP was recorded using Schiller BR 102- Plus. The cuff was fixed to the non-dominant arm and the device was set to obtain automatic BP readings at 15-min intervals during the day time and at 30-min intervals during the night-time. The patient was then sent home with instructions to perform his or her usual activities, to hold the arm immobile at the time of the measurements, note on a diary the occurrence of any unusual events, and return 24-h later for device removal. Day time and night time periods were defined individually according to the patient self-reported data of going-to-bed and getting-up times. Interpretation of ABP profile was done according to the recommendations of the British Hypertension Society.[11] Percentage nocturnal BP decline was defined by calculating the percentage of decline in both SBP and DBP during the night, using the following formula: (day time BP-night time BP)/day time BP × 100. A normal dipping pattern (dipper) was diagnosed when the reduction in the average SBP during the night period was >10% of mean SBP during the day. An abnormal dipper pattern (non-dipper) was diagnosed when the night average SBP reduction was <10% with respect to day values.[12]
SBP and DBP loads in the entire 24-h and separately for the day time and night time were calculated. Day time and night time BP loads were calculated using a threshold of 140/90mmHg and 120/80mmHg respectively.[13] The individual loads are the percentage of elevated readings during each time period. SBP and DBP variability was assessed as the standard deviation of the mean (co-efficient of variation) of 24-hour ambulatory SBP and DBP recordings.
Echocardiography assessment
All the patients had transthoracic 2D and 2D-derived M-mode echocardiography performed according to standard procedure, with simultaneous electrocardiographic recordings while in the left lateral decubitus position using a standard ultrasound machine (Philips SONOS 4500) with S3 transducer of frequency 3-1MHZ. LV end-diastolic measurements were taken during at least three cycles[14] and included LV internal diameter (LVIDD), posterior wall thickness (PWT) and interventricular septal thickness (IVST). Left ventricular mass index (LVMI) was estimated from the American Society of e0 chocardiographic f0 ormula (14) as stated below:
Estimated LVMI (g/m2) = 0.80 [1.04 (LVIDD + PWT + IVST)3 - (LVIDD)3 ] + 0.6g/BSA.
Upper normal limits for LV mass index were 134 and 110 g/m2 in men and women.[15] Relative wall thickness (2 × posterior wall thickness/LV diastolic diameter) was calculated.[16] A partition value of 0.45 for relative wall thickness was used for both men and women.[17] Patients with increased LV mass index and increased relative wall thickness were considered to have concentric hypertrophy, and those with increased LV mass index and normal relative wall thickness were considered to have eccentric hypertrophy. Those with normal LV mass index and increased or normal relative wall thickness were considered to have concentric remodeling or normal geometry, respectively.
Statistical analysis
Data are expressed as mean±SD and frequency as a percentage. Significant differences of the studied parameters between the four groups of LV geometry were determined by use of the analysis of variance (ANOVA). Multiple comparisons between the 4 groups were performed by one –way analysis of variance with the Tukey and Tamhane post hoc test. Student t test was used to compare two groups. Pearson's correlation was used to investigate the correlation of variable factors.
All statistical analyses were performed with commercially available computer program SPSS 13.0 (SPSS Inc., Chicago, IL). P < 0.05 was considered statistically significant.
RESULTS
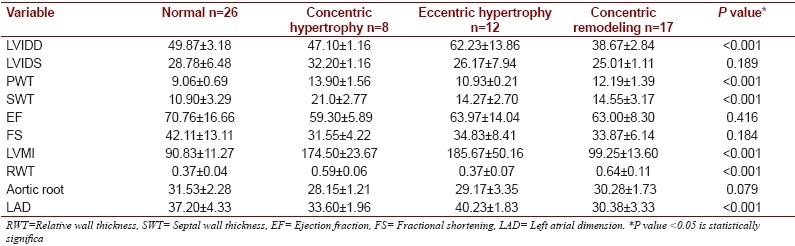
A total of 130 patients with a mean age of 54.08±11.88 years (range 31 -85 years) comprising 96 males and 34 females were studied. Sixty seven (51.5%) of the patients were on anti-hypertensive medications consisting mostly of calcium channel blockers, angiotensin receptor blockers/ angiotensin converting enzyme inhibitors and thiazide diuretics. Figures 1 and 2 show the patterns of LV geometry in the study population in general and treatment groups, respectively. Sixty eight (51.6%) of the patients had normal LV geometry, 38 (29%) had LV concentric remodeling, 12 (9.7%) had LV concentric hypertrophy and 12 (9.7%) had LV eccentric hypertrophy. Clinical and demographic characteristics of the patients with respect to geometric patterns in the study population and the subgroup of patients who were not on anti-hypertensive drugs are shown in Tables 1a and 1b, respectively. There were no significant differences in sex, weight, height, and body surface area (BSA). The patients with eccentric LV geometry were older and had significantly higher office SBP compared to those with normal LV geometry, LV concentric geometry and LV concentric remodeling. Echocardiographic parameters of the different groups are shown in Tables 2a and 2b. There were no significant differences in the echocardiographic LV systolic function indices of ejection fraction and fractional shortening. There was no significant difference in left atrial dimension and aortic root dimension between the groups, in the study population. However, patients with eccentric LV geometric pattern who were found only in those who were not on antihypertensive medications had significantly higher left atrial dimension than other forms of LV geometric pattern.
Figure 1.
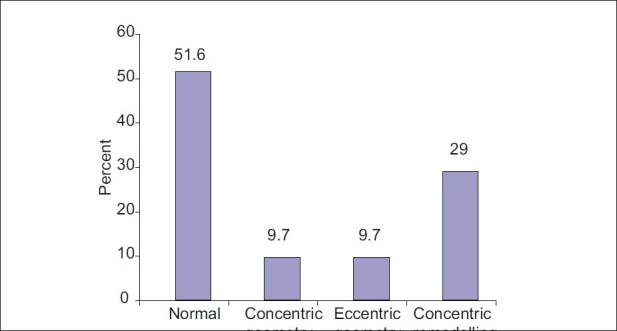
Left ventricular geometric pattern in the study population
Figure 2.
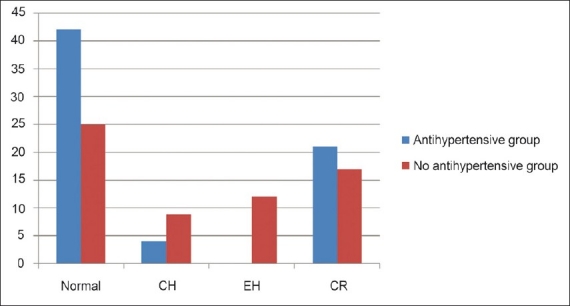
Left ventricular geometric pattern in patients on antihypertensive vs. no antihypertensive medications
Table 1a.
Demographic characterristics of different geometric patterns in the study population
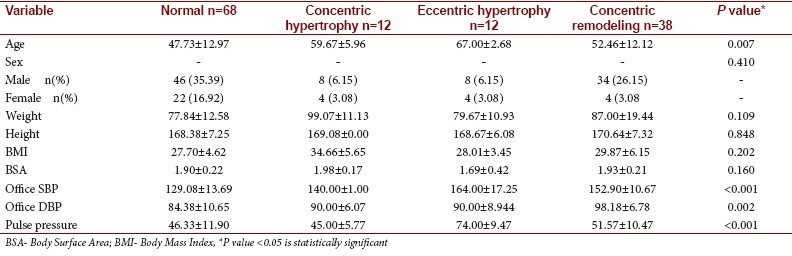
Table 1b.
Demographic characterristics of different geometric patterns in untreated hypertensives
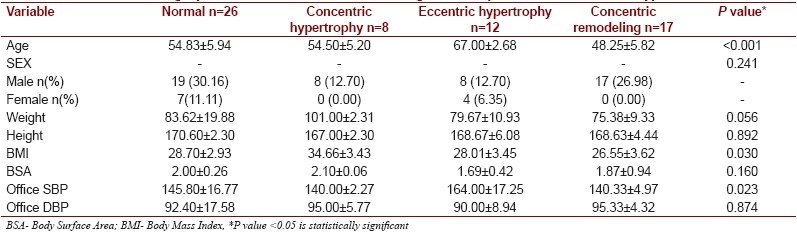
Table 2a.
Echocardiographic characteristics of different geometric patterns in the study population
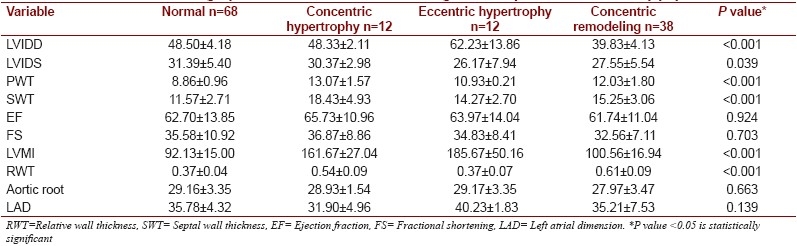
Table 2b.
Echocardiographic characteristics of different geometric patterns in untreated hypertensives
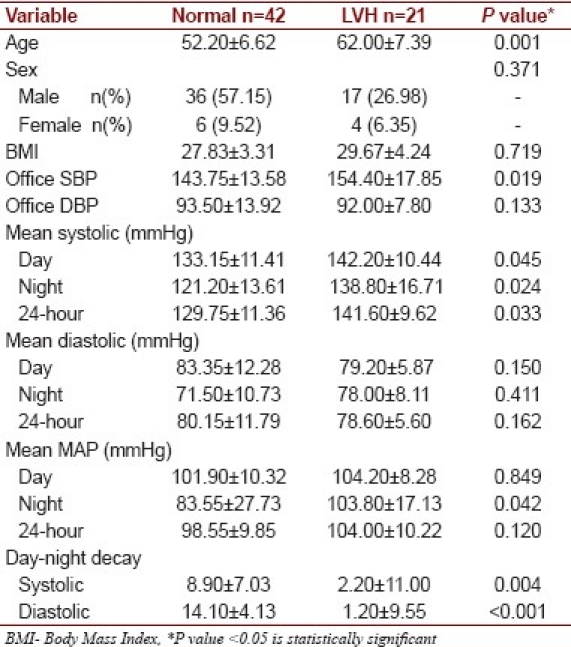
When the patients were stratified using only LVMI to normal LVMI and increased LVMI (i.e. LVH) as shown in [Table 3a], patients with LVH were found to be significantly older with higher office SBP than those without LVH. In similar vein, mean ambulatory SBP (day time, night time and 24-hour- average) was significantly higher in patients with LVH compared with those without LVH. Day-night SBP and DBP decay (i.e. percentage nocturnal decline in BP) were also significantly lower in LVH group than in the group without LVH. A similar trend was observed when a subgroup of those who were not on antihypertensive drugs was separated and was similarly compared [Table 3b].
Table 3a.
Ambulatory blood pressure parameters of normal and increased left ventricular mass index in the study population
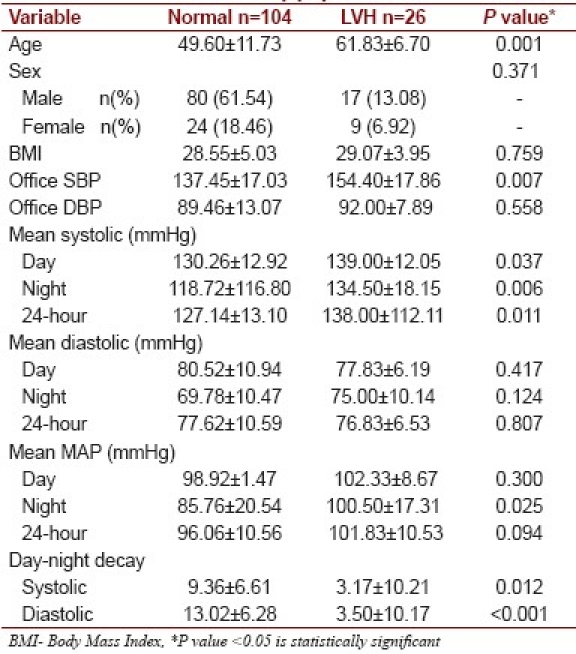
Table 3b.
Ambulatory blood pressure parameters of normal and increased left ventricular mass index in untreated hypertensives
Tables 4a and 4b depict ABP parameters of different LV geometric patterns.
Table 4a.
Ambulatory blood pressure parameters of different geometric patterns in the study population
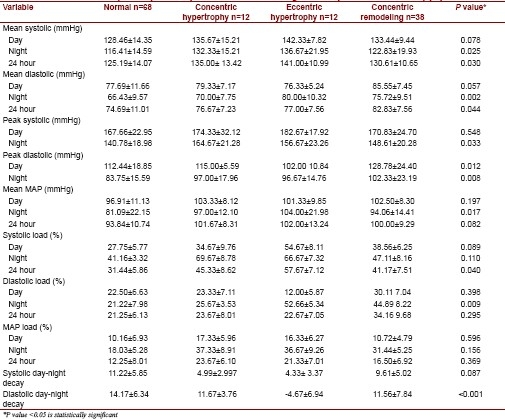
Table 4b.
Ambulatory blood pressure parameters of different geometric patterns in untreated hypertensives
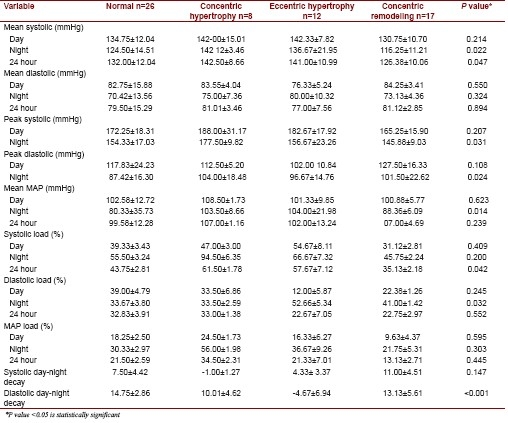
Analysis of frequencies of occurrence of normal and abnormal ABP variables in the study population showed that though all patients with eccentric LVH had normal day time mean ambulatory DBP, they all had abnormal day time mean ambulatory SBP, night time mean ambulatory SBP, elevated day time and night time SBP loads, as well as non-dipping DBP pattern. All the patients with concentric remodeling geometry had their night time DBP load elevated. Overall, 111(85.39%) of the patients had night time SBP load > 20%.
Significant correlates of LV mass index in this study population were age(r = 0.291, P = 0.022), mean ambulatory SBP (day time: r = 0.355, P = 0.004; night time: r = 0.343, P = 0.005; 24- hour average: r = 0.358, P = 0.004) and day-night decay (systolic: r = -0.388, P = 0.007; diastolic: r = -0.290, P = 0.022). Total (24-hours) SBP (r = 0.379, P = 0.031) but not DBP (r = 0.124, P = 0.0825) variability positively correlated with LV mass index.
DISCUSSION
In this study, the prevalence of LVH was 20% which is comparable with that reported earlier in an unselected population of hypertensive patients like ours.[13] The prevalence of abnormal LV geometry was 48.4% and LV concentric remodeling constituted the majority (29%) while eccentric hypertrophy and concentric hypertrophy had similar prevalence of 9.7% apiece. This is in contrast with work by Aje et al[9] at Ibadan, south western Nigeria where more than two third of their hypertensive patients had various altered LV geometry. The proportional prevalence of different altered LV geometry in that study also differs with this study. The reason for this difference may be related to the patient selection, use of different formulae and partitioning values for LVMI estimation. While our patients were unselected hypertensives, theirs were newly presenting hypertensives.
It was noted that patients with abnormal geometry were older with higher office systolic and mean ambulatory SBP (day time, night time and 24-hour average). Some authors have suggested that age significantly affects the occurrence of altered LV structure and geometric pattern in an upward trend fashion.[18]
Although increased LV mass predicts greater risk of cardiovascular events, independently of the presence of other risk factors, the role of LV geometry as an independent predictor of cardiovascular morbidity and mortality has been a controversial issue. The prospective study of Koren et al[6] showed that patients with normal LV architecture had the best prognosis; those with concentric LV hypertrophy had the worst and the other groups intermediate prognosis while there was no attenuation of risk over a period of 10 years despite conventional hypertensive treatment of most patients. The findings from the Framingham Heart Study[19,20] confirmed that subjects with concentric LV hypertrophy had the worst prognosis, followed by those with eccentric LV hypertrophy, concentric LV remodeling and normal LV geometry. The role of LV geometry as an independent predictor of cardiovascular morbidity and mortality was further emphasized by Verdecchia et al[21] who found that in hypertensive patients with normal LV mass on echocardiography, concentric LV remodeling was an important and independent predictor of increased cardiovascular risk. Though this is not a study on prognostic value of LV geometry, it was observed that patients with EH were older, with significantly higher office SBP, ambulatory SBPs and LV mass index.
In this study, ambulatory blood pressure variables at night time and 24hour average were significantly higher among patients with altered LV geometry compared with normal geometry. This also was the case with mean SBP and mean DBP at night and 24-hour average as well as peak systolic and DBP at night.Cross sectional studies which have investigated whether the target organ damage accompanying hypertensives is more closely related to 24-hour average than office BP have almost invariably shown this to be the case. In addition, findings of the study on ambulatory monitoring of pressure and lisinopril Administration (SAMPLE) also provided evidence that the end organ damage of hypertension is related to day time, night time and 24-hour average ABPs.[1]
A large number of studies have come to the conclusion that in hypertensive subjects in whom nocturnal BP falls was less than 10%, organ damage is much greater than in those in whom it falls more than 10% and that this is the case also for the organ damage progression and the incidence of cardiovascular disease.[20,21] In our study, day-night systolic and diastolic decay was significantly reduced in those patients with LVH compared with those without LVH. In addition, day-night systolic and diastolic decay was significantly lower than 10% in all the strata of altered geometric pattern but worst in patients with eccentric LV geometry.
Twenty-four-hour-average SBP correlated with LVMI in our study. This is in agreement with studies by Rowlands et al[22] and Devereux et al[23] (r = 0.36, 0.35 and 0.31, respectively). However, correlation coefficients of day time systolic and night time SBPs in our study were generally lower than in Rowlands but much better than Devereux. Our findings of inverse relation between the percentage decline in nocturnal BP and LV mass index is significant. This further confirms the importance of ‘non-dipping’ of nocturnal blood pressure as earlier described by O’Brien et al[12] on the development of LVH and its consequential increased cardiovascular risk.
Though mean ambulatory systolic and DBPs (night time and 24-hour average) were statistically significant among the LV geometric patterns, ambulatory systolic pressures were the significant correlates of LVMI in this study. LV wall stress is mostly related to SBP which may explain this finding.
One of the major limitations of this study is the small sample size. It was also difficult to determine the length of treatment for those who were on medications. Nonetheless, it is still possible to draw some significant conclusions from this study.
In conclusion, this study had demonstrated that in Nigerian hypertensive patients, presence of LVH is associated with higher mean ambulatory SBP and lower percentage nocturnal decline in systolic and DBP than its absence. These abnormalities appeared to be worse in patients with LV eccentric geometry when compared with other patterns of LV geometry, especially in untreated hypertensive patients.
Footnotes
Source of Support: Nil
Conflict of Interest: We declare no conflict of interest.
REFERENCES
- 1.Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, et al. ESH Working Group on Blood Pressure Monitoring. European Society of Hypertension guidelines for blood pressure monitoring at home: A summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008;26:1505–26. doi: 10.1097/HJH.0b013e328308da66. [DOI] [PubMed] [Google Scholar]
- 2.Devereux RB, Pickering TG. Relationship between the level, pattern and variability of ambulatory blood pressure and target organ damage in hypertension. J Hypertens. 1991;8:S34–8. [PubMed] [Google Scholar]
- 3.Liu JE, Roman MJ, Pini R, Schwartz JE, Pickering TG, Devereux RB. Cardiac and arterial target organ damage in adults with elevated ambulatory and normal office blood pressure. Ann Intern Med. 1999;131:564–72. doi: 10.7326/0003-4819-131-8-199910190-00003. [DOI] [PubMed] [Google Scholar]
- 4.Levy D, Garrison RJ, Savage DD, Kannel WP, Castelli WP. Prognostic implications of echocardiography determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322:1561–6. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 5.Ghali JK, Liao Y, Simmons B, Castaner A, Cao G, Cooper RS. The prognostic role of left ventricular hypertrophy in patients with or without coronary artery disease. Ann Intern Med. 1992;117:826–31. doi: 10.7326/0003-4819-117-10-831. [DOI] [PubMed] [Google Scholar]
- 6.Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in men and women with essential hypertension. Ann Intern Med. 1991;114:345–52. doi: 10.7326/0003-4819-114-5-345. [DOI] [PubMed] [Google Scholar]
- 7.Krumholz H, Larson M, Levy D. Prognosis of left ventricular geometric patterns in the Framingham heart study. J Am Coll Cardiol. 1995;25:879–84. doi: 10.1016/0735-1097(94)00473-4. [DOI] [PubMed] [Google Scholar]
- 8.Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Battistelli M, Bartoccini C, et al. Adverse prognostic significance of concentric remodeling of the left ventricule in hypertensive patients with normal left ventricular mass. J Am Coll Cardiol. 1995;25:871–8. doi: 10.1016/0735-1097(94)00424-O. [DOI] [PubMed] [Google Scholar]
- 9.Aje A, Adebiyi AA, Oladapo OO, Dada A, Ogah OS, Ojji DB, et al. Left ventricular geometric patterns in newly presenting Nigerian hypertensives: An echocardiographic study. BMC Cardiovasc Disord. 2006;6:4. doi: 10.1186/1471-2261-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National High Blood Pressure Education Program. The Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 11.O’Brien E, Coats A, Owens P, Petrie J, Padfield PL, Littler WA, et al. Use and interpretation of ambulatory blood pressure monitoring: Recommendations of the British Hypertension Society. BMJ. 2000;320:1128–34. doi: 10.1136/bmj.320.7242.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Brien E, Sheridan J, O’Malley K. Dippers and non-dippers. Lancet. 1988;2:397. doi: 10.1016/s0140-6736(88)92867-x. [DOI] [PubMed] [Google Scholar]
- 13.Tsioufis C, Stefanadis C, Goumas G, Pitsavos C, Toutouzas P. Relation of ambulatory blood pressure load with left ventricular geometry in untreated patients with mild-to-moderate hypertension. J Hum Hypertens. 1999;13:677–82. doi: 10.1038/sj.jhh.1000912. [DOI] [PubMed] [Google Scholar]
- 14.Sahn DJ, DeMaria A, Kisslo J, Weyman A. The committee on M-mode Standardization of the American Society of Echocardiography: Recommendations regarding quantitation in M-mode electrocardiography: Results of a survey of echocardiographic measurements. Circulation. 1978;58:1072–83. doi: 10.1161/01.cir.58.6.1072. [DOI] [PubMed] [Google Scholar]
- 15.Levy D, Savage DD, Garrison RJ, Anderson KM, Kannel WB, Castelli WP. Echocardiographic criteria for left ventricular hypertrophy: The Framingham Heart Study. Am J Cardiol. 1987;59:956–60. doi: 10.1016/0002-9149(87)91133-7. [DOI] [PubMed] [Google Scholar]
- 16.Reichek M, Devereux RB. Reliable estimation of peak left ventricular systolic pressure by M-mode echocardiographic determined end-diastolic relative wall thickness. Identification of severe valvular aortic stenosis in adult patients. Am Heart J. 1982;103:202–9. doi: 10.1016/0002-8703(82)90493-8. [DOI] [PubMed] [Google Scholar]
- 17.Iwashima Y, Horio T, Kuroda S, Takishita S, Kawano Y. Influence of plasma aldosterone on left ventricular geometry and diastolic function in treated essential hypertension. Hypertens Res. 2002;25:49–56. doi: 10.1291/hypres.25.49. [DOI] [PubMed] [Google Scholar]
- 18.de Simone G, Daniels SR, Kimball TR, Roman MJ, Romano C, Chinali M, et al. Evaluation of concentric left ventricular geometry in humans: Evidence for age-related systematic underestimation. Hypertension. 2005;45:64–8. doi: 10.1161/01.HYP.0000150108.37527.57. [DOI] [PubMed] [Google Scholar]
- 19.Mancia G, Zanchetti A, Agabiti-Rosei E, Benemio G, De Cesaris R, Fogari R, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy. Circulation. 1997;95:1464–70. doi: 10.1161/01.cir.95.6.1464. [DOI] [PubMed] [Google Scholar]
- 20.Verdecchia P, Schillaci G, Guerrieri M, Gatteschi C, Benemio G, Boldrini F, et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990;81:528–36. doi: 10.1161/01.cir.81.2.528. [DOI] [PubMed] [Google Scholar]
- 21.Verdecchia P, Schillaci G, Zampi I, Gatteschi C, Battistelli M, Bartoccini C, et al. Blunted nocturnal fall in blood pressure in hypertensive women with future cardiovascular morbid events. Circulation. 1993;88:986–92. doi: 10.1161/01.cir.88.3.986. [DOI] [PubMed] [Google Scholar]
- 22.Rowlands DB, Glover DR, Ireland MA, McLeay RA, Stallard TJ, Watson RD, et al. Assessment of left ventricular mass and its response to antihypertensive treatment. Lancet. 1982;1:467–70. doi: 10.1016/s0140-6736(82)91448-9. [DOI] [PubMed] [Google Scholar]
- 23.Devereux RB, Pickering TG, Harshfield GA, Kleinert HD, Denby L, Clark L, et al. Left ventricular hypertrophy in patients with hypertension: Importance of blood pressure response to regularly recurring stress. Circulation. 1983;68:470–6. doi: 10.1161/01.cir.68.3.470. [DOI] [PubMed] [Google Scholar]


