Abstract
Background
Mental disorders are a major contributor to the burden of disease in all regions of the world. There are limited data on the epidemiology of major depressive disorder in South Africa.
Methods
A nationally representative household survey was conducted between 2002 and 2004 using the World Health Organization Composite International Diagnostic Interview (CIDI) to establish a diagnosis of depression. The dataset analysed included 4 351 adult South Africans of all racial groups.
Results
The prevalence of major depression was 9.7% for lifetime and 4.9% for the 12 months prior to the interview. The prevalence of depression was significantly higher among females than among males. The prevalence was also higher among those with a low level of education. Over 90% of all respondents with depression reported global role impairment.
Conclusion
In comparison with data from other countries, South Africa has lower rates of depression than the USA but higher rates than Nigeria. The findings are broadly consistent with previous findings in South Africa. These findings are the first step in documenting a level of need for care in a context of significant under-funding of mental health services and research in South Africa
Mental disorders are a major contributor to the burden of disease in all regions of the world, with about 14% of the global burden attributable to neuropsychiatric disorders.1 Even in sub-Saharan Africa, a region with the highest burden of communicable disease, neuropsychiatric disorders account for nearly 10% of the total burden of disease.2 Mental disorders are not only linked to many other health conditions, but are also among the most costly medical disorders in terms of projected health care expenditures needed to treat them.3
Epidemiological studies and data on prevalence rates of major depressive disorders in Africa are limited. Of the studies that have been completed, many have used clinic attendance as a recruitment method,4 thus introducing a potential bias. In South Africa, small rural-based studies have found a prevalence rate of depressive symptomatology of 18%5 and a rate of depression of 27%.6 Other results include a prevalence of depression of 25.2%7 in an urban setting, while Cooper and colleagues8 found a 34.7% prevalence of postpartum depression in a peri-urban settlement in Cape Town. To date there have not been any nationally representative data on the prevalence of major depressive disorder in South Africa. In a resource-constrained setting such as South Africa, nationally representative data that include age of onset and role impairment comparisons are of crucial importance both in terms of highlighting the country’s burden of disease and to enable targeting of limited intervention funding.
Method
Sample
The study formed part of the South African Stress and Health (SASH) study,9 which was part of the World Health Organization’s World Mental Health (WMH) 2000 initiative. The SASH study is a national probability survey of adult South Africans living in households and hostel quarters (the latter were included to maximise coverage of young working-age males). Individuals of all race and ethnic backgrounds were included in the study. The sample was selected using a three-stage sample design. The first stage involved the stratified selection of primary sampling units based on the 2001 South African Census Enumeration Areas (EAs). The second stage involved the sampling of housing units within clusters selected in each EA. The third stage involved the random selection of one adult respondent in each sampled housing unit. Field interviewers made up to three attempts to contact respondents. A total sample of 5 089 households was selected for the SASH. Field interviews were obtained with 4 433 (87.1%) of the designated respondents. Based on quality control criteria, 4 351 of the field interviews were retained for use in the analysis. There were no differences in response rates across racial groups.
Instruments
The diagnostic interview used in the SASH was the World Health Organization (WHO) Composite International Diagnostic Interview Version 3.010 (CIDI 3.0), a fully structured lay-administered interview that generates diagnoses according to the criteria of both the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) and Diagnostic and Statistical Manual, 4th edition (DSM-IV) diagnostic systems, and has been widely used in epidemiological studies throughout the world. The CIDI was translated from English into six other languages used in South Africa (virtually all South Africans speak at least one of these languages), and then back-translated.
Respondents who were diagnosed with either 12-month or lifetime major depression were administered the Sheehan Disability Scale (SDS). The SDS assesses the extent to which depression interferes with functioning in the domains of work, household, relationship and social roles.11 It is a 10-point visual analogue scale labelled none (0) to very severe (10). Respondents were also asked whether they had received treatment for emotional problems during the preceding 12 months.
Procedure
Interviewers were trained in the administration of the CIDI in centralised group sessions lasting 1 week. Two formal pre-tests of all of the survey questions were completed, with a total of over 50 respondents participating. The interviews were conducted face-to face in seven different languages: English, Afrikaans, Zulu, Xhosa, Northern Sotho, Southern Sotho and Tswana. The protocol was reviewed by the ethics committee of the Medical University of South Africa, and all subjects gave informed consent. Interviews lasted an average of 3½ hours, with some requiring more than one visit to complete. Data were collected between January 2002 and June 2004.
Statistical analysis
All analyses reported accounted for the complex survey design based on person-level weights that incorporated sample selection, non-response and post-stratification factors. Data were analysed using Stata Version 10.0 (Stata Corporation, College Station, USA).
Results
The total sample of 4 351 adults was largely female (53.7%) and black (76.2%), although other racial groups were represented (10.4% coloured, 10% white, 3.4% Indian/Asian). Further, half were married, while most were unemployed (69.2%), had less than 12 years of education (62.7%), and lived in urban areas (59.7%) (Table I).
Table I.
Description of sample, according to prevalence of major depression
| Lifetime DSM-IV major depression* | 12-month DSM-IV major depression* | ||||
|---|---|---|---|---|---|
| Total population | % | OR (95% CI) | % | OR (95% CI) | |
| N (%) | 4 351 (100%) | 439 (9.7) | - | 223 (4.9) | - |
| Demographic characteristics | |||||
| Mean age (yrs) (SE) | 37.0 (0.26) | 37.8 | - | 37.9 | - |
| Age categories (yrs) | |||||
| 18 – 29 | 39.1 | 32.7 | - | 31.9 | - |
| 30 – 39 | 22.1 | 23.4 | - | 23.8 | - |
| 40 – 49 | 18.1 | 24.5 | - | 22.5 | - |
| ≥50 | 20.7 | 19.4 | - | 21.8 | - |
| Gender | |||||
| Male | 46.3 | 33.9 | 1.0 | 28.8 | 1.0 |
| Female | 53.7 | 66.1 | 1.75 (1.3 – 2.4) | 71.2 | 2.17 (1.5 – 3.2) |
| Race | |||||
| Black | 76.2 | 75.4 | 1.0 | 72.5 | 1.0 |
| Coloured | 10.4 | 11.1 | 1.05 (0.8 – 1.5) | 13.3 | 1.31 (0.9 – 2.0) |
| White | 10.0 | 8.9 | 0.84 (0.3 – 2.2) | 7.0 | 0.69 (0.2 – 2.2) |
| Indian/Asian | 3.4 | 4.6 | 1.42 (0.7 – 3.0) | 7.3 | 2.38 (1.0 – 5.7) |
| Currently married | 50.1 | 48.3 | 0.78 (0.6 – 1.0) | 52.5 | 0.95 (0.7 – 1.3) |
| Location | |||||
| Rural | 38.4 | 35.1 | 1.0 | 35.1 | 1.0 |
| Urban | 61.6 | 64.9 | 1.15 (0.9 – 1.5) | 64.9 | 1.15 (0.8 – 1.6) |
| SES tertile | |||||
| 0 | 30.4 | 31.4 | 1.0 | 31.9 | 1.0 |
| 1 | 33.3 | 30.5 | 0.90 (0.7 – 1.2) | 31.4 | 0.94 (0.6 – 1.4) |
| 2 | 36.3 | 38.1 | 1.03 (0.7 – 1.5) | 36.7 | 0.99 (0.6 – 1.6) |
| Socio-economic status | |||||
| Education | |||||
| None | 6.8 | 4.9 | 1.0 | 3.3 | 1.0 |
| Grade 1 – 7 | 19.1 | 27.6 | 2.11 (1.2 – 3.7) | 32.6 | 3.70 (1.5 – 9.3) |
| Grade 8 – 11 | 35.4 | 33.8 | 1.36 (0.8 – 2.2) | 36.1 | 2.18 (1.0 – 5.0) |
| Matric | 23.5 | 21.5 | 1.38 (0.8 – 2.4) | 13.9 | 1.28 (0.5 – 3.3) |
| Matric+ | 15.3 | 12.3 | 1.12 (0.6 – 2.1) | 14.1 | 1.94 (0.7 – 5.4) |
| Employed | 31.0 | 32.0 | 0.95 (0.6 – 1.4) | 30.6 | 0.89 (0.6 – 1.4) |
| Income categories (R), personal (mean (SD)) | - | - | |||
| 0 | 13.7 | 12.5 | 1.0 | 18.1 | 1.0 |
| 1 – 2 500 | 29.5 | 35.6 | 1.31 (0.8 – 2.2) | 28.6 | 0.69 (0.4 – 1.2) |
| 2 501 – 5 000 | 15.4 | 12.3 | 0.84 (0.5 – 1.4) | 11.0 | 0.51 (0.3 – 1.0) |
| 5 001 – 10 000 | 19.6 | 18.5 | 0.99 (0.6 – 1.8) | 17.0 | 0.62 (0.3 – 1.3) |
| ≥10 001 | 21.8 | 21.1 | 1.03 (0.6 – 1.8) | 25.3 | 0.85 (0.4 – 1.7) |
Odds ratios adjusted for age categories.
Prevalence of major depressive episode
The prevalence of major depressive episode (MDE) in the total sample was 9.7% for lifetime and 4.9% for the 12 months prior to the interview. The prevalence of MDE was significantly higher among female respondents, with females 1.75 times more likely to experience lifetime depression than males (95% confidence interval (CI) 1.3 – 2.4), and 2.17 times more likely to experience 12-month MDE than males (95% CI 1.5 – 3.2) (Table I).
Socio-demographic correlates
The prevalence of MDE was significantly higher among those with a low average level of education, people with Grade 1 – 7 schooling being 2.11 times more likely to have experienced lifetime MDE (95% CI 1.2 – 3.7) and 3.70 times more likely to have experienced 12-month MDE (95% CI 1.5 – 9.3) than those with higher levels of education (Table I). The prevalence of MDE was also significantly higher among people between the ages of 40 and 49 years, who were 1.71 times more likely to have experienced lifetime MDE (95% CI 1.3 – 2.3) than other age groups. No other socio-demographic correlates were related to either lifetime or 12-month MDE.
Age of onset and mean number of MDEs
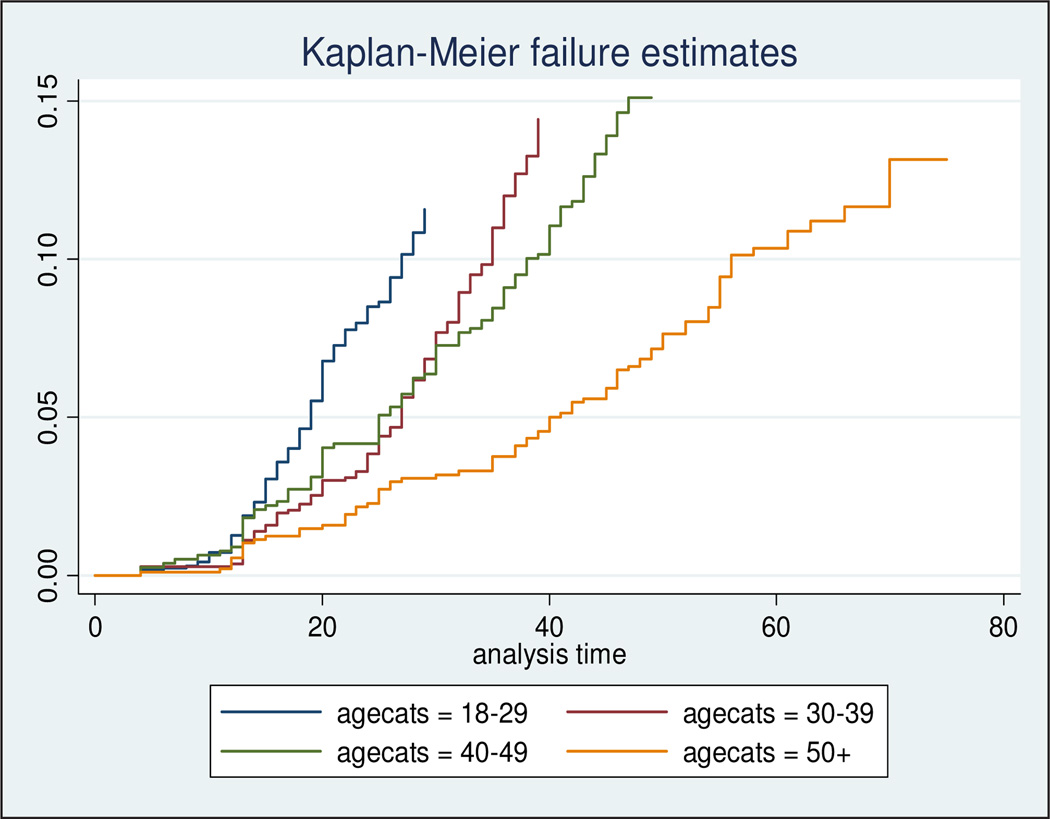
The mean age of onset of MDE was 25.8 years for the total sample, 26 years for females and 25.6 years for males. There were no significant differences for mean number of lifetime episodes across age cohorts or between genders. Kaplan-Meier curves for age at onset of depression were generated for four groups defined by age at interview (18 – 29 years, 30 – 39 years, 40 – 49 years and >50 years). Risk is low until the early teens, and then begins to rise increasingly steeply in more recent cohorts (Fig. 1).
Fig. 1.
Cumulative lifetime prevalence of MDE by birth cohort.
12-month treatment
In the past 12 months, 8.2% of people with lifetime major depressive disorder had spoken to a psychiatrist. People with major depression were 2.2 times more likely to report speaking to (or receiving treatment from) a psychiatrist in the past 12 months compared with those without lifetime major depression. Those with major depression were also over 2 times more likely to have spoken to another mental health professional, 1.47 times more likely to have spoken to a general practitioner, 2.03 times more likely to have spoken to a religious adviser, and over 2.5 times more likely to have spoken to a healer compared with those without lifetime major depression (Table II).
Table II.
Service use in the past 12 months by lifetime major depression
| Total population | DSM-IV major depression |
No DSM-IV major depression |
OR | p-value | |
|---|---|---|---|---|---|
| Lifetime major depression | |||||
| N (%) | 4 351 (100) | 439 (9.7) | 3 912 (90.3) | ||
| Psychiatrist | 4.3 | 8.2 | 3.9 | 2.20 | 0.001 |
| Any other mental | 3.5 | 6.4 | 3.2 | 2.07 | 0.011 |
| health professional* | |||||
| General practitioner† | 13.3 | 17.9 | 12.9 | 1.47 | 0.049 |
| Traditional healer | 6.5 | 9.0 | 6.2 | 1.50 | 0.067 |
| Any other health professional‡ | 7.6 | 8.5 | 7.5 | 1.15 | 0.491 |
| Religious or spiritual advisor§ | 6.9 | 12.0 | 6.3 | 2.03 | 0.001 |
| Any other healer¶ | 2.2 | 4.8 | 1.9 | 2.59 | <0.001 |
| 12-month major depression | |||||
| N (%) | 4 351 (100%) | 223 (4.9) | 4 128 (95.2) | ||
| Psychiatrist | 4.3 | 12.6 | 3.9 | 3.56 | <0.001 |
| Any other mental health professional* | 3.5 | 10.5 | 3.2 | 3.59 | <0.001 |
| General practitioner† | 13.3 | 20.7 | 13.0 | 1.76 | 0.014 |
| Traditional healer | 6.5 | 10.8 | 6.3 | 1.82 | 0.024 |
| Any other health professional‡ | 7.6 | 7.1 | 7.6 | 0.93 | 0.819 |
| Religious or spiritual advisor§ | 6.9 | 10.2 | 6.7 | 1.58 | 0.087 |
| Any other healer ¶ | 2.2 | 6.9 | 2.0 | 3.65 | <0.001 |
Any other mental health professional, such as a psychologist, psychotherapist, psychiatric social worker, mental health nurse or mental health counsellor.
A general practitioner or any other medical doctor.
Any other health professional, such as a nurse or physician’s assistant.
A religious or spiritual advisor, such as a minister, priest or rabbi.
Any other healer, such as a chiropractor or spiritualist.
Role impairment of 12-month MDE
Over 90% of respondents with a MDE reported global role impairment (using the Sheehan disability scale). Across all dimensions of the Sheehan scale the only significant gender difference was that women were more likely than men to report a home impairment (p=0.037) (Table III). Respondents with MDE reported a mean of 57 days out of role when, as a result of the depression, they were unable to perform their normal activities. Males over 50 years reported a markedly higher number of days out of role (128 days) than any other age cohort, while males in that age cohort reported almost three times the number of days out of role (128 days v. 66 days) than females of the same age.
Table III.
Role impairment and depression, by sex
| Lifetime major depressive disorder | 12-month major depressive disorder | |||||
|---|---|---|---|---|---|---|
| Men (%) |
Women (%) |
p-value | Men (%) |
Women (%) |
p-value | |
| Mean days out of role in the past 12 months (N) | 72.6 | 51.2 | 72.6 | 51.2 | ||
| Home | ||||||
| None | 70.2 | 56.6 | 0.037 | 29.5 | 18.7 | 0.052 |
| Mild | 12.2 | 7.5 | 28.9 | 14.1 | ||
| Moderate | 10.8 | 15.8 | 25.5 | 29.6 | ||
| Severe | 3.6 | 11.8 | 8.6 | 22.1 | ||
| Very severe | 3.2 | 8.3 | 7.5 | 15.5 | ||
| Work | ||||||
| None | 72.8 | 59.4 | 0.161 | 35.5 | 23.9 | 0.278 |
| Mild | 8.7 | 7.2 | 20.6 | 13.5 | ||
| Moderate | 9.5 | 16.5 | 22.4 | 30.9 | ||
| Severe | 4.6 | 12.6 | 11.0 | 23.5 | ||
| Very severe | 44.8 | 4.4 | 10.6 | 8.2 | ||
| Relationships | ||||||
| None | 72.2 | 58.5 | 0.180 | 34.3 | 22.2 | 0.311 |
| Mild | 2.0 | 10.5 | 16.6 | 19.7 | ||
| Moderate | 7.2 | 14.9 | 17.1 | 27.9 | ||
| Severe | 8.2 | 12.6 | 19.3 | 23.6 | ||
| Very severe | 5.4 | 3.6 | 12.7 | 6.7 | ||
| Social | ||||||
| None | 71.8 | 59.5 | 0.173 | 33.3 | 24.1 | 0.293 |
| Mild | 6.1 | 11.9 | 14.4 | 22.4 | ||
| Moderate | 11.5 | 11.6 | 27.1 | 21.7 | ||
| Severe | 3.9 | 11.0 | 9.2 | 20.5 | ||
| Very severe | 6.8 | 6.1 | 16.0 | 11.4 | ||
| Any impairment | 88.3 | 94.5 | n/a | 88.3 | 94.5 | n/a |
Discussion
The prevalence of MDE in South Africa was 9.8% for lifetime and 4.9% for the past 12 months. These rates were lower than those found in the in the National Comorbidity Survey Replication,12 where lifetime and 12-month prevalence rates were 16.2% and 6.6%, respectively. In the World Health Organization WMH survey prevalence rates for any mood disorder ranged from 3.3% in Nigeria to 21.4% in the USA, while projected lifetime risk for any mood disorder ranged from 7.3% in China to 31.4% in the USA.13 So while South African rates are lower than those in the USA they are considerably higher than an estimate in a recent survey of Yoruba-speaking Nigeria14 and higher than in the majority of other countries that have participated in the first wave of the WHO WMH initiative.15 The Nigerian figures are likely to be underestimates, which is underscored by Gureje and colleagues’16 recent finding that among people over the age of 65 in Nigeria the lifetime prevalence of major depressive disorder was 26.2% while the 12-month prevalence was 7.1%.
The high lifetime prevalence estimates for psychiatric disorders found here are broadly consistent with previous work in South Africa. A community prevalence study of psychiatric morbidity in a rural coloured village found a prevalence of psychiatric morbidity of 27.1%, with the majority of cases diagnosed with depressive or anxiety disorder.5 Similarly, the rate of depression in a local primary care clinic was 37%.17 The association of mood disorder with gender (female gender associated with higher rates of MDE) is consistent with findings in rich and low- and middle-income countries.
The mean age of onset (25.8 years for the total sample, 26 years for females and 25.6 years for males) is in line with the median age-of-onset distributions in both the National Comorbidity Survey12 and the WMH survey13 and elsewhere, where age at onset is concentrated in the late 20s.18
The results regarding role impairment suggest that MDE is a seriously impairing condition, which is in line with other findings. In the South African context, the mean 57 days out of role is markedly higher than (for example) the 35.1 mean days out of role in the National Comorbidity Survey.12 These data, together with the fact that males over 50 years reported 128 days out of role, has crucial implications for productivity in the workplace, considering that in a study of the effects of chronic medical conditions on work loss, the mean number of days out of role for most of the chronic conditions was less than 15.19
Such data have been criticised by those who argue that distress in the developing world should not be conflated with the presence of psychiatric disorders, and who question the applicability of the DSM classification system to non-Western countries.20 There is growing acceptance, however, that psychiatric disorders, as classified by the DSM-IV and diagnosed by instruments such as the CIDI, are accompanied by significant social and occupational impairment. This is certainly borne out by our findings. Furthermore, research on pathogenesis and intervention has demonstrated that such disorders are associated with psychobiological dysfunction and that efficacious and cost-effective treatments are available, even in a developing-world context.21,22 This is not to minimise the potentially important effects of cultural context on the experience and expression of psychiatric disorders.
The paucity of data on mental disorders in low- and middle-income countries (LAMICs) significantly hampers the development of new and innovative interventions. The use of a standard instrument to detect depression renders us vulnerable to the criticism that we are potentially ignoring relevant culturally specific idioms of distress. Developing instruments that are culturally appropriate to the population being investigated is a useful approach, in that local idioms of distress are incorporated. One of the disadvantages of such instruments, however, is that they may limit between-country comparisons, and thus the cost-effective adaptation of innovative interventions that have been developed elsewhere. Clearly, both quantitative and qualitative research skills (combining both epidemiological and anthropological approaches) are needed in order to develop a full understanding of the presentation and prevalence of affective disorders and models of the most appropriate care.
There are important limitations that should be noted, all of which are likely to make the lifetime prevalence estimates here conservative.23 People with psychiatric disorders have been shown in other countries to be less likely than others to participate in mental health surveys.24 Another important limitation of the survey is the lack of clinical validation of the CIDI in the South African study. While results were reassuring in CIDI clinical validation studies carried out in conjunction with the WMH surveys in the USA23 and Europe,25 the cultural heterogeneity of the South African subjects might have impacted adversely on the diagnostic accuracy of the instrument.
Rigorous data on the proportion of the health budget spent on mental health services in the South African setting are not readily available, but there is consensus that a gross lack of parity exists, with significant under-funding of mental health services and research.26 In addition, there is a lack of research related to developing mental health interventions that can be scaled up and that do not need to be delivered by mental health professionals – a critical intervention in LAMIC countries, given the existing human resource crisis. We hope that the data reported here take a first step in documenting a level of need for care that is sufficiently compelling to provide impetus for changes in mental health policy in South Africa, with an appropriate increase in funding for mental health services.
Acknowledgements
The South African Stress and Health study was carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation, field work and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH070884), the John D and Catherine T MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R01-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline and Bristol-Myers Squibb. The South African Stress and Health study was funded by grant R01-MH059575 from the National Institute of Mental Health and the National Institute of Drug Abuse with supplemental funding from the South African Department of Health and the University of Michigan. Dan Stein is also supported by the Medical Research Council of South Africa. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/
Contributor Information
Mark Tomlinson, Department of Psychology, Stellenbosch University, and Health Systems Research Unit, Medical Research Council.
Anna T Grimsrud, School of Public Health and Family Medicine, University of Cape Town.
Dan J Stein, Department of Psychiatry and Mental Health, University of Cape Town.
David R Williams, Department of Society, Human Development and Health, Harvard School of Public Health, and Department of African and African American Studies, Harvard University, Cambridge, Mass., USA.
Landon Myer, School of Public Health and Family Medicine, University of Cape Town.
References
- 1.Prince M, Patel V, Saxena S, et al. No health without mental health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 2.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 3.Stein D, Seedat S. From research methods to clinical practice in psychiatry: Challenges and opportunities in the developing world. Int Rev Psychiatry. 2007;19:573–581. doi: 10.1080/09540260701563536. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine. In her lifetime: Female morbidity and mortality in Sub-Saharan Africa. [accessed 3 September 2003];1996 http://books.nap.edu/books/0309054303/html/index/html. [Google Scholar]
- 5.Rumble S, Swartz L, Parry C, et al. Prevalence of psychiatric morbidity in the adult population of a rural South African village. Psychol Med. 1996;26:997–1007. doi: 10.1017/s0033291700035327. [DOI] [PubMed] [Google Scholar]
- 6.Rumble S. MSc thesis. University of Cape Town; 1994. Prevalence of psychiatric morbidity in the adult population of Mamre: an empirical and methodological investigation. [Google Scholar]
- 7.Gillis LS, Welman M, Koch A, Joyi M. Psychological distress and depression in urbanising elderly black persons. S Afr Med J. 1991;79:490–495. [PubMed] [Google Scholar]
- 8.Cooper PJ, Tomlinson M, Swartz L, Woolgar M, Murray L, Molteno C. Postpartum depression and the mother-infant relationship in a South African peri-urban settlement. Br J Psychiatry. 1999;175:554–558. doi: 10.1192/bjp.175.6.554. [DOI] [PubMed] [Google Scholar]
- 9.Williams DR, Herman A, Kessler RC, et al. The South African Stress and Health Study: Rationale and design. Metab Brain Dis. 2004;19:135–147. doi: 10.1023/b:mebr.0000027424.86587.74. [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int J Psychiatr Med. 1997;27:93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication. JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the world health organization’s world mental health survey initiative. World Psychiatry. 2007;6:168–176. [PMC free article] [PubMed] [Google Scholar]
- 14.Gureje O, Lasebikan VO, Kola L, et al. Lifetime and 12-month prevalence of mental disorders in the Nigerian Survey of Mental Health and Well-Being. Br J Psychiatry. 2006;188:465–471. doi: 10.1192/bjp.188.5.465. [DOI] [PubMed] [Google Scholar]
- 15.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 16.Gureje O, Kola L, Afolabi E. Epidemiology of major depressive disorder in elderly Nigerians in the lbadan Study of Ageing: a community-based survey. Lancet. 2007;370:957–964. doi: 10.1016/S0140-6736(07)61446-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carey P, Stein D, Zungu-Dirwayi N, Seedat S. Trauma and posttraumatic stress disorder in an urban Xhosa primary care population: Prevalence, comorbidity, and service use patterns. J Nerv Ment Dis. 2003;191:230–236. doi: 10.1097/01.NMD.0000061143.66146.A8. [DOI] [PubMed] [Google Scholar]
- 18.Lepine JP. Epidemiology, burden, and disability in depression and anxiety. J Clin Psychiatry. 2001;62 suppl 13:4–10. [PubMed] [Google Scholar]
- 19.Kessler RC, Greenberg PE, Mickelson KD, Meneades LM, Wang PS. The effects of chronic medical conditions on work loss and work cutback. J Occup Environ Med. 2001;43:218–225. doi: 10.1097/00043764-200103000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Kirmayer LJ. The place of culture in psychiatric nosology: Taijin kyofusho and DSM-III-R. J Nerv Ment Dis. 1991;179:19–28. doi: 10.1097/00005053-199101000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Stein DJ, Gureje O. Depression and anxiety in the developing world: is it time to medicalise the suffering? Lancet. 2004;364:233–234. doi: 10.1016/S0140-6736(04)16693-2. [DOI] [PubMed] [Google Scholar]
- 22.Chisholm D, Sanderson K, Ayuso-Mateos JL, Saxena S. Reducing the global burden of depression: Population-level analysis of intervention cost-effectiveness in 14 world regions. Br J Psychiatry. 2004;164:393–403. doi: 10.1192/bjp.184.5.393. [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, Wittchen H-U, Abelson JM, et al. Methodological studies of the Composite International Diagnostic Interview (CIDI) in the US national comorbidity survey (NCS) Int J Methods Psychiatr Res. 1998;7:33–35. [Google Scholar]
- 25.Haro J-M, Arbabzadeh-Bouchez S, Brugha TS, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health Surveys. Int J Methods Psychiatr Res. 2006;15:167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seedat S, Emsley RA, Stein DJ. Land of promise: challenges and opportunities for research in South Africa. Mol Psychiatry. 2004;9:891–892. doi: 10.1038/sj.mp.4001572. [DOI] [PubMed] [Google Scholar]