Abstract
Candid1, a live-attenuated Junin virus vaccine strain, was developed during the early 1980s to control Argentine hemorrhagic fever, a severe and frequently fatal human disease. Six amino acid substitutions were found to be unique to this vaccine strain, and their role in virulence attenuation in mice was analyzed using a series of recombinant viruses. Our results indicate that Candid1 is attenuated in mice through a single amino acid substitution in the transmembrane domain of the G2 glycoprotein. This work provides insight into the molecular mechanisms of attenuation of the only arenavirus vaccine currently available.
TEXT
Junin virus (JUNV), a New World arenavirus (family Arenaviridae), is the causative agent of Argentine hemorrhagic fever (AHF), a severe human disease with a 15 to 30% fatality ratio in untreated cases (7, 11). Arenaviruses are enveloped viruses with 2 single-stranded genomic RNA segments, S (∼3.4 kb) and L (∼7.2 kb), which encode 4 viral proteins in ambisense orientation. S encodes the glycoprotein precursor (GPC) and the nucleoprotein (N), while L encodes the matrix protein (Z) and the viral polymerase (L). Mature G1 and G2 surface proteins are generated by GPC cleavage by the Golgi protease SKI-1/S1P (9).
First isolated from a human patient in 1958 (23), JUNV causes periodic seasonal outbreaks involving up to 1,000 cases per year in areas of endemicity in Argentina (12). JUNV is maintained in nature by rodent reservoirs, primarily Calomys musculinus (22); transmission to humans occurs following inhalation of infectious aerosols or by direct contact with infected animal excreta (20). AHF treatment is limited to administering convalescent patient serum and supportive nursing care during the early disease stages (12).
The high fatality rates and public health impact of AHF prompted the development of a live-attenuated vaccine, Candid1, during the 1980s (7). After intensive testing of the vaccine prototype in animals and healthy human volunteers, large-scale phase III and IV human trials were performed in Argentina (21). The successful outcome of these studies was followed by the administration of Candid1 to over 200,000 people in areas of endemicity in central Argentina, significantly decreasing AHF incidence (11).
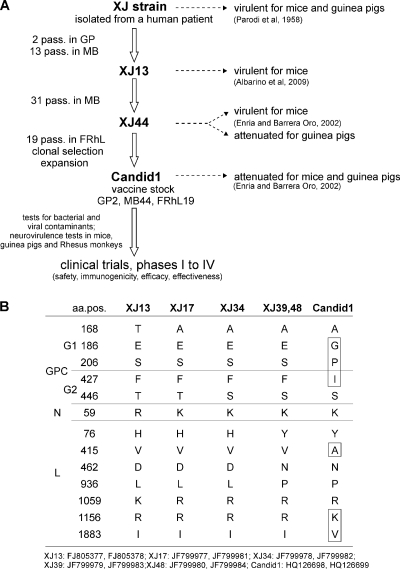
Despite the apparent quality, safety, and efficacy of the original Candid1 vaccine, concerns exist regarding its genetic homogeneity (10) and the limited understanding of the molecular mechanisms responsible for its attenuated phenotype (14, 15). The vaccine was developed by serial passages of the virulent human isolate XJ in guinea pigs, mice, and fetal rhesus lung (FRhL) cells (Fig. 1A). The resulting in vivo phenotype of the vaccine changed in at least 2 major steps. After numerous intracranial passages in mice, the virus became avirulent in guinea pigs (Fig. 1A) and was attenuated for mice after clonal selection and propagation in FRhL cells. It is likely that the final attenuation steps were essential toward generating the current Candid1 vaccine (7, 11).
Fig. 1.
(A) Development of the Candid1 vaccine. This live-attenuated vaccine virus was originated from human clinical material and was passaged twice in guinea pigs (GP2) and 44 times in mouse (MB44), followed by clonal selection and stock amplification through 19 passages in fetal rhesus monkey lung cells (FRhL19). Virulence in mice and guinea pigs is indicated on the right side of the figure. (B) Sequence comparisons of Candid1 and its parental strains. For XJ-derived viruses (XJ13, XJ17, XJ34, XJ39, and XJ48), total RNA was purified from mouse brain lysates and used for reverse transcriptase PCR (RT-PCR) amplifications and sequencing. For Candid1, total RNA extracted from an original vial of the vaccine was used as input material. Amino acid positions (aa.pos.) correspond to each individual viral protein: GPC, N, and L. No mutations were found in Z or in nontranslated regions. XJ48 was derived from the Candid1 parental strain XJ44 and had a sequence identical to that of XJ39. GenBank accession numbers are listed for each strain.
To study Candid1 attenuation, we previously developed a robust and highly efficient reverse genetics system for producing infectious JUNV based on the transfection of 2 plasmids transcribing the S and L antigenomic RNAs. This system allowed us to generate the virulent XJ13 strain (3) and a genetically defined stock of Candid1 (5).
To examine the molecular mechanisms underlying attenuation, we identified the exact genomic changes unique to Candid1 by comparing the complete genomic sequences of all available XJ-derived strains. To avoid spurious mutations that could have arisen during subsequent passages in cell culture, we used an original vial of the vaccine and the original mouse brain specimens to determine the complete genomic sequences of XJ13, XJ17, XJ34, XJ39, and Candid1. We did not include the sequence of XJ44 in our analyses, since its only available source was from late cell culture passages (6, 15). However, the sequence of a later-passage strain, XJ48, is identical to that of XJ39, suggesting that no mutations arose between XJ39 and XJ44. Sequence analyses showed that Candid1 accumulated 13 amino acid substitutions compared to XJ13, the most parental strain available. Seven of these changes were acquired during passages in mouse brain, and the remaining 6 (2 in G1, 1 in G2, and 3 in L) emerged during clonal selection in FRhL cells (Fig. 1B). Since the earlier 7 amino acid changes did not significantly reduce the virulent phenotype of XJ44 in mice (11), we hypothesized that the 6 remaining mutations were the most likely determinants of Candid1 attenuation.
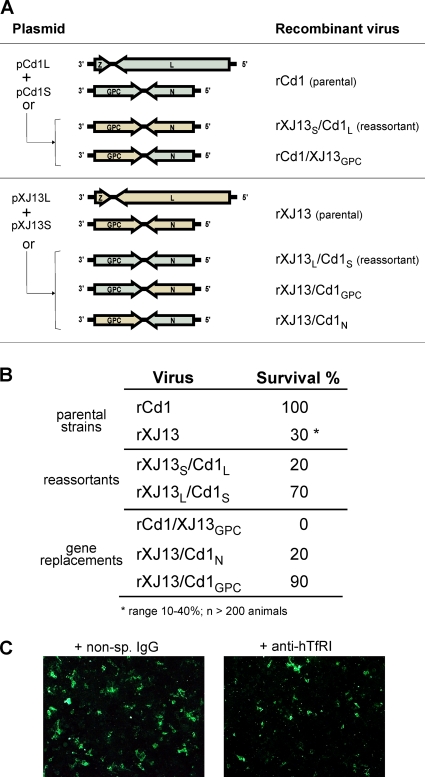
To examine the potential role of these genetic markers, we constructed a complete series of XJ13- and Candid1-derived recombinant viruses (Fig. 2A) as described previously (3) and compared their levels of virulence in the lethal mouse model. Recombinant viruses (rJUNV) were injected intracranially into 14-day-old mice (10/group) at a dose of 500 50% tissue culture infective doses (TCID50) per mouse; the infected mice were examined daily for signs of clinical disease or mortality for up to 28 days postinfection. Infection with the reverse genetics-generated parental strains rCandid1 and rXJ13 resulted in 100% and 30% survival, respectively (Fig. 2B, top). The reassortant viruses rXJ13S/Cd1L (containing the XJ13 S segment and the Candid1 L segment) and rXJ13L/Cd1S (containing the Candid1 S segment and the XJ13 L segment) led to 20% and 70% mouse survival, respectively, suggesting that the S segment plays a major role in Candid1 attenuation (Fig. 2B, middle).
Fig. 2.
(A) Schematic of plasmids used to generate fully infectious viruses. Recombinant viruses were generated in BSRT7/5 cells and passaged twice in VeroE6 cells as previously described (3, 4). The indicated combinations of plasmids were used to rescue the parental strains, S and L reassortant viruses, and viruses carrying gene replacements. The sequences of the parental strains correspond to GenBank accession no. HQ126700, HQ126701, FJ805379, and JN200801. (B) Virulence testing in the mouse model. Recombinant viruses were assayed by intracranially injecting 500 TCID50/mouse into 14-day-old mice. Infected mice (10 animals/group) were examined for clinical signs and mortality for 28 days postinfection. (C) hTfR1 receptor usage by JUNV Candid1. 293T cells were incubated for 30 min with 200 nM nonspecific mouse IgG2a (Southern Biotech) or anti-hTfR1 (clone M-A712; BD Biosciences) antibody. After treatment, cells were infected with 0.5 PFU/cell of JUNV Candid1. Twenty hours later, the cell monolayer was fixed and analyzed by immunofluorescence assay (IFA) using an anti-JUNV rabbit serum and an anti-rabbit Alexa Fluor 488 secondary antibody (Invitrogen).
We then determined whether the attenuation marker was located in GPC, in N, or in both genes by successfully exchanging genes between the XJ13 and Candid1 viruses (Fig. 2A, bottom). Injecting mice with rCd1/XJ13GPC, rXJ13/Cd1N, and rXJ13/Cd1GPC led to 0%, 20%, and 90% survival, respectively, indicating that the Candid1 GPC alone conferred the attenuated phenotype (Fig. 2B, bottom).
The above described observation led us to investigate the potential role of the unique amino acid substitutions located in the G1 and G2 structural glycoproteins of Candid1 in attenuation. The E186G and S206P substitutions in G1 could potentially disrupt interactions with the human cellular receptor hTfR1 (24) and affect viral entry into human cells. Earlier studies demonstrate that New World pathogenic arenaviruses, including Junin XJ13, Machupo, Guanarito, and Sabia viruses, all use hTfR1, and the specific G1 residues involved in the interaction between hTfR1 and G1 of the Machupo arenavirus have been identified by X-ray crystallography (1). However, these particular residues are conserved between JUNV XJ13 and Candid1 strains and do not include residue 186 or 206. Additionally, hTfR1 usage by Candid1 virus was confirmed by blocking viral entry into human cells with specific anti-hTfR1 antibodies (24, 25) (Fig. 2C).
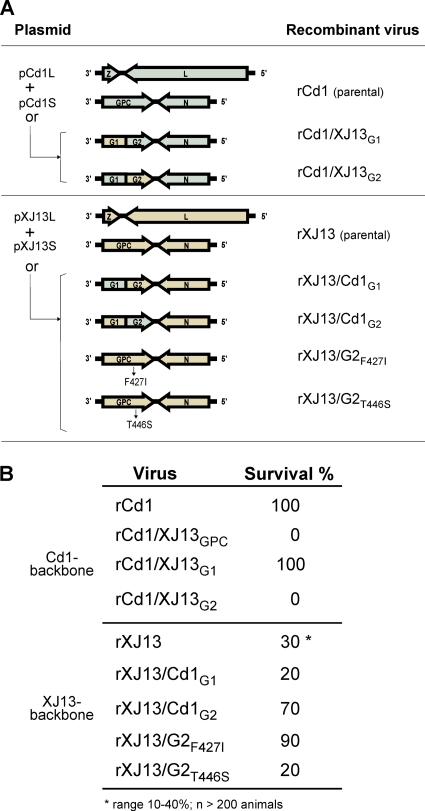
To experimentally examine the potential attenuation role of all amino acid substitutions in both G1 and G2, we constructed a new set of recombinant viruses exchanging G1 and G2 (Fig. 3A). Injecting mice with rCd1/XJ13G1 and rCd1/XJ13G2 resulted in 100% and 0% survival, respectively, indicating that G2 contained the major virulence determinant. This conclusion was further confirmed by testing the equivalent XJ13-derived viruses rXJ13/Cd1G1 and rXJ13/Cd1G2, which yielded 20% and 70% mouse survival, respectively (Fig. 3B).
Fig. 3.
(A) Schematic of plasmids used to generate fully infectious viruses. Recombinant viruses were generated as described before (3, 4). The indicated combinations of plasmids were used to rescue the parental strains, viruses carrying G1 and G2 replacements, and viruses carrying single-amino-acid changes. (B) Virulence assays in the mouse model were performed as explained in the legend for Fig. 2.
Sequence analysis of the G2 glycoprotein (Fig. 1B) revealed 2 amino acid substitutions, F427I and T446S, in Candid1 relative to XJ13; these are located in the transmembrane domain (TMD) and the cytoplasmic tail (CT), respectively. Since F427I, but not T446S, is unique to Candid1, we hypothesized that this mutation conferred attenuation and used recombinant viruses with both single amino acid substitutions (Fig. 3A) to test our hypothesis. As expected, rXJ13/G2F427I and rXJ13/G2T446S viruses exhibited very different phenotypes, yielding 90% and 20% mouse survival, respectively (Fig. 3B, bottom), confirming the role of the TMD mutation F427I in virulence attenuation.
The contribution of viral genomic elements to in vivo phenotype is well described for various arenaviruses (19, 26). Our findings identify for the first time a critical in vivo virulence determinant in the arenavirus G2 TMD. This result is consistent with earlier studies showing that the TMD of surface glycoproteins of other viruses affects their maturation and fusogenic or attachment properties (8, 16–18, 27). Additionally, the TMD and CT regions of JUNV G2 are essential for the transport and maturation of glycoproteins through interactions with the stable signal peptide (2). Interestingly, an F427A mutation was detected during a screening of small-molecule antiviral compounds and in a study on membrane fusion defects (28, 29).
To further examine whether this G2 TMD mutation could decrease virulence in other arenaviruses and to evaluate it as a potential target for generating live-attenuated vaccines for other arenaviral threat agents, we introduced Candid1 TMD and CT mutations into the equivalent positions of the GPC of Lassa virus (LASV), an Old World arenavirus (Fig. 4A). Initial experiments utilized HIV-based pseudotype particles expressing luciferase (13) and decorated with either the wild-type (wt) or mutant LASV GPC. As a negative control for the passive transfer of the luciferase signal, we used the ΔSKI1 mutant (5), which lacks the SKI-1/S1P cleavage recognition site and thus prevents GPC cleavage and generation of infectious particles. The TMD, but not CT, substitution significantly reduced infectivity, as seen by decreased viral particle entry (Fig. 4B and C). Using our previously described reverse genetics system (4), we attempted to rescue recombinant LASVs (rLASV) with engineered CT or TMD mutations. In contrast to recombinant XJ13 viruses rXJ13/G2F427I and rXJ13/G2T446S, which grew similarly to wt viruses, rLASV carrying the TMD, but not the CT, mutation exhibited greatly reduced in vitro growth as observed by the small number of large foci in transfected BSRT7/5 cells and during the first passage on VeroE6 cells (data not shown). Unexpectedly, the rLASVTMD mutant began growing robustly after a second passage in VeroE6 cells, coinciding with the generation of spontaneous mutations in the TMD region (Fig. 4D and E). In marked contrast, all working stocks of the other rJUNV and rLASV recombinant viruses were sequenced to completion (3, 5) and contained no unintended mutations. While these findings suggest that the TMD region is a fruitful target for attenuating other arenaviruses, an intensive mutation screening is required to find suitable positions for residue changes that attenuate virulence without altering growth rates.
Fig. 4.
(A) Sequence alignment of the critical G2 regions of JUNV and LASV. Amino acid changes were introduced into the TMD or the CT region of LASV GPC to mimic the equivalent location within Candid1. (B) Western blot analysis of the glycoprotein content of HIV-based pseudotypes. (C) 293T cells were infected with HIV-LASV pseudotypes, and luciferase activity was measured in the supernatant collected 3 days postinfection. RLU, relative luciferase units; error bars indicate standard deviations. (D) Sequence comparison of recombinant LASVs. Amino acid positions correspond to GPC. No mutations were found in rLASV or rLASVCT virus during passage in VeroE6 cells. The rLASVTMD mutant virus acquired spontaneous mutations after the second passage in VeroE6 cells. (E) Growth kinetics of recombinant LASV. Growth curves were generated by infecting VeroE6 cells with 0.1 PFU/cell of recombinant LASVs. Supernatants were collected at 24-h intervals, and virus titers were determined with a TCID50 assay. rLASV, wild type; rLASVCT, CT mutant; rLASVTMD, TMD mutant; rLASVTMD(rev), TMD revertant.
In conclusion, our experiments reveal a critical role of the TMD in JUNV virulence in mice. Our results also present an opportunity to improve upon the current Candid1 vaccine by eliminating genomic heterogeneity and to extrapolate to other rationally designed arenavirus vaccines.
Acknowledgments
We thank K. Conzelmann for providing BSRT7/5 cells and J. Barrera-Oro for providing an original vial of the Candid1 vaccine and the mouse brain lysates from which the XJ-derived viruses were propagated. We also thank Marina Khristova for her support with JUNV genome sequencing, Tatyana Klimova for her assistance during the editing process, and Brock Martin for his excellent support during animal experimentation under biosafety level 4 (BSL4) conditions.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Footnotes
Published ahead of print on 27 July 2011.
REFERENCES
- 1. Abraham J., Corbett K. D., Farzan M., Choe H., Harrison S. C. 2010. Structural basis for receptor recognition by New World hemorrhagic fever arenaviruses. Nat. Struct. Mol. Biol. 17:438–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Agnihothram S. S., York J., Nunberg J. H. 2006. Role of the stable signal peptide and cytoplasmic domain of G2 in regulating intracellular transport of the Junin virus envelope glycoprotein complex. J. Virol. 80:5189–5198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Albarino C. G., et al. 2009. Efficient reverse genetics generation of infectious Junin viruses differing in glycoprotein processing. J. Virol. 83:5606–5614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Albarino C. G., et al. 2011. Efficient rescue of recombinant Lassa virus reveals the influence of S segment noncoding regions on virus replication and virulence. J. Virol. 85:4020–4024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Albarino C. G., et al. 2011. Reverse genetics generation of chimeric infectious Junin/Lassa virus is dependent on interaction of homologous glycoprotein stable signal peptide and G2 cytoplasmic domains. J. Virol. 85:112–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Albarino C. G., et al. 1997. Molecular characterization of attenuated Junin virus strains. J. Gen. Virol. 78:1605–1610 [DOI] [PubMed] [Google Scholar]
- 7. Barrera Oro J. G., McKee K. T., Jr 1991. Toward a vaccine against Argentine hemorrhagic fever. Bull. Pan Am. Health Organ. 25:118–126 [PubMed] [Google Scholar]
- 8. Bissonnette M. L., Donald J. E., DeGrado W. F., Jardetzky T. S., Lamb R. A. 2009. Functional analysis of the transmembrane domain in paramyxovirus F protein-mediated membrane fusion. J. Mol. Biol. 386:14–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buchmeier M. J., Peters C. J., C. de la Torre J. 2007. Arenaviridae: the viruses and their replication, p. 1792–1827.In Knipe D. M., et al. (ed.), Fields virology, 5th ed., vol. 2. Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 10. Contigiani M., Medeot S., Diaz G. 1993. Heterogeneity and stability characteristics of Candid 1 attenuated strain of Junin virus. Acta Virol. 37:41–46 [PubMed] [Google Scholar]
- 11. Enria D. A., Barrera Oro J. G. 2002. Junin virus vaccines. Curr. Top. Microbiol. Immunol. 263:239–261 [DOI] [PubMed] [Google Scholar]
- 12. Enria D. A., Briggiler A. M., Sanchez Z. 2008. Treatment of Argentine hemorrhagic fever. Antiviral Res. 78:132–139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Flint M., Logvinoff C., Rice C. M., McKeating J. A. 2004. Characterization of infectious retroviral pseudotype particles bearing hepatitis C virus glycoproteins. J. Virol. 78:6875–6882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Goni S. E., et al. 2006. Genomic features of attenuated Junin virus vaccine strain candidate. Virus Genes 32:37–41 [DOI] [PubMed] [Google Scholar]
- 15. Goni S. E., et al. 2010. Molecular analysis of the virulence attenuation process in Junin virus vaccine genealogy. Virus Genes 40:320–328 [DOI] [PubMed] [Google Scholar]
- 16. Harman A., Browne H., Minson T. 2002. The transmembrane domain and cytoplasmic tail of herpes simplex virus type 1 glycoprotein H play a role in membrane fusion. J. Virol. 76:10708–10716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hout D. R., et al. 2005. Scrambling of the amino acids within the transmembrane domain of Vpu results in a simian-human immunodeficiency virus (SHIVTM) that is less pathogenic for pig-tailed macaques. Virology 339:56–69 [DOI] [PubMed] [Google Scholar]
- 18. Hsieh S. C., Tsai W. Y., Wang W. K. 2010. The length of and nonhydrophobic residues in the transmembrane domain of dengue virus envelope protein are critical for its retention and assembly in the endoplasmic reticulum. J. Virol. 84:4782–4797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liang Y., Lan S., Ly H. 2009. Molecular determinants of Pichinde virus infection of guinea pigs—a small animal model system for arenaviral hemorrhagic fevers. Ann. N. Y. Acad. Sci. 1171(Suppl. 1): E65–E74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Maiztegui J. I. 1975. Clinical and epidemiological patterns of Argentine haemorrhagic fever. Bull. World Health Organ. 52:567–575 [PMC free article] [PubMed] [Google Scholar]
- 21. Maiztegui J. I., et al. 1998. Protective efficacy of a live attenuated vaccine against Argentine hemorrhagic fever. AHF Study Group. J. Infect. Dis. 177:277–283 [DOI] [PubMed] [Google Scholar]
- 22. Mills J. N., et al. 1994. Prevalence of infection with Junin virus in rodent populations in the epidemic area of Argentine hemorrhagic fever. Am. J. Trop. Med. Hyg. 51:554–562 [PubMed] [Google Scholar]
- 23. Parodi A. S., et al. 1958. Concerning the epidemic outbreak in Junin. Dia Med. 30:2300–2301(In Spanish.) [PubMed] [Google Scholar]
- 24. Radoshitzky S. R., et al. 2007. Transferrin receptor 1 is a cellular receptor for New World haemorrhagic fever arenaviruses. Nature 446:92–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Radoshitzky S. R., et al. 2008. Receptor determinants of zoonotic transmission of New World hemorrhagic fever arenaviruses. Proc. Natl. Acad. Sci. U. S. A. 105:2664–2669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Riviere Y., Ahmed R., Southern P. J., Buchmeier M. J., Oldstone M. B. 1985. Genetic mapping of lymphocytic choriomeningitis virus pathogenicity: virulence in guinea pigs is associated with the L RNA segment. J. Virol. 55:704–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ronecker S., Zimmer G., Herrler G., Greiser-Wilke I., Grummer B. 2008. Formation of bovine viral diarrhea virus E1–E2 heterodimers is essential for virus entry and depends on charged residues in the transmembrane domains. J. Gen. Virol. 89:2114–2121 [DOI] [PubMed] [Google Scholar]
- 28. York J., Dai D., Amberg S. M., Nunberg J. H. 2008. pH-induced activation of arenavirus membrane fusion is antagonized by small-molecule inhibitors. J. Virol. 82:10932–10939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. York J., Nunberg J. H. 2009. Intersubunit interactions modulate pH-induced activation of membrane fusion by the Junin virus envelope glycoprotein GPC. J. Virol. 83:4121–4126 [DOI] [PMC free article] [PubMed] [Google Scholar]