Abstract
The current study assessed efficacy of combined cognitive behavioral therapy (CBT) and venlafaxine XR compared to venlafaxine XR alone in the treatment of generalized anxiety disorder (GAD) within settings where medication is typically offered as the treatment for this disorder. Patients with DSM-IV–diagnosed GAD who were recently enrolled in a long-term venlafaxine XR study were randomly offered (n=77), or not offered (n=40), the option of adding 12 sessions of CBT. Of those offered CBT, 33% (n=26) accepted and attended at least one treatment session. There were no differences between the combined treatment group and the medication only group on primary or secondary efficacy measures in any of the sample comparisons. Many patients who present in medical/psychopharmacology settings seeking treatment for GAD decline the opportunity to receive adjunctive treatment. Of those that receive CBT, there appears to be no additional benefit of combined treatment compared to venlafaxine XR alone.
Keywords: Generalized Anxiety Disorder, Cognitive-Behavioral Therapy, venlafaxine, combined treatment
1. INTRODUCTION
Generalized anxiety disorder (GAD) is a prevalent and chronic disorder with high rates of recurrence. The most recent data on the occurrence of DSM-IV GAD is from the National Comorbidity Survey Replication study (Kessler et al., 2005), which reported lifetime prevalence for DSM-IV GAD of 5.7% and 12-month prevalence of 3.1%. Projected lifetime prevalence revealed that 8.3% of the United States population can be expected to experience GAD at some time if they live to age 75 (Kessler et al., 2005). A large-scale naturalistic study of the course of anxiety disorders found that the probability of recovery from DSM-III-R GAD over a 12 year period was 58%, and the probability of subsequent recurrence among those who did recover was 45% (Yonkers et al., 1996; Yonkers et al., 2000).
Beyond the characteristic chronicity and high rates of recurrence, patients with GAD often experience significant impairments in psychosocial functioning, like poor emotional health (Robins & Regier, 1991), low occupational level (Massion et al., 1993), and increased risk of suicide (Boden et al., 2007). Role impairment in those with pure GAD (without co-morbidity) is comparable to pure major depressive disorder (MDD) as well as other mood disorders (Kessler et al., 1999; Wittchen et al., 2000; Grant et al., 2005). Moreover, significant disability similar to what would be expected from chronic medical illnesses can result from cases in which anxiety is not successfully treated (Fifer et al., 1994; Kessler et al., 2001).
Both medications and cognitive-behavioral psychotherapy (CBT) have been widely investigated as treatments for GAD. A standard package of CBT for GAD usually includes both cognitive restructuring and applied relaxation, along with education about the nature of anxiety, training in the recognition and monitoring of situational, physiological, cognitive, and behavioral cues associated with anxious responding, training in arousal reduction techniques such as progressive muscle relaxation, pleasant imagery and diaphragmatic breathing, and imaginal exposure to anxiety cues coupled with coping skill rehearsal (Newman & Borkovec, 2002; Roemer & Orsillo, 2002). A meta-analysis reviewed results of 19 studies investigating efficacy of CBT for GAD and found that CBT treatments were superior to wait-list controls, psychological placebos, and pill placebos (Mitte, 2005). CBT currently stands as the only psychotherapy method for GAD that has empirical support (Chambless et al., 1996). However, despite empirical support for CBT in treatment of GAD, amount of clinically significant change has only been moderate, with approximately half of patients displaying some ongoing clinical symptoms after treatment (Chambless & Gillis, 1993).
Psychopharmacological treatments have also been found to be effective in the treatment of GAD. The most investigated medications for GAD are benzodiazepines (Rickels & Rynn, 2002), but selective serotonin reuptake inhibitor (SSRI) and serotonin norepineprhine reuptake inhibitor (SNRI) antidepressants have been found to be efficacious (Mitte et al., 2005), and are now considered first-line pharmacotherapies for GAD. Similar to CBT, a satisfactory response to short-term SSRI/SNRI treatment occurs for only about 60% of patients and full remission in only about 37% of patients (Gelenberg et al., 2000; Pollack et al. 2001).
Given that both CBT and psychopharmacological treatments are commonly used in the treatment of GAD, yet neither alone results in a high rate of clinical response to treatment, it is remarkable that little research attention has been devoted to the efficacy of the combination of medication and psychotherapy. Only two studies have examined combinations of psychosocial and medication treatments for GAD; neither of these used SSRI or SNRI medications now accepted as front-line pharmacological treatments for GAD. In a study by Power and his colleagues (1990), five treatments were compared: CBT, diazepam, pill placebo, diazepam plus CBT, and pill placebo plus CBT. Patients (about 20 per condition) met DSM-III GAD criteria, although no structured interview was employed. Results indicated that the combined treatment fared the best, with 90.5% of patients in combined treatment showing clinically-significant change. However, this study is difficult to interpret because sample sizes were small, diagnosis was not established by structured interview, DSM-III diagnoses were used, and no assessment of adequacy of implementation of CBT was performed. In another study, 60 patients with GAD were randomized to receive buspirone plus anxiety management training; buspirone and non-directive therapy; placebo and anxiety management training; and placebo and non-directive therapy (Lader & Bond, 1998). There were no differences among the four groups, all of whom showed improvement. In summary, no studies have examined the efficacy of SSRI/SNRI medications and psychotherapy for GAD.
In designing a study of combined medication and psychotherapy for a psychiatric disorder, an important consideration is the context in which patients are seeking treatment. Some patients pursue treatment for symptoms from a primary care physician, or psychiatrist, and have a preference for receiving medication. Depending on patient preferences, the treating physician may then refer the patient for psychotherapy rather than prescribing medication, or perhaps more commonly as an adjunct to medication. Other patients may seek help for anxiety symptoms directly from a psychotherapist, who may or may not refer the patient for adjunctive medication treatment depending on patient preference, severity of illness, and other clinical considerations. Patients seeking treatment by a non-psychotherapist physician compared to a psychotherapist may differ in important characteristics, such as severity of symptoms, degree of psychic vs. somatic symptoms, and/or treatment preference, and these characteristics may be associated with differential responsiveness to medication compared to psychotherapy.
The issue of treatment context is particularly salient for the treatment of GAD because patients with GAD commonly show up in primary care medical practices and often are specifically seeking medication for their symptoms. The 12-month prevalence rate for GAD in primary care is approximately 4%, and much higher prevalence rates are apparent when DSM-IV symptom criteria are used without a duration criterion (Wittchen et al., 2002). When individuals with GAD present to a primary care physician, only 13% of them report a chief complaint of anxiety (Wittchen et al., 2002). More common complaints of GAD patients in primary care include somatic symptoms (48%), pain (35%), sleep disturbance (33%), and depression (16%) (Wittchen et al., 2002). Overall, use of medications for anxiety disorders has been increasing in both primary care and psychiatric settings (Harman et al., 2002). Thus, in clinical practice, psychotherapy, if it is offered at all, will therefore frequently be offered in the context of medication treatment for GAD and its occurrence is based on the presumption that the combination is likely more efficacious than either CBT or medication alone.
The current preliminary study was designed with these issues in mind. The availability of an ongoing study (Rickels et al., 2010) of long-term venlafaxine XR treatment of GAD being conducted at primary care site and a psychopharmacology clinic allowed us to ask the following questions: (1) what percent of patients who have initially sought medication for their GAD symptoms would be interested in combining medication with CBT, and (2) for patients who receive at least one session of CBT, does the combination of medication plus 12 weeks of CBT result in greater improvements in GAD symptoms, depression, and functioning compared to medication alone among patients who initially sought medication treatment (and received at least one dose of medication)?
2. METHOD
2.1 Study Design
The medication study was an 18-month, relapse prevention one consisting of three treatment phases (Rickels et al., 2010). The first phase was a 6-month open-label venlafaxine flexible-dose treatment phase (75mg–225mg/day). The second and third phases were each 6-month randomized, double-blind, placebo-controlled relapse phases. Only data from the first phase are included in the current report. Most patients (n=239) enrolled in the medication trial were recruited and seen in one of four primary care practices by research psychiatrists who were placed into the primary care sites. An additional group (n=95) of patients was enrolled in a psychopharmacology clinic in a university setting. Further details of the parent trial are available elsewhere (Rickels et al., 2010).
After the parent medication study was ongoing, the current combined treatment study was initiated. Patients who were enrolled in the medication study were randomly selected to be offered the option of adding 12 weeks of CBT in addition to venlafaxine XR. Patients were generally approached to consider the addition of CBT at the first study visit (week 2) after beginning medication. A 2:1 (CBT:medication) randomization scheme was used because of the existence of the large comparison group of patients on venlafaxine XR alone (n=159) that was already available from the parent study. Study visits occurred at baseline, biweekly for 8 weeks and monthly thereafter. This medication trial was conducted from 2005 to 2009 with approval and oversight by the local Institutional Review Board (IRB). The CBT addition was also approved by the IRB and was conducted from October, 2006 to March, 2008. Patients provided written informed consent for participation in the medication trial, and separately for the CBT addition study.
2.2 Participants
Patients were recruited through community outreach presentations, mailings, media advertising, and referrals from health care professionals including the primary care physicians at the primary care sites. To be eligible, patients needed to be over the age of 18, meet DSM-IV criteria for GAD (based on a diagnostic interview at baseline) and obtain scores ≥ 4 on the Clinical Global severity scale (CGI; Guy, 1976) and ≥ 20 on the Hamilton Anxiety Rating Scale (HAM-A; Hamilton, 1959). To eliminate patients with co-morbid disorders, patients were excluded if they had a score > 18 on the Hamilton Depression Scale (HAM-D; Hamilton, 1960), an episode of major depressive disorder in the previous six months, or any other current DSM-IV anxiety diagnoses. Patients also could not have any regular use of buspirone, anticonvulsants, neuroleptics, or antidepressants within 14 days of the commencement of the study.
All psychotherapists (2 women; 3 men) were doctoral-level licensed psychologists with experience in applying CBT for anxiety disorders and working as research protocol therapists. On average, the therapists were 10 years post-doctoral. The therapists were trained in a CBT for GAD treatment manual by an experienced CBT trainer/supervisor. The training procedures consisted of a workshop and didactic instruction, followed by supervision on at least one training case. The therapists attended weekly individual supervision sessions, and training case tapes were rated by the supervisor using rating scales developed for evaluating the integrity of CBT (Borkovec et al., 2002). The supervisor’s ratings indicated that none of the CBT sessions included interpretive reflections or any other intervention method clearly from psychodynamic, interpersonal, or experiential therapies.
2.3 Procedures
Interested patients received a telephone screen, which included the Anxiety Screening Questionnaire (ASQ-15) (Wittchen & Boyer, 1998). If the patient met the initial inclusion criteria, he or she was scheduled for an interview with a psychiatrist. The psychiatrist conducted a full psychiatric and medical evaluation, ensuring that all study criteria were fulfilled. Baseline assessments included the Structured Clinical Interview for DSM-IV (SCID; First et al., 1996), a physical examination, and assessment of demographic and illness variables.
All post-baseline assessments were performed by a psychiatrist, who also administered the venlafaxine XR in a flexible dose of 75 – 225 mg/d.
Participants who were offered to add CBT and elected to receive CBT received treatment sessions weekly for 12 weeks. No fees were charged for the CBT sessions. The CBT for GAD treatment manual that was implemented in the Borkovec and Costello (1993) and Borkovec et al. (2002) studies was used to guide treatment. This package includes the following techniques: applied relaxation/self-control desensitization (SCD) involving presentation of the multiple coping response CBT model and rationale; training in self-monitoring of environmental, somatic, affective, imaginal, and thought (especially worry) cues that trigger anxiety spirals with special emphasis on increasingly early cue detection; external and especially internal cue hierarchy development; formal slowed diaphragmatic breathing and progressive relaxation; training in cue-controlled and differential relaxation; applied relaxation training; development of coping self-statements to use in response to cues; and employment of self-statements and applied relaxation during formal SCD imagery for rehearsal of coping responses. Hierarchies for SCD are constructed from daily self-monitoring and in-session discussion with the patient. The CBT package also included the following cognitive therapy (Beck & Emery, 1985) techniques: presentation of the role of cognition in anxiety; training in self-monitoring of early worry and automatic thought occurrence; identification of cognitive predictions, interpretations, beliefs, assumptions, and core beliefs underlying the threatening nature of events or cues; logical analysis; examination of evidence; labeling of logical errors; decatastrophization; generation of alternative thoughts and beliefs; early application of these alternatives to daily living; the creation of behavioral experiments to obtain evidence for new beliefs; and use of cognitive perspective shifts learned in cognitive therapy during SCD rehearsals.
Adherence to the CBT treatment model was evaluated using the CBT for GAD adherence checklist previously used in CBT for GAD trials by Borkovec and Costello (1993) and Borkovec et al.(2002) The checklist was completed by the CBT supervisor after listening to audiotapes of treatment sessions. A total of 127 sessions was rated (an average of 4.9 sessions for each of the 26 patients that had at least one CBT session). On average, 70% of the sessions from each case were selected. Of all sessions checked for protocol adherence, 62 (48.8%) were from sessions 1–4, 36 (28.4%) from sessions 5–8, and 29 (22.8%) from sessions 9–12. Overall, no sessions contained any interventions that were not allowed as part of the CBT model. Of the list of 15 CBT techniques on the adherence checklist, the average session contained 7.7 (SD = 2.6) of these techniques.
2.4 Assessments
The HAM-A was used to measure anxiety symptoms and was the primary efficacy measure. The 17-item version of the HAM-D was used to assess severity of depressive symptoms. Clinical Global Impressions Severity and Improvement scale (CGI-S, CGI-I; Guy, 1976) were used to assess severity of illness and global improvement, respectively. The SCID, HAM-A, HAM-D, CGI-S, and CGI-I ratings were conducted by research psychiatrists trained and highly experienced in the use of these scales. The evaluators were not informed about which patients received CBT and were instructed to not ask about it.
Patient-report measures included the quality of life subscale of the General Health Questionnaire (GHQ/12-QL; Bech, 1993), the Penn State Worry Questionaire (Meyer et al., 1990), and the Hospital Anxiety and Depression (HAD) scale (Zigmond & Snaith, 1983). The GHQ/12-QL scale consists of 11 disability and quality of life items selected from the GHQ and summed for a total score. The HAD was used to assess patients’ report of anxiety and depressive symptoms.
The HAM-A, CGI-S, CGI-I, and HAD were assessed at each medication study visit and the HAM-D and GHQ/12-QL at intake and 24 weeks. Clinical response on the HAM-A was defined as a 50% or greater reduction from baseline to last value with the 24-week open label medication phase (Ballenger, 1999). Clinically significant change (Jacobson, Follette, & Revenstorf, 1984) was defined on the PSWQ as an estimated (based on linear mixed effects model) endpoint score of less than 50.9. This score was calculated using the PSWQ normative data provided by Gillis, Haaga, and Ford (1995) and the baseline PSWQ mean and SD from the current sample. The PSWQ mean and SD from the normative and current GAD samples were entered into the Jacobson et al. (1984) formula “c” for clinically significant change. This method provides a cutoff indicating whether or not the level of functioning by a patient is statistically more likely to be in the functional rather than the dysfunctional population.
2.5 Statistical Analysis
Baseline differences between treatment groups were examined using chi-square for categorical variables and t-tests for continuous variables. The primary analysis compared those patients randomized to CBT who attended at least one treatment session to those patients randomized to venlafaxine XR who received at least one medication dose. An additional set of analyses compared those patients randomized to CBT who attended at least one treatment session to the group of patients who received venlafaxine XR prior to the start of the current combined treatment study.
Analyses of efficacy variables that were measured repeatedly over time were conducted using mixed effects models that tested for differential slopes over time between the CBT plus venlafaxine XR and venlafaxine XR alone groups using only available scores (no imputation for missing data). These models were implemented using SAS Procedure Proc Mixed (Littell et al., 1996). Because the HAM-A demonstrated a relatively rapid improvement early in treatment and then a leveling off, a shifted log-transformation of time of assessment was implemented. Measures assessed at baseline and week 24 only were analyzed using analyses of covariance with the baseline score as the covariate. Response rates were compared across treatment groups using chi-square.
Because only a subset of patients who was randomly offered CBT elected to receive it, the possibility that patients who actually received CBT were different from those who received venlafaxine XR only was a concern. To address this, secondary analyses using propensity scores as covariates were created. Propensity scores were created by predicting treatment group from the following baseline characteristics of patients: age, gender, ethnicity (white/non-white), marital status (currently married vs. not), employment status (currently employed full time vs. not), and baseline scores on the subscale of the HAD, general health questionnaire total score, SCL-40 total score, HAM-A total score, and SF12 Physical component. Other secondary measures such as the HAM-D and CGI were considered but excluded from the propensity score due to high collinearity with the specified secondary measures or incompleteness of baseline data. Propensity scores were then used as a covariate in mixed effects models described above in secondary analyses.
3. RESULTS
3.1 Patient Disposition and Baseline Characteristics
Of 334 patients who were screened and accepted into the medication study (signed consent), 66 did not receive study drug (64 withdrew consent and 2 were protocol violators), leaving 268 patients who received at least one dose of open label venlafaxine XR treatment. Of the 268 who received venlafaxine XR, 159 (59.3%) patients completed the 6-month open-label phase. Reasons for attrition included withdrew consent (31), protocol deviation (11), lost to follow-up (16), adverse events (31), and other (20).
During the time period in which recruitment for the CBT study was ongoing, 77 patients (of the 334 enrolled in the medication trial) were randomly assigned to be offered CBT (i.e., to have the choice or receiving or not receiving CBT) and 40 patients to not be offered CBT. Of the 77 offered CBT, 45 expressed initial interest and asked to hear more information about the study, and 29 (37% of those offered) agreed to participate and signed a consent form. Of the 29 who agreed to participate, 26 attended at least one CBT session (33% of those offered CBT treatment). There were 12 (46%) patients (of the 26) who completed at least 10 CBT sessions. The average (SD) number of CBT treatment sessions obtained was 7.0 (4.4). Of the 40 not offered CBT, 5 did not receive a dose of venlafaxine XR. Both the combined treatment group and the venlafaxine XR only group continued in the study to week 24 at similar rates (65% of the 26 patients who began treatment in the combined group attended the week 24 assessment; 69% of the 35 patients who began venlafaxine XR only treatment attended the week 24 assessment).
There were no significant differences between those randomized to CBT (n=77) and those assigned to medication only (n=40) in terms of gender, ethnicity, race, marital status, employment status, or age (Table 1). There were also no significant demographic differences between those who received at least one sessions of CBT (n=26) and those that were assigned to medication and received at least one dose (n=35) or between those who received at least one session of CBT (n=26) and the non-randomized group of patients who received venlafaxine XR only prior to the initiation of the current trial (n=159).
Table 1.
Demographic Characteristics for Patients in CBT + Venlafaxine XR Versus Venlafaxine XR Alone
| Demographic Characteristic |
Randomized to CBT+VEN (n=77) |
Randomized to VEN Alone (n=40) |
Received 1 or More CBT Sessions (n=26) |
Non-randomized VEN Alone (n=159) |
|---|---|---|---|---|
| Gender, Women (%) | 68.8% | 52.5% | 65.4% | 62.8% |
| Ethnicity, Hispanic (%) | 3.9% | 2.5% | 7.7% | 5.54% |
| Race (%) | ||||
| White | 67.5% | 70.0% | 65.4% | 81.1% |
| Black | 31.2% | 27.5% | 30.8% | 16.5% |
| Asian | 1.3% | 0% | 3.8% | 1.8% |
| Other | 0% | 2.5% | 0% | 0.6% |
| Marital Status | ||||
| Single | 38.9% | 47.5% | 57.7% | 31.3% |
| Married | 46.8% | 37.5% | 26.9% | 48.5% |
| Divorced | 5.2% | 2.5% | 3.8% | 12.9% |
| Widowed | 5.2% | 10.0% | 7.7% | 7.4% |
| Other | 3.9% | 2.5% | 3.8% | 0% |
| Employment Status | ||||
| Full-time | 63.6% | 55.0% | 50.0% | 47.9% |
| Part-time | 6.5% | 2.5% | 7.7% | 9.8% |
| Homemaker | 1.3% | 5.0% | 0% | 9.2% |
| Unemployed | 9.1% | 7.5% | 19.2% | 12.9% |
| Student | 2.6% | 7.5% | 3.8% | 3.1% |
| Retired | 16.9% | 22.5% | 19.2% | 17.2% |
| Age, Mean (SD) | 46.3 (15.0) | 46.4 (19.3) | 47.5 (16.0) | 47.7 (15.8) |
VEN = venlafaxine XR.
At baseline, the mean HAM-A total score was higher for the combined treatment group (n=26) compared to the randomized venlafaxine XR group (n=35) (2.1 points higher; p < .05), and compared to the non-randomized group of patients (n=1598) that received venlfaxine XR (1.3 points higher; p < .05) (Table 2). This difference was also apparent in the randomized samples (n=40 for combined; n=77 for venlafaxine XR alone) (1.7 point difference, p < .05). A similar difference at baseline was apparent for the SF-12 Physical scale (p < .05; Table 2), but there were no other significant baseline differences on outcome measures between the treatment groups for the sample who received at least one sessions of CBT (n=26) and those that were assigned to medication and received at least one dose (n=35).
Table 2.
Means (SD, N) for Primary and Secondary Efficacy Measures
| Assessment Visit | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Measure | Baseline | Week 2 | Week 4 | Week 6 | Week 8 | Week 12 | Week 16 | Week 20 | Week 24 |
| HAM-A Total | |||||||||
| CBT+VEN | 25.9 (2.6, 26) | 20.9 (5.0, 26) | 17.3 (5.6, 26) | 13.5 (6.5, 26) | 12.7 (7.5, 26) | 10.8 (7.2, 25) | 8.1 (6.9, 20) | 6.2 (5.5, 18) | 6.5 (5.4, 17) |
| Ven (randomized) | 23.8 (2.7, 35) | 19.4 (5.1, 35) | 14.7 (5.6, 31) | 10.9 (5.5,28) | 7.8 (6.0, 27) | 5.9 (4.3, 26) | 4.3 (3.1, 27) | 4.3 (3.2, 25) | 3.4 (1.9, 24) |
| Ven (not randomized) | 24.6 (3.9, 159) | 19.3 (5.5, 158) | 15.0 (6.7, 142) | 11.5 (6.7, 132) | 9.9(6.6, 124) | 7.8 (6.3, 118) | 6.6 (5.5, 102) | 5.7 (5.5, 95) | 5.3 (5.0, 89) |
| HAD Anxiety | |||||||||
| CBT+VEN | 13.6(3.4,26) | 11.7 (4.8, 26) | 10.9 (4.5, 26) | 9.2 (4.7, 26) | 9.0 (4.7, 25) | 6.9 (4.3, 25) | 6.9 (5.2, 20) | 6.2 (4.6, 18) | 6.2 (3.3, 15) |
| VEN (randomized) | 13.0 (4.2, 38) | 10.9 (5.1, 35) | 8.3 (5.0, 31) | 7.1 (4.6, 28) | 5.7 (4.1, 27) | 4.1 (3.4, 26) | 4.6 (3.4, 27) | 4.9 (3.6, 24) | 4.7 (4.5, 24) |
| VEN (not randomized) | 13.3 (3.4, 159) | 10.6 (4.5, 158) | 9.6 (4.3, 140) | 8.5 (4.4, 131) | 7.5 (4.5, 124) | 5.9 (4.7, 116) | 6.0 (4.1, 103) | 6.0 (4.4, 96) | 5.3(4.3, 87) |
| HAD Depression | |||||||||
| CBT+VEN | 9.8 (5.7, 26) | 8.5(5.1, 26) | 7.9 (5.1, 26) | 6.3(5.0, 26) | 7.0(5.3, 25) | 5.5 (4.6, 25) | 5.6 (4.9, 20) | 4.3 (4.3, 18) | 4.7 (3.9,15) |
| Ven (randomized) | 7.3 (3.4, 35) | 6.8 (3.9, 35) | 5.3 (3.8, 31) | 4.5 (3.3, 28) | 3.4 (3.3, 27) | 2.9 (2.7, 26) | 2.0 (2.3, 27) | 2.1 (2.3, 24) | 2.9 (3.1, 24) |
| Ven (not randomized) | 9.1 (4.1, 159) | 7.9 (4.3, 158) | 6.7 (3.8, 140) | 6.1 (4.1, 131) | 5.7 (4.4, 124) | 4.7 (4.1, 116) | 4.5 (4.1, 103) | 4.1 (3.9, 96) | 3.8 (3.7, 87) |
| HAM-D-17 | |||||||||
| CBT+VEN | 13.1 (2.2, 26) | 7.0 (3.4, 23) | 5.1 (4.0, 17) | ||||||
| VEN (randomized) | 12.3 (2.8, 35) | 3.9 (2.6, 26) | 3.0 (1.7, 24) | ||||||
| VEN (not randomized) | 13.5 (3.0, 156) | 5.9 (4.6, 110) | 4.7 (4.5, 90) | ||||||
| CGI-Severity | |||||||||
| CBT+VEN | 4.7(0.6, 26) | 4.1 (0.6, 26) | 3.6 (0.8, 25) | 3.0(1.0, 26) | 2.9 (1.3,26) | 2.4 (1.1, 25) | 2.1 (1.1, 19) | 1.7 (0.9, 17) | 1.8 (1.1, 17) |
| VEN (randomized) | 4.7 (0.5, 34) | 3.9 (0.7, 35) | 3.2 (1.0, 31) | 2.6 (1.0, 28) | 1.9 (1.0, 25) | 1.6 (0.7, 26) | 1.4 (0.6, 27) | 1.4 (0.6, 25) | 1.2 (0.4, 24) |
| VEN (not randomized) | 4.5 (0.6, 158) | 4.0 (0.8, 158) | 3.4 (1.0, 142) | 2.8 (1.1, 133) | 2.5 (1.2, 124) | 2.0 (1.1, 118) | 1.9 (1.1, 102) | 1.7 (1.0, 97) | 1.6 (0.9,89) |
| CGI-Improvement (item 2) | |||||||||
| CBT+VEN | 2.6 (1.9, 26) | 3.3 (0.7, 26) | 2.7 (0.9, 25) | 2.4 (0.9, 26) | 2.3 (1.2, 26) | 1.9 (1.0, 25) | 1.6 (0.8, 19) | 1.4 (0.7, 17) | 1.4 (0.6, 17) |
| VEN (randomized) | 3.1 (1.7, 34) | 3.2 (1.0, 35) | 2.4 (0.8, 31) | 2.0 (0.8, 28) | 1.5 (0.8, 25) | 1.4 (0.6, 26) | 1.2 (0.4, 27) | 1.2 (0.4, 25) | 1.1(0.3, 24) |
| VEN (not randomized) | 1.8 (2.0, 158) | 3.2 (0.8, 158) | 2.7 (0.9, 142) | 2.2 (0.9, 133) | 1.9 (0.9, 124) | 1.7 (1.1, 18) | 1.5 (0.8, 102) | 1.4 (0.8, 97) | 1.3 (0.7, 89) |
| GHQ/12Q | |||||||||
| CBT+VEN | 34.5 (7.0, 26) | 24.8 (7.3, 25) | 23.8 (6.6, 16) | ||||||
| VEN (randomized) | 32.2 (6.4, 33) | 20.4 (5.2, 26) | 22.9 (5.6, 23) | ||||||
| VEN (not randomized) | 32.7 (6.5, 153) | 23.2 (7.0, 116) | 23.5 (5.5, 86) | ||||||
| PSWQ | |||||||||
| CBT+VEN | 61.8 (9.5, 26) | 48.6 (11.8, 25) | 46.4 (11.1, 17) | ||||||
| VEN (randomized) | 57.9 (12.7, 33) | 42.3 (13.0, 26) | 45.1 (14.0, 24) | ||||||
| VEN (not randomized) | 60.4 (12.0, 155) | 48.5 (12.8, 114) | 46.0 (13.8, 85) | ||||||
| SF-12 – Physical Component | |||||||||
| CBT+VEN | 46.1 (13.6, 25) | 46.2 (12.5, 24) | 45.5 (12.7, 17) | ||||||
| VEN (randomized) | 52.7 (10.7, 32) | 51.9 (6.9, 26) | 49.7 (7.0, 25) | ||||||
| VEN (not randomized) | 50.0(10.0,149) | 49.3 (9.1, 112) | 49.9 (8.8, 80) | ||||||
| SF-12 – Mental Component | |||||||||
| CBT+VEN | 28.5 (9.8, 25) | 46.2 (12.6, 24) | 45.5 (12.7, 17) | ||||||
| VEN (randomized) | 31.4 (10.9, 32) | 48.3 (9.5, 26) | 49.8 (10.4, 25) | ||||||
| VEN (not randomized) | 31.7 (9.5, 149) | 47.0(10.9,112) | 48.2(9.8, 80) | ||||||
VEN = venlafaxine XR. The VEN “randomized” sample are those patients who were randomized and received at least one dose of study medication. The VEN “all” includes all patients from the VEN “randomized” sample plus additional patients who received at least one dose of study medication in the parent medication trial (i.e., participated in the parent trial before the current combined treatment study was initiated). HAM-A = Hamilton Anxiety Rating Scale. HAD = Hospital Anxiety Depression Scale. HAM-D-17 = Hamilton Rating Scale for Depression. CGI = Clinical Global Impression. GHQ = General Health Questionnaire. PSWQ = Penn State Worry Questionnaire.
3.2 Efficacy
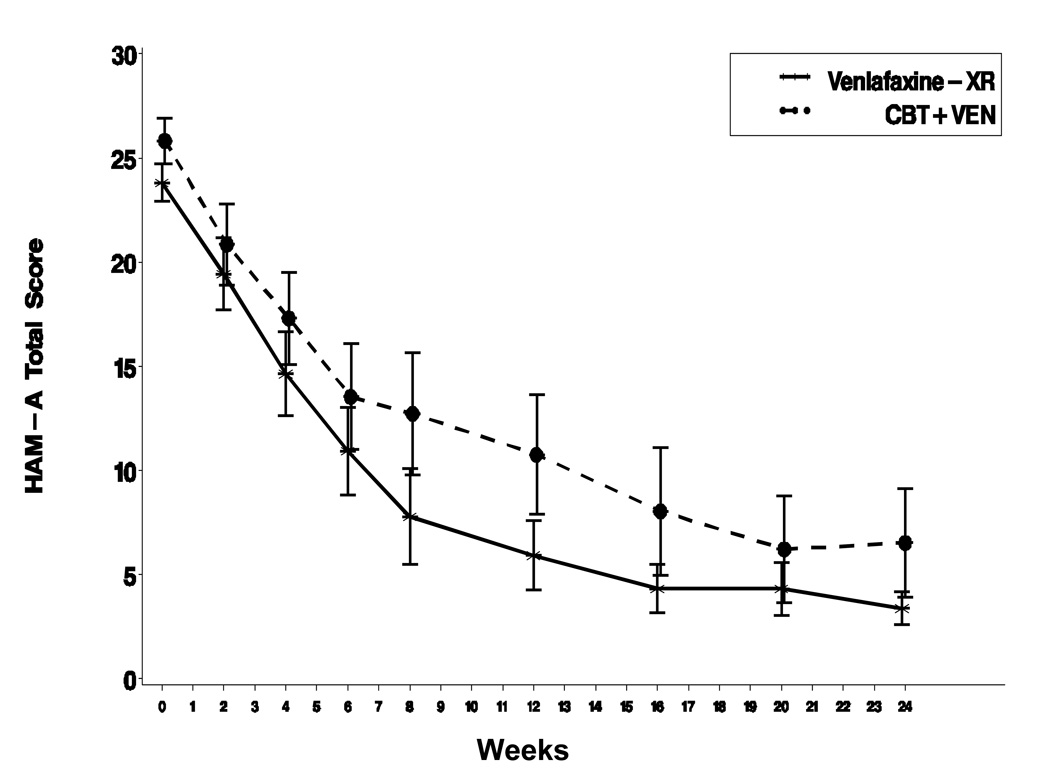
Mixed model analyses comparing the 26 patients who received combined treatment with at least one CBT session to the 35 patients randomized to venlafaxine XR only (and received one dose) on HAM-A total scores revealed no significant difference between the treatment groups (p=.17) (Figure 1). Similarly, there was not a significant difference on the HAM-A total score between combined CBT plus venlafaxine XR and venlafaxine XR alone when the combined (n=26) group was compared to the non-randomized patients (n=159) who received venlafaxine XR alone (and received one dose) from the parent study (p=.96). Additional analyses using the propensity score (derived from predicting the group (n=26) that received combined treatment vs. the non-randomized group (n=159) that received venlafaxine XR (and received one dose) as a covariate also revealed no significant differences between the treatment groups on HAM-A total score slopes (p=.33).
Figure 1.
Mean HAM-A total scores for patients who received at least one session of combined treatment (n=26) versus those randomized to receive only medication and received at least one dose (n=35).
There were also no significant differences between the combined treatment group and the venlafaxine XR only group on any of the secondary efficacy measures (Table 2). The use of a propensity score covariate in the comparison of the combined group (n=26) vs. non-randomized patients (n=159) who received venlafaxine XR alone also failed to result in any significant differences between the treatment groups (p=.98).
Patients in both treatment groups improved considerably, with 65% of patients in the combined treatment group (n=26) meeting criteria for HAM-A clinical response by week 24 (or endpoint) compared to 71% in the venlafaxine XR only (n=35) group (p=.63). Among the non-randomized (n=159) patients who received only venlafaxine XR in the parent study, the HAM-A response rate was 67%. On the PSWQ, 73% (19/26) of those in combined treatment, and 80% (28/35) of those who were randomized to receive venlafaxine XR alone achieved clinically significant change by endpoint, Between-group effect sizes (Cohen’s d), calculated on endpoint scores after propensity score adjustment were: HAM-A total score = −.21; HAD Anxiety = −.36; HAD Depression = .01; HAM-D total score = −.61; CGI Severity = −.61; CGI-Improvement = −.44; PSWQ = .16; GHQ/12Q = −.12; SF-12 Physical = −.29; SF-12 Mental = −.28 (negative effect sizes indicate combined treatment had less improvement compared to medication alone).
Mixed model analyses including only patients that completed at least 7 CBT sessions compared to those who received at least 7 weeks of medication alone also revealed no significant differences between the groups on rates of change on HAM-A total scores, either in analyses that compared those who received combined treatment (n=14) to those randomized to medication alone (n=27) (p=.10) or analyses that compared combined treatment (n=14) to the non-randomized group that received medication alone (n=126) (p=.90). In both cases, rates of change were slightly faster within the medication alone group compared to the combined treatment group.
4. DISCUSSION
The current study found no evidence of additional benefit for combined CBT and venlafaxine XR compared to venlafaxine XR alone in the treatment of GAD. Moreover, within the context of primary care and specialty psychopharmacology treatment settings, only one–third of patients who were offered the opportunity to add CBT to their recently initiated medication treatment elected to do so.
Lack of increased efficacy for combined treatment found here is discrepant from the results of Power and colleagues (1990), who found that combined CBT and medication treatment was more efficacious than CBT, medication, a pill placebo, or a pill placebo plus CBT. However, the Power study (1990) used a small sample (20 participants per condition), employed DSM-III diagnostic criteria, and did not use a structured interview to ascertain diagnosis. Additionally, the current study used the SNRI venlafaxine XR whereas Power and colleagues investigated a benzodiazepine.
Another factor that could have contributed to the lack of a combined treatment effect was the relative high response rate for the venlafaxine XR only group, leaving little room for additional improvement. Even if there had been no “floor” effect, it is possible that there was a bias on the part of patients in the combined treatment condition to attribute any gains they achieved to medications. During audiotapes of CBT sessions, the CBT supervisor noted that participants frequently commented on the positive impact of their medications, and this seemed to make it more difficult for the therapist to engage them fully in homework practice of CBT techniques. This is consistent with a recent study of largely unmedicated patients receiving CBT for GAD showing that to the degree that therapists were able to change expectation for treatment success, such change partially mediated outcome and this effect was unrelated to preceding or concurrent changes in symptoms (Newman & Fisher, in press).
Lack of an effect for combined treatment relative to venlafaxine XR alone may also have been influenced by the setting for the study. The patients were recruited at primary care clinics and a psychopharmacology clinic and only after agreeing to participate in a medication trial. Nevertheless, two-thirds of the patients offered CBT in this study turned it down, suggesting a lack of interest in psychotherapy among many patients who seek medication treatment in these settings. In the treatment of major depressive disorder, several studies have suggested that preference for medication vs. psychotherapy can impact treatment outcome (Chilvers et al., 2001; Lin et al., 2005). Thus, in the current study, resistance to or lack of interest in psychotherapy treatment could have limited any benefit from the addition of CBT. Furthermore, those patients who agreed to receive CBT may have been more treatment resistant compared to those who did not elect to receive CBT, thereby leading to more treatment resistant patient in the combined treatment group compared to those who received medication alone.
Although the setting for the study may have limited the outcomes for combined treatment, performing this study at primary care clinics and a psychopharmacology clinic was of interest because many GAD patients present for the first time in these settings. In addition, such patients are highly likely to be prescribed anxiolytic medication, whether or not they are referred for psychotherapy. Thus, the results generalize to one important segment of the service delivery system, although generalizability of the findings to other settings where psychotherapy is typically delivery is an open question that needs to be examined in further studies.
The design of the study is also important for understanding the lack of any incremental benefit for combined treatment, It is unknown whether CBT alone would have achieved as high a response rate as venlafaxine XR alone in the context of the study’s setting and patient population. Thus, it is possible that combined treatment is superior to CBT alone for patients seeking a psychopharmacological intervention. Future research can address this possibility.
Comparing the results found here to previous studies of combined therapy versus monotherapy, the current findings suggest that, in regard to response to combined treatment, GAD is more similar to other anxiety disorders than major depressive disorder. Studies of panic disorder (Barlow et al., 2000), social phobia (Blomhoff et al., 2001), and obsessive-compulsive disorder (Kozak et al., 2000) have not shown any benefit for combined CBT and medication compared to monotherapy. Studies of chronic depression, however, have found that combined treatment is significantly more beneficial than psychotherapy or medication alone (Thase et al., 1997; Keller et al., 2000). While some researchers propose that GAD is most closely related to major depression (Brown et al., 1998; Barlow, 2002), these results suggest that GAD is more similar to anxiety disorders, at least in terms of response to combined treatment.
This preliminary study of combined treatment has limitations, including the aforementioned method of recruiting patients. Additionally, there were strict exclusion criteria, namely having a co-morbid psychiatric diagnosis. In particular, exclusion of major depressive disorder, a disorder that is often co-morbid with GAD, is an important limitation of this study because this exclusion reduces the generalizability of the results to the broad population of GAD patients seen in clinical practice. Another limitation is that conclusions from this study should be restricted to the specific form of CBT treatment that was implemented. It is possible that CBT packages that include other techniques (e.g., worry exposure, stimulus control/worry time, cognitive restructuring with a focus on problem orientation and developing tolerance of uncertainty), not part of the CBT manual used in the current study but part of CBT manuals that have demonstrated efficacy in some prior studies (e.g., Ladouceur et al., 2000; Wetherell et al., 2003), would show different results than found here when combined with medication.
5. CONCLUSON
No benefit was found for adding CBT to medication treatment, as compared to medication alone, in the context of patients who were seeking medication treatment. Generalizability of these results across different settings and using different methods of recruitment should be evaluated in future research, as such findings have direct clinical relevance.
Research highlights.
Patients seeking medication for GAD were offered cognitive-behavior therapy (CBT).
One–third accepted and attended at least one CBT treatment session.
Combined treatment was not superior to venlafaxine XR alone on any outcome measures.
Acknowledgements
This research was supported by National Institute of Mental Health (NIMH) grant R34-MH072678. The parent study was supported by NIMH grant R01-065963. Wyeth Laboratories provided study medications for the parent study. The authors report no financial involvement or affiliation with any organization whose financial interests may be affected by material in this article.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Ballenger JC. Clinical guidelines for establishing remission in patients with depression and anxiety. Journal of Clinical Psychiatry. 1999;60:29–34. Retrieved from http://www.psychiatrist.com/pastppp/tocs.asp?toc=t60x22. [PubMed] [Google Scholar]
- Barlow DH. Anxiety and its disorders. 2nd ed. New York: Guilford; 2002. [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. Journal of the American Medical Association. 2000;283:2529–2536. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- Bech P. Rating scales for psychopathology, health status and quality of life. New York: Springer-Verlag; 1993. [Google Scholar]
- Beck AT, Emery G. Anxiety disorders and phobias: A cognitive perspective. New York: Basic Books; 1985. [Google Scholar]
- Blomhoff S, Haug TT, Hellstrom K, Holme I, Humble M, Madsbu HP, Wold JE. Randomised controlled general practice trial of sertraline, exposure therapy and combined treatment in generalised social phobia. British Journal of Psychiatry. 2001;179:23–30. doi: 10.1192/bjp.179.1.23. [DOI] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM, Horwood LJ. Anxiety disorders and suicidal behaviors in adolescence and young adulthood: Findings from a longitudinal study. Psychological Medicine. 2007;27:431–440. doi: 10.1017/S0033291706009147. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. Journal of Consulting & Clinical Psychology. 1993;61:611–619. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting & Clinical Psychology. 2002;70:288–298. [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Gillis MM. Cognitive therapy of anxiety disorders. Journal of Consulting & Clinical Psychology. 1993;61:248–260. doi: 10.1037//0022-006x.61.2.248. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Sanderson WC, Shoham V, Bennett Johnson S, Pope KS, Crits-Christoph P, McCurry S. An update on empirically validated therapies. The Clinical Psychologist. 1996;49:5–18. [Google Scholar]
- Chilvers C, Dewey M, Fielding K, Gretton V, Miller P, Palmer B, Harrison G. Antidepressant drugs and generic counseling for treatment of major depression in primary care: randomized trial with patient preference arms. British Medical Journal. 2001;322:772–775. doi: 10.1136/bmj.322.7289.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fifer SK, Mathias SD, Patrick DL, Mazonson PD, Lubeck DP, Buesching DP. Untreated anxiety among adult primary care patients in a Health Maintenance Organization. Archives of General Psychology. 1994;51:740–750. doi: 10.1001/archpsyc.1994.03950090072010. Retrieved from http://archpsyc.ama-assn.org/content/vol51/issue9/index.dtl. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for Axis I DSM-IV disorders (Version 2.0) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Gelenberg AJ, Lydiard RB, Rudolph R, Aguiar L, Haskins JT, Salinas E. Efficacy of venlafaxine extended-release capsules in nondepressed outpatients with generalized anxiety disorder: A 6-month randomized controlled trial. Journal of the American Medical Association. 2000;283:3082–3088. doi: 10.1001/jama.283.23.3082. [DOI] [PubMed] [Google Scholar]
- Gillis MM, Haaga DAF, Ford GT. Normative values for the Beck Anxiety Inventory, Fear Questionnaire, Penn State Worry Questionnaire, and Social Phobia and Anxiety Inventory. Psychological Assessment. 1995;7:450–455. [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Ruan WJ, Goldstein RB, Huang B. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2005;35:1747–1759. doi: 10.1017/S0033291705006069. [DOI] [PubMed] [Google Scholar]
- Guy W, editor. ECDEU assessment manual for psychopharmacology, revised. DHEW Pub. No. (ADM) 76-338. Rockville, MD: National Institute of Mental Health; 1976. [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harman JS, Rollman BL, Hanusa BH, Lenze EJ, Shear MK. Physician office visits of adults for anxiety disorders in the United States, 1985–1998. Journal of General Internal Medicine. 2002;17:165–172. doi: 10.1046/j.1525-1497.2002.10409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Follette WC, Revenstorf D. Psychotherapy outcome research: methods for reporting variability and evaluating clinical significance. Behavior Therapy. 1984;15:336–352. [Google Scholar]
- Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, Zajecka J. A comparison of nefazodone, the cognitive-behavioral analysis system of psychotherapy, and their combination for the treatment of chronic depression. The New England Journal of Medicine. 2000;342:1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;6:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Keller MB, Wittchen HU. The epidemiology of generalized anxiety disorder. Psychiatric Clinics of North America. 2001;24:19–39. doi: 10.1016/s0193-953x(05)70204-5. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Stang P, Wittchen HU, Stein M, Walters EE. Lifetime comorbidities between social phobia and mood disorders in the US National Comorbidity Survey. Psychological Medicine. 1999;29:555–567. doi: 10.1017/s0033291799008375. [DOI] [PubMed] [Google Scholar]
- Kozak JM, Leibowitz MR, Foa EB. Cognitive behavior therapy for obsessive-compulsive disorder: The NIMH sponsored collaborative study. In: Goodman WK, Rudorfer MV, editors. Obsessive-compulsive disorders: Contemporary issues in treatment: Personality and clinical psychology series. Mahwah, NJ: Erlbaum; 2000. [Google Scholar]
- Lin P, Campbell DG, Chaney EF, Liu C-F, Heagerty P, Felkber BL, Hedrick SC. The influence of consumer preference on depression treatment in primary care. Annals of Behavioral Medicine. 2005;30:164–173. doi: 10.1207/s15324796abm3002_9. [DOI] [PubMed] [Google Scholar]
- Lader MH, Bond AJ. Interaction of pharmacological and psychological treatments of anxiety. British of Journal Psychiatry. 1998;17:42–48. Retrieved from http://bjp.rcpsych.org/ [PubMed] [Google Scholar]
- Ladouceur R, Dugas MJ, Freeston MH, Leger E, Gagnon F, Thibodeau N. Efficacy of a cognitive-behavioral treatment for generalized anxiety disorder: Evaluation in a controlled clinical trial. Journal of Consulting and Clinical Psychology. 2000;68:957–964. [PubMed] [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS system for mixed models. Cary, North Carolina: SAS Institute; 1996. [Google Scholar]
- Massion AO, Warshaw MG, Keller MB. Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. American Journal of Psychiatry. 1993;150:600–607. doi: 10.1176/ajp.150.4.600. Retrieved from http://ajp.psychiatryonline.org/content/vol150/issue4/index.dtl. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behavior Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mitte K. Meta-analysis of cognitive-behavioral treatments for generalized anxiety disorder: A comparison with pharmacotherapy. Psychological Bulletin. 2005;131:785–795. doi: 10.1037/0033-2909.131.5.785. [DOI] [PubMed] [Google Scholar]
- Mitte K, Noack P, Steil R, Hautzinger M. A meta-analytic review of the efficacy of drug treatment in generalized anxiety disorder. Journal of Clinical Psychopharmacology. 2005;25:141–150. doi: 10.1097/01.jcp.0000155821.74832.f9. [DOI] [PubMed] [Google Scholar]
- Newman MG, Borkovec TD. Cognitive-behavioral therapy for worry and generalized anxiety disorder. In: Simos G, editor. Cognitive behavioural therapy: A guide for the practising clinician. New York: Taylor & Francis; 2002. pp. 150–172. [Google Scholar]
- Newman MG, Fisher AJ. Expectancy/ Credibility change as a mediator of cognitive behavioral therapy for generalized anxiety disorder: mechanism of action or proxy for symptom change? International Journal of Cognitive Therapy. 2010;3:245–261. doi: 10.1521/ijct.2010.3.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack MH, Zaninelli R, Goddard A, McCafferty JP, Bellew KM, Burnham DB, Iyengar MK. Paroxetine in the treatment of generalized anxiety disorder: Results of a placebo-controlled, flexible-dosage trial. Journal of Clinical Psychiatry. 2001;62:350–357. doi: 10.4088/jcp.v62n0508. Retrieved from http://www.psychiatrist.com/pastppp/tocs.asp?toc=t6205. [DOI] [PubMed] [Google Scholar]
- Power K, Simpson R, Swanson V, Wallace L, Feistner A, Sharp D. A controlled comparison of cognitive-behaviour therapy diazepam, and placebo, alone and in combination, for the treatment of generalized anxiety disorder. Journal of Anxiety Disorders. 1990;4:267–292. [Google Scholar]
- Rickels K, Etemad B, Khalid-Khan S, Lohoff F, Rynn M, Gallop R. Time to relapse after 6 and 12 months treatment of generalized anxiety disorder with venlafaxine XR. Archives of General Psychiatry. 2010;76:1274–1281. doi: 10.1001/archgenpsychiatry.2010.170. [DOI] [PubMed] [Google Scholar]
- Rickels K, Rynn M. Pharmacotherapy of generalized anxiety disorder. Journal of Clinical Psychiatry. 2002;63:9–16. Retrieved from http://www.psychiatrist.com/pastppp/tocs.asp?toc=t63s14. [PubMed] [Google Scholar]
- Robins LN, Regier DA. Psychiatric disorders in America: the epidemiologic catchment area study. New York: The Free Press; 1991. [Google Scholar]
- Roemer L, Orsillo SM. Expanding our conceptualization of and treatment for generalized anxiety disorder: Integrating mindfulness/acceptance-based approaches with existing cognitive-behavioral models. Clinical Psychology- Science & Practice. 2002;9:54–68. [Google Scholar]
- Thase ME, Greenhouse JB, Frank E, Reynolds CF, Pilkonis PA, Hurley K, Kupfer DJ. Treatment of major depression with psychotherapy or psychotherapy-pharmacotherapy combinations. Archives of General Psychiatry. 1997;54:1009–1015. doi: 10.1001/archpsyc.1997.01830230043006. Retrieved from http://archpsyc.ama-assn.org/content/vol54/issue11/index.dtl. [DOI] [PubMed] [Google Scholar]
- Wetherell JL, Gatz M, Craske MG. Treatment of generalized anxiety disorder in older adults. Journal of Consulting and Clinical Psychology. 2003;71:31–40. doi: 10.1037//0022-006x.71.1.31. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Boyer P. Screening for anxiety disorders. British Journal of Psychiatry. 1998;173:10–17. [PubMed] [Google Scholar]
- Wittchen HU, Carter RM, Pfister H, Montgomery SA, Kessler RC. Disabilities and quality of life in pure and comorbid generalized anxiety disorder and major depression in a national survey. International Clinical Psychopharmacology. 2000;15:319–328. doi: 10.1097/00004850-200015060-00002. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Kessler RC, Beesdo K, Krause P, Hofler M, Hoyer J. Generalized anxiety and depression in primary care: prevalence, recognition, and management. Journal of Clinical Psychiatry. 2002;63:24–34. Retrieved from http://www.psychiatrist.com/pastppp/tocs.asp?toc=t63x08. [PubMed] [Google Scholar]
- Yonkers KA, Dyck IR, Warshaw M, Keller MB. Factors predicting the clinical course of generalized anxiety disorder. British Journal of Psychiatry. 2000;176:544–549. doi: 10.1192/bjp.176.6.544. Retrieved from http://bjp.rcpsych.org/content/vol176/issue6/ [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Warshaw MG, Massion AO, Keller MB. Phenomenology and course of generalized anxiety disorder. British Journal of Psychiatry. 1996;168:308–313. doi: 10.1192/bjp.168.3.308. Retrieved from http://bjp.rcpsych.org/content/vol168/issue3/ [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]