Abstract
Background
Laparoscopic surgery has gained popularity over open conventional surgery as it offers benefits to both patients and health care practitioners. Although the overall risk of complications during laparoscopic surgery is recognized to be lower than during laparotomy, inadvertent serious complications still occur. Creation of the pneumoperitoneum and placement of laparoscopic ports remain a critical first step during endoscopic surgery. It is estimated that up to 50% of laparoscopic complications are entry-related, and most injury-related litigations are trocar-related. We sought to evaluate the current practice of laparoscopic entry among Canadian general surgeons.
Methods
We conducted a national survey to identify general surgeon preferences for laparoscopic entry. Specifically, we sought to survey surgeons using the membership database from the Canadian Association of General Surgeons (CAGS) with regards to entry methods, access instruments, port insertion sites and patient safety profiles. Laparoscopic cholecystectomy was used as a representative general surgical procedure.
Results
The survey was completed by 248 of 1000 (24.8%) registered members of CAGS. Respondents included both community and academic surgeons, with and without formal laparoscopic fellowship training. The demographic profile of respondents was consistent nationally. A substantial proportion of general surgeons (> 80%) prefer the open primary entry technique, use the Hasson trocar and cannula and favour the periumbilical port site, irrespective of patient weight or history of peritoneal adhesions. One-third of surgeons surveyed use Veress needle insufflation in their surgical practices. More than 50% of respondents witnessed complications related to primary laparoscopic trocar insertion.
Conclusion
General surgeons in Canada use the open primary entry technique, with the Hasson trocar and cannula applied periumbilically to establish a pneumoperitoneum for laparoscopic surgery. This surgical approach is remarkably consistent nationally, although considerably variant across other surgical subspecialties. Peritoneal entry remains an important patient safety issue that requires ongoing evaluation and study to ensure translation into safe contemporary clinical practice.
Abstract
Contexte
La chirurgie laparoscopique a gagné en popularité par rapport à la chirurgie ouverte classique en raison des avantages qu’elle offre, tant pour les patients que pour les professionnels de la santé. Même si on reconnaît que le risque global de complications est moindre durant la chirurgie laparoscopique que durant la laparotomie, il survient parfois par inadvertance des complications graves. La création d’un pneumopéritoine et l’installation des dispositifs d’accès laparoscopiques demeurent une première étape cruciale lors de toute chirurgie endoscopique. On estime que jusqu’à 50 % des complications laparoscopiques sont liées à l’insertion et que la plu-part des poursuites pour traumatisme mettent en cause une lésion causée par le trocart lui-même. Nous avons voulu évaluer la pratique actuelle des chirurgiens généraux canadiens en matière d’insertion des instruments laparoscopiques.
Méthodes
Nous avons réalisé un sondage à l’échelle nationale pour connaître les préférences des chirurgiens généraux en matière d’insertion laparoscopique. Plus spécifiquement, nous avons voulu interroger les chirurgiens inscrits à la base de don-nées des membres de l’Association canadienne des chirurgiens généraux (ACCG) en ce qui a trait aux méthodes d’insertion, aux instruments d’accès, à la localisation des dispositifs d’insertion et aux profils de sécurité des patients. On a utilisé la cholécystectomie laparoscopique comme intervention type en chirurgie générale.
Résultats
Parmi les 1000 membres inscrits de l’ACCG, 248 (24,8 %) ont répondu au sondage. Les répondants provenaient du milieu communautaire et universitaire et pouvaient ou non avoir suivi un stage formel en laparoscopie. Le profil démographique des répondants était uniforme à l’échelle nationale. Une proportion substantielle (> 80 %) de chirurgiens généraux préfèrent la technique d’insertion primaire ouverte, utilisent un trocart et une canule de Hasson et privilégient la région périombilicale pour l’insertion, indépendamment du poids ou des antécédents d’adhérences péritonéales des patients. Le tiers des chirurgiens interrogés utilisent l’insufflation par aiguille de Veress dans leurs pratiques. Plus de 50 % des répondants ont été témoins de complications liées à l’insertion de trocarts laparoscopiques au site de l’orifice primaire.
Conclusion
Les chirurgiens généraux du Canada utilisent la technique d’insertion primaire ouverte avec trocart et canule de Hasson et privilégient la région périombilicale pour établir un pneumopéritoine en vue de la chirurgie laparoscopique. Cette approche chirurgicale semble appliquée avec une remarquable constance à l’échelle nationale, mais varie considérablement parmi les autres spécialités chirurgicales. La question de l’insertion péritonéale demeure importante pour la sécurité des patients et il faudra continuer à évaluer et à examiner cet enjeu pour assurer une pratique clinique moderne sécuritaire.
Laparoscopic surgery has revolutionized the practice of most surgical subspecialties over the past 2 decades. In general, laparoscopic surgery results in smaller scars, less postoperative pain and a quicker recovery when compared with laparotomy.1,2 Furthermore, there is evidence to suggest that the overall risk of complications following laparoscopic surgery is lower than with laparotomy.3,4 Despite the relative safety of laparoscopic techniques, inadvertent serious injuries to bowel, bladder and vascular structures do occur.5,6 It is recognized that the most common cause of serious laparoscopic complications are related to primary trocar insertion.7,8
Most laparoscopic surgical procedures require establishment of a pneumoperitoneum and placement of peritoneal ports. There are many techniques and devices available that afford safe laparoscopic entry; however, there is currently no uniform consensus as to the optimal approach. Specifically, entry techniques include the noninsufflated open (Hasson) method; the conventional closed entry method with Veress needle CO2 preinsufflation; and the optical entry methods that include the visual Veress needle system, the disposable optical trocars and the trocarless reusable threaded visual cannula system (EndoTIP; Box 1). It is possible that surgeons’ preferences for laparoscopic entry will vary depending on their training (specialty and subspecialty), geographic location and clinical experiences.
Box 1. Contemporary primary peritoneal entry methods.
Noninsufflated entry method
Direct trocar and cannula
Open trocar and cannula
Preinsufflated entry method with Veress needle
Conventional closed trocar and cannula
Shielded trocar and cannula
Radially expanding trocar and cannula
Visual entry method (with or without preinsufflation)
Visual Veress needle
Visual disposable trocar and cannula
Visual reusable (EndoTIP) cannula
A recent Cochrane review of laparoscopic entry techniques failed to demonstrate any evidence of benefit in terms of safety of one technique over another.9 Moreover, in an effort to mitigate inadvertent laparoscopic entry mishaps, improve patient safety and harmonize clinical practice, several international surgical bodies, including the European Association of Surgery (EAS) and the Society of Obstetricians and Gynaecologists of Canada (SOGC), have recently published laparoscopic entry clinical practice guidelines (CPGs).10,11 Interestingly, despite several similar international risk management efforts, surveys of practitioners in Canada and the United Kingdom have revealed heterogeneity in laparoscopic entry practices that are not always consistent with contemporary recommendations.12,13
We aimed to evaluate the current practice patterns of general surgeons in Canada regarding laparoscopic entry. Specifically, we sought to analyze data according to demographic factors (e.g., region, sex, training, years of clinical experience) and compare practice patterns to recently published CPGs to increase awareness of all available peritoneal entry options.
Methods
We conducted a national survey to evaluate surgeon preferences for laparoscopic port creation. Specifically, we sought to survey general surgeons with regards to surgical technique, laparoscopic entry device use and safety profile during laparoscopic cholecystectomy. We obtained research ethics board approval from the St. Joseph’s Health Centre, University of Toronto.
Surveys were conducted using the national membership database from a subspecialty surgical society (Canadian Association of General Surgeons; CAGS). All laparoscopic entry methods were clearly defined at the start of the survey.
The survey questionnaire packages with a pledge of strict confidentiality and anonymity were forwarded via email and surface mail to all practising Canadian general surgeons who were members of CAGS. The paper version was developed using the TeleForm program to allow collected responses to be digitally entered using optical character recognition. We created the electronic survey forms using the SurveyMonkey Web survey system. Surveys were translated into French for francophone respondents to enhance participation.
The electronic survey was distributed by CAGS via their monthly webpage publication. Paper surveys were subsequently mailed with a self-addressed, stamped envelope to all CAGS members early in 2009. Members were instructed to complete either the electronic or paper questionnaire, but not both.
Statistical analysis
We collated and evaluated the results from the paper and email formats. We compiled, codified and entered survey responses into a database. Data analysis was performed using the statistical program SPSS 17.0 (SPSS Inc.). Statistical significance was calculated with χ2 analysis.
Results
The survey was sent to 1000 practising general surgeons (the total membership of CAGS in 2008) and generated a total of 248 responses (24.8% response rate). Respondents included both community and academic surgeons with and without formal laparoscopic fellowship training. In all, 242 (97.6%) respondents indicated that they currently perform laparoscopic surgery. The demographic profile of respondents is summarized in Table 1: 80.8% were men, and most (62%) had been in practice for more than 10 years. In general, the geographic provincial representation of respondents appears to reflect the relative population base for each province and territory in Canada. Statistical analyses revealed no significant differences in response rates based on demographic factors.
Table 1.
Demographic characteristics of general surgeons responding to a survey on laparoscopic entry practices
| Characteristic | No. (%) |
|---|---|
| Sex | |
| Male | 189 (80.8) |
| Female | 45 (19.2) |
| Location of practice | |
| Alberta | 28 (12.1) |
| British Columbia | 36 (15.5) |
| Manitoba | 7 (3.0) |
| New Brunswick | 7 (3.0) |
| Newfoundland and Labrador | 4 (1.7) |
| Northwest Territories | 0 (0) |
| Nova Scotia | 14 (6.0) |
| Nunavut | 0 (0) |
| Ontario | 91 (39.2) |
| Prince Edward Island | 2 (0.9) |
| Quebec | 32 (13.8) |
| Saskatchewan | 7 (3.0) |
| Yukon | 1 (0.4) |
| Outside Canada | 3 (1.3) |
| Language | |
| English | 226 (91.1) |
| French | 22 (8.9) |
| Number of years in practice | |
| < 1 | 3 (1.3) |
| 1–5 | 37 (15.8) |
| 6–10 | 49 (20.9) |
| > 10 | 145 (62.0) |
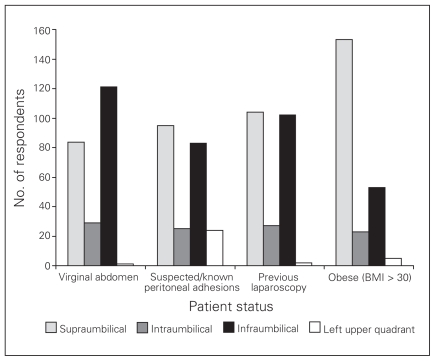
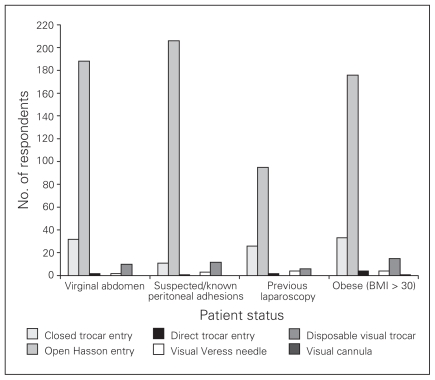
The preferred laparoscopic primary entry locations, instruments and methods for general surgeons are summarized in Figures 1 and 2. In a virginal abdomen, the umbilical region is the primary port site of choice with 51.5% of surgeons favouring infraumbilical and 35.7% preferring supraumbilical entry locations. The most common laparoscopic primary entry method used by Canadian general surgeons is the open Hasson entry technique (80.3%). A smaller proportion of surgeons (13.7%) reported using a closed Veress-insufflated trocar and cannula entry method. About 4.3% reported using the disposable visual trocar for peritoneal entry.
Fig. 1.
Preferred primary peritoneal entry location.
Fig. 2.
Preferred primary peritoneal entry method. Note that no surgeons indicated a preference for radially expanding trocar.
When peritoneal adhesions are known to exist or are suspected, the umbilical site remains the most popular choice of entry location (41.9% supraumbilical, 36.6% infraumbilical); however, in this situation, 10.6% of general surgeons reported preferring the left upper quadrant port placement site. Use of the open Hasson cannula entry technique is more prevalent when peritoneal adhesions are suspected, with 88.4% of surgeons favouring this approach. When performing an elective laparoscopic operation, such as a cholecystectomy, Canadian general surgeons clearly prefer open periumbilical port insertion, irrespective of previous abdominal surgery.
It appears that general surgeons prefer to place supraumbilical ports (65.4%) versus infraumbilical (22.6%) primary ports in obese patients.
In all, 35.3% of general surgeons reported using a Veress needle in their surgical practices. To verify correct placement of the Veress needle, 87.7% of surgeons used the “double click sound test,” and 71.6% of respondents anticipated an initial intraperitoneal pressure of less than 10 mm Hg. The preferred pressure before inserting the primary trocar was reported to be less than 15 mm Hg among 91.7% of respondents. Surgeons were questioned as to their strategies when incorrect Veress needle placement was suspected: 82.7% would reinsert the needle, 59.3% would lift the anterior abdominal wall, 39.5% would use an alternate insufflation location and 46.9% would attempt an alternate primary entry method. When the needle required reinsertion, most general surgeons reported that they would make 2 (47.6%) or 3 (41.5%) additional attempts before considering an alternate entry method or location.
A total of 57.3% of respondents had either experienced or witnessed a serious laparoscopic primary port entry complication. Most of the complications were related to the open Hasson entry method (56.6%), the Veress needle insertion (47.8%) or the closed trocar entry after Veress needle insufflation (27.9%). Most complications were identified intraoperatively (88.3%), with only 7.3% identified after patient discharge from hospital. The reported complications included injuries to the small bowel (71.4%), large bowel (25.6%), large vessel (25.6%), omentum (9.8%) and small vessel (9.8%).
Remarkably, respondents indicated that 77.5% of primary trocar complications resulted in some form of permanent injury, with an estimated 3.1% resulting in patient death. Seventy-one percent of respondents reported that entry-related complications did not result in subsequent litigation on the part of the patient.
Secondary port entry complications were either experienced or witnessed by 22.7% of respondents. Interestingly, when a secondary entry complication occurred, 79.2% of surgeons reported that the secondary port had been inserted under direct vision. Most of these secondary port complications were identified intraoperatively (79.6%), whereas 11.1% were identified after patient discharge from hospital.
Injuries to the small vessels, such as the inferior epigastric artery and vein, were reported to constitute about 52% of secondary port complications. Respondents also reported injuries to the small bowel (26%), large bowel (18%), bladder (10%) and large vessels (8%). Again, most respondents (80.4%) indicated that these complications resulted in permanent injuries; however, none resulted in death. Most surgeons (75%) indicated that complications resulting from secondary port placement did not result in litigation.
Discussion
The establishment of laparoscopic ports is an essential component of most endoscopic surgical procedures. Although relatively rare, entry-related complications are estimated to account for about one-fifth of all laparoscopy medical liability insurance claims.14–17 Our study indicated that more than half of practising general surgeons in Canada had witnessed a serious complication related to primary port access.
A recent review of entry-related complications in malpractice claims filed in the Netherlands from 1993 to 2005 revealed that claims were equally divided between general surgeons and gynecologists.14 Although a considerable number of publications on laparoscopic entry are from gynecologic surgeons,18–21 our survey response from 248 practising general surgeons seems to indicate serious interest among general surgeons in laparoscopic port safety issues and emerging technologies.
This national laparoscopic entry survey had an acceptable response rate and conveyed current laparoscopic entry practices among Canadian general surgeons. There were no recognized differences in practice patterns associated with geographic location, sex and number of years in practice. Our data indicate that about 80% of Canadian general surgeons favour the open Hasson cannula insertion technique for elective laparoscopy. This is consistent with published literature in both North America and Europe.22–24 This open technique contrasts the preferred closed Veress needle insufflation primary entry technique favoured by about 80% of gynecologists.12 The reasoning behind this striking contrast in laparoscopic entry techniques between surgical disciplines is difficult to explain; however, it appears to be related to teaching patterns during residency and clinical experience.
Although open laparoscopy is intended to avoid major vessel and bowel entry injury, inadvertent serious primary port insertion mishaps are not entirely eliminated.25–28
There are several publications extolling the safety of a given laparoscopic primary entry technique; however, a recent comprehensive Cochrane review on the topic failed to reveal any significant differences among contemporary techniques.9 This likely reflects the limited statistical power to demonstrate a difference between these techniques when the incidence of vessel and bowel injury is so low. Despite the extremely low incidence of serious complications, 2 separate meta-analyses have demonstrated statistically higher rates of vascular and bowel injury with closed versus open laparoscopy.29,30 The fact that more than 35% of general surgeons selectively use the Veress needle in their practices indicates some variance with regards to laparoscopic access capabilities and choice.
Survey respondents also clearly described their preference for a periumbilical primary entry location. Published guidelines advocate the use of the left upper quadrant port entry site as a default location in high-risk and obese patients and in patients with suspected peritoneal adhesions.31,32 The reasons are that there is usually less subcutaneous fat in the left upper quadrant than the periumbilical region, that the likelihood of parietal peritoneal bowel adhesions is generally rare and that the insertion of parietal peritoneum and abdominal muscles to the lower costal margin offers counter-pressure to the advancing trocar. These, among other factors, are believed to protect against unintended visceral injury during peritoneal entry overshoot. It is recommended that all practising general surgeons be familiar with this safe entry location. Despite these recommendations, only 10.6% of practising general surgeons reported using the left upper quadrant primary port entry site when umbilical adhesions were suspected, and only 2% of surgeons used this site in obese patients.
There appears to be an appropriate level of intraoperative vigilance among general surgeons regarding port entry injuries, given that most primary and secondary port mishaps were recognized at the time of laparoscopy. Evidence suggests that failure to indentify intraoperative laparoscopic port entry injuries leads to serious morbidity and increased mortality.33,34 Interestingly, it appears from our survey that few laparoscopic entry complications were reported to result in medicolegal litigation.
Patients with previous abdominal surgery and those known to have peritoneal adhesions present a higher risk for peritoneal entry complications.35 When consenting to surgery, high-risk patients must be preoperatively informed of the possibility of alternate entry method (visual entry), the probability of a different access site (left upper quadrant) or the likelihood of conversion to laparotomy.36
Peritoneal entry is a critical initial step in most laparoscopic procedures. Our national survey indicates that Canadian general surgeons favour a remarkably uniform technical approach to establishing peritoneal ports and pneumoperitoneum. This approach is consistent across all provinces yet considerably different from reported gynecology practices, reflecting an apparent discipline disconnect between specialties.
Admittedly, several aspects of laparoscopic port dynamics and patient safety remain unclear and need to be elucidated. Given the importance of patient safety and surgical risk management in minimally invasive surgery, further evaluation will be necessary to determine factors influencing the manner by which endoscopists evaluate, teach and adopt emerging laparoscopic entry technologies in Canada.
Acknowledgments
The authors appreciate the invaluable assistance of Mr. Roger Harris, Director of Audio-Visual Services and Ms. Barbara Iwasiuk, librarian, George Pennal Research Library, St. Joseph’s Health Centre, during preparation of this paper.
Footnotes
Competing interests: None declared for Dr. Compeau and Ms. McLeod. Dr. Ternamian declared having received speaker fees and travel assistance from Bayer, Johnson & Johnson, Storz and Abbott.
Contributors: Drs. Compeau and Ternamian designed the study, analyzed the data and wrote the article. All authors acquired the data and approved the article’s publication.
References
- 1.Chapron C, Fauoconnier A, Goffinet F, et al. Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynaecological pathology: results of meta-analysis. Hum Reprod. 2002;17:1334–42. doi: 10.1093/humrep/17.5.1334. [DOI] [PubMed] [Google Scholar]
- 2.Harrell AG, Heniford BT. Minimally invasive abdominal surgery: lux et ventas past, present, and future. Am J Surg. 2005;190:239–43. doi: 10.1016/j.amjsurg.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 3.Jansen FW, Kapiteyn K, Trimpos T, et al. Complication of laparoscopy: a prospective multicentre observational study. Br J Obstet Gynaecol. 1997;104:595–600. doi: 10.1111/j.1471-0528.1997.tb11539.x. [DOI] [PubMed] [Google Scholar]
- 4.Palmer R. Safety in laparoscopy. J Reprod Med. 1974;13:1–5. [PubMed] [Google Scholar]
- 5.Jansen FW, Kolman W, Bakkum EA, et al. Complications of laparoscopy: an inquiry about closed versus open entry technique. Am J Obstet Gynecol. 2004;190:634–8. doi: 10.1016/j.ajog.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 6.Yuzpe AA. Pneumoperitonium needle and trocar injuries in laparoscopy: a survey on possible contributing factors and prevention. J Reprod Med. 1990;35:485–90. [PubMed] [Google Scholar]
- 7.Nezhat FR, Silfen SL, Evans D, et al. Comparison of direct insertion of disposable and standard reusable laparoscopic trocars and previous pneumoperitonium with Veress needle. Obstet Gynecol. 1991;78:148–50. [PubMed] [Google Scholar]
- 8.Garry R. Towards evidence-based laparoscopic entry techniques: clinical problems and dilemma. Gynaecol Endosc. 1999;8:315–26. [Google Scholar]
- 9.Ahmad G, Duffy JMN, Phillips K, et al. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2008;(2):CD006583. doi: 10.1002/14651858.CD006583.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Vilos GA, Ternamian A, Dempster J, et al. Clinical Practice Gynaecology Committee, The Society of Obstetricians and Gynaecologists of Canada. Laparoscopic entry: a review of techniques, technologies, and complications. SOGC Clinical Practice Guideline No. 193, May 2007. J Obstet Gynaecol Can. 2007;29:433–65. doi: 10.1016/S1701-2163(16)35496-2. [DOI] [PubMed] [Google Scholar]
- 11.Neudecker J, Sauerland S. The European Association for Surgery clinical practice guideline on the pneumoperitonium for laparoscopic surgery. Surg Endosc. 2002;16:1121–43. doi: 10.1007/s00464-001-9166-7. [DOI] [PubMed] [Google Scholar]
- 12.Kroft J, Aneja A, Tyrwhitt J, et al. Laparoscopic peritoneal entry preferences among Canadian gynaecologists. J Obstet Gynaecol Can. 2009;31:641–8. doi: 10.1016/s1701-2163(16)34243-8. [DOI] [PubMed] [Google Scholar]
- 13.Varma R, Gupta JK. Laparoscopic entry techniques: clinical guideline, national survey, and medicolegal ramifications. Surg Endosc. 2008;22:2686–97. doi: 10.1007/s00464-008-9871-6. [DOI] [PubMed] [Google Scholar]
- 14.Wind J, Van Berge Henegouwen JEL, Gouma MI, et al. Medical liability insurance claims in laparoscopy. Surg Endosc. 2007;21:2094–9. doi: 10.1007/s00464-007-9315-8. [DOI] [PubMed] [Google Scholar]
- 15.Catarci M, Carlini M, Santioro E. Major and minor injuries during creation of pneumopertoneum: a multicentre study of 12,919 cases. Surg Endosc. 2001;15:566–9. doi: 10.1007/s004640000381. [DOI] [PubMed] [Google Scholar]
- 16.Munro MG. Laparoscopic access: complications, technologies, and techniques. Curr Opin Obstet Gynecol. 2002;14:365–74. doi: 10.1097/00001703-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Richardson RF, Sutton CJG. Complications of first entry: a prospective laparoscopic audit. Gynaecol Endosc. 1999;8:327–34. [Google Scholar]
- 18.Teoh B, Sen R, Abbott J. An evaluation of four tests used to ascertain Veress needle placement at closed laparoscopy. J Minim Invasive Gynecol. 2005;12:153–8. doi: 10.1016/j.jmig.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 19.Molloy D, Kalloo PD, Cooper M. Laparoscopic entry: a literature review and analysis of techniques and complications of primary port entry. Aust N Z J Obstet Gynaecol. 2002;42:246–54. doi: 10.1111/j.0004-8666.2002.00246.x. [DOI] [PubMed] [Google Scholar]
- 20.Garry R. Complications of laparoscopic entry. Gynaecol Endosc. 1997;6:319–29. [Google Scholar]
- 21.Härkki-Sirén P, Kurki T. A nationwide analysis of laparoscopic complications. Obstet Gynecol. 1997;89:108–12. doi: 10.1016/s0029-7844(96)00390-0. [DOI] [PubMed] [Google Scholar]
- 22.Hasson HM. Open laparoscopy as a method of access in laparoscopic surgery. Gynaecol Endosc. 1999;8:353–62. [Google Scholar]
- 23.Hasson HM. A modified instrument and method for laparoscopy. Am J Obstet Gynecol. 1971;110:886–7. doi: 10.1016/0002-9378(71)90593-x. [DOI] [PubMed] [Google Scholar]
- 24.Long JB, Giles DL, Cornella JL, et al. Open laparoscopic access technique: review of 2010 patients. J Soc Laparoendosc Surg. 2008;12:372–5. [PMC free article] [PubMed] [Google Scholar]
- 25.Hasson HM, Rotman C, Rana N, et al. Open laparoscopy: 29-year experience. Obstet Gynecol. 2000;96:763–6. doi: 10.1016/s0029-7844(00)01026-7. [DOI] [PubMed] [Google Scholar]
- 26.Wherry DC, Marohn MR, Malanoski MP, et al. An external audit of laparoscopic cholecystectomy in the steady state performed in a medical treatment facility of the Department of Defense. Ann Surg. 1996;224:145–54. doi: 10.1097/00000658-199608000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chapron C, Carvello L, Chopin N, et al. Complications during set- up procedures for laparoscopy in gynecology: open laparoscopy does not reduce the risk of major complications. Acta Obstet Gynecol Scand. 2003;82:1125–9. doi: 10.1046/j.1600-0412.2003.00251.x. [DOI] [PubMed] [Google Scholar]
- 28.Pring CM. Aortic injury using the Hasson trocar: a case report and review of the literature. Ann R Coll Surg Engl. 2007;89:W3–5. doi: 10.1308/147870807X160416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Larobina M, Nottle P. Complete evidence regarding major vascular injuries during laparoscopic access. Surg Laparosc Endosc Percutan Tech. 2005;15:119–23. doi: 10.1097/01.sle.0000166967.49274.ca. [DOI] [PubMed] [Google Scholar]
- 30.Bonjer HJ, Hazebroek EJ, Kazemier G, et al. Open versus closed establishment of pneumoperitoneum in laparoscopic surgery. Br J Surg. 1997;84:599–602. [PubMed] [Google Scholar]
- 31.Agarwala N, Lu CY. Safe entry technique during laparoscopy: left upper quadrant entry using the ninth intercostal space: a review of 918 procedures. J Minim Invasive Gynecol. 2005;12:55–61. doi: 10.1016/j.jmig.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 32.Vilos AG, Volis GA, Abu-Rafea B, et al. Effect of body habitus and parity on the initial Veres intraperitoneal CO2 insufflation pressure during laparoscopic access in women. J Minim Invasive Gynecol. 2006;13:108–13. doi: 10.1016/j.jmig.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 33.Champault G, Cazacu F, Taffinder N. Serious trocars accidents in laparoscopic surgery: a French survey of 103,852 operations. Surg Laparosc Endosc. 1996;6:367–70. [PubMed] [Google Scholar]
- 34.Corson SL, Chandler JG, Way LR. Survey of laparoscopic entry injuries provoking litigations. J Am Coll Surg. 2001;192:478–90. doi: 10.1016/s1072-7515(01)00820-1. [DOI] [PubMed] [Google Scholar]
- 35.String A, Berber E, Foroutani A, et al. Use of the optical access trocar for safe and rapid entry in various laparoscopic procedures. Surg Endosc. 2001;15:570–3. doi: 10.1007/s004640080056. [DOI] [PubMed] [Google Scholar]
- 36.Fuller J, Ashar B, Carey-Corrado J. Trocar-associated injuries and fatalities: an analysis of 1399 reports to the FDA. J Minim Invasive Gynecol. 2005;12:302–7. doi: 10.1016/j.jmig.2005.05.008. [DOI] [PubMed] [Google Scholar]