Abstract
Objectives
Mass psychogenic illness can be a significant problem for triage and hospital surge in disasters; however, research has been largely limited to posthoc observational reports. Reports on the impact of public media during a disaster have suggested both salutary as well as iatrogenic psychological effects. This study was designed to determine if psychogenic illness can be evoked and if media will exacerbate it in a plausible, controlled experiment among healthy community adults.
Methods
A randomized controlled experiment used a simulated biological threat and elements of social contagion—essential precipitants of mass psychogenic illness. Participants were randomly assigned to one of three groups: no-intervention control group, psychogenic illness induction group, or psychogenic illness induction plus media group. Measures included three assessments of symptom intensity, heart rate, blood pressure, as well as questionnaires to measure potential psychogenic illness risk factors.
Results
The two psychogenic induction groups experienced 11 times more symptoms than the control group. Psychogenic illness was observed in both men and women at rates that were not significantly different. Higher rates of lifetime history of traumatic events and depression were associated with greater induction of illness. Media was not found to exacerbate symptom onset.
Conclusions
Psychogenic illness relevant to public health disasters can be evoked in an experimental setting. This sets the stage for further research on psychogenic illness and strategies for mitigation.
Keywords: disaster medicine, mass media, psychogenic illness, trauma, psychosomatic
Recent events, both sociopolitical and biomedical, raise awareness of the importance of improving our understanding of the human response to mass biological incidents such as the purposeful release of infectious agents or toxins (eg, anthrax and sarin gas) or the natural spread of illness such as severe acute respiratory syndrome or pandemic influenza.1-4 Inherent in such biological events is the risk of mass psychogenic illness, which can be even more problematic than the symptoms resulting from the actual exposure.4 Mass psychogenic illness occurs when people in group settings experience symptoms of illness that are without identifiable organic cause but that appear linked to an environmental trigger. In some cases, the index cases involve identifiable organic illness, with the symptoms then spreading to many people who lack organic illness. Some observe that mass psychogenic illness involves a shared belief among the affected people as to the cause of the symptoms.5 Common symptoms include nausea, dizziness, fainting, headache, abdominal pain, and hyperventilation.6-8
There is a consensus that mass psychogenic illness is a social phenomenon that strikes otherwise healthy people, that it is transmitted most efficiently in cohesive social groups, such as schools and workplaces, and that it is more often seen in populations that are subject to high levels of psychological, social, or political stress.8 There is also a consensus that affected people experience “real” symptoms—symptoms that are not imagined or “all in the head.”9
Responses of emergency managers and the media to initial reports of unexplained illness are believed to amplify the phenomenon, spreading threatening information that lead more people to report symptoms. Steps such as evacuating students, mobilizing emergency responders, or hospitalizing people for minor symptoms are cited as promoting psychogenic episodes.10-15
Mass psychogenic illness can tax the resources of public health agencies and healthcare providers. When it occurs in tandem with a natural or manmade disaster, it can overwhelm health resources, multiplying demand and preventing care from being effectively targeted. For instance, when terrorists released toxic sarin gas in the subways of Tokyo, more than 85 percent of the 5,500 people seeking hospital treatment were found to be psychogenic patients.16 Moreover, during contagious infections, psychogenic illness can lead to the erosion of social distancing through individuals seeking medical evaluation that results in further spread of the biological agent.17,18
Although planning for psychogenic symptoms is recognized as important for emergency preparedness, to date, most studies of mass psychogenic illness have been posthoc observational reports of events such as toxic odors, vaccination campaigns, or radiation exposure.5,8 Four experimental studies have reported induction of psychogenic symptoms, and all used university students. Lindberg19 found a significant increase in symptoms among students who were told that sand on the floor of a room could be toxic when compared with those who were told the environment was normal. Mazzoni and coworkers20,21 conducted two experiments using inhalation of a “suspected environmental toxin” (actually ambient air) and examined the impact of symptomatic confederates and expected symptoms. They found a significant induction of symptoms over those who did not inhale the air and a main effect of social contagion (comparing experimental conditions with and without confederates). In their second study, designed to explore sex differences, they found an equivalent induction in both sexes. The fourth experiment also used presentation of a “chemical pollutant” and observed a significant increase in symptoms.22
No experimental studies have examined the effects of media reports on mass psychogenic illness, despite the extensive literature demonstrating a relationship between consumption of disaster media and rates of acute anxiety and post-traumatic stress disorder.23,24
Observational studies suggest a number of factors that are associated with an increased risk of psychogenic symptoms. Psychological factors (somatization, neuroticism, depression, and anxiety) are associated with higher rates of unexplained symptom reporting,25-28 as are lower education, lower socioeconomic status, minority race, history of abuse or trauma, and female sex.21,29-32
This study was designed to test an experimental protocol of psychogenic illness induction involving a plausible public health scenario for community adults. It was designed to mimic naturalistic scenarios in which psychogenic illness has been observed. Second, it incorporates an evaluation of the impact of media exposure on illness induction. Specifically, we hypothesized that 1) we could achieve a controlled induction of psychogenic symptoms in healthy community adult volunteers when compared with an unexposed control group in the context of a simulated biological event, 2) exposure to content-relevant media will increase psychogenic symptoms, 3) demographic and psychological risk factors will be associated with increased psychogenic symptoms, and 4) the experimental protocol will induce psychogenic symptoms without harm or long-term consequences to participants.
Methods
Participants
Community adult volunteers were recruited through advertisements on the Internet and in local newspapers. Standardized telephone screening (physical and psychiatric health) of respondents (n = 106) was conducted by the General Clinical Research Center (GCRC) nurses. Based on the screening, 67 adults (63 percent) were determined by the physician investigator to be eligible for the study. Strict exclusion criteria included any major or chronic medical or psychiatric condition or current acute illness. Of those eligible, 14 adults (21 percent) declined to participate, and another 14 were scheduled to participate but did not show up for the experiment. The demographic characteristics (gender, age, marital status, race, and education) of the 28 participants who were eligible, but did not participate, were not significantly different than those of the analyzed sample study.
Study participants (n = 39) were randomly assigned and stratified by age and sex to three conditions, Pill-only (n = 13), Pill + Media (n = 16), and Control (n = 10). These numbers are unequal, because some scheduled participants failed to arrive for the experiment as described earlier, and the control group was designed to be smaller. One participant in the Pill-only group was removed from the study after blood pressure readings indicated malignant hypertension, a pre-existing condition only acknowledged by the participant at the experiment. This resulted in an analysis sample of n = 38. The participants’ mean age was 42.3 years (standard deviation [SD] = 13.6), and 58 percent were women. About 50 percent (n = 20) were college graduates, 34 percent were married, and 79 percent were White (Table 1). The University Institutional Review Board approved the research design. Participants were compensated $150 for their participation.
Table 1.
Demographic characteristics of the sample (N = 38)
| Age (mean, SD) | 42.3 (13.6) |
| Female | 58 percent |
| Race (White) | 79 percent |
| Married | 34 percent |
| Education | |
| High school graduate | 13 percent |
| Some college | 37 percent |
| College graduate or more | 50 percent |
| SF36v2 Mental Health Component | 54.0 (6.4) |
| SF36v2 Physical Health Component | 54.6 (7.4) |
Measures
The SF 36v2 Health Survey
This widely used 36-item short-form global health survey was included to characterize the physical and mental health status of the sample. Version 2 of the scale is linked to US national norms and uses a mean of 50 and an SD of 10.33 Reliability and validity have been extensively reported.
Self-reported symptoms
The primary outcome measure was the number and severity of self-reported symptoms. Participants rated 54 physical symptoms three times at 1-hour intervals on a slight adaptation of Pennebaker’s Inventory of Limbic Languidness (PILL) symptom list.34 The list included all the non-specific symptoms reported in cases of psychogenic illness and unexplained medical conditions, such as nausea, fatigue, face flushing, and headache, and participants rated them on an intensity scale of 0 (not at all) to 3 (severe). The total score was the sum of the intensity ratings across all 54 symptoms. The PILL has demonstrated good reliability. Cronbach’s α range from 0.88 to 0.91; 2-month test-retest reliability ranges from 0.79 to 0.83.34
Physiological measures of arousal
GCRC nurses measured heart rate (wrist palpation) and blood pressure (standard cuff) at each assessment.
Psychogenic illness risk factors
The NEO-PI Neuroticism Scale
This is a widely used 48-item scale with scores reported as standardized T-scores.35 Neuroticism, a personality characteristic of chronic negative affect, is associated with reporting more frequent and more severe physical symptoms in the absence of objective disease.36 The NEO-PI has demonstrated good reliability and high internal consistency.35-37
Traumatic Life Events Questionnaire
Physical or sexual abuse and domestic violence in childhood, as well as current abuse or violence in adulthood, have been found to be associated with functional somatic syndromes in adulthood.29,38,39 This 23-item scale measures 22 types of potentially traumatic events including natural disasters, exposure to warfare, robbery involving a weapon, and physical abuse.40 Three subscales measure the count of events, the count of events associated with fear or helplessness, and the total number of occurrences. It has demonstrated good temporal stability in a variety of populations and also similar rates of trauma exposure when compared with an interview method.40
Perceived Stress Scale
This widely used 10-item scale, designed for community samples, measures the degree to which situations in one’s life are perceived as unpredictable, uncontrollable, and stressful.41 Studies have demonstrated good reliability and validity.42
Symptom Checklist-90-R
Six of nine psychological dimensions (57 items) were selected for this study: somatization, interpersonal sensitivity, depression, anxiety, phobic anxiety, and paranoid ideation.43 Standardized T-scores (mean = 50, SD = 10) according to the SCL-90R manual are reported. The α-coefficients range from 0.77 to 0.90. Test-retest reliability ranges between 0.80 and 0.90 after 1 week of therapy.43 Higher scores on somatization, depression, and anxiety are hypothesized to be associated with greater induction of psychogenic illness.25-27 Phobic anxiety and paranoid ideation were included for exploratory analysis.
Design and procedures
This study was a randomized controlled trial using three groups: Control (no experimental manipulation), Pill-only, and Pill + Media. Each group was assigned to a separate treatment room near the nursing station in a university hospital’s clinical research unit (GCRC). Participants were consented before the experiment began. The control group did not ingest the pill, did not include actors, and did not watch the media. They were engaged in quiet activities, such as reading and conversation.
Two conditions are thought necessary to induce mass psychogenic illness: 1) perceived exposure to an illness-causing agent and 2) observation of other persons’ developing symptoms.
The first was achieved by stating that the rationale of the study was to test the side effects of a new carrier compound for an antiviral medication that would be used to increase bioavailability in the event of pandemic influenza. The volunteers were told that the compound does not produce serious side effects and that the study was conducted to further evaluate milder side effects. In fact, the pill contained cellulose, a benign substance not known to have any side effects.
The second condition, social contagion, was created by placing confederates (professional actors; one male and one female per active experimental group) among the participants in the two Pill groups to feign illness during the study. Nausea, dizziness, and headache were among the symptoms displayed. Prior to the experiment, rehearsals were conducted to standardize the actors’ behavior. The nurses, who did not know who the actors were, attended to all participants who displayed symptoms by taking their blood pressure and pulse more frequently, giving them cool cloths for their forehead, providing bowls for potential vomiting, and sometimes placing them on a gurney outside the experiment room, but within view of the other participants. The actors displayed “sick” behavior through facial expression, posture, and verbalizations.
The second focus of the experiment was to investigate the effect of health media on the induction of psychogenic symptoms. An hour-long Public Television video about the 1918 flu pandemic was viewed by the Pill + Media group only. The video contained interviews with survivors and vivid images of death and illness.
All three groups were identically assessed three times: baseline (before pill or media), 1 hour, and 2 hours after baseline. Participants rated their current symptoms (PILL questionnaire), and nurses measured the participants’ heart rate and blood pressure. Immediately after the baseline assessment, both pill groups ingested the cellulose pill. Approximately 20 minutes later, the actors began to feign symptoms. After the second assessment, the Pill + Media group watched the pandemic documentary. When not engaged in an experiment activity, all participants were free to talk, read, or do other quiet activity.
After the third assessment, each group was read a debriefing statement. It described the true purpose of the study, disclosed the presence of actors, and revealed that the pill was cellulose. Each participant was also interviewed privately with a structured script to ascertain reaction to the experiment and to allow for questions. Participants were contacted 24-48 hours later by telephone or e-mail to ascertain their well-being and determine if symptoms or concerns persisted. This extensive exchange with participants was conducted to make qualitative judgments about the safety of the experiment and to guide modifications for future applications of the experimental protocol.
After debriefing, participants were given the psychosocial risk factor questionnaires to complete within the week and mail back. Previous pilot work had suggested that giving the questionnaires before the experiment would raise suspicions about the true purpose of the study.
Data analysis
Analysis of variance (ANOVA) was used to test for baseline group differences. The primary hypotheses were examined with repeated measures ANOVA for the group by time interactions in planned comparisons. Pearson or Spearman correlations were performed to examine the degree of association between the symptom change scores and the risk factors. Cohen’s d was used to report effect sizes.
Results
Randomization was successful in that the experimental groups did not differ in age, gender, marital status, race, and education (Table 1). Mental and physical health of the study sample was generally better than the US population norm (between the 60th to 70th percentiles) based on the SF36v2 health measure (Table 2).
Table 2.
Means (SD) of self-reported measures of risk factors for psychogenic illness by experimental group
| Measures of psychosocial risk factors | Pill (n = 13) | Pill + Media (n = 15) | Control (n = 10) |
|---|---|---|---|
| NEO-PI Neuroticism Scale | 41.6 (13.4) | 40.7 (14.4) | 38.6 (9.0) |
| Traumatic Life Events Questionnaire | |||
| Count of events | 5.1 (2.6) | 7.4 (5.6) | 3.5 (1.8) |
| Count of events with fear or helplessness | 2.7 (2.2) | 3.9 (4.6) | 1.8 (1.8) |
| Number of total occurrences | 14.2 (9.7) | 21.7 (23.7) | 7.7 (4.7) |
| Perceived Stress Scale | 10.0 (7.0) | 13.3 (6.7) | 8.5 (5.2) |
| Symptom Checklist-90-R | |||
| Somatization | 46.5 (10.1) | 44.1 (10.1) | 44.7 (8.8) |
| Interpersonal sensitivity | 49.9 (11.9) | 54.6 (12.3) | 45.5 (8.5) |
| Anxiety | 44.6 (10.2) | 46.8 (11.9) | 45.4 (11.0) |
| Depression | 51.3 (10.1) | 51.8 (14.1) | 45.0 (13.1) |
| Phobic anxiety | 46.5 (6.6) | 50.4 (10.5) | 47.3 (7.4) |
| Paranoid ideation | 50.5 (9.5) | 53.9 (13.1) | 46.9 (6.7) |
Self-reported symptoms
The first hypothesis was tested by comparing the change in symptoms between assessments 1 and 2 and between 1 and 3 for the two combined Pill groups with the Control group. The results indicate induced psychogenic illness with both Pill groups reporting more symptoms than the Control group from assessments 1 to 2 (t = 1.75, p = 0.085, d = 0.74) and from assessments 1 to 3 (t = 2.97, p = 0.004, d = 0.92). As can be seen in Figure 1, both experimental groups (Pill-only and Pill + Media) showed a similar increase in reported symptoms between assessments when compared with the Control group. On average, the symptom reports by assessment 3 were 11 times higher (2.29 vs 0.20) for the two Pill groups when compared with the Control group. Individual participants reported between 0 and 11 individual symptoms. The most commonly reported symptoms were dry mouth, itchy eyes or skin, headache, pressure in head, blurred vision, fatigue, nausea, indigestion, and coughing. Most symptoms were reported to be of mild intensity.
Figure 1.
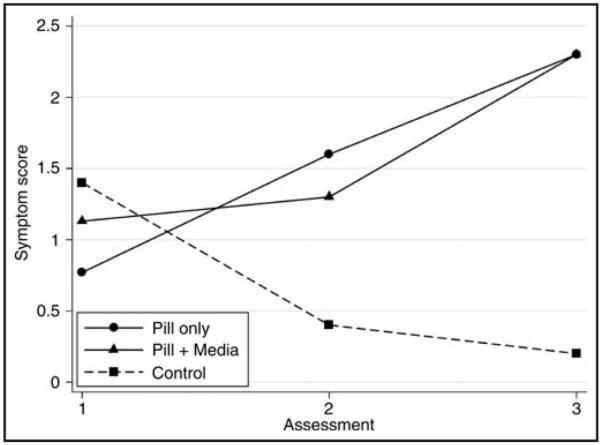
Self-reported symptom score at each assessment by experimental group.
The second hypothesis that media exposure would increase symptom reports was tested by comparing the differential change in symptoms in the Pill and Pill + Media groups from assessment 2 to assessment 3. Between these assessments, the Pill + Media group watched the documentary. Contrary to the hypothesis, the Pill + Media group did not report more symptoms than the Pill-only group (p > 0.72).
Vital signs
All three groups showed a marked reduction in heart rate from assessment 1 to assessment 2 (t = 21.72, p < 0.0001), with no significant difference between the two Pill and Control groups (Figure 2). From assessment 2 to assessment 3, the heart rate continued to decelerate only in the Pill + Media group (t = 1.89, p = 0.06). There were no group effects observed for blood pressure.
Figure 2.
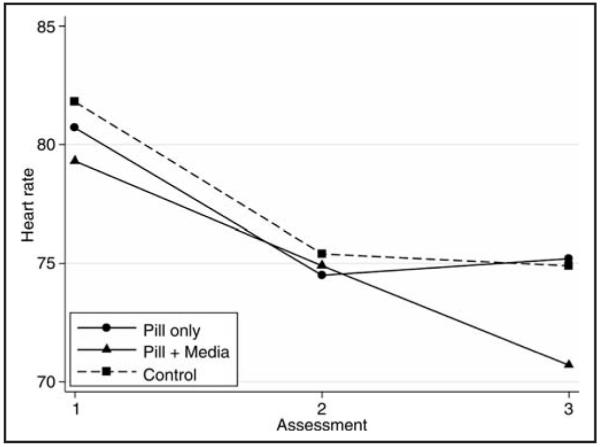
Heart rate at each assessment by experimental group.
Risk factors
All participants returned the psychosocial questionnaires within a week of the experiment. There were no significant differences among the experimental groups on any psychosocial measures (Table 2). When compared with the US population norms, the sample had low levels on several risk factors. The scores on the Perceived Stress Scale were approximately 50 percent lower than those for the US population norms,42 indicating an emotionally robust sample. Likewise, the somatization and anxiety scores on the SCL-90R were about a half SD lower than the general population.
The third hypothesis that risk factors would be associated with level of psychogenic illness induction was tested with correlations among the participants in the two Pill groups (n = 28). The demographic variables, age, gender, and educational status, were not associated. Among the psychosocial measures, total number of traumatic life events in one’s life (Traumatic Life Events Questionnaire) was positively associated with the increase in number of symptoms reported from assessment 1 to assessment 2 (r = 0.41, p = 0.03). There was also the suggestion that depression (SCL90R) may be an important risk factor (r = 0.36, p = 0.06). None of the other predictors approached significance.
Safety of the experiment
All participants reported that they believed the stated rationale of the study and were surprised when informed of the true purpose of the study and the presence of actor confederates. They described the documentary as sad, depressing, and interesting. During interviews, they noted that they felt safe in a hospital environment and did not believe that they would be given anything that would hurt them. The 24- to 48-hour follow-up with all participants indicated that this experiment did not have harmful mental or physical health consequences to study participants.
Discussion
Research on psychological processes in the context of public health disasters is difficult to conduct, and, as a result, little experimental research is available. Disaster planning, especially for hospital surge, maintenance of social distancing, and management of discreet community psychogenic outbreaks, would benefit from a deeper understanding of the phenomenon. This could pave the way for improved procedures for public preparedness, emergency health communications, and triage during a public health disaster. With this goal in mind, we designed an experimental protocol to determine if we could induce psychogenic symptoms in a safe and controlled setting. Unlike prior experimental work with college students,19-22 we studied community adults in a protocol simulating a plausible public health scenario. We also incorporated a probe of the effects of content-related media on symptom induction. Because of the novel nature of this investigation and the priority of protecting research volunteers, eligibility criteria excluded participants with any acute or chronic medical or psychological condition. This resulted in a sample that was healthier than the general population and that had fewer psychological risk factors for psychogenic illness.
Despite these constraints, this protocol was successful in inducing psychogenic symptoms relative to the control group. Study participants who were given the “antiviral compound pill” and who were exposed to confederates who feigned illness reported symptoms 11 times greater than the control group. There was variability across participants in that some reported no symptoms, whereas others reported up to 11 different symptoms. In the context of a public health emergency, the reported symptoms would indicate the need for medical evaluation. Interestingly, both men and women were vulnerable to experiencing psychogenic illness, a finding also observed by Lorber.20
One explanation for the symptom induction could be the expectations generated by the symptoms listed in the consent form as possible reactions. Lorber et al.20 found that their participants’ psychogenic symptoms were higher for the four symptoms that were suggested compared with another four symptoms that were not. Our consent form listed 15 symptoms as examples. Among these, only five symptoms were reported by participants, and they are some of the most typical non-specific symptoms (eg, nausea, headache, and fatigue); and 10 of the suggested symptoms were not reported. In addition, nine other symptoms that were not suggested on the consent were reported, including blurred vision, skin rash, and pressure in head. The social contagion (confederate actors) in the experiment was also an important source of suggestion. Their illness behavior demonstrated that the administered pill could cause symptoms. However, the study participants’ symptom reports were also more extensive than those displayed by the actors. Thus, we believe that this is an evidence that participants’ experience of psychogenic illness is more complex than a simple reflection of suggested symptoms. The literature on unexplained medical symptoms finds that reported symptoms reflect the somatic sensations perceived during vigilant self-assessment.25,44 Furthermore, the presence of a plausible agent facilitates the attribution of somatic sensations—that might normally be ignored—to the agent.45,46
It is noteworthy that all three groups reported more symptoms in assessment 1 than the control group reported in assessments 2 and 3. We speculate that this reflected initial anxiety about the study, which was allayed for the control participants when they learned that they would not receive the pill, but not allayed for the two other groups.
The second hypothesis stated that the Pill + Media group would report higher rates of psychogenic symptoms than the Pill-only group. This hypothesis was not supported. Both groups showed a continued increase in symptoms between assessments 2 and 3, with no differential increase in the Pill + Media group. One possible conclusion is that media does not exacerbate psychogenic symptoms. Another conclusion is that our media selection, an historical documentary, may not have been sufficiently analogous to the news reports that have been observed to exacerbate psychogenic outbreaks.3,47
We expected that heart rate and blood pressure would reflect arousal and anxiety, presumed facilitators of the psychogenic illness response. The physiological measures did not yield a systematic pattern other than a drop in heart rate across assessments. As we suggested for the higher rate of symptoms at baseline, this may indicate a reduction in arousal after beginning the experiment.48 It may further suggest that induction of mass psychogenic illness is not simply an anxiety or arousal response, as heart rate returned to a more normative level while symptoms increased in the two Pill groups. In fact, we observed a marked decrease in heart rate for the media group. This is consistent with the phenomenon of tonic deceleration, reported in the media literature, in which heart rate decelerates in response to orienting toward and attention to a negative or threatening stimulus.49 The slowed heart rate confirms that our participants were paying attention to the documentary, although their interview reports of sadness and concern did not escalate the psychogenic illness process.
Studies of disaster media exposure suggest that higher rates of media exposure are positively associated with post-traumatic stress disorder and depression.23,24 Media exposure is also reported to enhance the spread of psychogenic illness in perceived “toxic exposure” situations.3,47 Vasterman et al.50 concluded that “people tend to adopt the explanations offered by the media and integrate them into their story about their own health complaints.” Alternatively, the media has also demonstrated the potential to convey accurate information and realistic messages of hope as an alternative to media hype and risk amplification.50,51 These contrasting approaches and outcomes during disaster reporting need to be investigated in controlled experimental conditions to determine their validity; only then we will have the information necessary to generate scientifically sound recommendations for public health authorities and the public media.
The third focus of the study was the relationship of psychogenic illness risk factors and the observed induction in this study. Of the risk factors measured, two variables emerged as suggesting higher vulnerability to psychogenic illness: the number of lifetime traumatic life events and level of depression. The failure to find more associations may reflect the above-average mental and physical health of our study population and the small sample size. We would expect potentially more relationships in a larger study population that is more representative of the general population.
In conclusion, this study successfully used an experimental protocol to induce psychogenic symptoms in a mentally and physically healthy community population in the context of a medical event. It confirms that there is a safe and feasible way to experimentally induce psychogenic symptoms in a community population. This line of research holds the potential to improve the management of large-scale biological events. Further development is warranted to maximize the induction of psychogenic symptoms as well as to confirm its safety and reliability in larger, varied study populations. Demographic and psychological characteristics of individuals who are predisposed to develop psychogenic illness should be further studied to identify those most at risk. This would allow testing of strategies for educating individuals and healthcare providers to prevent, recognize, and manage psychogenic symptoms, thereby reducing the healthcare and economic burden. In addition, we need to clarify what role, if any, media plays in the spread of psychogenic illness so that we can provide health information to the public that minimizes psychogenic symptoms.
Acknowledgments
The authors express their gratitude to Doerte Junghaenel, PhD, Susan Donelan, MD, Dianne Pagani, the research team, and GCRC staff for their assistance in conducting this study, and the Clinical Skills Center for training the actors. Arthur A. Stone, PhD, and Stefan Schneider, PhD, provided statistical assistance. This research was supported by grants to Joan E. Broderick, PhD, principal investigator, from the National Institutes of Health (1R21LM009819), GCRC Grant (M01-RR10710) from the National Center for Research Resources, and by Stony Brook University Medical Center Targeted Research Opportunities Program: Pandemic Influenza-Related Research Award.
Contributor Information
Joan E. Broderick, Department of Psychiatry and Behavioral Science, Stony Brook University, Stony Brook, New York..
Evonne Kaplan-Liss, Department of Preventive Medicine and School of Journalism, Stony Brook University, Stony Brook, New York..
Elizabeth Bass, Center for Communicating Science, School of Journalism, Stony Brook University, Stony Brook, New York..
References
- 1.Drazen JM. SARS—Looking back over the first 100 days. N Engl J Med. 2003;349(4):319–320. doi: 10.1056/NEJMp038118. [DOI] [PubMed] [Google Scholar]
- 2.Johnson NP, Mueller J. Updating the accounts: Global mortality of the 1918-1920 “Spanish” influenza pandemic. Bull Hist Med. 2002;76(1):105–115. doi: 10.1353/bhm.2002.0022. [DOI] [PubMed] [Google Scholar]
- 3.Jones TF, Craig AS, Hoy D, et al. Mass psychogenic illness attributed to toxic exposure at a high school. N Engl J Med. 2000;342(2):96–100. doi: 10.1056/NEJM200001133420206. [DOI] [PubMed] [Google Scholar]
- 4.Knudson GB. Nuclear, biological, and chemical training in the U.S. Army Reserves: Mitigating psychological consequences of weapons of mass destruction. Mil Med. 2001;166(12 Suppl):63–65. [PubMed] [Google Scholar]
- 5.Clements CJ. Mass psychogenic illness after vaccination. Drug Saf. 2003;26(9):599–604. doi: 10.2165/00002018-200326090-00001. [DOI] [PubMed] [Google Scholar]
- 6.Boss LP. Epidemic hysteria: A review of the published literature. Epidemiol Rev. 1997;19(2):233–243. doi: 10.1093/oxfordjournals.epirev.a017955. [DOI] [PubMed] [Google Scholar]
- 7.Bartholomew RE. Rethinking the dancing mania. Vol. 24.4. The Committee for Skeptical Inquiry; [Accessed September 28, 2010]. July/August, 2000. Available at http://www.csicop.org/si/show/rethinking_the_dancing_mania. [Google Scholar]
- 8.Pastel RH, Mulvaney J. Fear of radiation in U.S. military medical personnel. Mil Med. 2001;166(12 Suppl):80–82. [PubMed] [Google Scholar]
- 9.White PD, Moorey S. Psychosomatic illnesses are not “all in the mind”. J Psychosom Res. 1997;42(4):329–332. doi: 10.1016/s0022-3999(96)00296-6. [DOI] [PubMed] [Google Scholar]
- 10.Kharabsheh S, Al-Otoum H, Clements J, et al. Mass psychogenic illness following tetanus-diphtheria toxoid vaccination in Jordan. Bull World Health Organ. 2001;79(8):764–770. [PMC free article] [PubMed] [Google Scholar]
- 11.Hefez A. The role of the press and the medical community in the epidemic of “mysterious gas poisoning” in the Jordan West Bank. Am J Psychiatry. 1985;142(7):833–837. doi: 10.1176/ajp.142.7.833. [DOI] [PubMed] [Google Scholar]
- 12.Page LA, Petrie KJ, Wessely SC. Psychosocial responses to environmental incidents: A review and a proposed typology. J Psychosom Res. 2006;60(4):413–422. doi: 10.1016/j.jpsychores.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Winters W, Devriese S, Van Diest I, et al. Media warnings about environmental pollution facilitate the acquisition of symptoms in response to chemical substances. Psychosom Med. 2003;65(3):332–338. doi: 10.1097/01.psy.0000041468.75064.be. [DOI] [PubMed] [Google Scholar]
- 14.Yzermans CJ, Donker GA, Kerssens JJ, et al. Health problems of victims before and after disaster: A longitudinal study in general practice. Int J Epidemiol. 2005;34(4):820–826. doi: 10.1093/ije/dyi096. [DOI] [PubMed] [Google Scholar]
- 15.ten Veen PM, Morren M, Yzermans CJ. The influence of news events on health after disaster: A longitudinal study in general practice. J Trauma Stress. 2009;22(6):505–515. doi: 10.1002/jts.20462. [DOI] [PubMed] [Google Scholar]
- 16.Smithson A. Rethinking the lessons of Tokyo. In: Smithson A, Levy L, editors. Ataxia: The Chemical and Biological Terrorism Threat and the US Response. The Henry Stimson Center; Washington, DC: 2000. pp. 71–111. [Google Scholar]
- 17.Bootsma MCJ, Ferguson NM. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc Natl Acad Sci USA. 2007;104(18):7588–7593. doi: 10.1073/pnas.0611071104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci USA. 2007;104(18):7582–7587. doi: 10.1073/pnas.0610941104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lindberg MA. The role of suggestions and personality characteristics in producing illness reports and desires for suing the responsible party. J Psychol. 2002;136(2):125–140. doi: 10.1080/00223980209604144. [DOI] [PubMed] [Google Scholar]
- 20.Lorber W, Mazzoni G, Kirsch I. Illness by suggestion: Expectancy, modeling, and gender in the production of psychosomatic symptoms. Ann Behav Med. 2007;33(1):112–116. doi: 10.1207/s15324796abm3301_13. [DOI] [PubMed] [Google Scholar]
- 21.Mazzoni G, Foan L, Hyland ME, et al. The effects of observation and gender on psychogenic symptoms. Health Psychol. 2010;29(2):181–185. doi: 10.1037/a0017860. [DOI] [PubMed] [Google Scholar]
- 22.Lange LJ, Piette JD. Perceived health status and perceived diabetes control: Psychological indicators and accuracy. J Psychosom Res. 2005;58(2):129–137. doi: 10.1016/j.jpsychores.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 23.Schuster MA, Stein BD, Jaycox LH, et al. A national survey of stress reactions after the September 11, 2001, terrorist attacks. N Engl J Med. 2001;345(20):1507–1512. doi: 10.1056/NEJM200111153452024. [DOI] [PubMed] [Google Scholar]
- 24.Schlenger WE, Caddell JM, Ebert L, et al. Psychological reactions to terrorist attacks: Findings from the National Study of Americans’ Reactions to September 11. JAMA. 2002;288(5):581–588. doi: 10.1001/jama.288.5.581. [DOI] [PubMed] [Google Scholar]
- 25.Barsky AJ, Borus JF. Functional somatic syndromes. Ann Int Med. 1999;130(11):910–921. doi: 10.7326/0003-4819-130-11-199906010-00016. [DOI] [PubMed] [Google Scholar]
- 26.Barsky AJ, Orav EJ, Bates DW. Distinctive patterns of medical care utilization in patients who somatize. Med Care. 2006;44(9):803–811. doi: 10.1097/01.mlr.0000228028.07069.59. [DOI] [PubMed] [Google Scholar]
- 27.Kroenke K, Spitzer RL, Williams JBW, et al. Physical symptoms in primary care: Predictors of psychiatric disorders and functional impairment. Arch Fam Med. 1994;3(9):774–779. doi: 10.1001/archfami.3.9.774. [DOI] [PubMed] [Google Scholar]
- 28.Watson D, Clark LA. Negative affectivity: The disposition to experience aversive emotional states. Psychol Bull. 1984;96(3):465–490. [PubMed] [Google Scholar]
- 29.Craig T, Boardman A, Mills K, et al. The South London Somatisation Study. I. Longitudinal course and the influence of early life experiences. Br J Psychiatry. 1993;163(5):579–588. doi: 10.1192/bjp.163.5.579. [DOI] [PubMed] [Google Scholar]
- 30.Escobar JI, Burnam MA, Karno M, et al. Somatization in the community. Arch Gen Psychiatry. 1987;44(8):713–718. doi: 10.1001/archpsyc.1987.01800200039006. [DOI] [PubMed] [Google Scholar]
- 31.Swartz M, Blazer D, George L, et al. Somatization disorder in a community population. Am J Psychiatry. 1986;143(11):1403–1408. doi: 10.1176/ajp.143.11.1403. [DOI] [PubMed] [Google Scholar]
- 32.Kroenke K, Spitzer RL. Gender differences in the reporting of physical and somatoform symptoms. Psychosom Med. 1998;60(2):150–155. doi: 10.1097/00006842-199803000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Ware JE, Kosinski M, Dewey JE. How to Score Version 2 of the SF-36 Health Survey. QualityMetric, Incorporated; Lincoln, RI: 2000. [Google Scholar]
- 34.Pennebaker JW. The Psychology of Physical Symptoms. Springer-Verlag; New York: 1982. [Google Scholar]
- 35.Costa PT, McCrae RR. The NEO Personality Inventory Manual. Psychological Assessment Resources; Odessa, FL: 1985. [Google Scholar]
- 36.Watson D, Pennebaker JW. Health complaints, stress, and distress: Exploring the central role of negative affectivity. Psychol Rev. 1989;96(2):234–254. doi: 10.1037/0033-295x.96.2.234. [DOI] [PubMed] [Google Scholar]
- 37.Hultsch DF, Hertzog C, Dixon RA, et al. Memory Change in the Aged. Cambridge University Press; Cambridge, England: 1998. [Google Scholar]
- 38.Walker E, Katon W, Hansom J, et al. Medical and psychiatric symptoms in women with childhood sexual abuse. Psychosom Med. 1992;54(6):658–664. doi: 10.1097/00006842-199211000-00005. [DOI] [PubMed] [Google Scholar]
- 39.McCauley J, Kern D, Kolodner K, et al. Relation of low-severity violence to women’s health. J Gen Intern Med. 1998;13(10):687–691. doi: 10.1046/j.1525-1497.1998.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kubany ES, Leisen MB, Kaplan AS, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psycholog Assess. 2000;12(2):210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- 41.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 42.Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health: The Claremont Symposium on Applied Social Psychology. Sage Publications; Newbury Park, CA: 1988. pp. 31–67. [Google Scholar]
- 43.Derogatis LR. SCL-90-R: Symptom checklist-90-R: Administration, Scoring and Procedures Manual. 3rd ed National Computer Systems, Inc.; Minneapolis, MN: 1994. [Google Scholar]
- 44.Serlie AW, Erdman RA, Passchier J, et al. Psychological aspects of non-cardiac chest pain. Psychother Psychosom. 1995;64(2):62–73. doi: 10.1159/000288993. [DOI] [PubMed] [Google Scholar]
- 45.Schachter S, Singer JE. Cognitive, social, and physiological determinants of emotional state. Psychol Rev. 1962;69:379–399. doi: 10.1037/h0046234. [DOI] [PubMed] [Google Scholar]
- 46.Leventhal H, Meyer D, Nerenz D. The common sense representation of illness danger. In: Rachman S, editor. Contributions to Medical Psychology. Pergamon Press; New York: 1980. pp. 7–30. [Google Scholar]
- 47.Gallay A, Van Loock F, Demarest S, et al. Belgian coca-cola-related outbreak: Intoxication, mass sociogenic illness, or both? Am J Epidemiol. 2002;155(2):140–147. doi: 10.1093/aje/155.2.140. [DOI] [PubMed] [Google Scholar]
- 48.Waugh CE, Panage S, Mendes WB, et al. Cardiovascular and affective recovery from anticipatory threat. Biol Psychol. 2010;84(2):169–175. doi: 10.1016/j.biopsycho.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schwerdtfeger A. Trait anxiety and autonomic indicators of the processing of threatening information: A cued S1-S2 paradigm. Biol Psychol. 2006;72(1):59–66. doi: 10.1016/j.biopsycho.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 50.Vasterman P, Yzermans CJ, Dirkzwager AJE. The role of the media and media hypes in the aftermath of disasters. Epidemiol Rev. 2005;27(1):107–114. doi: 10.1093/epirev/mxi002. [DOI] [PubMed] [Google Scholar]
- 51.Njenga FG, Nyamai C, Kigamwa P. Terrorist bombing at the USA Embassy in Nairobi: The media response. East Afr Med J. 2003;80(3):159–164. doi: 10.4314/eamj.v80i3.8686. [DOI] [PubMed] [Google Scholar]


