Dear Editor,
With interest we read the recent observational cohort study by Royakkers et al. [1] that shows that higher levels of cystatin C do not predict the development of acute kidney injury (AKI) nor the need for renal replacement therapy (RRT). Apart from the hypothesis that cystatin C could detect AKI 1 or 2 days earlier than serum creatinine, which was not confirmed in the study by Royakkers, it is also thought that serum cystatin C is less influenced by RRT than creatinine, and thus better reflects residual glomerular filtration rate (GFR). Determining residual GFR is difficult to establish in the critically ill patient with no steady state in renal function and large changes in fluid balance.
As creatinine is a small-sized molecule that is eliminated from the blood during RRT, it is not useful for estimating the residual GFR. Cystatin C is a medium-sized molecule (13.3 kDa). Calculated from measurements in the efferent and afferent line and from the ultrafiltrate line, it has been shown that the removal of cystatin C by continuous venovenous hemofiltration (CVVH) is less than 30% of its generation and is therefore thought not to influence serum cystatin C significantly. Although the reduction ratio of cystatin C is dependent on the type of membrane, dialysis dose, volume, and ultrafiltration rate, it is advocated that cystatin C can be used to estimate the residual GFR in patients on RRT [2]. Importantly, changes in serum cystatin C were not determined in this study.
We determined serum creatinine and cystatin C in 6 patients with septic shock with AKI 48 and 24 h prior and following the initiation of CVVH. CVVH was performed using the Prismaflex (Gambro) system with an AN100 ST filter (polyacrylonitrile), a blood flow of 200 ml/min, and a predilution substitution flow of 2,000 ml/h. CVVH was started according to the criteria for initiation of RRT that were standardized by the Acute Dialysis Quality Initiative (ADQI) consensus [3].
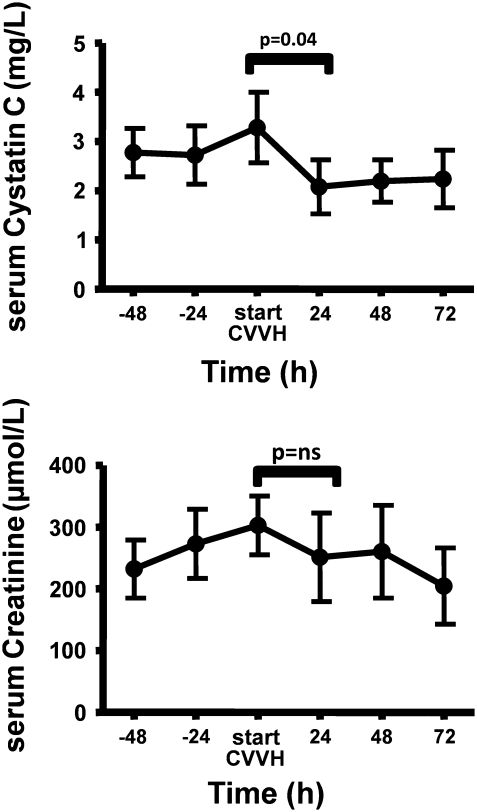
We compared the serum creatinine and cystatin C at initiation and after 24 h of CVVH with a paired Student’s t test. We observed that serum cystatin C decreased significantly following initiation of CVVH (p = 0.04), whereas the decrease of serum creatinine within the first 24 h was not significant (ns, p = 0.66), as shown in Fig. 1.
Fig. 1.
Time course of serum cystatin C and serum creatinine before and after initiation of continuous venovenous hemofiltration in patients with acute kidney injury in severe sepsis or septic shock. Values are means ± SEM
This observation was previously described in patients that received intermittent hemodialysis; a higher dose of dialysis resulted in a decreased level of serum cystatin C, indicating that dialysis removes cystatin C from the patient [4]. In a previous study, 3 h of intermittent hemodialysis using a polymethylmethacrylate filter decreased cystatin C concentrations by 30 ± 7% [5]. This supports the hypothesis that in different types of renal replacement therapy serum cystatin C concentrations are reduced.
In addition to the inability of cystatin C to predict AKI better or earlier than serum creatinine, our finding highlights the limited value of cystatin C in assessing residual GFR in patients with sepsis-induced AKI.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
An author’s reply to this comment is available at: doi:10.1007/s00134-011-2348-4.
References
- 1.Royakkers AA, Korevaar JC, van Suijlen JD, Hofstra LS, Kuiper MA, Spronk PE, Schultz MJ. Serum and urine cystatin C are poor biomarkers for acute kidney injury and renal replacement therapy. Intensive Care Med. 2011;37:493–501. doi: 10.1007/s00134-010-2087-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baas MC, Bouman CS, Hoek FJ, Krediet RT, Schultz MJ. Cystatin C in critically ill patients treated with continuous venovenous hemofiltration. Hemodial Int. 2006;10(Suppl 2):S33–S37. doi: 10.1111/j.1542-4758.2006.00115.x. [DOI] [PubMed] [Google Scholar]
- 3.Bellomo R, Angus D, Star RA. The acute dialysis quality initiative–part II: patient selection for CRRT. Adv Ren Replace Ther. 2002;9:255–259. doi: 10.1053/jarr.2002.35570. [DOI] [PubMed] [Google Scholar]
- 4.Al-Malki N, Heidenheim PA, Filler G, Yasin A, Lidnsay RM. Cystatin C levels in functionally anephric patients undergoing dialysis: the effect of different methods and intensities. Clin J Am Soc Nephrol. 2009;4:1606–1610. doi: 10.2215/CJN.02910509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mayeur N, Rostaing L, Nogier MB, Jaafar A, Cointault O, Kamar N, Conil JM, Fourcade O. Kinetics of plasmatic cytokines and cystatin C during and after hemodialysis in septic shock-related acute renal failure. Crit Care. 2010;14:R115. doi: 10.1186/cc9064. [DOI] [PMC free article] [PubMed] [Google Scholar]